Abstract
Self reported measures of poor health and morbidities from developing countries tend to be viewed with considerable skepticism. Examination of the social gradient in self-reported health and morbidity measures provides a useful test of the validity of self-reports of poor-health and morbidities. The prevailing view, in part influenced by Amartya Sen, is that socially disadvantaged individuals will fail to perceive and report the presence of illness or health-deficits because an individual’s assessment of their health is directly contingent on their social experience. In this study, we tested whether the association between self-reported poor-health/morbidities and socioeconomic status (SES) in India follows the expected direction or not. Cross sectional logistic regression analyses were carried out on a nationally representative population based sample from the 1998–99 Indian National Family Health Survey (INFHS); and 1995–96 and 2004 Indian National Sample Survey (INSS). Four binary outcomes were analyzed: any self-reported morbidity; self-reported sickness in the last 15 days; self-reported sickness in the past year; and poor self-rated health. In separate adjusted models, individuals with no education reported higher levels of any self-reported, self-reported sickness in the last 15 days, self-reported sickness in the last year, and poor self-rated health compared to those with most education. Contrary to the prevailing thesis, we find that the use of self-rated ill health has face validity as assessed via its relationship to SES. A less dismissive and pessimistic view of health data obtained through self-reports seems warranted.
Keywords: Validity, India, Subjective health, Socioeconomic Status (SES), morbidity
Introduction
Self reported measures of poor health and morbidities from developing countries tend to be viewed with considerable skepticism. In an influential editorial, Amartya Sen argued that there is a fundamental disconnect between an individual’s subjective perception of their health and the objective or actual health condition that they may have (A. Sen, 2002; A. K. Sen, 1993). According to Sen, because an individual’s assessment of their health is directly contingent on their social experience, socially disadvantaged individuals will fail to perceive and report the presence of illness or health-deficits (A. Sen, 2002). For instance, an individual with no formal knowledge of diseases but residing in an area with substantial disease burden that unfortunately has inadequate social infrastructure facilities may be inclined to treat disease symptoms as “normal” given their lack of awareness, and therefore, health-expectation. Sen, therefore, reasons that perceptions and self-reports of health – which he refers to as the “internal” view of health – can be “extremely misleading” as they obscure the true extent of health deprivation more likely to be captured through “objective” or “external” assessments (A. Sen, 2002).
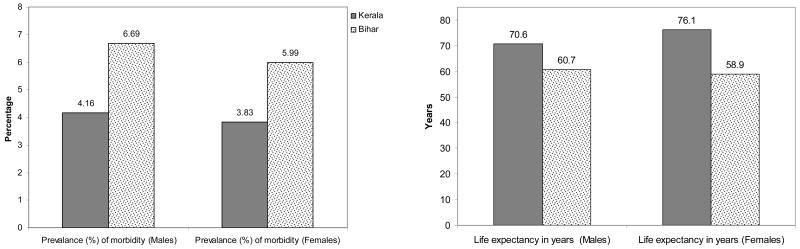
The empirical test of the validity of self-reported health and morbidity measures in developing countries is based on examining the association between socioeconomic status (SES) and self-reported health and morbidity measures. If a positive (or a null) association between SES and self reports of poor-health/morbidities is observed such that high SES individuals report higher (or the same) prevalence of ill-health compared to low SES individuals, then such evidence has been used to cast doubt on the use of self-reported measures of health or disease status in population-based surveys. In a recent paper Manesh and colleagues used a similar approach to assess social gradients in mothers’ report of diarrhea among children and argued that reported measures of morbidities are misleading, based on the absence of an observed association (Manesh, Sheldon, Pickett, & Carr-Hill, 2008). For instance, in arguing against the use of self-reported health measures, Sen compared aggregated self-reported morbidity rates and life expectancy between two Indian states – Kerala and Bihar, with Kerala reporting considerably higher rates of morbidities despite experiencing the highest level of longevity, while Bihar with low levels of longevity reporting lower rates of morbidities (A. Sen, 2002). The argument was that Bihar, with a substantially illiterate population and meager health provision, may have a very low perception of illness, even though there is likely to be substantial disease burden as reflected in Bihar’s low life expectancy figures. Conversely, Kerala, with high levels of literacy and adequate health provision, is better positioned to identify and perceive morbidities. As Sen put it, “in this charmed internal comparison”, Bihar would be incorrectly identified as “healthy” when compared to Kerala. Others have also used this motivation to criticize the use of self-rated health (King, Murray, Salomon, & Tandon, 2004; Salomon, Tandon, & Murray, 2004).
It may be noted that the aggregated data on morbidity rates reported by Sen in his 2002 editorial, is from the “mid-1970s” (A. Sen, 2002). Indeed, the data from more recent years on life expectancy and self-reported morbidities in Kerala and Bihar show that Bihar not only has lower life expectancy as compared to Kerala, it also has higher levels of self-reported morbidities, as one would expect (Figure 1).
Figure 1. Life expectancy and age-adjusted prevalence of any reported morbidity for men and women in Kerala and Bihar.
Source: India: Human Development Report 2005, UNDP; Bihar and Kerala: Registrar General of India (2003) SRS Based Abridged Life Tables, SRS Analytical Studies, Report No. 3 of 2003, New Delhi: Registrar General of India; INFHS-2, 1998–1999.
We examined the most recent, large-scale and nationally representative disaggregated data to investigate the association between education and various self-reported poor health/morbidity measures in India; a country classified by the World Bank as a “low income” economy, with a per capita gross national income of $875 or less, in 2005 (Bank, 2005). We tested whether there is, in fact, an inverse association (as expected) between SES (as measured by educational attainment) and self-reported ill-health in India. If the direction of the educational gradient is counter to our hypothesis – or if no association is observed – this would tend to lend credence to the view that self-rated measures of health are inherently untrustworthy in this developing country setting.
Methods
We used two data sources for the study: the 1998–99 Indian National Family Health Survey (INFHS),(IIPS, 2000) – a large representative cross-sectional survey of households and individuals aged <1 to 95 years; and the 1995–96 and 2004 Indian National Sample Survey (INSS) of households and individuals (India, 1998, 2006).
Four separate and different types of self-rated ill-health were analyzed from the two data sources. The INFHS obtained self-reported morbidity based on the respondents’ answer to the following question: “Does anyone, listed as a member of this household in this survey, suffer from asthma/malaria/jaundice/tuberculosis?” We created a binary self-reported morbidity variable with 1 if the individual reported any one of the listed morbidities, 0 otherwise. The INSS obtained self-reported morbidity based on the respondents’ binary answer (yes or no) to two separate questions: “Have you been sick in the last 15 days?” and “Have you been sick in the last 365 days?”. The respondents in both the surveys answered the presence or absence of morbidity for themselves as well as for other household members. Finally, in one sub-sample of elderly population aged 60 and above, the INSS also measured overall health perception using the following question: “What is your perception about your current state of health: excellent/very good; good/fair; poor?” We created a binary self-reported poor health variable for every individual with 1 if the individual reported poor, 0 otherwise.
The key individual predictor variable of interest was education. Of the several markers of socioeconomic status, education is perhaps most appropriately suited for this investigation. Lack of health-awareness, and therefore health-expectation, is argued as the major reason why socially disadvantaged individuals are less likely to be aware of adverse health condition and therefore less likely to report one. Further, formal educational attainment can be considered a reasonable marker of individuals’ level of awareness and health expectation, besides being a chronic marker of social disadvantage. Education was measured in terms of years of education for every individual, and was grouped using the following Indian educational benchmarks: illiterate (no formal education), primary (≤5 years), secondary (6–12 years), and post-secondary (≥13 years).
All results were adjusted for age, sex, caste, religion, urban/rural status and economic standard of living. In the INFHS, economic standard of living was measured by creating a linear index of household assets and material possessions (Filmer & Pritchett, 1998), while in the INSS economic standard of living was based on consumption-based expenditure data (Deaton, 2001; India, 2002).
Logistic regression modeling approach was utilized, with the standard errors accounting for the multi-stage sampling design of the surveys. To facilitate interpretation, results are presented in terms of odds ratios (OR) and 95% confidence intervals (CI).
Two additional sets of analyses were conducted to assess whether the less educated individuals are less likely to report their ill-health status. For the first set of analysis, we used the 1998–99 INFHS, which contained an objective measure of anemia for the ever-married women between ages 15–49 (n= 74719; after excluding those with no measurements on anemia and no information on the covariates considered in this study). Anemia was diagnosed based on hemoglobin levels. Capillary hemoglobin concentration was measured in grams per deciliter using the HemoCue system which has been shown to be accurate and is widely used (WHO, 1997). We used the clinical cut-offs to define severe (<7 gm/deciliter) and moderate anemia (7–9.99 gm/deciliter) among women (WHO, 1997). We estimated logistic regression models within each of the severely and moderately anemic strata, of self-reported morbidity (outcome) and education, adjusting for age, urban/rural status, caste and economic standard of living.
For the second set of analysis, we utilized the 2004–05 INSS. While INSS did not collect any objective health information, respondents who replied affirmatively to the question of being sick in the last 15 and 365 days were further asked if they were aware of the diagnosis related to the sickness. We stratified samples based on three broad categories of self-reports of diagnosis: Diagnosis 1: diarrhea, gastritis, worm infestation, amebiasis, bronchial asthma, anemia, hepatitis, tuberculosis, sexually transmitted diseases, malaria, filariasis, whooping cough; Diagnosis 2: heart disease, hypertension, prostatic disorders, neurological and psychiatric disorders, diabetes, cancer; and Diagnosis 3: locomotor, visual, speech, and hearing disabilities. Diagnoses 1 and 2 reflect loosely the diseases from the early and middle-to-later stages of the epidemiologic transition, while Diagnosis 3 reflects physical disabilities. We estimated logistic regression models within each strata of self reported diagnosis of overall self-rated poor health (outcome) and education, adjusting for age, sex, urban/rural status, and economic standard of living.
Results
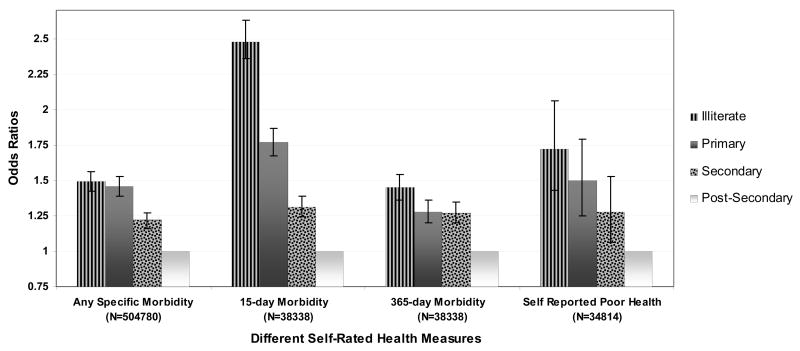
Using the highest educational attainment category as reference, in the INFHS sample, individuals who had no formal education reported higher levels of any self-reported morbidity (OR 1.49, 95% CI 1.42–1.56) even after adjusting for age, sex, caste, urban/rural status and economic standard of living. The association followed an inverse gradient; as educational attainment decreases the odds of reporting morbidities increase (Figure 2). The inverse educational gradient was also observed when we examined specific morbidities separately, such that the odds ratios for reporting any specific morbidity for individuals with no education was substantially higher compared to those with most education [Asthma: OR 1.91 (95% CI 1.76–2.08); Tuberculosis: OR 1.58 (95% CI 1.32–1.89); Malaria: OR 1.09 (95% CI 1.02–1.17); Jaundice: OR 1.15 (95% CI 1.05–1.26)].
Figure 2. Odds ratios and 95% confidence intervals for self-reported morbidity and self-reported poor health among elderly by educational attainment for All India.
Note: Models are adjusted for age, sex, caste, urban/rural status, and economic standard of living / income. The overall effect of education on any given self-rated health measures was statistically significant at p<0.0001.
The inverse association between educational attainment and morbidity was also observed in the INSS 2004 sample for both the 15-day morbidity as well as 365-day morbidity. Individuals with no education were 2.5 times (95% CI 2.34–2.63) and 50% (95% CI 1.36–1.54) more likely to report sick in the last 15 days or 365 days, respectively, compared to those with post-secondary education. The patterns were similar for the 1995–96 INSS sample as well (data not shown).
In the 2004 INSS sample, elderly individuals with no formal education were 72% more likely to report poor health (95% CI 1.43–2.06), compared to those with post-secondary education, with a dose-response relationship between education and log odds of reporting poor health. The inverse gradient between education and self-rated poor health was even stronger in the 1995–96 INSS sample, with elderly individuals with no education being 2.5 times (95% CI 1.94–3.37) more likely to report poor health (Figure 2).
Thus, regardless of the nature of the self-reported health question, we consistently found that those with low or no education were significantly more likely report morbidities or perceive poor health, compared to those with higher levels of education.
We conducted several additional tests in the INFHS sample to examine several subsidiary questions that can be potentially linked to the aim of ascertaining whether those with low education are less likely to report poor health/morbidities. First, the inverse association between education and self-reported poor health/morbidities, shown in Figure 2, was robust to adjustment for any state-level differences which was achieved via specifying fixed effects for each Indian state. Second, we conducted a multilevel test of whether village- (in rural areas) or ward-level (in urban areas) education were associated with individual self-reported morbidity. We found that for a 10% increase in the illiteracy level of the village/ward, the odds of reporting any morbidity was 1.02 (95% CI 1.00–1.04). Thus, low levels of individual and area education were associated with an increased probability of self-rated morbidity. Finally, we conducted a multilevel test of whether state economic development (measured through per capita income and percent poverty (India, 2002) predicted the individual likelihood of self-reported morbidity, conditional on individual education, and other variables. We observed that for 1 standard deviation (SD) increase in state per capita income (SD=Indian Rupees 1323) or proportion people in a state who are poor (SD=0.12), the odds ratios for reporting any morbidity were 0.78 (95% CI 0.60–1.01), and 1.55 (95% CI 1.25–1.92), respectively. In summary, the likelihood of reporting morbidities was higher among disadvantaged individuals and disadvantaged villages/wards or states.
Table 1 presents the adjusted association between self-reported morbidity and education within sub-samples of women with same levels of severe or moderate anemia that were objectively measured. We found that among severely anemic women, those with no formal education were more likely to report presence of any morbidity (OR: 1.82, 95% CI 1.28–2.57) as compared to women with post-secondary education. However, the overall education-morbidity relationships were not statistically significant. Evaluating the education-morbidity association within the sub-sample of women with moderate anemia we found that less educated women are more likely to report morbidities, with the overall relationship being not statistically significant.
Table 1.
Odds ratios and 95% confidence intervals for self-reported morbidity among sub-samples of ever-married women (aged 15–49) who, objectively speaking, are severely or moderately anemic by socioeconomic status for All India.
| Severely Anemic | Moderately Anemic | |
|---|---|---|
| Educational categories | N=1189 | N=11117 |
| p=0.52 | p=0.54 | |
| Illiterate | 1.82 (1.28, 2.57) | 1.37 (0.90, 2.08) |
| Primary | 1.24 (0.24, 6.41) | 1.32 (0.87, 2.00) |
| Secondary | 0.85 (0.15, 4.74) | 1.28 (0.84, 1.96) |
| Post-Secondary | 1 | 1 |
Note: Models are adjusted for age, caste, urban/rural status, and economic standard of living.
Table 2 presents the adjusted association between overall self-rated poor health and education within sub-samples of elderly with same self-reports of diagnostic groupings. Conditional on the self-report of diagnosis strata, there was no evidence to suggest that those with no education are less likely to report poor-health. On the contrary, elderly individuals with no formal education were more likely to perceive poor health, with the odds ratios varying between 1.24 and 2.00 across the three self-reported diagnosed disease strata.
Table 2.
Odds ratios and 95% confidence intervals for overall self-rated poor health among sub-samples of the elderly based on self-diagnosis of diseases by socioeconomic status for All India, 2004–05
| Diagnosis 1 | Diagnosis 2 | Diagnosis 3 | |
|---|---|---|---|
| Educational categories | N=3017 | N=5324 | N=2256 |
| p <0.0001 | p <0.0001 | p <0.4154 | |
| Illiterate | 1.88 (1.05, 3.38) | 2.00 (1.49, 2.68) | 1.24 (0.55, 2.76) |
| Primary | 1.44 (0.81, 2.58) | 1.57 (1.18, 2.09) | 1.16 (0.52, 2.58) |
| Secondary | 1.15 (0.63, 2.08) | 1.29 (0.97, 1.71) | 0.91 (0.40, 2.05) |
| Post-Secondary | 1 | 1 | 1 |
Note: Models are adjusted for age, sex, caste, urban/rural status, and income. Diagnosis 1 includes diarrhea, gastritis, worm infestation, amoebiosis, bronchial asthma, anemia, hepatitis, tuberculosis, sexually transmitted diseases, malaria, filariasis, whooping cough; Diagnosis 2 includes heart disease, hypertension, prostatic disorders, neurological and psychiatric disorders, diabetes, cancer); and Diagnosis 3 includes locomotor, visual, speech, hearing.
Discussion
Contrary to the prevailing view that there is a positive (or null) association between measures of SES and self-reported poor health/morbidities in less-developed countries, we found that those with less education are more likely to report specific morbidities, sickness and overall poor health in India. We also found that conditional on the same levels of objective health condition, low educated women are more likely to report the presence of any specific morbidities compared to those with higher education. Taken together, our study shows that any potential “under-reporting” is not only smaller than the difference in prevalence of illness between the socially disadvantaged and the advantaged; the same is even true within groups with the same objective diagnosis. The inverse association between SES and self-reported poor health/morbidities should be anticipated since on objective measures such as mortality or undernutrition, the burden clearly falls disproportionately on socially disadvantaged populations in India (Subramanian, Nandy, Irving, Gordon, Lambert, & Davey Smith, 2006; Subramanian, Smith, & Subramanyam, 2006; Subramanian & Smith, 2006). Moreover, socially disadvantaged groups in India have also been observed to have higher prevalence of self-reported unhealthy behaviors (e.g., tobacco and alcohol use) (Subramanian, Nandy, Irving, Gordon, & Davey Smith, 2005; Subramanian, Nandy, Kelly, Gordon, & Davey Smith, 2004).
We acknowledge that our analysis does not provide a conclusive test of the extent to which there is under-reporting of poor health/morbidity status by low SES individuals. A broader set of objectively measured indicators of health (e.g. biomarkers) would have been ideal. In addition, it would have been more informative if the survey had collected self-reports of anemia-specific symptoms such as dizziness, weakness, tiredness, shortness of breath etc. In other words, the worse overall health rating by low educated women with anemia could have been due to other unobserved health conditions. Indeed, our findings could have been observed under conditions in which socially disadvantaged individuals may still have been underestimating the extent or severity of their morbidities, even while being more likely to perceive and report the presence of illness. Thus, Sen’s thesis may still have some force, and would be difficult to test in the absence of more objective measures of health status. We should also note that perhaps the basis for reporting morbidities can depend upon the specific nature of the morbidity, and in this study we used cause-specific morbidities in an “interchangeable” manner. Furthermore, examining specific morbidities is also contingent on the context of epidemiologic transition. In the context of India, where not only is there substantial presence of communicable diseases but also notable presence of non-communicable diseases (and often the social patterning tends to be distinct), the sets of specific disease conditions that go into the basket of evaluating reported morbidities is likely to influence the association between SES and reported morbidity. Notwithstanding these caveats, the patterns presented for the different specific morbidities were similar to the one observed for any morbidity thereby providing evidence for internal consistency. Also, the use of the global self-rated health question for the elderly presented in this study helps overcome these limitations. We should also note that measures of reported morbidity were answered by the respondent for all the members of the household. However, the patterns remain the same when we restrict the analysis to only respondents. Finally, generalizations based on our study are obviously most applicable to India, and the extent to which our conclusions may be applicable to other developing or low income countries is an important empirical question.
Our findings of an inverse association between SES and self-reported poor health/morbidities are consistent with other relevant findings in the public health literature. For instance, the recent report from India using the 2003 World Health Survey is consistent with the patterns observed in our study (IIPS and WHO, 2006). According to the report, “respondents who reported to be in bad and very bad health state are 21 percent among the illiterates compared to five percent among those with 11 years or higher level of schooling”(IIPS and WHO, 2006)(p.79). A similar pattern emerges for income as well, with those reporting moderate and very bad health state declining substantially at the higher income quintiles (IIPS and WHO, 2006). Second, while self-rated health has been shown to be a robust predictor of mortality in the context of industrialized countries (Baron-Epel, 2004; Idler & Benyamini, 1997; Sickles & Taubman, 1997), similar evidence, until recently, has been absent in the context of developing countries. Using longitudinal data from Indonesia, a study showed that “individuals who perceive their health to be poor” are significantly more likely to die in subsequent follow-up periods than their counterparts who view their health as good, even after inclusion of measures of nutritional status, physical functioning, symptoms of poor physical health and depression, and hypertension (Frankenberg & Jones, 2004). Another recent study from Bangladesh reported that self-reported health was significantly associated with measured physical performance among adult men and women aged 50 and older (Rahman & Barsky, 2003). Finally, the World Health Survey was innovative in its use of “anchoring vignettes” to test the validity of self-rated health assessments across cross-cultural settings. In our interpretation of the studies published thus far using anchoring vignettes (Salomon et al., 2004), there is nothing to suggest that related self-rated questions perform substantially poorer in any significant manner.
In conclusion, the skepticism surrounding the use of self-reported health/morbidity measures in the context of developing countries has little empirical support. While efforts to collect “objective” health data should be encouraged, this need not come at the cost of discounting the use of self-reports of health and morbidity. Besides the obvious strength in terms of the ease, speed, and economy of collecting such information, our study, we believe, provides an empirical basis that such information is by no means “misleading”, as has been claimed. Hence, the skeptical view of self-report health data needs to be reappraised.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. SV Subramanian, Harvard School of Public Health Boston, UNITED STATES, svsubram@hsph.harvard.edu
Malavika A Subramanyam, Harvard School of Public Health.
Sakthivel Selvaraj, Public Health Foundation of India.
Ichiro Kawachi, Harvard School of Public Health.
References
- Bank W. Country Classification. DC: World Bank; 2005. [Google Scholar]
- Baron-Epel O. Self-reported health. In: Anderson NB, editor. Encyclopedia of Health and Behavior. Thousand Oaks, California: Sage Publications; 2004. pp. 714–719. [Google Scholar]
- Deaton A. Counting the World’s Poor: Problems and Possible Solutions. World Bank Research Observer. 2001;16(2):125–147. [Google Scholar]
- Filmer D, Pritchett L. Estimating wealth effects without income or expenditure data - or tears: educational enrolment in India. Washington DC: World Bank; 1998. [DOI] [PubMed] [Google Scholar]
- Frankenberg E, Jones NR. Self-rated health and mortality: does the relationship extend to a low income setting? J Health Soc Behav. 2004;45(4):441–452. doi: 10.1177/002214650404500406. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- IIPS. National Family Health Survey 1998–99. Mumbai: International Institute of Population Sciences; 2000. [Google Scholar]
- India G. o. Morbidity and Treatment of Ailments, NSS 52nd Round (July 1995–June 1996) New Delhi: National Sample Survey Organisation, Ministry of Statistics and Programme Implementation, Government of India; 1998. [Google Scholar]
- India G. o. National Human Development Report 2001. New Delhi: Planning Commission, Government of India; 2002. [Google Scholar]
- India G. o. Morbidity, Health Care and the Condition of the Aged, NSS 60th Round (January - June 2004) New Delhi: National Sample Survey Organisation, Ministry of Statistics and Programme Implementation, Government of India; 2006. [Google Scholar]
- King G, Murray CJL, Salomon JA, Tandon A. Enhancing the validity and cross-cultural comparability of measurement in survey research. American Political Science Review. 2004;98(1):191–207. [Google Scholar]
- Manesh AO, Sheldon TA, Pickett KE, Carr-Hill R. Accuracy of child morbidity data in demographic and health surveys. Int J Epidemiol. 2008;37(1):194–200. doi: 10.1093/ije/dym202. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Iron deficiency: indicators for assessment and strategies for prevention. Geneva: World Health Organization; 1997. [Google Scholar]
- Rahman MO, Barsky AJ. Self-reported health among older Bangladeshis: how good a health indicator is it? Gerontologist. 2003;43(6):856–863. doi: 10.1093/geront/43.6.856. [DOI] [PubMed] [Google Scholar]
- Salomon JA, Tandon A, Murray CJ. Comparability of self rated health: cross sectional multi-country survey using anchoring vignettes. Bmj. 2004;328(7434):258. doi: 10.1136/bmj.37963.691632.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Institute for Population Sciences & World Health Organization (IIPS and WHO) Health System Performance Assessment: World Health Survey, 2003. Mumbai: International Institute for Population Sciences; 2006. [Google Scholar]
- Sen A. Health: perception versus observation. Bmj. 2002;324(7342):860–861. doi: 10.1136/bmj.324.7342.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen AK. Positional objectivity. Philosophy and Public Affairs. 1993;22:126–145. [Google Scholar]
- Sickles RC, Taubman P. Mortality and morbidity among adults and elderly. In: Rozenzweig MR, SO, editors. Handbook of Population and Family Economics. North-Holland; Amsterdam: 1997. [Google Scholar]
- Subramanian SV, Nandy S, Irving M, Gordon D, Davey Smith G. Role of socioeconomic markers and state prohibition policy in predicting alcohol consumption among men and women in India: a multilevel statistical analysis. Bull World Health Organ. 2005;83(11):829–836. [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Nandy S, Irving M, Gordon D, Lambert H, Davey Smith G. The mortality divide in India: the differential contributions of gender, caste, and standard of living across the life course. Am J Public Health. 2006;96(5):818–825. doi: 10.2105/AJPH.2004.060103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Nandy S, Kelly M, Gordon D, Davey Smith G. Patterns and distribution of tobacco consumption in India: cross sectional multilevel evidence from the 1998–9 national family health survey. Bmj. 2004;328(7443):801–806. doi: 10.1136/bmj.328.7443.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Smith GD. Patterns, distribution, and determinants of under-and overnutrition: a population-based study of women in India. Am J Clin Nutr. 2006;84(3):633–640. doi: 10.1093/ajcn/84.3.633. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Smith GD, Subramanyam M. Indigenous Health and Socioeconomic Status in India. PLoS Med. 2006;3(10) doi: 10.1371/journal.pmed.0030421. [DOI] [PMC free article] [PubMed] [Google Scholar]