Abstract
Purpose
Hot flashes are a significant problem for many breast cancer survivors. Hot flashes can cause discomfort, disrupted sleep, anxiety, and decreased quality of life. A well-tolerated and effective mind-body treatment for hot flashes would be of great value. On the basis of previous case studies, this study was developed to evaluate the effect of a hypnosis intervention for hot flashes.
Patients and Methods
Sixty female breast cancer survivors with hot flashes were randomly assigned to receive hypnosis intervention (five weekly sessions) or no treatment. Eligible patients had to have a history of primary breast cancer without evidence of detectable disease and 14 or more weekly hot flashes for at least 1 month. The major outcome measure was a bivariate construct that represented hot flash frequency and hot flash score, which was analyzed by a classic sums and differences comparison. Secondary outcome measures were self-reports of interference of hot flashes on daily activities.
Results
Fifty-one randomly assigned women completed the study. By the end of the treatment period, hot flash scores (frequency × average severity) decreased 68% from baseline to end point in the hypnosis arm (P < .001). Significant improvements in self-reported anxiety, depression, interference of hot flashes on daily activities, and sleep were observed for patients who received the hypnosis intervention (P < .005) in comparison to the no treatment control group.
Conclusion
Hypnosis appears to reduce perceived hot flashes in breast cancer survivors and may have additional benefits such as reduced anxiety and depression, and improved sleep.
INTRODUCTION
Hot flashes (or vasomotor symptoms) are a major clinical problem for many women as they enter menopause and for breast cancer survivors. Hot flashes occur as a result of estrogen depletion,1 can significantly alter daily activities, and can affect perceptions of mood and sleep.2,3 Furthermore, hot flashes are a common adverse effect of ovarian ablation, tamoxifen, and aromatase inhibitors used in breast cancer treatment. It has been demonstrated that up to 78% of female chemotherapy recipients and 72% of tamoxifen recipients experience hot flashes.4 Estrogens have been the treatment of choice for hot flashes, but estrogens have been associated with an increased risk of breast cancer and, therefore, are generally avoided for breast cancer survivors.5 Nonhormonal pharmacologic agents are either not effective for some women or have adverse effects. Given the limited safe and effective options, it is imperative that effective new interventions with minimal adverse effects be developed to help breast cancer survivors who experience hot flashes.
Hypnosis is a mind-body therapy that has few negative adverse effects and that may be of significant benefit in reducing the frequency and severity of hot flashes in breast cancer survivors. Several small studies have suggested that hypnosis intervention may have a positive effect on the reduction of hot flashes. An early study by Stevenson and Delprato6 reported that four women were able to reduce self-reported hot flashes by 41% to 90% from baseline when provided with instruction in relaxation, self-suggestions of cool thoughts, and temperature biofeedback. Three reports have indicated that hypnosis may be an especially promising intervention for hot flashes.7-9 We have developed a well-defined hypnosis intervention in our laboratory; recently, in a small exploratory study,8 we reported a reduction in hot flashes in 16 women after hypnosis intervention. Pursuant to this, the present study was developed to additionally assess the efficacy of hypnosis intervention for the treatment of hot flashes in a randomized, prospective study.
PATIENTS AND METHODS
Eligible patients were at least 18 years of age, had a history of primary breast cancer without evidence of detectable disease, and had a self-reported history of at least 14 hot flashes per week for a period of at least 1 month before study entry. Patients were not allowed to receive any chemotherapy, androgens, estrogens, progestational drugs, or any treatment for hot flashes. Women taking antihormonal agents for breast cancer (eg, tamoxifen, raloxifene) were permitted into the study if they had been taking the drug for at least 1 month before enrollment and had remained on a stable dose. Patients were asked to not participate in any other mind-body therapy (ie, relaxation therapy, biofeedback, yoga) and to not use any other complementary or alternative therapy during the study period.
Participants were equally and randomly assigned to either hypnosis or to a no-treatment control arm. Random assignment was made sequentially from a confidential, computer-generated list of permuted blocks of varying size. All patients were required to give their written informed consent as dictated by federal guidelines and approved by an institutional review board. After random assignment, patients were asked to complete a daily hot flash diary for 1 week before any treatments for hot flashes. Baseline measures also included the Hot Flash Related Daily Interference Scale (HFRDIS),2 Center for Epidemiologic Studies Depression Scale (CES-D),10 Hospital Anxiety and Depression Scale-Anxiety Subscale (HADS-A),11 and Medical Outcomes Study Sleep Scale (MOS-Sleep Scale).12 Patients then received either the hypnosis intervention or remained on a no-treatment waiting list for 5 weeks. At the end of the study period, all participants repeated the measures for a second time.
The hypnosis intervention followed a treatment manual that was developed specifically for this study and was delivered by a clinician with a doctoral degree in psychology who had completed at least 40 hours of training in hypnotherapy provided by the principal investigator. Training followed the guidelines and learning objectives outlined in the publication, Standards of Training in Clinical Hypnosis.13
Patients in the hypnosis intervention condition were scheduled for five weekly sessions, each to last approximately 50 minutes. At each session, a hypnotic induction was completed according to a standard transcript. (The treatment manual is available from G.E. on request). Hypnotic suggestions for each session included the following: hypnotic induction; mental imagery and suggestions for relaxation; mental imagery for coolness; deepening hypnosis and dissociation from hot flashes; positive suggestions and imagery for the future; self-hypnosis; and the alert, “In a few moments, return to conscious alertness.”
In addition, participants were given instruction in self-hypnosis practice and were provided with an audiocassette tape recording of a hypnotic induction and of instructed in-home practice. Although the hypnotic induction followed a transcript, specific imagery for relaxation and imagery for coolness were individualized on the basis of each patient's preference regarding such imagery.
Statistical Considerations
The primary end point for this study was both the frequency of hot flashes and a hot flash severity score. For the participants, the number and severity of hot flashes per day was computed for the baseline week and for the final week. In addition, the severity of hot flashes was computed. One point was given for each mild hot flash, two points for each moderate hot flash, three points for each severe hot flash, and four points for each very severe hot flash. The hot flash score was calculated by multiplying the severity average for a week times the hot flash frequency for that week.
The results of this pre-test–post-test control group design were analyzed via multivariate analysis of covariance and analysis of covariance. The hot flash severity score, the HFRDIS, the HADS anxiety sub-scale, the CES-D depression scale, and the MOS-Sleep Scale were used as pre- and post-tests in these analyses. As follow-up, these post-test scores were also analyzed via a series of two-sample t tests. Confidence intervals of 95% for the change from baseline to end-of-study were computed for all measures for both groups. All statistical tests were performed as two-tailed tests and used a level of significance of P = .05.
A sample size of 25 in each group was based on an 80% power to detect a difference of at least 30% from baseline to follow-up with a .05 one-sided significance level.14
Missing data were handled by using various imputation methods (eg, patients who completed all data, average value carried forward, last value carried forward, and minimum or maximum value carried forward) and were carried out to assess the impact of missing data on the results. The amount of missing data was minimal, and the analyses indicated that the results were consistently demonstrated.
RESULTS
Eight-six patients were screened for this study, of which 26 either did not meet eligibility criteria or did not want to participate. A total of 60 women were randomly assigned. Approximately 20% of the participants who had enrolled were either lost to follow-up (n = 3) or withdrew (n = 6); three had been assigned to the treatment group, and six had been assigned to the control group. Reasons for those who did not complete the study included: being too busy/no desire to continue for personal reasons (n = 7) and not able to be reached (n = 2).
Demographic data from the participants who were randomly assigned to each condition are presented in Appendix Table A1, online only. The baseline average number of hot flashes was well balanced for the study arms. At baseline, there was no significant difference between the participants in each condition, with the exception that there were a greater number of participants who had earned a graduate degree in the treatment group than would be expected by chance (P = .04), but educational levels were relatively evenly distributed between the treatment and control conditions for those who completed the study.
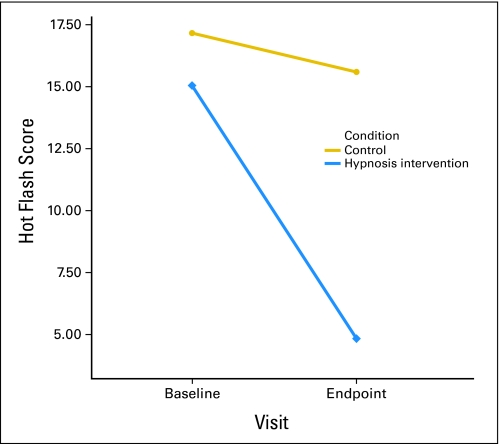
Table 1 lists the results of the initial analyses. The first analysis compared the final measures of hot flashes (hot flash score, HFRDIS) of hypnosis versus control group participants by using a one-way multivariate analysis of covariance. Baseline hot flash scores and the HFRDIS score were used as covariates to control for individual differences. As listed in the table, the results were statistically significant; those in the hypnosis condition reported statistically significantly lower scores on the multivariate hot flash outcome measure than did those in the control group. The effect size (ηp2 = 0.479) is considered of large magnitude when using conventional criteria15 and suggests that the difference should be visible to the naked eye. The means and standard deviations for pre- and post-test scores by group are listed in Appendix Table A2, online only, for these and other outcome variables, which shows improvement in hot flash outcome for both measures. Those in the hypnosis group showed statistically significantly better outcomes for both the hot flash score and the interference score. These results are displayed graphically in Figure 1and Appendix Figure A1, online only.
Table 1.
Effect of Hypnosis Intervention on Hot Flashes, Sleep, and Mood
| Measure and Test | Analyses
|
|||
|---|---|---|---|---|
| F | df | P | η2 (partial) | |
| Hot flashes (HFRDIS) | 19.804 | 2,43 | < .001 | 0.479 |
| Sleep (MOS-Sleep) | 45.757 | 1,48 | < .001 | 0.488 |
| Mood (HADS-A, CES-D) | 6.083 | 2,44 | < .005 | 0.217 |
Abbreviations: HFRDIS, Hot Flash Related Daily Interference Scale; MOS-Sleep, Medical Outcomes Study Sleep Scale; HADS-A, Hospital Anxiety and Depression Scale-Anxiety Subscale; CES-D, Center for Epidemiologic Studies Depression Scale.
Fig 1.
Hot flash scores pre- and post-test by treatment condition.
Table 1 also lists the results of an analysis of covariance of the effects of the hypnosis treatment on participants’ sleep. Ratings on the MOS-Sleep Scale at baseline and at study end were used as the covariate and outcome, respectively. As listed in the table, the difference between groups after treatment was statistically significant and had a large effect size. In Appendix Table A2, the hypnosis group showed significant improvement compared with the control group and improvement compared with their baseline scores.
The third analysis summarized in Table 1 shows the results of the hypnosis treatment on two psychological outcomes, depression and anxiety. The HADS-A and CES-D were used as both pre- and post-test for this multivariate analysis of covariate (MANCOVA). As listed in Table 1, the two groups were indeed statistically significantly different at post-test and had a moderate effect size. Descriptive data and follow-up analyses are listed in Appendix Table A2. Participants in the hypnosis treatment showed statistically significant improvement compared with control participants for both anxiety and depression. Effect sizes for both outcomes were of moderate magnitude.
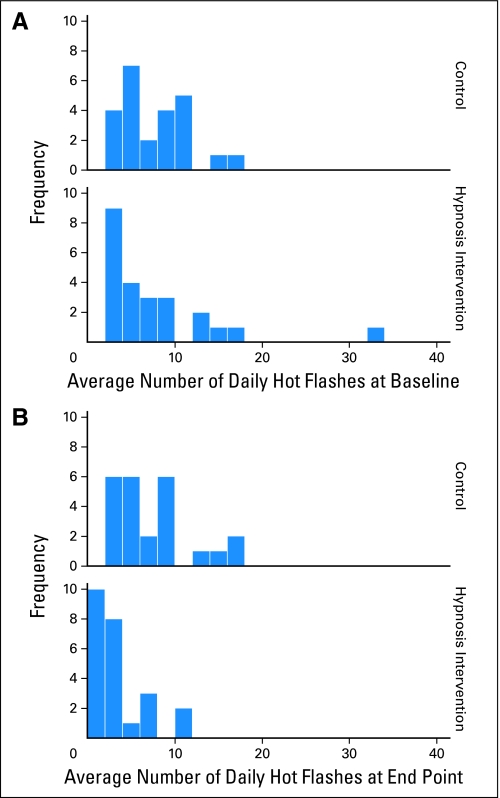
The hot flash score used in the primary analysis was made up of hot flash frequency and severity. Additional follow-up focused on the frequency of hot flashes at baseline and post-test. As in previous analyses, ANCOVA (which used hot flash frequency at pre-test as a covariate and hot flash at end point as the dependent variable) revealed a statistically significant improvement for the hypnosis group compared with the control group. Hot flash scores (frequency × average severity) decreased 68% from baseline to end point in the hypnosis arm (P < .001). Figure 2 shows the distribution of participants’ scores at pre- and post-test by experimental condition. The figure shows the similarity in the two groups at pre-test and the consistent improvement in hot flash frequency for the hypnosis group at post-test.
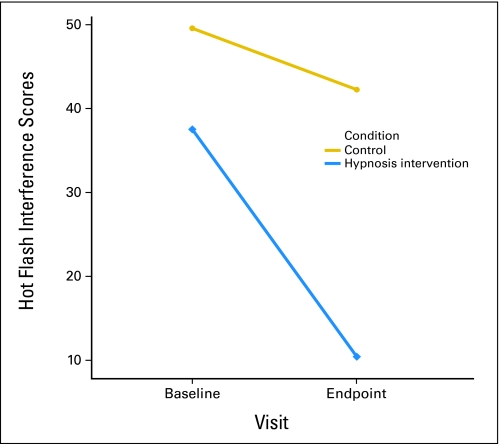
Fig 2.
Hot flash interference scores at pre- and post-test by treatment condition.
To additionally investigate the effects of the hypnosis treatment on the extent that hot flashes interfered with daily life, the items from the HFRDIS (both pre- and post-test) were analyzed in a MANCOVA, with follow-up of individual items. For this scale, women rated the extent that hot flashes have interfered with 10 different aspects of their lives (ie, work, social activities, leisure activities, sleep, mood, concentration, relations with others, sexuality, enjoyment of life, overall quality of life), each on a 10-point scale. The overall MANCOVA was statistically significant (F[10,29] = 4.73; P < .001) and had a large effect size (ηp2 = 0.620); at post-test, hot flashes interfered significantly less in the lives of women in the treatment group compared with those in the control group. Follow-up analyses of each item showed that all items were statistically significantly less interfering (P < .05) for those in the experimental group, with the exception of an item asking about interference with sexuality (P = .124). Effect sizes (ηp2) ranged from 0.061 to 0.437 and from 0.150 to 0.437 for statistically significant items.
DISCUSSION
The results from this study support our pre-study hypothesis that a hypnosis intervention does significantly reduce hot flashes. The effect size was large, and a 68% reduction in hot flash scores indicated a clinically significant reduction. Satisfaction with the hypnosis intervention was favorable, and none of the patients complained or dropped out of treatment because of any negative adverse effects. This is generally consistent with our previous impressions from case studies of hypnosis for hot flashes7,8 and with research on hypnosis for symptom management, and it suggests that hypnosis is a well-tolerated intervention for most patients.16-18
Some criticism of this study is that observations were limited to 5 weeks and that it does not provide data regarding long-term follow-up. However, a ≤ 5-week time period has been used in a series of clinical trials that assessed pharmacologic therapies for alleviating hot flashes in breast cancer survivors, and it does allow comparison.5,19-23 Our anecdotal experience has given us reason to believe that patients who continue to practice self-hypnosis continue to benefit with maintenance of reductions.8 Subsequent studies should use a longer-term follow-up period to determine if sustained symptom relief is achieved with hypnosis.
Although it could be argued that physiologic monitoring of hot flashes is needed to validate the reduction of hot flashes, the use of self-report diaries, as used in this study, has long been established as a valid approach to obtain data on subjective phenomena, such as patient-reported symptoms.19,20,24-26 Self-report diaries have been used in the majority of studies of interventions for hot flashes, and they provide the advantage of data about severity.14 Nonetheless, there may be some clinical utility in using physiologic recordings in clinical trials to gain a better understanding of the mechanism of action and the physiologic impact of hypnosis on hot flashes.
It has been established previously that women with unrelieved hot flashes suffer negative emotional consequences, such as anxiety, depression, interrupted sleep, and decreased quality of life.2,3,27 It is reasonable to hypothesize that interventions that effectively relieve hot flashes would also result in improved mood, affect, and daily activities, including sleep. Women who received the hypnosis intervention in this study did, in fact, report significant improvement on each of these secondary outcomes. Not surprisingly, on enrollment, participants reported significant interference with daily activities as a result of their hot flash experiences. HFRDIS total scores range from 0 to 100. The mean baseline HFRDIS score for the treatment group was 39.52; in contrast, the post-treatment HFRDIS scores were significantly lower than pretreatment, and the mean score was only 10.42. Therefore, this study suggests that hypnosis for hot flashes has additional side benefits that include decreased interference with daily activities and quality of life.
In terms of anxiety, the mean HADS score at baseline was below the cutoff score reported in the literature that indicates possible clinically relevant anxiety. The women who participated in the hypnosis intervention group reported significant reductions in anxiety, which supports the concept that hypnosis to treat hot flashes is also effective to alleviate even subclinical symptoms of anxiety.
However, the reason for these benefits is not entirely clear. Individuals who have negative affect (eg, anxiety, depression) may be more likely to attend to and to report physical symptoms,28 and/or unrelieved hot flashes may result in more frustration and negative consequences.14,27 In either case, this study suggests that the effect of hypnosis is to improve emotional and psychosocial adjustment of women who experience hot flashes.
The mechanism of action of hypnosis to reduce hot flashes is unknown, and this question was not addressed in this study. A substantial placebo effect has been observed in multiple hot flash studies.14,19,20,22,29-33 On average, hot flash frequencies diminish by 20% to 30% with 4 weeks of placebo.14 Also, evidence from other studies suggests that women may tend to under-report hot flashes.34 The feeling of security that results from a mind-body intervention, such as hypnosis, may reinforce this tendency. It is generally accepted that treatments that result in hot flash score reductions of less than 40% should be considered consistent with placebo effect; therefore, interventions that result in hot flash score reductions of greater than 50% should be considered greater than would be expected from placebo.14 These study findings indicate that hypnosis is likely to reduce hot flashes to a greater degree than placebo, by 68%. In this study, the mean number of hot flashes, regardless of severity, exceeded seven per day at baseline. Women who received the hypnosis intervention reported an average reduction of 4.39 hot flashes per day, whereas the women in the control group remained relatively unchanged. It is interesting to note that we did not observe the placebo effect for self-reported hot flashes that is typically observed in clinical trials. This outcome most likely is because the control was a no-treatment condition, which is consistent with findings that hot flashes remain stable over time if left untreated. However, given the percent reduction in hot flashes, the effectiveness of the hypnosis intervention would likely hold up against a parallel arm. A randomized clinical trial is currently underway by the authors to compare the hypnosis intervention to a placebo control and to additionally address the possible underlying mechanisms (eg, stress, serotonin).
Seasonal effects are unlikely to account for findings in this study, because the study intervention occurred during a period longer than 1 year and because the effect size was large. Another concern could be the possible use of other complementary therapies. Patients in this study were required to discontinue all other treatments for hot flashes, with the exception of vitamin E, which has had limited efficacy in relieving hot flashes.21
Women are interested in alternatives to traditional hormone therapy and pharmacologic interventions, and this study demonstrates the feasibility and potential effectiveness of hypnosis as an alternative treatment. However, certification in the professional use of hypnosis requires considerable training13 and practice. Also, some patients may not be good candidates for hypnosis. For example, hypnosis should be avoided or should only be used with caution in patients with a history of severe psychopathology (eg, borderline personality disorder, schizophrenia, post-traumatic stress disorder).35 Also, it is possible that some patients may be in the low range of hypnotizability and, as a result, may benefit less. Future studies should assess these variables. Despite these limitations, it has been our impression that most patients can benefit from hypnosis. However, long-term, randomized, placebo-controlled studies will be needed to identify the long-term effect and integrative role of hypnosis in the treatment of hot flashes.
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTSOF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory Role: Vered Stearns, Concert Pharmaceuticals (C), JDS Pharmaceuticals (C), Myself (C) Stock Ownership: None Honoraria: None Research Funding: Vered Stearns, Novartis, Pfizer Expert Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Gary Elkins, Joel Marcus, Vered Stearns, Michelle Perfect, Hasan Rajab, Christopher Ruud, Lynne Palamara, Timothy Keith
Administrative support: Gary Elkins
Provision of study materials or patients: Gary Elkins
Collection and assembly of data: Gary Elkins, Joel Marcus, Vered Stearns, Michelle Perfect, Hasan Rajab, Christopher Ruud, Lynne Palamara, Timothy Keith
Data analysis and interpretation: Gary Elkins, Joel Marcus, Vered Stearns, Michelle Perfect, Hasan Rajab, Christopher Ruud, Lynne Palamara, Timothy Keith
Manuscript writing: Gary Elkins, Joel Marcus, Vered Stearns, Michelle Perfect, Hasan Rajab, Christopher Ruud, Lynne Palamara, Timothy Keith
Final approval of manuscript: Gary Elkins
Acknowledgments
We thank Jennifer Gibbons-Ramirez, Ashley Kossie, Glen Cryer, Meg Chrisler, and Teresa Cook for their assistance with data collection and manuscript preparation.
Appendix
Fig A1.
Distribution of hot flash frequencies pre- and post-test by treatment condition.
Table A1.
Demographic Characteristics of the Sample by Treatment Group
| Characteristic | Treatment Group
|
|||
|---|---|---|---|---|
| Control
|
Hypnosis
|
|||
| No. | % | No. | % | |
| Mean age, years | 58 years, 2 months | 55 years, 10 months* | ||
| Ethnicity | ||||
| White | 22 | 92 | 26 | 96* |
| African-American | 1 | 4 | 0 | 0* |
| Hispanic | 1 | 4 | 1 | 4* |
| Education | ||||
| High school | 15 | 63 | 8 | 30† |
| Bachelor's degree | 6 | 25 | 9 | 33† |
| Master's degree | 3 | 13 | 10 | 37† |
| Marital status | ||||
| Single | 3 | 13 | 1 | 4* |
| Married | 19 | 79 | 22 | 82* |
| Separated | 1 | 4 | 1 | 4* |
| Widowed | 1 | 4 | 0 | 0* |
| Other | 3 | 11* | ||
| No. of daily hot flashes | ||||
| Mean | 7.52 | 7.77* | ||
| Range | 0.77 | 1.30 | ||
| < 5 | 7 | 29 | 13 | 48* |
| 5-10 | 10 | 42 | 6 | 22* |
| > 10 | 7 | 29 | 8 | 30* |
P value not significant.
P = .04.
Table A2.
Hypnosis Versus Test Condition Pre- and Post-Test Outcomes
| Variable | Measures
|
Analyses
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test
|
Post-Test
|
|||||||||||
| Control
|
Hypnosis
|
Control
|
Hypnosis
|
|||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | F | df | P | ηp2 | |
| Hot flash score | 17.17 | 10.37 | 15.05 | 13.75 | 15.60 | 10.71 | 4.84 | 5.02 | 26.30 | 1,44 | < .001 | 0.374 |
| HFRDIS | 49.54 | 24.26 | 39.52 | 23.35 | 42.23 | 21.95 | 10.42 | 10.69 | 33.41 | 1,44 | < .001 | 0.432 |
| MOS-Sleep | 22.90 | 7.52 | 24.26 | 8.17 | 24.50 | 7.63 | 13.71 | 4.35 | 45.76 | 1,48 | < .001 | 0.488 |
| HADS-A | 5.83 | 5.05 | 5.89 | 4.34 | 6.46 | 5.36 | 3.23 | 3.19 | 9.30 | 1,45 | .004 | 0.171 |
| CES-D | 30.22 | 9.32 | 29.48 | 7.72 | 31.38 | 9.21 | 24.58 | 6.45 | 9.93 | 1,45 | .003 | 0.181 |
| Hot flash frequency | 7.52 | 3.77 | 7.77 | 6.77 | 7.43 | 4.33 | 3.38 | 2.87 | 26.14 | 1,45 | < .001 | 0.367 |
NOTE. F values are based on the univariate follow-up tests for the multivariate analysis of covariate analyses when applicable.
Abbreviations: SD, standard deviation; HFRDIS, Hot Flash Related Daily Interference Scale; MOS-Sleep, Medical Outcomes Study Sleep Scale; HADS-A, Hospital Anxiety and Depression Scale-Anxiety Subscale; CES-D, Center for Epidemiologic Studies Depression Scale.
Supported by Grant No. 1R21 CA100594-01 from the National Cancer Institute and Grant No. U01 AT004634-02 from the National Center for Complementary and Alternative Medicine, National Institutes of Health.
Presented at the 4th Annual Meeting of the American Psychosocial Oncology Society, January 29, 2007, Austin, TX.
Authors’ disclosures of potential conflicts of interest and author contributions are found at the end of this article.
Clinical trial information can be found for the following: 1R21 CA100594-01.
REFERENCES
- 1.Ganong W: Menopause, in: Review of Medical Physiology. Norwalk, CT, Appleton and Lange, 1993, pp 384-396
- 2.Carpenter JS: The Hot Flash Related Daily Interference Scale: A tool for assessing the impact of hot flashes on quality of life following breast cancer. J Pain Symptom Manage 22:979-989, 2001 [DOI] [PubMed] [Google Scholar]
- 3.Lamb MA: Effects of cancer on the sexuality and fertility of women. Semin Oncol Nurs 11:120-127, 1995 [DOI] [PubMed] [Google Scholar]
- 4.Carpenter JS, Andrykowski MA, Cordova M, et al: Hot flashes in postmenopausal women treated for breast carcinoma: Prevalence, severity, correlates, management, and relation to quality of life. Cancer 82:1682-1691, 1998 [PubMed] [Google Scholar]
- 5.Loprinzi CL, Michalak JC, Quella SK, et al: Megestrol acetate for the prevention of hot flashes. N Engl J Med 331:347-352, 1994 [DOI] [PubMed] [Google Scholar]
- 6.Stevenson DW, Delprato D: Multiple component self-control program for menopausal hot flashes. J Behav Ther Exp Psychiatry 14:137-140, 1983 [DOI] [PubMed] [Google Scholar]
- 7.Elkins G, Marcus J, Palamara L, et al: Can hypnosis reduce hot flashes in breast cancer survivors? A literature review. Am J Clin Hypn 47:29-42, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Elkins GR, Stearns V, Marcus J, et al: Pilot evaluation of hypnosis for treatment of hot flashes in breast cancer survivors. Psycho-Oncology 16:487-492, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Younus J, Simpson I, Collins A, et al: Mind control of menopause. Women's Health Issues 13:74-78, 2003 [DOI] [PubMed] [Google Scholar]
- 10.Radloff LS: The CES-D scale; A self-report depression scale for research in the general population. Applied Psychological Measurement, Thousand Oaks, CA, Sage Publications, 1977, pp 385-401
- 11.Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361-370. 1983 [DOI] [PubMed] [Google Scholar]
- 12.Stewart AL, Ware JE: Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham, NC, Duke University Press 1992
- 13.Elkins GR, Hammond DC: Standards of Training in Clinical Hypnosis: Preparing Professionals for the 21st Century. Am J Clin Hypn 41:55-64, 1998 [DOI] [PubMed] [Google Scholar]
- 14.Sloan JA, Loprinzi CL, Novotny PJ, et al: Methodologic lessons learned from hot flash studies. J Clin Oncol 19:4280-4290. 2001 [DOI] [PubMed] [Google Scholar]
- 15.Keith TZ: Multiple regression and beyond. Boston, Allyn & Bacon, 2006
- 16.Montgomery GH, DuHamel KN, Redd WH: A meta-analysis of hypnotically induced analgesia: How effective is hypnosis? Int J Clinical and Experimental Hypnosis, 48:138-153, 2000 [DOI] [PubMed] [Google Scholar]
- 17.Patterson DR, Jensen MP: Hypnosis and clinical pain. Psychol Bull 129:495-521, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Elkins GR, Patterson D, Jensen M: Hypnotherapy for the management of chronic pain, Int J Clin Exp Hypn 55:275-287, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldberg RM, Loprinzi CL, O'Fallon JR, et al: Transdermal clonidine for ameliorating tamoxifen-induced hot flashes. J Clin Oncol 12:155-158, 1996 [DOI] [PubMed] [Google Scholar]
- 20.Loprinzi CL, Pisansky TM, Fonseca R, et al: Pilot evaluation of venlafaxine hydrochloride for the therapy of hot flashes in cancer survivors. J Clin Oncol 16:2377-2381, 1998 [DOI] [PubMed] [Google Scholar]
- 21.Barton DL, Loprinzi CL, Quella SK, Sloan MH, Veeder JR, Egner PF, Stella PJ, Swan DK, Vaught NL, Novotny P: Prospective evaluation of vitamin E for hot flashes in breast cancer survivors. J Clin Oncol 16:495-500, 1998 [DOI] [PubMed] [Google Scholar]
- 22.Loprinzi CL, Kugler JW, Sloan JA, et al: Venlafaxine in management of hot flashes in survivors of breast cancer: A randomised controlled trial. Lancet 356:1486-1490. 2000 [DOI] [PubMed] [Google Scholar]
- 23.Stearns V, Isaccs C, Rowland J, et al: A pilot trial assessing the efficacy of paroxetine hydrochloride (Paxil) in controlling hot flashes in breast cancer survivors. Ann Oncol 11:17-22, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Maunsell E, Allard P, Dorval M, et al: A brief pain diary for ambulatory patients with advanced cancer: Acceptability and validity. Cancer 88:2387-2397, 2000 [PubMed] [Google Scholar]
- 25.Richardson A: The health diary: An examination of its use as a data collection method. J Adv Nurs 19:782-791, 1994 [DOI] [PubMed] [Google Scholar]
- 26.Lippa R, Donaldson SI: Self-monitoring and idiographic measures of behavioral variability across interpersonal relationships. J Pers 58:465-479, 1990 [Google Scholar]
- 27.Carpenter JS, Johnson DH, Wagner LJ, et al: Hot flashes and related outcomes in breast cancer survivors and matched comparison women. Oncol Nurs Forum 29:E16-25, 2002 [DOI] [PubMed] [Google Scholar]
- 28.Watson D, Pennebaker JW: Health complaints, stress and distress: Exploring the central role of negative affectivity. Psychol Review 96:234-254, 1989 [DOI] [PubMed] [Google Scholar]
- 29.Quella SK, Loprinzi CL, Barton JA, et al: Evaluation of soy phytoestrogens for the treatment of hot flashes in breast cancer survivors: A north central cancer treatment group trial. J Clin Oncol 18:1068-1074, 2000 [DOI] [PubMed] [Google Scholar]
- 30.Lancar R, Kramar R, Haie-Meder C: Non-parametric methods for analyzing recurrent complications of varying severity. Stat Med 14:2701-2712, 1995 [DOI] [PubMed] [Google Scholar]
- 31.Loprinzi CL, Goldberg RM, O'Fallon JR, et al: Transdermal clonidine for ameliorating post-orchiectomy hot flashes. J Urol 151:634-636, 1994 [DOI] [PubMed] [Google Scholar]
- 32.Loprinzi CL, Sloan JA, Perez PA, et al: Phase III evaluation of fluoxetine for treatment of hot flashes. J Clin Oncol 20:1578-1583, 2002 [DOI] [PubMed] [Google Scholar]
- 33.Van Patten CL, Olivotto IA, Chambers KG, et al: Effect of Soy Phytoestrogens on Hot Flashes in Postmenopausal women with breast cancer: A randomized, controlled clinical trial. J Clin Oncol 20:1449-1455, 2002 [DOI] [PubMed] [Google Scholar]
- 34.Carpenter JS, Andrykowski MA, Freedman RR, et al: Feasibility and psychometrics of an ambulatory hot flash monitoring device. Menopause 6:209-215, 1999 [DOI] [PubMed] [Google Scholar]
- 35.Rhue JW, Lynn SJ, Kirsch I: Handbook of Clinical Hypnosis. Washington, DC, American Psychological Association, 1993