Summary
Background
To determine efficacy and safety of postoperative titrated morphine in elderly patients when intravenous boluses of morphine were adapted to age.
Methods
In the Post Anaesthesia Care Unit (PACU), patients complaining of pain received morphine until adequate pain relief. Intravenous morphine was titrated as 3 mg boluses for young (age ≤ 65 yrs) and 2 mg for elderly patients (> 65 yrs) respectively, every 5 min.
Results
Three hundred fifty young and 68 elderly patients were included. No significant difference between the two groups was detected in Numerical Rating Scale (NRS, 0 = no pain; 10 = worst imaginable pain) at the onset of titration: 7.4 ± 1.7 vs 7.5 ± 1.7, the area under the curves of NRS versus morphine boluses: 97.7 ± 59.6 vs 98.2 ± 62, the number of boluses required to obtain pain relief: 3 ± 1.3 vs 3 ± 1.3, the percentage of titration failure: 10% vs 9% and the incidence of excessive sedation: 18% vs 21%. On the other hand, renal clearance was significantly reduced in elderly patients compared to the young: 55 ± 21 vs 85 ± 15 ml/min; p < 0.0001.
Conclusion
With a lower dose of morphine, elderly patients beneficiated comparable efficient and safe pain relief as younger. The decrease in renal clearance of morphine, support the reduction of intravenous bolus doses of morphine in patients aged > 65 yrs in the immediate postoperative period.
Keywords: Adult; Age Factors; Aged; Aged, 80 and over; Analgesics; Opioid; administration & dosage; Area Under Curve; Clinical Protocols; Female; Humans; Kidney Function Tests; Male; Middle Aged; Morphine; administration & dosage; Pain Measurement; methods; Pain, Postoperative; drug therapy; Prospective Studies; Treatment Outcome
Keywords: Postoperative period, pain postoperative, morphine, aged, age groups
Introduction
Elderly patients represent a large and rapidly increasing proportion of surgical patients 1,2. Proper assessment and management of postoperative pain in these patients is of importance because inadequate analgesia is likely to increase postoperative confusion, cardiovascular morbidity and delayed rehabilitation 3,4. Nonetheless, pain is still poorly treated in older postoperative patients 5. Intravenous administration of morphine is generally used for the treatment of postoperative pain in the post-anaesthesia care unit (PACU). The use of small intravenous boluses of morphine provides efficient and rapid onset of analgesia 6. Boluses of 2- or 3-mg every 5 min are most frequently used 7–10. Parameters according to which the bolus dose must be adjusted, either weight or age, are still debated. Based on the assumption that titration is performed over a short period in which age-related changes in pharmacokinetics and pharmacodynamics might be less important than for prolonged postoperative periods 11,12, the same protocol of intravenous morphine titration based on weight has been proposed in both young and elderly patients 9. However, several teams 13,14 take into account the patient’s age rather than weight to adapt the bolus dose because of age-related changes in the metabolism and clearance of morphine even over a short period 15.
The aim of this observational prospective study was to compare the quality and safety of postoperative analgesia in younger and older surgical patients when intravenous boluses of morphine were adapted to age. We hypothesized that with a lower dose of morphine, the older patients will beneficiate the same quality of postoperative analgesia as younger ones.
Methods
We prospectively collected data on unselected patients who required intravenous morphine titration. The patients were included consecutively as they presented over an eight months period. During the study period, the anaesthetic and postoperative pain management did not differ from routine practice; hence, ethics committee approval and informed consent were not required.
Setting
This prospective study was carried out in a university hospital. This hospital has 402 surgical beds and admits on average 12 000 surgical patients each year. All surgical procedures performed in our institution (i.e. orthopaedic, general, urological and gynaecological) were included in the study.
Patients
All in-patients undergoing surgery under general anaesthesia, were included in the study. Patients having at least one of the following criteria were not included: regional block, epidural or spinal anaesthesia, inability to read or speak French, the likelihood of delayed postoperative tracheal extubation in the PACU, ASA physical status over 3.
Treatment and measurements
We prospectively collected the demographic characteristics, surgical, intraoperative analgesics, and postoperative pain management data of each patient. Operations were classified as major, intermediate, and minor procedures according to the expected level of postoperative pain as previously proposed 7 (table 1).
Table 1.
Types of operation classified as major, intermediate, and minor procedures according to the expected level of postoperative pain
| Major | Intermediate | Minor |
|---|---|---|
| Gastrectomy | Appendicectomy | Minor urological procedures (transurethral prostatectomy, testicular surgery) |
| Splenectomy | Laparoscopic procedures | Circumcision |
| Liver/pancreatic surgery | Mastectomy | Superficial surgery |
| Oesophageal surgery | Inguinal hernia | Examination under anesthesia/anal fissure/repair/anal stetch |
| Laparotomy/bowel resection | Vaginal/hysterectomy | Varicose veins |
| Laparotomy/cholecystectomy | Thyroidectomy | |
| Laparotomy/hysterectomy | Total hip replacement | |
| Haemorrhoidectomy | ||
| Thoracic surgery | ||
| Spine fusion | ||
| Renal surgery | ||
| Total knee replacement or arthrolysis | ||
| Adenoidectomy |
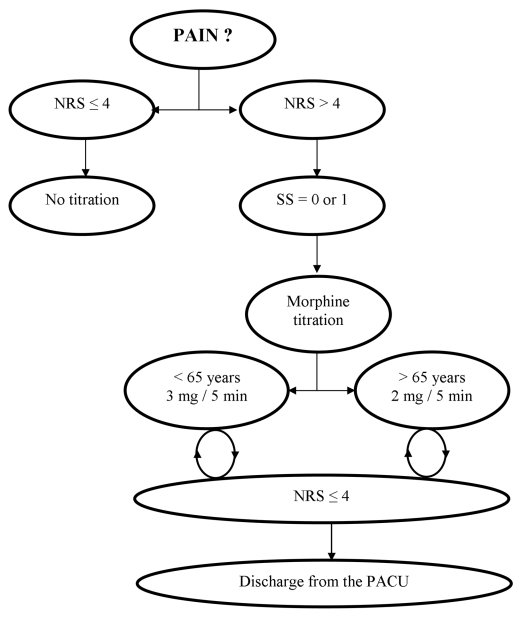
In the PACU after surgery, patients complaining of pain were given intravenous bolus doses of morphine that were repeated until the patient felt comfortable. In the standardised protocol currently used in our hospital, the bolus dose was adjusted to age, 3 mg (≤ 65 yrs) or 2 mg (> 65 yrs) and pain intensity level was assessed using a Numerical Rating Scale (NRS, 0 = no pain; 10 = worst imaginable pain) (figure 1). The protocol set no limit for the total dose that could be given in the absence of excessive sedation (SS > 1). Titration failure was defined as an unchanged NRS after five boluses.
Figure 1. Standard protocol for morphine titration in PACU.
Pain assessment with the Numerical Rating Scale (NRS): ask the patient to rate his pain, 0 = no pain to 10 = worst imaginable pain. Sedation Score (SS): look at the patient and decide which of the following apply: awake = 0; dozing intermittently = 1; mostly sleeping = 2; only awakens when aroused = 3.
For patients who did not require morphine titration because of low pain intensity (NRS ≤ 4), postoperative analgesia was achieved with intravenous paracetamol, ketoprofen, nefopam or tramadol. Patients were not discharged from the recovery room until they were comfortable with a NRS ≤ 4.
End Points
Patients were divided into a young (≤ 65 yrs) and old (> 65 yrs) group. The primary end point was the log of area under the curves (AUC) of NRS during titration versus morphine boluses. This endpoint reflects the cumulative pain of the patients. The secondary end points were the number of morphine boluses needed to achieve a NRS ≤ 4, the percentage of patients with titration failure and the percentage of patients with excessive sedation in each group. Also, renal function was evaluated in a subset of 30 patients in each group to characterise age-related pharmacokinetic changes. No additional blood samples were performed in these patients because we used tests which were available in the preoperative assessment. Estimated clearance was determined using the Cockroft-Gault formula.
Statistics
The primary outcome measure was the log AUC of NRS during titration and the objective was to demonstrate the equivalence of the log AUC in both groups (young and elderly). The difference of means (young minus elderly) was supposed to be within the interval (−0.3, 0.3) (in the log scale). When the number of patients in each group is 70, an equivalence test will have 80% power to reject the null hypothesis that young patients and elderly patients are not equivalent (i.e., the difference in means is 0.3 or more from 0 in the same direction) in favor of the alternative hypothesis that the means of the two groups are equivalent, assuming that the expected difference is 0, the common standard deviation is 0.6 and that alpha is equal to 5%.
For other comparisons between young and elderly patients, superiority tests were used as appropriate (i.e., chi square tests for qualitative outcomes and t test for continuous outcomes). All statistical superiority tests were 2-sided at the 0.05 level of significance. All statistical analyses were performed using SAS 9.2.
Results
Four hundred eighteen patients were included in the study. Mean patient age was 47.8 ± 16 yrs, 166 (40%) patients were men and 252 (60%) were women. They were admitted after orthopaedic surgery in 213 (51%) patients, abdominal surgery in 127 (30.5%) patients, urologic surgery in 36 (8.5%) patients and thoracic surgery in 11 (2.5%) patients. Three hundred fifty patients (84%) were 65 yr old or younger and 68 (16%) were older than 65 yr of age. The main characteristics of these two populations are shown in table 2. Type of surgery in regards of the expected level of postoperative pain (major, intermediate, minor) was comparable between groups. Percentage of patients receiving intraoperative analgesics or analgesics in association with morphine titration in the PACU was not significantly different between groups.
Table 2.
Main characteristics of young and elderly patients.
| Elderly patients (n = 68) | Young patients (n = 350) | P Value | |
|---|---|---|---|
| Age (yr) | 74 ± 6 | 43 ± 12 | – |
| Male sex | 19 (28) | 147 (42) | 0.03 |
| Height (cm) | 164 ± 8 | 168 ± 10 | 0.0006 |
| Weight (kg) | 68 ± 14 | 77 ±25 | < 0.0001 |
| BMI | 25 ± 5 | 28 ± 16 | <0.01 |
|
Type of surgery Major Intermediate Minor |
24 (35) 42 (62) 2 (3%) |
99 (28) 238 (68) 13 (4) |
NS |
| Intraoperative analgesics administration | 62 (91) | 313 (89) | NS |
| Analgesics administration in PACU | 24 (35) | 98 (28) | NS |
| Creatinine clearance (ml/min) | 55 ± 21 | 85 ± 15 | < 0.0001 |
Data are means ± SD or number (percentages).
NS = not significant; BMI = Body mass index; Analgesics = paracetamol, nefopam, tramadol or ketoprofen; PACU = postanaesthesia care unit.
The mean AUC for the elderly patients was equal to 98.19 ± 61.95 and to 97.75 ± 59.64 for the young patients. The mean log AUC difference was equal to −0.03 with a 90% confidence interval equal to (−0.17, 0.10). The confidence interval fit within the equivalence range showing equivalence between young and elderly people.
No difference was found on initial NRS score at the onset of morphine titration, the number of boluses to achieve pain relief and the percentage of titration failure (table 3). In the same manner, the number of patients with excessive sedation was not significantly different. In contrast, the creatinine clearance was altered in the older group and significantly reduced compared to the young group (table 1; p < 0.0001).
Table 3.
Comparison of morphine titration characteristics
| Elderly patients (n = 68) | Young patients (n = 350) | P Value | |
|---|---|---|---|
| Initial NRS | 7.5 ± 1.7 | 7.4 ± 1.6 | NS |
| Number of morphine boluses | 3.0± 1.5 | 3.0± 1.3 | NS |
| Titration failure | 6 (9) | 35 (10) | NS |
| Excessive sedation | 14 (21) | 64 (18) | NS |
| Titration failure or excessive sedation | 20 (29) | 99 (28) | NS |
Data are means ± SD or number (percentages).
NRS = Numerical rating scale; Titration failure was defined as an unchanged NRS after five boluses; Excessive sedation = SS > 1.
Discussion
The current study suggests that when intravenous morphine boluses (2- or 3-mg) are adjusted to age, postoperative analgesia characteristics are the same in young and elderly patients. Most importantly, for the older patients, the protocol used permits to achieve rapid and efficient analgesia equivalent as in young patients with no significant increased sedation in the elderly.
In accordance with several previous reports, elderly required less morphine for comparable levels of analgesia 11,12,16. This pattern is consistent with works that found in elderly patients an increased brain sensitivity to the effects of opioids 17–20. In addition to these pharmacodynamic changes, even for short-term period, age related opioid pharmacokinetics changes must play an important role. Owen and colleagues have reported after a single intravenous dose of 10 mg/70 kg morphine a higher drug concentration in the peripheral compartment in older subjects for 1.5 hr after dosing 15. This observation could be explained by the progressive reduction in the functional capabilities of the kidney with age that leads to a significant decrease in the renal clearance of opioids and their metabolites 21. The decrease of renal clearance in elderly patients reported in the current study is supposed to be associated with an accumulation of morphine metabolites such as morphine-6-glucuronide 22,23. with a longer duration of analgesia 18 and increased risk of morphine-related adverse effects. On the other hand, it could be argued that a protocol based on weight (bolus of 2 mg morphine every 5 min for body weight ≤ 60 kg or 3 mg for body weight > 60 kg) has been safely administered to elderly patients 9. However, in this study, only the short postoperative period in the PACU was evaluated and it can not be ruled out that for the later period in the surgical ward, older patients would exhibited more sedation and periods of hypoxemia.
Since several studies have suggested that elderly patients report lower pain intensity than younger surgical patients 24,25, it could also be argued that a protocol based on weight would better prevent the risk of undertreatment in elderly patients. Nevertheless, it has been demonstrated that age differences in postoperative pain are scale dependent 26. The NRS seems to be the most appropriate to evaluate postoperative pain in patients more than 65 years of age 27. Using this scale, we found no significant difference between the two groups for pain intensity score at the onset of titration (7.5 ± 1.7 vs 7.4 ± 1.7, respectively for elderly and young patients).
The results of the present study suggest that older patients and younger have equivalent pain management. For comparable surgical procedures, there was no difference between the groups for the analgesics (paracetamol, ketoprofen, nefopam or tramadol) administered intraoperatively or in the PACU. Furthermore, the same rate of titration failure in the two groups also suggested that elderly patients were not undertreated with the protocol used. There were a significantly greater percentage of women in elderly patients. Sex-related differences in the perception of pain and susceptibility to opioids remain a matter of debate. Aubrun and colleagues have recently reported in a study comparing pain scores and postoperative morphine consumption in the PACU that women had a higher initial VAS and required a greater dose of intravenous morphine titrated. However, they observed the disappearance of sex-related differences in elderly patients (> 75 yr) 28. In our study, since the mean age for elderly was 74 yr, it could be suggested that the sex ratio difference observed had no impact on morphine requirements in these subjects.
In conclusion, as the proportion of elderly people in the population increases, the need for appropriate management of postoperative pain in this group also grows. The results of the current study suggest that a protocol of intravenous morphine titration adapted to age is efficient and safe in elderly patients. We observed that lower doses of morphine in elderly patients are required to obtain comparable pain relief during the immediate postoperative period. The amount of morphine spared in older patients could reduce the risk of delayed opioid undesirable side effects.
Acknowledgments
We thank the nurses of the post-anaesthesia care unit (Department of Anaesthesia, Hospital Bichat, 46 rue Henri Huchard, F-75018 Paris).
References
- 1.Clergue F, Auroy Y, Péquignot F, Jougla E, Lienhart A, Laxemarie MC. French survey of anaesthesia in 1996. Anesthesiology. 1999;91:1509–20. doi: 10.1097/00000542-199911000-00045. [DOI] [PubMed] [Google Scholar]
- 2.Rooke GA, Reves JG, Rosow C. Anesthesiology and geriatric medicine (editorial) Anesthesiology. 2002;96:2–4. doi: 10.1097/00000542-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Organizations JCoAoH. Pain: Current understanding of assessment, management, and treatments. 2005 December 2001; Available at: www.jcaho.org.
- 4.Ferrell BR, Shaffner M. Pharmacoeconomics and medical outcomes in pain management. Semin Anesth. 1997;16:152–9. [Google Scholar]
- 5.Karani R, Meier DE. Systemic pharmacologic postoperative pain management in the geriatric orthopaedic patient. Clin Orthop Relat Res. 2004;425:26–34. doi: 10.1097/01.blo.0000132403.53010.6f. [DOI] [PubMed] [Google Scholar]
- 6.Edward WT, Breed RJ. The treatment of acute postoperative pain in postanesthesia care unit. Anesthesiol Clin. 1990;8:235–65. [Google Scholar]
- 7.Dahmani S, Dupont H, Mantz J, Desmonts JM, Keita H. Predictive factors of early morphine requirements in the post-anaesthesia care unit (PACU) Br J Anaesth. 2001;87:385–9. doi: 10.1093/bja/87.3.385. [DOI] [PubMed] [Google Scholar]
- 8.Aubrun F, Monsel S, Langeron O, Coriat P, Riou B. Postoperative titration of intravenous morphine. Eur J Anaesthesiol. 2001;18:159–65. doi: 10.1046/j.0265-0215.2000.00796.x. [DOI] [PubMed] [Google Scholar]
- 9.Aubrun F, Monsel S, Langeron O, Coriat P, Riou B. Postoperative titration of intravenous morphine in the elderly patient. Anesthesiology. 2002;96:17–23. doi: 10.1097/00000542-200201000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Paqueron X, Lumbroso A, Mergoni P, Aubrun F, Langeron O, Coriat P, Riou B. Is morphine-induced sedation synonymous with analgesia during intravenous morphine titration? Br J Anaesth. 2002;89:697–701. [PubMed] [Google Scholar]
- 11.Gagliese L, Jakson M, Ritvo P, Wowk A, Katz J. Age is not impendiment to effective use of patient controlled analgesia by surgical patients. Anesthesiology. 2000;93:601–610. doi: 10.1097/00000542-200009000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Macintyre PE, Jarvis DA. Age is the best predictor of postoperative morphine requirements. Pain. 1995;64:357–364. doi: 10.1016/0304-3959(95)00128-X. [DOI] [PubMed] [Google Scholar]
- 13.Keita H, Geachan N, Dahmani S, Couderc E, Armand C, Quazza M, Mantz J, Desmonts JM. Comparison between patient-controlled analgesia and subcutaneous morphine in elderly patients after total hip replacement. Br J Anaesth. 2003;90:53–7. doi: 10.1093/bja/aeg019. [DOI] [PubMed] [Google Scholar]
- 14.Pico L, Hernot S, Zlotine N, Nègre I, Samii K, Fletcher D. Peroperative titration of morphine for postoperative nanlgesia after total hip arthroplasty. Can J Anaesth. 2000;47:309–14. doi: 10.1007/BF03020943. [DOI] [PubMed] [Google Scholar]
- 15.Owen JA, Sitar DS, Berger L, Brwnell L, Duke PC, Mitenko PA. Age-related morphine kinetics. Clin Pharmacol Ther. 1983;34:364–8. doi: 10.1038/clpt.1983.180. [DOI] [PubMed] [Google Scholar]
- 16.Burns JW, Hodsman NBA, McLintock TTC, Gillies GWA, Kenny GNC, McArdle CS. The influence of patient characteristics on the requirements for postoperative analgesia. Anaesthesia. 1989;44:2–6. doi: 10.1111/j.1365-2044.1989.tb11086.x. [DOI] [PubMed] [Google Scholar]
- 17.Wall RT. Use of analgesics in the elderly. Clin Geriatr Med. 1990;6:345–64. [PubMed] [Google Scholar]
- 18.Kaiko RF. Age and morphine analgesia in cancer patients with postoperative pain. Clin Pharmacol Ther. 1980;28:823–6. doi: 10.1038/clpt.1980.241. [DOI] [PubMed] [Google Scholar]
- 19.Kaiko RF, Wallenstein SL, Rogers AG, Grabinski PY, Houde RW. Narcotics in the elderly. Med Clin North Am. 1982;66:1079–89. doi: 10.1016/s0025-7125(16)31383-9. [DOI] [PubMed] [Google Scholar]
- 20.Belleville JW, Forrest WH, Miller E, Brown BW. Influence of age on pain relief from analgesics. JAMA. 1971;217:1835–41. [PubMed] [Google Scholar]
- 21.Muravchick S. Anesthesia for the elderly. In: Miller RD, editor. Anesthesia. 4. New York, NY: Churchill Livingstone; 1994. pp. 2143–56. [Google Scholar]
- 22.Osborne R, Joel S, Grbenik K, Trew D, Slevin M. The pharmacokinetics of morphine and morphine glucuronides in kidney failure. Clin Pharmacol Ther. 1993;54:158–67. doi: 10.1038/clpt.1993.127. [DOI] [PubMed] [Google Scholar]
- 23.Chauvin C, Sandouk P, Scherrmann JM, Farinotti R, Strumza P, Duvaldestin P. Morphine pharmacokinetics in renal failure. Anesthesiology. 1987;66:327–31. doi: 10.1097/00000542-198703000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Kalkman CJ, Visser K, Moen J, Bonsel GJ, Grobbee DE, Moons KG. Preoperative prediction of severe postoperative pain. Pain. 2003;105:415–23. doi: 10.1016/S0304-3959(03)00252-5. [DOI] [PubMed] [Google Scholar]
- 25.Bisgaard T, Klarskov B, Rosenberg J, Kehlet H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain. 2001;90:261–9. doi: 10.1016/S0304-3959(00)00406-1. [DOI] [PubMed] [Google Scholar]
- 26.Gagliese L, Katz J. Age differences in postoperative pain are scale dependent: a comparison of measures of pain intensity and quality in younger and older surgical patients. Pain. 2003;103:11–20. doi: 10.1016/s0304-3959(02)00327-5. [DOI] [PubMed] [Google Scholar]
- 27.Gagliese L, Weizblit N, Ellis W, Chan VWS. The mesurement of postoperative pain: A comparison of intensity scales in younger and older surgical patients. Pain. 2005;117:412–20. doi: 10.1016/j.pain.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Aubrun F, Salvi N, Coriat P, Riou B. Sex-and age-related differences in morphine requirements for postoperative pain relief. Anesthesiology. 2005;103:156–60. doi: 10.1097/00000542-200507000-00023. [DOI] [PubMed] [Google Scholar]