Abstract
The current study examined drug treatment-related reductions in alcohol and marijuana use, cigarette smoking, and non-drug offending among male adolescents who had been adjudicated of a serious (almost exclusively felony) offense. Results indicated that the “real world” drug treatments that these adolescents experienced had significant effects on substance use, which could not be explained solely by incarceration in controlled environments. However, effects on cigarette smoking and criminal offending were found only for treatments that included family involvement. Results suggest that involving families in adolescents’ treatment may be useful for promoting desistence from criminal offending in this population.
Keywords: substance use, juvenile offending, treatment
Introduction
Juvenile criminal offending is a significant social and public policy concern, with approximately 1 million adolescents in the United States formally processed within the justice system each year (National Mental Health Association, 2000; Snyder, 2002). Adolescent offenders show high rates of substance use as well as clinical substance use disorders, with estimated prevalences of disorder ranging from 25–67% across studies and justice system settings (Johnson et al., 2004; Teplin et al., 2002). Moreover, substance use has been shown to maintain offending behavior (Hussong et al., 2004; Wiesner et al., 2005; Young et al., 2007), with bi-directional relations between substance use and offending that form a “drug-crime cycle” (Vanderwaal et al, 2001).
Multiple mechanisms likely underlie these bi-directional relations between substance use and offending, including both shared risk factors and mutual influences. Substance use itself involves illegal behaviors (e.g., buying, and possessing illegal drugs), and these activities may also maintain adolescents’ membership in an antisocial peer network, within which social norms and opportunities support criminal offending. Substance use may also create a need for income that can be met through criminal activity. Moreover, the pharmacological effects of substance use may impair judgment and decision-making, and thus increase participation in illegal behavior. Finally, substance use may interfere with adolescents’ abilities to successfully occupy and fulfill adult roles (Yamaguchi & Kandel, 1985), which prevent them from ”maturing out” of criminal behavior (Chen & Kandel, 1995; Bachman et al., 1997).
Not surprisingly, then, substance abuse treatment is often seen as a potentially useful intervention to achieve reductions in both substance use and in criminal offending. A small but rapidly growing number of studies have shown that substance use treatment can produce statistically significant reductions in use among juvenile offenders (or in samples in which the majority but not all of the participants are juvenile offenders (e.g., Hser et al., 2001; Dennis et al., 2005; Randall & Cunningham, 2003). However, as noted by Morral, McCaffrey, and Ridgeway (2004), most studies of adolescent drug treatment examine ‘research’ therapies, which are theory-driven and delivered with high fidelity within tightly controlled research settings and designs. By contrast, Morral et al. (2004) note that the most common treatments that are actually received by adolescent offenders are not ‘research therapies,’ but rather ‘community therapies,’ which are delivered under non-standardized conditions by leaders who may not be highly trained (and perhaps themselves in recovery from drug abuse). Moreover, these differences in treatment implementation are likely to affect outcomes. Studies have suggested that the treatment effects seen in tightly controlled efficacy trials are greatly reduced when treatment is implemented in real-world settings (Curtis et al., 2004).
Little is known about the effects of the variety of drug treatments that are typically delivered to juvenile offenders in the ‘real world’ rather than in the context of a treatment outcome research study. Morral et al. (2004) found that one such program was effective in reducing substance use among juvenile offenders, but was not successful in reducing their criminal offending. The first goal of the current study was to examine the effects of substance abuse treatments that were received by a sample of serious juvenile offenders in the ‘real world’ rather than in the context of a treatment outcome study. We refer to these interventions as treatment “as usual,”1 and we test their effects on reducing substance use and criminal offending. A noteworthy contribution of the study is that is focuses on a sample of serious (almost exclusively felony) offenders, who are a rarely-studied but important subgroup from a policy perspective.
Moreover, within the adolescent drug treatment literature, different treatment approaches have shown some positive results (including cognitive behavior therapies, contingency management, multidimensional family therapy, multisystemic therapy, residential treatment and 12-step methods), but no one treatment modality has proved to be consistently superior (Dennis et al., 2005; Morral et al., 2006). Accordingly, rather than advocate for one particular treatment modality, several groups, including the National Institute on Drug Abuse (2006) and the American Academy of Child and Adolescent Psychiatry (Bukstein et al., 2005), have described a set of elements that are thought to define high quality treatment and thus constitute “best practices” or “quality elements” (Drug Strategies, 2005). For example, the NIDA (2006) principles of drug treatment for criminal justice populations note that treatment must last long enough to produce stable changes, and that those with severe drug problems or co-occurring disorders usually require treatment that lasts at least three months. Both the American Academy of Child and Adolescent Psychiatry standards and the Drug Strategies best practices note that substance abuse treatment for adolescents requires family involvement.
These best practices were generated through a consensus of expert professional judgment using available empirical evidence, and little is known about either their use or impact. Some research suggests that programs actually incorporate approximately half of the elements that are recommended, both in the general adolescent population (Brannigan et al., 2004) and within the juvenile justice system (Henderson et al., 2007). Thus, adolescents do not routinely receive treatment that includes all of these best practices. Importantly, there is only limited evidence about how these elements actually affect treatment outcomes for juvenile offenders. Accordingly, a second goal of the current study was to examine whether treatments that lasted at least 90 days (compared to shorter treatments) and treatments including family involvement (compared to treatments without family involvement) were associated with greater reductions in substance use and offending.
Furthermore, the literature on adolescent drug treatment has recently noted that cigarette smoking is often overlooked as a treatment outcome because of the (mistaken) belief that attempts at smoking cessation will undermine sobriety (Bobo et al., 1998). However, the serious negative health consequences of cigarette smoking are well-known, and adolescents’ decreased smoking after substance use treatment has actually been associated with decreases in other forms of substance use (Myers, Doran, & Brown, 2007). Because cigarette smoking is often overlooked as a treatment outcome, little is currently known about whether drug treatment influences cigarette smoking among adolescent offenders. Accordingly, a third goal of the current study was to examine treatment effects on cigarette smoking outcomes.
Finally, any effort to examine the relations among substance use, substance use treatment as usual, and criminal offending among adolescents in the justice system faces significant methodological challenges. First, adolescents in the justice system are not typically randomly assigned to interventions, and this limits the strength of any inferences that can be drawn about treatment effects. A recent, innovative approach to this problem was provided by McCaffrey, Ridgeway, and Morral (2004) in which they used propensity score estimation with boosted regression to address the selection issue. The current study adopted this approach, and used propensity score weighting in tests of treatment effects (see also Morral et al., 2004 for an empirical example). Second, adolescents in the justice system are differentially housed in controlled environments (such as prison, detention, or residential treatment) for varying periods of time, and their access to substances (and opportunities for criminal offending) vary as a function of their exposure to these restricted settings (Piquero et al., 2001). Most previous studies have simply ignored the effects of placement in controlled environments, which may overestimate treatment effects (McCaffrey et al., 2007). Although there is no perfect solution to this problem, the current analyses extended prior research by including the proportion of “supervised” time (“PST,” i.e., residence in a controlled environment) at each time point as a covariate in the models, as well as testing whether treatment effects varied as a function of time spent in controlled settings. Third, the current study examined effects on a range of outcomes including alcohol use, marijuana use, cigarette smoking, and non-drug criminal offending both in the short-term (six months after treatment) and the long-term (12 months after treatment).
In summary, more detailed information is needed about the effects of real world drug treatments with juvenile offenders. The current study examined the relation of such drug treatments to reductions in substance use and criminal offending among a sample of male serious juvenile offenders. In addition, the current study assessed the use and impact of two recommended elements of treatment. That is, we tested whether treatment duration of at least 90 days (compared to shorter treatments) as well as treatments including family involvement (compared to no family involvement) were associated with greater reductions in substance use and offending. We expanded the view of relevant outcomes by examining treatment effects on cigarette smoking. A noteworthy contribution of the study is that it focuses on a sample of male serious (almost exclusively felony) offenders, who are a rarely-studied but important subgroup from a policy perspective.
Methods
Participants
The present sample consisted of 429 male adolescent juvenile offenders from an ongoing longitudinal study of desistance from crime (Pathways to Desistance Project; Mulvey, Steinberg, Fagan, Cauffman, Piquero, Chassin, et al., 2004). This subsample was selected to include all of the males who reported some substance use at the beginning of the study and who either received no drug treatment at all (the untreated group) or received some treatment with a subsequent 12-month period of no treatment, in order to allow for the observation of a long-term outcome (see below for specific selection criteria).
The full sample (N=1354, 86% male, ages 14–17 at the time of the referring offense) were recruited in Phoenix (n = 654) and Philadelphia (n = 700) after a review of court files indicated that they had been adjudicated delinquent or found guilty of a serious offense (almost entirely felonies). Eligible crimes included felony offenses against persons and property, as well as several misdemeanor weapons offenses and sexual assault. Enrollment of males with a drug offense was capped at 15% in order to ensure a heterogeneous sample with respect to criminal offending. The range of committing offenses was 40.6% for violent crimes against persons (e.g., murder, rape, robbery, assault), 25.6 for property crimes (e.g., arson, burglary, receiving stolen property), 10.1% for weapons, 3.9% for sex crimes, 15.8% for drug-related crimes, and 4% for other crimes (e.g., conspiracy, intimidation of a witness). On average, court records indicated a lifetime history of about 2 prior petitions to court (not including probation violations).
Sample retention has been excellent. Two percent of participants dropped out of the study and two and a half percent have died. Of the remaining participants, retention ranged from 92–93% over the follow-up periods (90–91% of all living participants; 88%–89% of all those who enrolled at wave 1).
For the current analyses, a sub-sample was selected according to the following criteria: 1) male participants 2) at baseline, reported past 6 months use of alcohol, marijuana, or other illegal drugs 3) for the untreated group, reported receiving no substance use treatment over the entire 36 month study 4) for the treated group reported substance use treatment at either the 6-month, 12-month, 18-month, or 24-month interviews with a subsequent 12month period of no treatment and 4) having no missing data on the treatment variable across all 6 waves. This resulted in a sample of 429 participants. These 429 participants did not significantly differ from the total male sample in average age (16.1 in both cases), race (38% African American, 38% Hispanic, 20% Non-Hispanic Caucasian and 4% “Other” in the current subsample versus corresponding percentages of 42%, 34%, 19% and 5% in the total sample), prevalence of DSM-IV past year substance abuse or dependence at baseline (using the Composite International Diagnostic Interview, CIDI, World Health Organization, (WHO, 1997), 32% in the current subsample compared to 34% in the total sample) and self-reported criminal offending at baseline (using SRO variety scores, Huzinga, Esbensen, & Weihar, 1991).
Procedure
Research participants provided informed consent and all of the procedures for this study met the requirements of the Arizona State University Institutional Review Board and the Helsinki Declaration of 1975. Data were collected with computer-assisted interviews every 6 months at the participants’ homes, in libraries (or other public places), or in facilities. All measures and associated skip patterns were programmed onto laptop computers. Trained interviewers read each item aloud and, to maximize privacy, respondents could choose to enter their responses on a key pad (in some incarceration facilities, this option was not available). Honest reporting was encouraged and confidentiality was assured by confidentiality protections provided by statute to the Department of Justice. On average, interviews took about 2 hours to complete (with the exception of the baseline interview, which was completed on two consecutive days; approximately two hours each day) and participant payments ranged from $50 to $115 depending upon the interview period (see Schubert et al., 2004 for details).
Measures
Proportion of Supervised Time (PST)
At each interview, participants self-reported overnight stays in controlled environments including jails, prisons, detention centers, and residential treatment facilities, all of which limit access to alcohol, illegal drugs and, to some extent, opportunities for criminal offending (Piquero, Blumstein, Brame, Haapanen, Mulvey, & Nagin, 2001). The Proportion of Supervised Time (PST) variable was calculated by taking the total number of days that participants spent in controlled environments during the recall period and dividing it by the total number of days in the recall period, resulting in proportion scores ranging from 0 to 1. Across the 36 months of data used for this study, 21% of the sample were never in a supervised setting and the average time spent in a supervised setting was .32 (SD = .27), or 11.5 months. The proportion of supervised time at each six-month interval was used as a time-varying covariate in the analyses.
Alcohol, Marijuana, and Cigarette Use
At each interview, participants self-reported the frequency of their past-six month use of alcohol, marijuana use and cigarette smoking with items taken from previous research (Chassin, Rogosch & Barrera, 1991;Sher, 1987). Because of the non-normal distribution of the data, the responses were collapsed from eight categories into five: 0 (never), 1 (1 to 5x times), 2 (1–3x per month), 3 (1–3x per week), and 4 (4x per week or more). However, this still did not normalize the distribution for cigarette smoking. Accordingly, we transformed this outcome using the following expression .
Non-Drug Criminal Offending
At each interview, adolescents self-reported their engagement (over the past 6 months) in 22 criminal behaviors including both property crimes and aggressive offending (Huzinga, Esbensen, & Weihar, 1991). For the current outcome measure, we used the number of different offenses that were reported (i.e., a variety score), after eliminating three drug-related offenses (i.e., possession, use, and sales of illegal drugs) to avoid overlap with the substance use outcomes (leaving 19 SRO items). A non-drug offending score was created by calculating a percentage of the items endorsed. Adequate reliability and validity as well as some evidence of measurement equivalence across race and gender have been reported elsewhere on the complete instrument (see Knight, Little, Losoya, & Mulvey, 2004). On average, participants included in these analyses reported (at baseline) committing three different non-drug offenses in the past six months.
Substance Abuse Treatment
At each six-month interview, adolescents self-reported the drug and alcohol treatments they received over the past six months using a modified version of the Child and Adolescent Services Assessment (CASA; Ascher, Farmer, Burns & Angold 1996). For each form of treatment, we asked whether the treatment was specifically for drug or alcohol problems. Participants self-reported whether they had seen a mental health professional (e.g., a psychologist, therapist, or counselor), attended community support groups like AA or NA, been hospitalized or stayed in a drug or alcohol unit of a hospital (including detoxification), attended a day program in a hospital, or received court-ordered drug or alcohol treatment. Thirty four percent of the current sample (N=146) received treatment at 6, 12, 18, or 24 months. Duration of treatment was determined based on the length of time that a participant reported receiving treatment rather than by the intended or planned length of intervention, and was dichotomized, as 90 days or more (62% of those treated) versus less than 90 days (38%). Family involvement in treatment was dichotomized as any (27%) versus none (73%)
Four time-points were defined to assess treatment effects. The pretreatment score was the alcohol, marijuana use, cigarette smoking, or non-drug criminal offending reported at 6-months before treatment was received; the concurrent treatment score was the alcohol, marijuana use, cigarette smoking, or non-drug criminal offending reported at the same wave that treatment was received; the 6-month post treatment score was the alcohol, marijuana use, cigarette smoking or non-drug criminal offending reported 6-months after treatment was received (this time-point was used to assess the short-term treatment effect); and the 12-month post treatment score was the alcohol, marijuana use, cigarette smoking or non-drug criminal offending reported 12-months after treatment was received (this time-point was used to assess the long-term treatment effect). Each model used three-time points to estimate either the short-term treatment effect where the third time-point was the outcome measured 6 months post-treatment or the long-term treatment effect where the third time-point was the outcome measured 12 months post-treatment.
Untreated Group
The Untreated group (N=283 or 66% of the subsample) was composed of all participants who did not receive treatment over the 36 months. In order to synchronize the substance use scores of the treatment group with the untreated group, participants from the untreated group were allocated at random by selecting cases that match the time-period when participants received treatment.
Propensity Score Variables
Because adolescents in the justice system are not randomly assigned to drug and alcohol treatment, propensity score analyses were conducted to correct for pre-treatment differences using the baseline and first follow up values on a wide range of pre-treatment characteristics. The specific characteristics selected were modeled after those used in Morral et al. (2004) who used propensity scores for a similar purpose in modeling non-random assignment to substance abuse treatment in an adolescent sample. The 41 characteristics were: dummy coded variables for race (Caucasians, Hispanics, and African-Americans) school participation (having GED or attending school), alcohol and drug abuse or dependence diagnoses (from the CIDI), maximum number of drugs used (lifetime and past-six-months), frequency of drug use (lifetime and past-six-months), sum of ten possible alcohol or drug dependence symptoms (lifetime and past-six-months), sum of 17 possible alcohol or drug-related social consequences (lifetime and past-six months), number of recorded prior juvenile court appearances, self-reported offending (SRO subscales of Property Crimes, Violent Crimes, and Drug Crimes), PST during the initial six months of study, parental education (highest year), parent criminality (participant report of mother and father arrests, dichotomized and summed 0–2), parental heavy drinking (participant report of mother and father heavy drinking dichotomized and summed, 0–2), peer drug advocacy (sum of three items: How many of your friends sold drugs?”, “How many friends claim you need to be high on drugs to have a good time?”, and “How many of your friends suggested that you should sell drugs?”, from Thornberry et al., 1994), peer criminality and mental health (proportion of 4 closest friends arrested or jailed), gang involvement during the initial six months of study, Major Depression and Post-traumatic Stress Syndrome diagnoses from the CIDI (WHO, 1997), current overall psychological functioning (Global Severity Index (GSI) of the Brief Symptom Inventory (BSI), Derogatis & Melisaratos, 1983; and impulse control, Weinberger & Schwartz, 1990). 2
Results
Propensity Score Model
Propensity scores were calculated using the GBM algorithm (Ridgeway, 2004). The probabilities (p) were used as weights (w) in these models and defined as Tx + (1−Tx) × w, where Tx is a indicator variable for treatment (1 = Treated, 0 =Untreated), and w=1/(1−p) is the odds ratio of a participant who received treatment (Hirano, Imbens & Ridder, 2003). The weights (the inverse of the nonparametric propensity score) were applied to substance use scores and non-drug offending scores for participants in the group that did not receive drug treatment. This serves to reduce the differences between the treated and untreated groups on the variables that are potentially confounded with receiving treatment (Morral et al., 2004). We repeated the same procedures and created sets of propensity scores for comparing: a) treatment versus no treatment; b) treatment for more than 90 days versus no treatment; c) treatment for less than 90 days versus no treatment; d) treatment for more than 90 days versus for less than 90 days; e) treatment with family involvement versus no treatment; f) treatment without family involvement versus no treatment; and g) treatment with family involvement versus treatment without family involvement. In each case, we first tested the adequacy of the propensity score model in reducing differences between the two groups by comparing them on the 41 potentially confounding variables (that were described earlier in the methods section) both before and after weighting the untreated group scores.
For the overall comparison (treatment versus no treatment), the mean effect size (Cohen’s d) for the group differences before weighting was .26 (range .05 to .50), and the treated and untreated groups significantly differed on 29 of the 41 (70.7%) potentially confounding variables (t-tests, all, ps < .05). After weighting, the mean effect size dropped to .06 (range .01 to .17), and there were no significant between-group differences.
Comparing treatment that lasted 90 days or more to the untreated group, before weighting, the mean effect size for the group differences was 0.22 (range .01 to .71), and the groups significantly differed on 23 of the 41 (56.1%) variables (t-tests, all ps <.05). After weighting, the mean effect size was reduced to .11 (range .01 to .23), and there was only one significant group difference (fewer than expected by chance). For treatment of less than 90 days compared to the untreated group, before weighting the mean effect size for the group differences was .29 (range.05 to .63), and the groups differed on 26 (64.4%) of the variables. After weighting, the mean effect size was reduced to .12 (range.01 to .25), and there were no significant between group differences. For longer compared to shorter treatment, before weighting, the mean effect size for the group differences was .22 (range .01 to .84), and the groups differed on 10 (24.3%) of the variables. After weighting, the mean effect size was reduced to .14 (range .01 to .72), and the groups differed on 2 variables (the number that would be expected by chance).
Comparing treatment with family involvement to the untreated group, before weighting, the mean effect size for the group differences was 0.29 (range .01 to .84), and the groups significantly differed on 19 (46.3%) of the variables (t-tests, all ps <.05). After weighting, the mean effect size was reduced to .13 (range .01 to .45), and there was only one significant difference (below what would be expected by chance). Comparing treatment without family involvement to the untreated group, before weighting, the mean effect size for the group differences was .24 (range .01 to .44), and the groups differed on 24 (58.5%) of the variables. After weighting, the mean effect size was reduced to .08 (range .01 to .21), and there was only one significant difference (below what would be expected by chance). Finally, comparing treatment with and without family involvement, before weighting, the mean effect size for the group differences was .19(range .01 to .68), and the groups significantly differed on two of the predictor variables. After weighting, the mean effect size was reduced to .10 (range .01 to .26), and there were no significant differences. Thus, in each case, our propensity score models were successful in eliminating the number of significant between-group differences either completely, or to chance levels or below.
Testing the Effects of Treatment
Treatment effects were tested in a series of Hierarchical Linear Modeling analyses using Proc Mixed implemented in SAS Version 9 (SAS Institute Inc, 1999) to examine rates of within-person change in adolescents’ frequency of alcohol use, marijuana use, and cigarette smoking, as well as non-drug criminal offending. Using multilevel analyses that included the propensity-score derived weights described earlier, variability in substance use and offending were represented in a Level-1 model that accounted for within-person variability and included initial status, growth, and the time-varying effect of PST (i.e., proportion of supervised time at that six-month interval). The Level-2 model represented the sources of between-person differences over time that were associated with treatment. We also tested (in separate models because of sample size constraints) for variation in treatment effects as a function of treatment duration and family involvement. When Level-1 and Level-2 models are combined the interactive effects of PST on treatment and time-related change in substance use are estimated; thus, substance use and offending scores were adjusted by PST.
An important feature was the inclusion of deflection terms in the Level-1 models (as suggested by Raudenbush, 2001). As noted earlier, we used reports of the outcomes at three time points for examining the short-term treatment effects use (6-months prior to treatment, at the time of treatment, and 6- months post-treatment), and for the long-term treatment effects use (6-months prior to treatment, at the time of treatment, and 12- months post-treatment). For the treatment group, the deflection terms represent the change in the slope of the substance use/offending scores before and after receiving treatment. For the untreated group, the deflection term represents the natural change in the substance use/offending scores over the same time period.
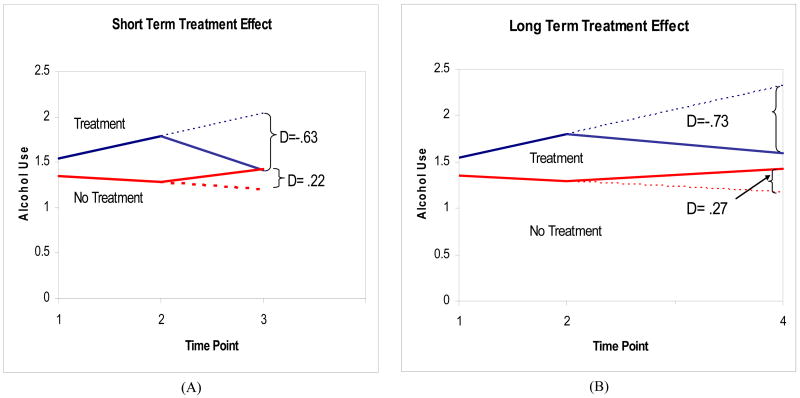
These deflection terms allowed us to test the effects of treatment in two ways. First, among those who received treatment, we compared their predicted scores based on their pre-treatment slope to their observed post-treatment scores, and tested whether this difference significantly differed from zero. That is, a beneficial effect of treatment should produce an observed post-treatment score that was significantly lower than the score that was predicted on the basis of the pretreatment slope. An example is provided in Figure 1a. The negative deflection (i.e., −.63) for those who received treatment indicates that there is a difference of −.63 between the observed and expected post-treatment alcohol use scores in the treated group. Moreover, this deflection was significantly different from zero. Table 1 presents each deflection score for both the treated and untreated groups, and the asterisks associated with these scores indicate whether they significantly differed from zero.
Figure 1.
Example model testing treatment effects on alcohol use. The letter D indicates the deflection, which is the difference between the predicted and observed score. The solid line indicates the actual observed scores and the dotted lines indicate the predicted scores at PST=0. The deflections are identical across levels of PST because there were no significant PST by treatment interactions. Time points are: 1= pre treatment, 2= concurrent, 3=6-months after treatment, and 4=12-months after treatment.
Table 1.
Short-Term and Long-Term Deflections in Alcohol Use, Marijuana Use, Cigarette Use, and Offending Among Adolescents Receiving and Not Receiving Substance Use Treatment
| Treatment Comparison | Alcohol Use |
Marijuana Use |
Cigarette Useb |
Non-drug Offending |
||||
|---|---|---|---|---|---|---|---|---|
| Overall: | Short |
Long |
Short |
Long |
Short |
Long |
Short |
Long |
| Treatment (n=146) | −.63 ** | −.73 * | −.19 | .37 | −.20 | −.36 + | −.02 | .01 |
| No Treatment (n=283) | .22 | .27 | .36 | .33 | −.12 | −.11 | .00 | .00 |
| t-valuea | −3.11 ** | −2.27 * | −1.65 | −.07 | −.50 | −.90 | −.76 | .20 |
|
|
||||||||
| Duration: | ||||||||
| ≥90 Days (n=91) | −.80 ** | −1.47 ** | −.86 * | −.97 + | .19 | −.10 | −.07 * | −.08 + |
| No Treatment (n=283) | .11 | .13 | .29 | .34 | −.17 | −.15 | −.01 | −.02 |
| t-valuea | −2.55 * | −2.78 * | −2.58 * | −1.80 + | 1.58 | .14 | −1.52 | −1.05 |
|
|
||||||||
| <90 Days (n=55) | −.58 ** | −.63 * | −.07 | .72 | −.24* | −.32 * | −.02 | .02 |
| No Treatment (n=283) | .17 | .28 | .41 | .45 | −.03 | −.02 | −.01 | .00 |
| t- valuea | −3.05 ** | −2.30 * | −1.67 | .61 | −1.42 | −1.22 | −.47 | .40 |
|
|
||||||||
| ≥90 Days (n=91) | −.83 + | −1.33 + | −.91 + | −1.05 | .17 | −.04 | −.07 | −.09 |
| <90 days (n=55) | −.65 | −1.11 | .19 | .33 | −.43 | −.52 | −.01 | .00 |
| t- valuea | −.24 | −.20 | −1.28 | −1.05 | 1.36 | .68 | −.68 | −.79 |
|
|
||||||||
| Family Involvement: | Short |
Long |
Short |
Long |
Short |
Long |
Short |
Long |
| Family Involved (n=40) | −.92 ** | −1.44 ** | −.51 + | −.32 | −.67** | −1.54 ** | −.14 ** | −.14 ** |
| No Treatment (n=283) | .20 | .19 | −.03 | −.15 | .10 | .12 | −.01 | −.03 |
| t- valuea | −3.13 ** | −3.03 ** | −1.14 | −.26 | −3.80** | −4.96 *** | −3.97 *** | −2.09 * |
|
|
||||||||
| Family Not Involved (n=106) | −.59 ** | −.64 * | −.13 | .53 | −.15 | −.26 | .00 | .04 |
| No Treatment (n=283) | .17 | .31 | .39 | .42 | −.13 | −.14 | .00 | .00 |
| t- valuea | −2.84 ** | −2.16 * | −1.58 | .21 | −.11 | −.44 | .01 | .75 |
|
|
||||||||
| Family Involved (n=40) | −.95 * | −1.43 * | −.61 | −.51 | −.68 ** | −1.45 ** | −.14 ** | −.14 * |
| Family Not Involved (n=106) | −.22 | .19 | −.12 | .81 | .04 | .10 | .02 | .06 |
| t- valuea | −1.06 | −1.54 | −.64 | −1.10 | −1.86+ | −2.39 * | −2.36 * | −1.81 + |
p<.10.
p<.05.
p <.01.
Note: Negative deflections indicate reductions in substance use and offending. Asterisks indicate that the deflections are significantly different than zero.
Asterisks associated with the t-value indicate that the deflections from the two comparison groups significantly differ from each other. All t-test comparisons were based upon the error term from the overall analysis.
Cigarette use was transformed using the following expression: .
Another method of evaluating treatment effects is to compare the deflections in the treated group with the deflections in the untreated group (see Figure 1). If treatment has a beneficial effect, there should be larger negative deflections in the treated group than in the untreated group. For example, in Figure 1A, this represents a comparison of the −.63 difference between the observed and expected alcohol use in the treated group compared to the +.22 difference between the observed and expected alcohol use in the untreated group. In this example, the alcohol use of those who received treatment was .63 scale points lower than their expected use based on their pre-treatment slope, whereas the alcohol use of those who did not receive treatment was .22 scale points higher than their expected use (the same values for the long-term effect are in Figure 1B). Differences between the deflection scores for the treated and untreated groups were evaluated with t-tests. Table 1 presents the t-values and the significance levels for each comparison.3,4
Across the different models, there were significant main effects of PST, such that in all models, higher PST was significantly associated with less alcohol use and less marijuana use, and this was also true for cigarette smoking in all but one model. PST was significantly related to non-drug offending in only one model. Importantly, however, none of the models showed significant PST by treatment interactions for any outcome. Accordingly, we do not present findings involving PST (although the effects of PST are controlled in all reported models).
Overall Effects of Treatment v., No Treatment
Table 1 presents deflection scores for the treated and the untreated groups, as well as the t-values that test the significance of the difference between the two deflections. There was a significant effect of treatment in reducing observed alcohol use from its predicted level in both the short and the long-term, and a marginally significant reduction from predicted levels of cigarette smoking in the short-term. These deflections were significantly different from the untreated group for alcohol use in the short-term and the long-term, but not for any other outcome. Treatment was associated with lowering of alcohol use from its predicted level by .63 of a scale point (in the short term) to .73 of a scale point (in the long term) on a five- point scale of drinking frequency.
Effects of Treatment Duration
Treatment of 90 Days or More vs. No Treatment
As shown in Table 1, treatment that lasted longer than 90 days was associated with significant short-term and long-term reductions in observed alcohol use compared to predicted levels, as well as significant reductions from predicted levels of marijuana use in the short-term (and marginally in the long term), and marginally significant long-term reductions from predicted levels of non-drug offending. These deflection scores for the long-duration treatment group significantly differed from those of the untreated group for alcohol use (in both the short-term and long-term) and marijuana use (significant in the short-term and marginally significant in the long-term). However, there were no significant differences between the long-duration treatment group and untreated group deflections for cigarette smoking or self-reported offending. Reductions in alcohol and marijuana use from predicted levels ranged from .80 to 1.47 scale points on a 5-point scale of frequency.
Treatment of Less Than 90 Days vs. No Treatment
Table 1 shows that treatment that lasted less than 90 days was associated with significant short-term and long-term deflections in alcohol use and significant short-term and long-term deflections in cigarette smoking. However, the treated and untreated groups significantly differed in their deflections only for alcohol use (both short-term and long-term). . Reductions from predicted drinking were approximately .60 of a scale point on a 5-point scale of drinking frequency.
Treatment of 90 days or more vs. treatment of less than 90 days
Table 1 shows that longer treatment was associated with marginal negative deflections in alcohol use, but the deflections for the longer-duration treatment and shorter-duration treatment groups did not significantly differ for any outcome.
Effects of Family Involvement in Treatment
Treatment with Family Involvement vs. No Treatment
As shown in Table 1, treatment that included family involvement was associated with significant or marginally significant reductions in observed versus predicted scores for all outcomes except for long-term marijuana use. Moreover, the family involvement and untreated groups significantly differed in their deflections for all outcomes except marijuana use (short-term and long-term). The average reductions from predicted alcohol and cigarette use ranged from .67 to 1.44 scale points on a five point scale.
Treatment without Family Involvement vs. No Treatment
As shown in Table 1, treatment without family involvement was associated with a significant negative deflection in alcohol use (both in the short-term and the long-term) and the alcohol use deflections for the non-family treated and untreated groups significantly differed. However, there were no significant effects on outcomes other than alcohol use. Treatment without family involvement was associated with reductions in alcohol use of approximately .6 of a scale point on a five-point scale (both short-term and long-term).
Treatment with Family Involvement vs. Treatment without Family Involvement
Table 1 shows that treatment with family involvement was associated with significant reductions in observed compared to predicted use of alcohol and in cigarettes, and in observed compared to predicted non-drug offending (both short-term and long-term). However, the deflection scores for those treated with and without family involvement significantly differed from each other only in cigarette smoking and non-drug offending.
Discussion
Because adolescent offenders have high rates of substance use disorders (Johnson et al., 2004) and because substance use has been shown to delay desistance from offending (Hussong et al., 2004) treatment for substance use disorders has been considered as one method for promoting desistance among juvenile offenders. However, despite a rapidly growing literature, there is still much to be learned about the impact of drug treatment for this population. In particular, little is known about the effects of the usual treatments received in the real world as opposed to those that are administered under more tightly controlled conditions as part of a research trial; little is known about the use and impact of recommended best practices in substance use treatment, little is known about the effects of substance use treatment on cigarette smoking, and little is known about treatment effects for serious juvenile offenders. The current study provides some information about these questions.
The first finding of note was that these real world substance use treatments had significant effects. Among our sample of male serious juvenile offenders, those who reported receiving some substance use treatment had levels of post-treatment substance use frequency that were reduced from the levels that were predicted by their pre-treatment trajectories. Moreover, their levels of use were reduced to a greater extent than the natural over-time changes that were observed among those who received no treatment. This result is encouraging because it was seen in both short-term (six month) and long-term (12-month) outcomes and was obtained above and beyond a consideration of the percentage of time that the adolescents spent being housed in a controlled residential environment (in which substance use opportunities are likely to be curtailed). Thus, these results can not be entirely explained by incapacitation effects. Although we do not have detailed information about the content, quality, or implementation of these real world treatments, the current findings suggest that, as a group, the various interventions that are being delivered to serious juvenile offenders have some detectable positive effects.
Importantly, however, the pattern of effects was also qualified in that effects varied depending on the duration of treatment, the involvement of families, and the particular outcome that was measured. One recommendation (by NIDA, 2006) is that treatment must last for a “sufficient” duration such that those with serious substance use problems may require a period of at least three months of treatment. Almost two-third of our treated cases received treatment that lasted this long, which is encouraging in terms of the incorporation of this recommendation into naturally occurring interventions. Because we measured only the length of the time that the adolescents received treatment, we cannot know the actual intended length of the interventions. However, our data showed that treatment that lasted three months or more constituted the only circumstance in which marijuana use was significantly reduced. Perhaps relative to the use of alcohol and cigarettes, the use of illegal drugs is a marker for the increased severity that requires longer treatment duration.
However, the only circumstance in which cigarette smoking and criminal offending behaviors were significantly reduced was when treatments included family involvement. Moreover, only approximately one quarter of our participants received treatments that included family involvement. This is lower than recent data from a national survey of program directors in the juvenile justice system, in which the majority of program directors (particularly for community-based programs) reported incorporating family involvement in their interventions (Henderson et al., 2007). However, those findings were self-reports from a limited sample of program directors who responded to the survey. The low rates of treatment including family involvement in our sample may more accurately reflect the types of services that are actually received by serious juvenile offenders, especially given that most of these services are received in more secure institutional settings than in community settings (see Mulvey, Schubert, & Chung, 2007).
Cigarette smoking is a target of intervention that is often overlooked in adolescent substance use treatment, despite the importance of its associated mortality and morbidity. Moreover, rather than undermining sobriety, is has been demonstrated that reductions in cigarette smoking after substance use treatment are actually correlated with lower levels of post-treatment adolescent alcohol use (Myers et al., 2007). The findings that only treatments including family involvement reduced cigarette smoking might reflect the fact that adolescents are more likely to smoke cigarettes in the presence of their family members than they are to use other substances in the presence of their family members, providing a relatively greater opportunity for family influence on cigarette smoking.
Criminal offending, of course, is the outcome of most direct interest in terms of justice system policy implications, and only interventions with family involvement produced statistically significant reductions in non-drug offending (compared to treatments without family involvement). Our findings are consistent with those that have supported the use of family therapy (multidimensional family therapy, multisystemic therapy, functional family therapy) in reducing antisocial behavior among adolescents (Liddle, 2004; Woolfendon et al., 2002). Moreover, some evidence of effect was still detectable one-year after the termination of treatment. Thus, even though alcohol use was reduced in treatments without family involvement, broader impact on important outcomes (cigarette smoking and non-drug offending) was only obtained with family involvement. Given the rather low prevalence of family involvement in treatment in our sample (approximately one quarter of the treated cases), justice system policies that help to engage families might be useful in promoting desistance from criminal offending.
Although our findings support the utility of drug treatment for serious juvenile offenders, the magnitude of these effects is also consistent with the broader literature in suggesting statistically significant but relatively modestly-sized effects. In our data, reductions were in the range of two-thirds to one and a half scale points on a five-point scale. Although it is encouraging that these reductions were observed in a sample of serious offenders and above and beyond the consideration of “supervised time,” the magnitude of these effects also points to the need for innovative strategies to increase the impact of these interventions. Moreover, continuing post-treatment aftercare interventions are likely to be needed to build on initial gains.
Although the current study is important in studying real world treatments as usual, in studying the effects of treatment duration and family involvement, in studying a sample of serious juvenile offenders, and in considering the effects of treatment on multiple outcomes, there are also limitations that suggest caution about conclusions as well as future research directions. First, studying treatment as usual means that findings were produced by a heterogeneous mix of interventions, precluding recommendations concerning a single specific treatment modality, and we lack information on the quality of the treatments that were provided. However, our findings concerning treatment duration and family involvement have clear implications for practice. Second, our findings are based on self-report data. Because our inferences are based on change over multiple time points and because interviews were not conducted in the context of a treatment outcome study, there is lowered likelihood that social desirability biases would systematically influence the estimates of treatment-related changes in substance use over time. Nevertheless, official arrest records are being added to our data base, and future analyses of official arrest data will be an important addition to our outcomes. Third, although our use of propensity score adjustment reduces the biases associated with non-random assignment to treatment (and our propensity score adjustments eliminated any between-group differences to chance levels), we lack the strongest level of inference that would be provided by random assignment to treatment. Thus, our findings can supplement but cannot replace the more precise knowledge that is gained through randomized clinical trials. Fourth, our sample size is relatively small (particularly for those who received family treatment) and did not contain adequate numbers to study female offenders. This suggests both a need for replication and also that the study of female offenders is an important future direction. Finally, because we wished to examine relatively long-term (one-year) outcomes, we studied adolescents who had experienced a one-year post-treatment interval in which they reported receiving no drug treatment interventions. This means that we could not examine the effects of any aftercare interventions. Because substance use disorders are chronic relapsing and remitting disorders, the provision of post-treatment aftercare is an important component of intervention. Larger effects on outcomes might have been produced if aftercare interventions had been examined (cf., Chung, Schubert, & Mulvey, 2007).
In summary, the current study examined the effects of real world drug treatments as usual on a sample of serious juvenile offenders. Results showed that treatment significantly reduced substance use levels compared to adolescents’ predicted trajectories and did so to a greater extent than the naturally occurring changes over time among adolescent offenders who did not receive treatment. Moreover, these findings were produced above and beyond a consideration of time spent in controlled residential environments, and thus cannot be entirely explained by incapacitation effects. However, the pattern of findings varied with treatment duration and the presence of family involvement, as well as with the outcome that was studied. Only treatments that lasted for at least 90 days were successful in reducing marijuana use and only treatments that incorporated family involvement were successful in reducing cigarette smoking and non-drug criminal offending. The fact that only one quarter of our participants reported receiving treatments that incorporated family involvement suggests that this recommended element is not being incorporated into interventions with serious offenders and that policy initiatives to encourage family involvement within juvenile justice interventions may yield positive outcomes. Strategies to promote family involvement, increase the magnitude of treatment effects, and incorporate aftercare interventions to build on initial success are all important future research directions.
Acknowledgments
The project described was supported by funds from the following: Office of Juvenile Justice and Delinquency Prevention, National Institute of Justice, John D. and Catherine T. MacArthur Foundation, William T. Grant Foundation, Robert Wood Johnson Foundation, William Penn Foundation, Center for Disease Control, National Institute on Drug Abuse (R01DA019697), Pennsylvania Commission on Crime and Delinquency, and the Arizona Governor’s Justice Commission. We are grateful for their support. The content of this paper, however, is solely the responsibility of the authors and does not necessarily represent the official views of these agencies.
Several colleagues provided valuable advice on this manuscript. We thank Dr. Antonio Morgan-Lopez, Dr. Robert Brame, and Dr. Alex Piquero for their comments on our quantitative methods, Dr. Andrew Morral for discussion of our propensity score methods, and Dr. Ed Mulvey for comments on earlier drafts.
Footnotes
We refer to these interventions as “treatments as usual” rather than using Morral et al.’s (2004) term “community therapies.” The term “community therapy” might be misleading when applied to a sample of serious juvenile offenders who largely receive treatments in residential correctional settings that are not embedded in the community (Mulvey, Schubert, & Chung, 2007). Our use of the term “treatments as usual” is meant to refer to the interventions that were received by our sample of serious juvenile offenders in the “real world” rather than in the context of a treatment outcome research study
Details regarding these propensity score variables are available upon request.
| (1) |
| (2) |
This model includes the pretreatment growth rates for the treated and untreated groups (i.e., β11), and the interaction of the pre-treatment growth with PST (i.e., β31). Testing treatment effects relies on the parameters associated with the deflection (i.e., Δ10, or Δ11), and the deflection interacting with PST (i.e., Δ20 or Δ21). To test whether the deflections in the treated group and the untreated group were significantly different from zero, we used (Δ10 + Δ11)/SE(Δ10+ Δ11) with a standard error defined as . To test whether the deflections in the treatment group were significantly different from the deflections in the untreated group, we examined the t-test for the Δ11 parameter estimate.
For brevity, the rest of the parameters (e.g., β11 or β31) in the model are not reported in the text, but they were estimated to calculate the linear trend from the pretreatment to the post treatment period as well as the deflection after treatment
Initial models included the effects of baseline substance use disorder diagnosis and its interaction with treatment. However, because there were no significant treatment by diagnosis interactions, the effects of diagnosis were not considered further. The absence of these interactions with diagnosis may be because we measured diagnosis only at baseline, whereas treatment was provided at any time in the next twenty-four months. That is, although treatment could have different effects on adolescents who do and do not meet formal diagnostic criteria for substance use disorder, the effects of diagnosis might not be detectable unless diagnosis is measured at the time of treatment provision. Consistent with this interpretation, for the treated group, substance use generally increased from baseline to the time of treatment provision. This suggests that some of these treated adolescents might have crossed the threshold for diagnosis some time after the baseline assessment.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arbuckle J. Full information estimation in the presence of incomplete data. In: Marcoulides G, Schumacker R, editors. Advanced structural equation modeling: Issues and techniques. Mahwah, NJ: Erlbaum; 1996. pp. 243–277. [Google Scholar]
- Ascher BH, Farmer EMZ, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): Description and psychometrics. Journal of Emotional and Behavioral Disorders. 1996;4:12–20. [Google Scholar]
- Bachman JG, O’Malley PM, Schulenberg JE, Johnston LD, Bryant A, Merline A. The Decline of Substance Use in Young Adulthood: Changes in Social Activities, Roles, and Beliefs. Mahwah, NJ: Erlbaum; 1997. [Google Scholar]
- Bobo J, McIlvain H, Lando H, Walker R, Leed-Kelly A. Effect of Smoking Cessation Counseling on Recovery from Alcoholism: Findings from a Randomized Community Intervention Trial, Addiction. 1998;93:877–887. doi: 10.1046/j.1360-0443.1998.9368779.x. [DOI] [PubMed] [Google Scholar]
- Brannigan R, Schackman B, Falco M, Millman R. The quality of highly regarded adolescent substance abuse treatment programs: Results of an in-depth national survey. Archives of Pediatric and Adolescent Medicine. 2004;158:904–909. doi: 10.1001/archpedi.158.9.904. [DOI] [PubMed] [Google Scholar]
- Bukstein O, Bernet W, Arnold V, Breitchman J, Shaw J, Benson S, Kinlan J, McClellan J, Stock S, Ptakowski K the Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:609–621. doi: 10.1097/01.chi.0000159135.33706.37. [DOI] [PubMed] [Google Scholar]
- Chassin L, Rogosch F, Barrera M. Substance use and symptomatology among adolescent children of alcoholics. Journal of Abnormal Psychology. 1991;100:449–463. doi: 10.1037//0021-843x.100.4.449. [DOI] [PubMed] [Google Scholar]
- Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. American Journal of Public Health. 1995;85:41–47. doi: 10.2105/ajph.85.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Chung HL, Schubert CA, Mulvey EP. An empirical portrait of community reentry among serious juvenile offenders in two metropolitan cities. Criminal Justice and Behavior. 2007;34:1402–1426. doi: 10.1177/0093854807307170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis N, Ronan K, Borduin C. Multisystemic treatment: A meta-analysis of outcome studies. Journal of Family Psychology. 2004;18:411–419. doi: 10.1037/0893-3200.18.3.411. [DOI] [PubMed] [Google Scholar]
- Dempster AP, Laird NM, Rubin DB. Maximum likelihood estimation for incomplete data via the EM algorithm (with discussion) Journal of the Royal Statistical Society, Series B. 1977;39:1–38. [Google Scholar]
- Dennis M, Godley S, Diamond G, Tims F, Babor T, Donaldson J, Liddle H, Titus J, Kaminger Y, Webb C, Hamilton N, Funk R. The Cannabis Youth Treatment Study: Main Findings from Two Randomized Trials. Journal of Substance Use Treatment. 2005;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Derogatis L, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Drug Strategies. Bridging the Gap: A Guide to Drug Treatment in the Juvenile Justice System. Drug Strategies; Washington, DC: 2005. [Google Scholar]
- Henderson C, Young D, Jainchill N, Hawke J, Farkas S, Davis R. Program use of effective drug treatment practices for juvenile offenders. Journal of Substance Abuse Treatment. 2007;32:272–290. doi: 10.1016/j.jsat.2006.12.021. [DOI] [PubMed] [Google Scholar]
- Hirano K, Imbens G, Ridder G. Efficient estimation of average treatment effects using the estimated propensity scores, Econometrica. 2003;71(4):1161–1189. [Google Scholar]
- Hser YI, Grella C, Hubbard R, Hsieh S, Fletcher B, Brown B, Anglin D. An evaluation of drug treatments for adolescents in four US cities. Archives of General Psychiatry. 2001;58:689–695. doi: 10.1001/archpsyc.58.7.689. [DOI] [PubMed] [Google Scholar]
- Huizinga D, Esbensen F, Weiher A. Are there multiple pathways to delinquency? Denver youth survey. Journal of Criminal Law and Criminology. 1991;82:83–118. [Google Scholar]
- Knight GP, Little M, Losoya SH, Mulvey EP. The self-report of offending among serious juvenile offenders: Cross-gender, cross-ethnic/race measurement equivalence. Youth Violence and Juvenile Justice. 2004;2(3):273–295. doi: 10.1177/1541204004265878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Curran PJ, Moffitt TE, Caspi A, Carrig MM. Substance abuse hinders desistance in young adults’ antisocial behavior. Development and Psychopathology. 2004;16:1029–1046. doi: 10.1017/s095457940404012x. [DOI] [PubMed] [Google Scholar]
- Johnson TP, Cho YI, Fendrich M, Graf I, Kelly-Wilson K, Pickup L. Treatment need and utilization among youth entering the juvenile corrections system. Journal of Substance Abuse Treatment. 2004;26:117–128. doi: 10.1016/S0740-5472(03)00164-8. [DOI] [PubMed] [Google Scholar]
- Liddle H. Family-based therapies for adolescent alcohol and drug use: Research contributions and future research needs. Addiction. 2004;99:76–92. doi: 10.1111/j.1360-0443.2004.00856.x. [DOI] [PubMed] [Google Scholar]
- McCaffrey DF, Ridgeway G, Morral AR. Propensity score estimation with boosted regression for estimating causal effects in observational studies. Psychological Methods. 2004;9:403–425. doi: 10.1037/1082-989X.9.4.403. [DOI] [PubMed] [Google Scholar]
- McCaffrey D, Morral A, Ridgeway G, Griffin B. Interpreting treatment effects when cases are institutionalized after treatment. Drug and Alcohol Dependence. 2007;89:126–138. doi: 10.1016/j.drugalcdep.2006.12.032. [DOI] [PubMed] [Google Scholar]
- Morral AR, McCaffrey DF, Ridgeway G. Effectiveness of community-based treatment for substance-abusing adolescents: 12-month outcomes of youths entering Phoenix Academy or alternative probation dispositions. Psychology of Addictive Behaviors. 2004;18:257–268. doi: 10.1037/0893-164X.18.3.257. [DOI] [PubMed] [Google Scholar]
- Morral A, McCaffrey D, Ridgeway G, Mikherji A, Beighley C. The relative effectiveness of 10 adolescent substance abuse treatment programs in the United States. Technical Report. Rand Drug Policy Research Center; Santa Monica, CA: 2006. [Google Scholar]
- Mulvey EP, Steinberg L, Fagan J, Cauffman E, Schubert C, Piquero A, Losoya S, Chassin L, Knight G, Brame R. Theory and research on desistance from antisocial activity among adolescent serious offenders. Youth Violence and Juvenile Justice. 2004:1–24. doi: 10.1177/1541204004265864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvey EP, Schubert CA, Chung HL. Service use after court involvement in a sample of serious adolescent offenders. Children and Youth Services Review. 2007;29:518–544. doi: 10.1016/j.childyouth.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus: Statistical analysis with latent variables user’s guide Version 3. Los Angeles, CA: Muthen & Muthen; 2004. [Google Scholar]
- Myers M, Doran N, Brown S. Is Cigarette Smoking Related to Alcohol Use During the 8 Years Following Treatment for Adolescent Alcohol and Other Drug Abuse? Alcohol and Alcoholism. 2007;42:226–233. doi: 10.1093/alcalc/agm025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Principles of Drug Abuse Treatment for Criminal Justice Populations: A Research-Based Guide. US Government Printing Office; 2006. NIH Publication NO. 06–5316. [Google Scholar]
- National Mental Health Association. Justice for juveniles: How communities respond to mental health and substance abuse needs of youth in the juvenile justice system (Executive Summary) [Accessed February 17, 2005];2000 Available at: http://www.nmha.org/children/justjiv/execsum.cfm.
- Piquero A, Blumstein A, Brame R, Haapanen R, Mulvey E, Nagin DS. Assessing the impact of exposure time and incapacitation on longitudinal trajectories of criminal offending. Journal of Adolescent Research. 2001;16:54–74. [Google Scholar]
- Piquero A, Farrington D, Blumstein A. The criminal career paradigm. In: Tonrey M, editor. Crime and Justice: A Review of Research. Vol. 30. Chicago: University of Chicago Press; 2003. pp. 359–506. [Google Scholar]
- Randall J, Cunningham P. Multisystemic therapy: A treatment for violent substance-abusing and substance-dependent juvenile offenders. Addictive Behaviors. 2003;28:1731–1739. doi: 10.1016/j.addbeh.2003.08.045. [DOI] [PubMed] [Google Scholar]
- Ridgeway G. Boosted logistic regression. Technical Report Rand Corporation Statistics Group; Santa Barbara CA: 2004. [Google Scholar]
- Schubert CA, Mulvey EP, Steinberg L, Cauffman E, Losoya S, Hecker T, Chassin L, Knight G. Operational lessons from the Pathways to Desistance project. Youth Violence and Juvenile Justice Journal. 2004;2:237–255. doi: 10.1177/1541204004265875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder H. Juvenile Arrests 2000. Washington, DC: Office of Juvenile Justice and Delinquency Prevention; 2002. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Adolescent treatment admissions by gender: 2005. Drug and Alcohol Services Information System Report, Office of Applied Studies. 2007 www.oas.samhsa.gov.
- Teplin L, Abram K, McClelland G, Dulcan M, Mericle A. Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2002;59:1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry T, Krohn M. Taking stock of delinquency: An overview of findings from contemporary longitudinal studies. New York: Kluewer; 2003. [Google Scholar]
- Thornberry T, Lizotte A, Krohn M, Farnworth M, Jang S. Delinquent peers, beliefs, and delinquent behavior: A longitudinal test of interactional theory. Criminology. 1994;32:47–83. [Google Scholar]
- Vanderwaal C, McBride D, Terry-McElrath Y, Van Buren H. Breaking the juvenile drug-crime cycle: A guide for practitioners and policy makers. US Department of Justice, Office of Justice Programs, National Institute of Justice. 2001 http://www.ojp.usdoj.gov/nij.
- Wiesner M, Kim HK, Capaldi DM. Developmental trajectories of offending: Validation and prediction to young adult alcohol use, drug use, and depressive symptoms. Development and Psychopathology. 2005;17:251–270. doi: 10.1017/s0954579405050133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolfenden S, Williams K, Peat J. Family and parenting interventions for conduct disorder and delinquency: A meta-analysis of randomized controlled trials. Archives of Diseases of Cihldhood. 2002;86:251–256. doi: 10.1136/adc.86.4.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview (CIDI) researcher’s manual. Washington DC: American Psychiatric Press; 1997. [Google Scholar]
- Yamaguchi K, Kandel DB. On the resolution of role incompatibility: Life event history analysis of family roles and marijuana use. American Journal of Sociology. 1985;90:1284–1325. [Google Scholar]
- Young D, Dembo R, Henderson C. A national survey of substance abuse treatment for juvenile offenders. Journal of Substance Abuse Treatment. 2007;32:255–266. doi: 10.1016/j.jsat.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]