Abstract
Objective
To study socioeconomic inequalities in AIDS mortality in Barcelona, Spain, during the periods 1991–6 (before highly active antiretroviral therapy (HAART)) and 1997–2001 (post‐HAART) taking into account individual as well as community effects of socioeconomic level.
Design
Cross‐sectional design.
Setting
Barcelona, Spain.
Participants
All residents aged ⩾20 years. All AIDS‐related deaths occurring between 1991 and 2001 were studied. The individual variables analysed were age, sex, educational level, neighbourhood of residence and HIV transmission group. Male unemployment was used as the community‐level indicator of neighbourhood deprivation. Multilevel Poisson regression models were fitted to estimate the relationship between AIDS mortality and the individual‐ and community‐level variables.
Results
At the individual level, AIDS mortality relative risks (RR) were higher among intravenous drug users (IDUs) with lower educational level in both periods. For the younger population, the RR of AIDS‐related mortality associated with having little education compared with having a primary education or more was 4.7 (95% CI 3.6 to 6.1) in men and 5.2 (95%CI 3.6 to 7.7) in women in the pre‐HAART period, and 4.7 (95% CI 2.7 to 8.1) in men and 4.5 (95% CI 1.4 to 14.1) in women in the post‐HAART period. At the community level, an area effect in AIDS mortality was found, which was more important in neighbourhoods having high deprivation in both periods, although the effect was most important in the post‐HAART period.
Conclusions
This study has shown inequalities in AIDS mortality in terms of both individual variables and a community‐level variable in the pre‐HAART as well as in the post‐HAART period. These socioeconomic inequalities of AIDS mortality must be considered when prevention and treatment strategies are implemented.
Social factors are critical to understanding infectious disease patterns.1 HIV infection and AIDS have been related to socioeconomic position and to social and material deprivation, such as poverty, use of drugs, prostitution and immigration, both before and after the introduction of highly active antiretroviral therapy (HAART).2,3 AIDS concentrates in the socially most vulnerable groups and poorest countries.4 Several studies have shown that AIDS mortality is higher in areas with greater neighbourhood deprivation than in other areas and in people belonging to disadvantaged socioeconomic levels before the introduction of HAART5,6,7,8 as well after.9,10
Recently, a study reviewed the social epidemiology of AIDS, identifying three levels of determinants of HIV/AIDS vulnerability: (1) individual factors that include biological, demographic and behavioural risk factors as well as socioeconomic position; (2) social‐level factors that include neighbourhood effects, social networks, cultural context and so on; and (3) structural factors that include structural violence and discrimination (eg, racism, sexism, classism), legal structures, demographic change and the political environment.1
Southern European countries, such as Spain, are among the countries with the highest AIDS rates in Europe, mainly owing to AIDS acquired by drug users through sharing of drug‐injection paraphernalia.11 Spain has a National Health System and access to health services and HAART has been free for everyone since 1996.
Although several studies have analysed socioeconomic inequalities in AIDS mortality, none of them have used multilevel models to study individual as well as contextual effects. Therefore, our objective was to study socioeconomic inequalities in AIDS mortality in Barcelona for the periods 1991–6 (pre‐HAART) and 1997–2001 (post‐HAART), taking into account individual and community effects of socioeconomic level.
Methods
Design and study population
Barcelona, the second largest city in Spain (1 600 000 inhabitants), is located on the northeastern coast. The study used a cross‐sectional design, including all Barcelona residents aged ⩾20 years. All AIDS‐related deaths included in the mortality register, which occurred among these residents between 1991 and 2001, were included. This mortality register has a high degree of completeness, including all deaths of residents in the city. The underlying causes of death were coded using the International Classification of Diseases—9th revision until 1999, and the codes attributed to AIDS/HIV in Spain were 279.5 (AIDS) and 795.8 (HIV without other specified causes). After 1999, the codes used were B20–B24 of the International Classification of Diseases—10th revision.
The educational level and the neighbourhood of the deceased were obtained through a record linkage between the mortality register and the municipal census (87.4% of cases were linked), and transmission group was obtained through a record linkage with the AIDS cases register of Barcelona (85.6% of cases were linked). These are probabilistic linkages based on the name, the surname and date of birth of the deceased.12
Information on the population regarding age, sex, the highest completed level of education and neighbourhood of residence comes from the 1991, 1996 and 2003 Municipal Census, an administrative register not subject to statistical secrecy. To obtain the populations at risk for the periods 1991–6 (pre‐HAART) and 1997–2001 (post‐HAART), estimations of the intercensal population for the years 1993 (for the 1991–6 period) and 1999 (for the 1997–2001 period) were obtained based on a geometric curve. Every resident in Barcelona is registered in the municipal census, which is continually updated to incorporate data on migration, births and deaths.
Variables and indicators analysed
The individual variables studied were age, sex, highest completed level of studies (educational level), neighbourhood of residence at the moment of death and HIV transmission group.
Educational level was grouped into illiterate or no education (0–4 years of schooling), primary education not finished (5–6 years of schooling) and more than primary studies finished (⩾7 years of schooling).
Three HIV transmission groups were studied: (1) homosexual/bisexual: includes men with homosexual and bisexual practices who were not injecting drug users (IDUs); (2) heterosexual/other: includes men with heterosexual practices not IDUs, all women not IDUs, and men and women with other risk factors (eg, blood transmission) who were not IDUs; and (3) IDUs: includes all men and women IDUs. We studied two age groups: 20–39 and ⩾40 years. For IDUs, the second age group was 40–49 years because there were very few deaths in those older than 49 years.
Barcelona has 38 neighbourhoods, their populations varying, in 1996, between 1081 and 95 382 inhabitants (mean 39 705 inhabitants per neighbourhood). As a deprivation indicator of the neighbourhood, we used the 1991 and 1996 male unemployment rates (men actively looking for work divided by the total men in the labour market >16 years) obtained from the 1991 and 1996 censuses.
Data analysis
All analyses were carried out separately for men and women, for each AIDS transmission group and for two periods: 1991–6 (pre‐HAART) and 1997–2001 (post‐HAART). Age‐specific AIDS mortality rates were calculated for each educational level.
Multilevel models allow the simultaneous examination of the effects of group and individual‐level variables on individual‐level outcomes.13 Multilevel Poisson regression models were fitted using data grouped by age, educational level and neighbourhood using the hierarchical linear and non‐linear modelling statistical program.14 The dependent variable was the logarithm of the AIDS mortality rate. The models were structured at two levels: at the first level, we took into account individual variables (age and educational level groups) and at the second level, the community‐level variable (male unemployment or deprivation). The effect of educational level was separated by age group because of the interactions observed in age‐specific death rates. To estimate these models, we included all the cases with no missing values in any variable (n = 2250, 87.4% of all AIDS‐related deaths and n = 1946, 75.6% for transmission groups). Because the relationship between mortality and male unemployment was exponential, we decided to categorise the male unemployment in quintiles.
These models estimate the relationship between individual (age and educational level) and neighbourhood variables and AIDS mortality. The steps in the construction of the models are as follows (1) study the differences in mortality among neighbourhoods (a multilevel model—empty model—with only a random parameter that is the constant); (2) include individual variables (age and educational level); and (3) include deprivation of the neighbourhood. Moreover, we have included the values of the second‐level variations of each of these models, the proportional change in these variances and the median relative risk (RR), a measure used to quantify the variation among neighbourhoods (the higher the median RR, the higher the between‐neighbourhoods variation).15
Results
Description of the population and AIDS mortality rates
During the 11‐year period studied, 2087 AIDS‐related deaths were reported among men (1669 pre‐HAART and 418 post‐HAART) and 488 among women (379 pre‐HAART and 109 post‐HAART; table 1). More than half of those who died were <40 years of age. IDU was the most frequent transmission group. One third of the cases had less than primary studies. Neighbourhood male unemployment ranged from 5.5% to 22.8% in 1991 and from 8.5% to 32% in 1996.
Table 1 Number of AIDS‐related deaths and percentage by age, transmission group and educational level.
| Variables | Pre‐HAART | Post‐HAART | ||||||
|---|---|---|---|---|---|---|---|---|
| Men | % | Women | % | Men | % | Women | % | |
| Age groups (years) | ||||||||
| 20–29 | 279 | 16.7 | 130 | 34.3 | 26 | 6.2 | 12 | 11.1 |
| 30–39 | 819 | 49.1 | 179 | 47.2 | 202 | 48.3 | 64 | 58.7 |
| 40–49 | 349 | 20.9 | 37 | 9.8 | 101 | 24.2 | 20 | 18.3 |
| 50–59 | 132 | 7.9 | 19 | 5 | 50 | 12 | 6 | 5.5 |
| ⩾60 | 90 | 5.4 | 14 | 3.7 | 39 | 9.3 | 7 | 6.4 |
| Transmission group | ||||||||
| IDU | 765 | 45.8 | 205 | 54.1 | 182 | 43.5 | 56 | 51.4 |
| Homosexual and bisexual | 562 | 33.7 | — | — | 74 | 17.7 | — | — |
| Heterosexual and other | 149 | 8.9 | 131 | 34.6 | 56 | 13.4 | 24 | 22 |
| Missing data | 193 | 11.6 | 43 | 11.3 | 106 | 25.4 | 29 | 26.6 |
| Educational level | ||||||||
| Illiterate and no education | 151 | 9 | 49 | 12.9 | 45 | 10.8 | 13 | 11.9 |
| Primary not finished | 521 | 31.2 | 137 | 36.2 | 148 | 35.4 | 47 | 43.2 |
| Primary finished, secondary and university | 777 | 46.6 | 154 | 40.6 | 176 | 42.1 | 43 | 39.4 |
| Missing data | 220 | 13.2 | 39 | 10.3 | 49 | 11.7 | 6 | 5.5 |
| Total | 1669 | 100 | 379 | 100 | 418 | 100 | 109 | 100 |
HAART, highly active antiretroviral therapy; IDU, injecting drug user.
Barcelona, men and women, in the pre‐HAART (1991–1996) and post‐HAART (1997–2001) periods.
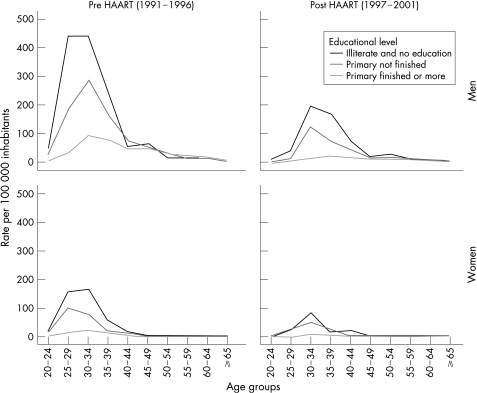
Figure 1 shows age‐specific AIDS mortality rates for men and women in the pre‐HAART and post‐HAART periods. For the groups aged between 20 and 39 years, AIDS mortality rates varied with educational level and sex. Rates were higher in the lowest educational level group, in men and in the pre‐HAART period. For example, in the pre‐HAART period the 30–34 year age‐group rates for men were 442.8/100 000 inhabitants in those who were illiterate or had no education, 286.2 in those with primary education not finished and 92.3 in those who had completed more than primary studies. For women, the corresponding rates were 166.1, 79.5 and 23.3. Educational level inequalities in death rates fell with increasing age. This pattern was similar to that observed in the post‐HAART period, although the rates were smaller.
Figure 1 AIDS‐related mortality by age and educational level. (age‐specific per 100 000 inhabitants). Barcelona, men and women, in the pre‐highly active antiretroviral therapy (HAART) (1991–6) and post‐HAART (1997–2001) periods.
Multilevel models
Tables 2 and 3 show, respectively, for men and women, the results of the multilevel models for the pre‐HAART (1991–6) and post‐HAART (1997–2001) periods. At the individual level, for total AIDS‐related deaths in the 20–39 year age group, the RR among those having no education compared with those having primary studies or more was 4.7 in the pre‐HAART period (95% CI 3.6 to 6.1) in men, and 5.2 (95% CI 3.6 to 7.7) in women, and 4.7 in the post‐HAART period (95% CI 2.7 to 8.1) in men and 4.5 (95% CI 1.4 to 14.1) in women. This pattern was the same in all the transmission groups, in men as well in women, and in the two periods, although RR for male IDUs having no education was higher in the post‐HAART period.
Table 2 Multilevel associations between AIDS‐related mortality and individual‐(educational level and age group) and community‐level (neighbourhood deprivation) effects by transmission groups in men.
| Independent variables and neighbourhood variability | IDUs | Homosexual/bisexual | Heterosexual/other | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | RR | 95% CI | n | RR | 95% CI | n | RR | 95% CI | n | RR | 95% CI | |
| Pre‐HAART (1991–6) | ||||||||||||
| 20–39‐year age group | ||||||||||||
| Illiterate and no education | 50 | 4.30 | 3.08 to 6 | 10 | 2.48 | 1.47 to 4.17 | 5 | 5.1 | 1.6 to 16.28 | 76 | 4.69 | 3.63 to 6.07 |
| Primary not finished | 260 | 3.21 | 2.74 to 3.75 | 44 | 1.38 | 1.04 to 1.83 | 15 | 1.99 | 0.98 to 4.04 | 354 | 2.81 | 2.54 to 3.12 |
| Primary finished or more | 297 | 1 | 151 | 1 | 30 | 1 | 525 | 1 | ||||
| ⩾40‐year age group* | ||||||||||||
| Illiterate and no education | 7 | 1.84 | 0.75 to 4.52 | 35 | 0.66 | 0.45 to 0.96 | 20 | 0.84 | 0.51 to 1.38 | 74 | 0.57 | 0.43 to 0.77 |
| Primary not finished | 36 | 3.07 | 1.77 to 5.31 | 88 | 0.93 | 0.79 to 1.1 | 23 | 0.66 | 0.41 to 1.06 | 166 | 0.86 | 0.72 to 1.04 |
| Primary finished or more | 20 | 1 | 157 | 1 | 43 | 1 | 251 | 1 | ||||
| Neighbourhood deprivation† | ||||||||||||
| 1, Most deprived | 3.99 | 2.56 to 6.21 | 2.31 | 1.07 to 4.97 | 3.75 | 2.6 to 5.41 | 3.13 | 2.10 to 4.66 | ||||
| 2 | 1.54 | 1.02 to 2.33 | 0.75 | 0.38 to 1.45 | 1.19 | 0.86 to 1.65 | 1.15 | 0.80 to 1.66 | ||||
| 3 | 1.11 | 0.73 to 1.68 | 0.89 | 0.47 to 1.68 | 1.21 | 0.87 to 1.68 | 1.01 | 0.71 to 1.42 | ||||
| 4 | 1.03 | 0.71 to 1.5 | 1.12 | 0.59 to 2.11 | 0.78 | 0.51 to 1.2 | 1.02 | 0.73 to 1.44 | ||||
| 5, Least deprived | 1 | 1 | 1 | 1 | ||||||||
| Variability | p Value | Variability | p Value | Variability | p Value | Variability | p Value | |||||
| Neighbourhood variability | 0.0428 | 0.062 | 0.3085 | <0.001 | <0.001 | >0.5 | 0.0583 | <0.001 | ||||
| Post‐HAART (1997–2001) | ||||||||||||
| 20–39‐year age group | ||||||||||||
| Illiterate and no education | 15 | 7.99 | 4.24 to 15.05 | 3 | 4.94 | 1.3 to 18.78 | 0 | 0‡ | 0 to ∞‡ | 19 | 4.68 | 2.72 to 8.07 |
| Primary not finished | 59 | 3.96 | 2.41 to 6.5 | 4 | 0.95 | 0.25 to 3.61 | 5 | 2.28 | 0.67 to 7.82 | 86 | 3.02 | 1.88 to 4.86 |
| Primary finished or more | 52 | 1 | 14 | 1 | 7 | 1 | 89 | 1 | ||||
| ⩾40‐year age group* | ||||||||||||
| Illiterate and no education | 4 | 2.35 | 0.7 to 7.90 | 6 | 0.84 | 0.32 to 2.2 | 4 | 0.69 | 0.21 to 2.22 | 26 | 0.82 | 0.5 to 1.33 |
| Primary not finished | 13 | 1.48 | 0.59 to 3.71 | 14 | 0.86 | 0.48 to 1.56 | 14 | 1.11 | 0.49 to 2.51 | 60 | 0.93 | 0.65 to 1.34 |
| Primary finished or more | 17 | 1 | 25 | 1 | 18 | 1 | 84 | 1 | ||||
| Neighbourhood deprivation† | ||||||||||||
| 1, Most deprived | 11.56 | 5.19 to 25.77 | 8.60 | 3.58 to 20.63 | 8.10 | 3.3 to 19.86 | 11.39 | 6.39 to 20.28 | ||||
| 2 | 5.75 | 2.65 to 12.51 | 1.66 | 0.64 to 4.34 | 1.20 | 0.48 to 3 | 3.17 | 1.96 to 5.12 | ||||
| 3 | 2.35 | 0.98 to 5.68 | 1.81 | 0.68 to 4.86 | 0.73 | 0.24 to 2.21 | 1.74 | 0.96 to 3.16 | ||||
| 4 | 1.64 | 0.73 to 3.67 | 1.58 | 0.54 to 4.57 | 0.77 | 0.34 to 1.72 | 1.38 | 0.76 to 2.52 | ||||
| 5, Least deprived | 1 | 1 | 1 | 1 | ||||||||
| Variability | p Value | Variability | p Value | Variability | p Value | Variability | p Value | |||||
| Neighbourhood variability | <0.001 | >0.5 | <0.001 | 0.269 | <0.001 | 0.459 | 0.0687 | 0.058 | ||||
HAART, highly active antiretroviral therapy; IDUs, injecting drug users.
Barcelona, in the pre‐HAART (1991–1996) and post‐HAART (1997–2001) periods.
*IDUs 40–49‐year age group.
†Percentage male unemployment.
‡The number of cases in the socioeconomic group is 0.
Table 3 Multilevel associations between AIDS‐related mortality and individual‐(educational level and age group) and community‐level‐(neighbourhood deprivation) effects by transmission groups in women.
| Independent variables and neighbourhood variability | IDUs | Heterosexual/other | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | RR | 95% CI | n | RR | 95% CI | n | RR | 95% CI | |
| Pre‐HAART (1991–6) | |||||||||
| 20–39‐year age group | |||||||||
| Illiterate and no education | 18 | 5.35 | 3.16 to 9.05 | 6 | 3.80 | 1.46 to 9.87 | 28 | 5.23 | 3.56 to 7.67 |
| Primary not finished | 75 | 3.58 | 2.71 to 4.73 | 30 | 2.96 | 1.83 to 4.77 | 109 | 3.20 | 2.41 to 4.27 |
| Primary finished or more | 80 | 1 | 43 | 1 | 140 | 1 | |||
| ⩾40‐year age group* | |||||||||
| Illiterate and no education | 2 | 3.13 | 0.44 to 22.15 | 15 | 1.56 | 0.72 to 3.37 | 20 | 1.31 | 0.63 to 2.74 |
| Primary not finished | 8 | 4.79 | 1.11 to 20.62 | 18 | 1.53 | 0.96 to 2.43 | 28 | 1.59 | 1.01 to 2.51 |
| Primary finished or more | 2 | 1 | 10 | 1 | 14 | 1 | |||
| Neighbourhood deprivation† | |||||||||
| 1, Most deprived | 5.71 | 2.92 to 11.15 | 4.23 | 2.48 to 7.22 | 5.32 | 3.22 to 8.8 | |||
| 2 | 2.49 | 1.19 to 5.22 | 0.94 | 0.51 to 1.72 | 1.80 | 1.07 to 3.02 | |||
| 3 | 1.48 | 0.76 to 2.91 | 1.27 | 0.74 to 2.15 | 1.44 | 0.9 to 2.33 | |||
| 4 | 2.18 | 1.09 to 4.38 | 0.57 | 0.19 to 1.73 | 1.34 | 0.73 to 2.45 | |||
| 5, Least deprived | 1 | 1 | 1 | ||||||
| Variability | p Value | Variability | p Value | Variability | p Value | ||||
| Neighbourhood variability | <0.001 | >0.5 | <0.001 | 0.003 | 0.1274 | <0.001 | |||
| Post‐HAART (1997–2001) | |||||||||
| 20–39‐year age group | |||||||||
| Illiterate and no education | 2 | 2.84 | 0.54 to 14.97 | 2 | 9.06 | 1.85 to 44.42 | 5 | 4.48 | 1.42 to 14.1 |
| Primary not finished | 23 | 4.99 | 2.73 to 9.11 | 6 | 4.02 | 1.37 to 11.79 | 35 | 4.90 | 3.08 to 7.8 |
| Primary finished or more | 19 | 1 | 8 | 1 | 32 | 1 | |||
| ⩾40‐year age group* | |||||||||
| Illiterate and no education | 3 | 7.81 | 1.53 to 39.8 | 1 | 1.54 | 0.07 to 31.78 | 6 | 0.73 | 0.27 to 1.99 |
| Primary not finished | 3 | 1.84 | 0.47 to 7.15 | 3 | 3.19 | 0.2 to 50.07 | 12 | 1.07 | 0.41 to 2.81 |
| Primary finished or more | 3 | 1 | 1 | 1 | 11 | 1 | |||
| Neighbourhood deprivation† | |||||||||
| 1, Most deprived | 20.75 | 5.12 to 84.16 | 3.27 | 0.67 to 16 | 6.69 | 4.23 to 10.59 | |||
| 2 | 2.04 | 0.46 to 9.11 | 1.57 | 0.32 to 7.62 | 0.94 | 0.59 to 1.5 | |||
| 3 | 2.56 | 0.57 to 11.54 | 1.15 | 0.18 to 7.36 | 1.20 | 0.51 to 2.82 | |||
| 4 | 2.94 | 0.68 to 12.69 | 2.13 | 0.45 to 9.99 | 1.10 | 0.63 to 1.92 | |||
| 5, Least deprived | 1 | 1 | 1 | ||||||
| Variability | p Value | Variability | p Value | Variability | p Value | ||||
| Neighbourhood variability | <0.001 | >0.5 | <0.001 | 0.251 | <0.001 | >0.5 | |||
HAART, highly active antiretroviral therapy; IDU, injecting drug user.
Barcelona, in the pre‐HAART (1991–6) and post‐HAART (1997–2001) periods.
*IDUs 40–49‐year age group.
†Percentage male unemployment.
Among the second age group—that is, those aged >40 years (40–49 years in IDUs)—only IDUs had an RR higher among people with primary education not finished in the pre‐HAART period (RR 3.1; 95% CI 1.8 to 5.3 in men and RR 4.8; 95% CI 1.1 to 20.6 in women) and among women with the lowest education level in the post‐HAART period (RR 7.8; 95% CI 1.5 to 39.8 in women with no education). The homosexual/bisexual subjects of this age group with the lowest educational level presented RR <1, being significant in the pre‐HAART period (RR 0.66; 95% CI 0.45 to 0.96). The heterosexual transmission group aged >40 years did not present statistically significant differences.
Even after controlling for individual educational level and age group, variability between the neighbourhoods persisted (table 4). When the percentage of neighbourhood deprivation was introduced at the second level of the model, the variability diminished, ceasing to be important among the IDUs and the male heterosexual/other group in the pre‐HAART period and in all the transmission groups in the post‐HAART period. It is worth mentioning that in the pre‐HAART period, among the female heterosexual and homosexual/bisexual transmission groups, the second‐level variance in the model was higher than in the other transmission groups. This fact shows that the variability in neighbourhood death rates is not completely explained by the variables included in the model.
Table 4 Second‐level variances (σj2), proportional change in variances and the median rate ratio, for each of these models: (1) empty model, (2) only the individual variables, and (3) individual variables and neighbourhood deprivation.
| IDUs | Homosexuals/bisexuals | Heterosexuals | Total | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| rj2 | p Value | PCV | MRR | rj2 | p Value | PCV | MRR | rj2 | p Value | PCV | MRR | rj2 | p Value | PCV | MRR | |
| Pre‐HAART (1991–6) | ||||||||||||||||
| Men | ||||||||||||||||
| Model 1 (empty) | 0.36 | <0.001 | 1.77 | 0.38 | <0.001 | 1.8 | 0.17 | 0.027 | 1.49 | 0.25 | <0.001 | 1.61 | ||||
| Model 2 (individual variables) | 0.28 | <0.001 | 20.67 | 1.66 | 0.42 | <0.001 | −11.87 | 1.86 | 0.19 | 0.004 | −14.37 | 1.53 | 0.24 | <0.001 | 4.8 | 1.59 |
| Model 3 (community‐level variable) | 0.04 | 0.062 | 88.06 | 1.22 | 0.31 | <0.001 | 18.76 | 1.7 | <0.01 | >0.5 | 100 | 1 | 0.06 | <0.001 | 76.38 | 1.26 |
| Women | ||||||||||||||||
| Model 1 (empty) | 0.17 | 0.144 | 1.48 | 0.56 | <0.001 | 2.04 | 0.37 | <0.001 | 1.79 | |||||||
| Model 2 (individual variables) | 0.31 | <0.001 | −84.3 | 1.7 | 0.85 | <0.001 | −50.49 | 2.4 | 0.45 | <0.001 | −20.77 | 1.9 | ||||
| Model 3 (community‐level variable) | <0.01 | >0.5 | 99.99 | 1 | <0.01 | 0.003 | 100 | 1 | 0.13 | <0.001 | 65.81 | 1.41 | ||||
| Post‐HAART (1997–2001) | ||||||||||||||||
| Men | ||||||||||||||||
| Model 1 (empty) | 0.57 | 0.001 | 2.06 | 0.48 | 0.025 | 1.93 | 1.04 | <0.001 | 2.64 | 0.77 | <0.001 | 2.31 | ||||
| Model 2 (individual variables) | 0.47 | <0.001 | 17.76 | 1.92 | 0.89 | <0.001 | −85.37 | 2.45 | 1.05 | <0.001 | −0.87 | 2.65 | 0.75 | <0.001 | 2.6 | 2.28 |
| Model 3 (community‐level variable) | <0.01 | >0.5 | 100 | 1 | <0.01 | 0.269 | 100 | 1 | <0.01 | 0.459 | 100 | 1 | 0.07 | 0.058 | 91.07 | 1.28 |
| Women | ||||||||||||||||
| Model 1 (empty) | 0.83 | 0.007 | 2.38 | <0.01 | >0.5 | 1 | 0.61 | 0.003 | 2.1 | |||||||
| Model 2 (individual variables) | 0.82 | <0.001 | 0.88 | 2.37 | <0.01 | >0.5 | 100 | 1 | 0.61 | <0.001 | −1.14 | 2.11 | ||||
| Model 3 (community‐level variable) | <0.01 | >0.5 | 100 | 1 | <0.01 | 0.251 | 100 | 1 | <0.01 | >0.5 | 100 | 1 | ||||
HAART, highly active antiretroviral therapy; IDUs, injecting drug users; MRR, median rate ratio; PCV, proportional change in variances.
Barcelona, men and women, in the pre‐HAART (1991–1996) and post‐HAART (1997–2001) periods.
The higher the neighbourhood deprivation, the higher the RR, the increase being non‐linear. For example, among IDUs, the RR was 4 (95% CI 2.6 to 6.2) in men and 5.7 (95% CI 2.9 to 11.2) in women, in the neighbourhoods with the highest deprivation compared with those with the lowest in the pre‐HAART period. The RR between neighbourhoods increased in the post‐HAART period. For example, among IDUs, the RR was 11.6 (95% CI 5.2 to 25.8) in men and 20.8 (95% CI 5.1 to 84.2) in women, in the neighbourhoods with the highest deprivation compared with those with the lowest in the post‐HAART period. This pattern was similar across the various other transmission groups.
Discussion
Individual‐ and community‐level effects matter
This study has shown that there are inequalities in AIDS mortality in terms of individual variables (educational level, age and sex), as well as in terms of a community‐level variable (deprivation of the neighbourhood) before and after the introduction of HAART in a Spanish city where there is a National Health System and HAART is free. We are not aware of any similar studies trying to simultaneously ascertain the effects of contextual deprivation and individual variables in AIDS‐related mortality, which shows that apart from individual socioeconomic level, the area deprivation also has an effect. Moreover, inequalities in educational level are more important in the young population than in the older groups. AIDS‐related mortality also increases with neighbourhood deprivation in a non‐linear manner, that is, it increases the most in the areas with highest deprivation and mainly in the post‐HAART period. The pattern of AIDS‐related mortality among IDUs shows rates higher in men than in women, and also in people with low educational level in both periods, as well as in deprived neighbourhoods. In the homosexual/bisexual and heterosexual transmission groups, educational‐level inequalities were important in the young population, but not in older groups, in both periods.
This study complements other studies carried out in Barcelona. One reported social inequalities in the distribution of AIDS incidence among the neighbourhoods of the city before the HAART period (ecological design). The inequality pattern was different in the different transmission categories: material and social deprivation was related to AIDS in IDUs and heterosexual contacts, but they were inversely related to homosexual/bisexual contacts.16 Another study tried to determine whether AIDS mortality before and after the introduction of HAART had increased or decreased differentially by socioeconomic group, and found that although AIDS mortality evolved differently for different socioeconomic groups (increasing and decreasing more in lower socioeconomic groups), the pattern of inequalities in AIDS mortality by socioeconomic group remained stable, in the sense that lower socioeconomic groups had higher mortality than the more privileged ones, and inequalities did not change after the introduction of HAART.17 This study adds the complementary view offered by multilevel analyses.
The individual effect
Fewer studies have been conducted using individual variables (eg, social class, educational level), before as well as after HAART. For example, an interview‐based study, carried out in 1993, of men and women diagnosed with AIDS in 11 US states found that the lower the educational level and social class, the higher the incidence of AIDS, which was also higher among unemployed people.7 A study carried out in Brazil described how AIDS incidence rates increased more, between 1991–4 and 1995–8, in people of low socioeconomic level, changing the pattern of the disease by socioeconomic status (although the prevalence was still higher among higher socioeconomic groups).8 Regidor et al18 examined the association between education and mortality from specific causes of death in Madrid, Spain, in 1996–7 after the introduction of HAART, finding that people of low educational level had higher AIDS mortality.
Probably, the educational‐level inequalities found in this study are related to different factors, taking into account that AIDS mortality is related to the incidence of AIDS and to disease progression after HIV infection. Before HAART, inequalities in AIDS mortality were due to inequalities in factors related to HIV infection and the incidence of AIDS, because the disease was lethal (such as lifestyle and health‐related behaviours). In southern Europe, these behaviours are related to the use of drugs, such as sharing needles or risky sexual behaviours. Most IDUs with low socioeconomic level are a marginalised group, concentrated in deprived inner‐city neighbourhoods, who acquire AIDS through sharing drug‐injection paraphernalia and sexual contacts.19
Since the introduction of HAART,20 AIDS has become a chronic disease and other factors now help to explain educational‐level inequalities. The first factor is the lack of access to treatment for disadvantaged people,21 even though Spain has a National Health System and the treatment is free. In this sense, one Spanish study has reported that 8.4% of IDUs have not had an HIV test, and that 36.8% of IDUs who are HIV positive have never taken HAART.19 Although in this study it was not possible to investigate differences in plasma viral load, CD4 cell count, comorbidity or resistance to treatment between different socioeconomic groups, because these variables were not available, a study conducted in British Columbia (Canada) found that socioeconomic status was strongly associated with HIV‐related mortality in the HAART period, after adjusting for all these variables. One possible explanation of this perhaps is that individuals of lower socioeconomic groups were less likely to receive triple therapy.22 Second, there are differences in adherence to treatments between people of different educational levels: because HAART is a long and complex treatment,23 people of low educational level may have more difficulties in following it. Third, comorbidity may also play a role: the presence of other diseases mainly in the lowest educational level groups, such as hepatitis C, may affect HIV prognosis.20
In our study, the RR of death due to AIDS, between educational levels, decreased at older ages and was even inversely related to educational level in the homosexual/bisexual transmission groups >40 years in the first period. The higher RR among people in disadvantaged social classes at younger ages has also been reported previously. Various explanations have been offered. First, the survival advantage of people of privileged social classes implying that some individuals of the most disadvantaged group could die before reaching old age. Second, illiteracy denotes a worse socioeconomic situation in young people than in older people, as nowadays access to basic education is far greater.24,25,26 The results found in the homosexual/bisexual group at older ages (higher mortality among high educational level) could be explained, apart from the reasons mentioned above, by the manner of acquiring and dying from AIDS over time. In this sense, the inverse relationship found reflects the pattern that existed at the beginning of the epidemic.
Another aspect to be mentioned is sex differences. Absolute differences between educational levels, with respect to AIDS mortality, are more important in men. Our previous study on AIDS mortality trends showed that for the lowest socioeconomic group of the heterosexual transmission group, rates were higher and increased more for women than for men.17 Zierler and Krieger27 have highlighted the necessity of studying women's experiences with discrimination and subordination (related to their lack of power) to understand sex differences in the epidemic. In this sense, in a deprived socioeconomic situation, many women with low self‐esteem have trouble negotiating safe sexual practices with their infected partners,19,28 having more possibilities to acquire AIDS. Therefore, increasing AIDS among heterosexual women has to be carefully surveyed and studied.
The community‐level effect
A multilevel approach such as that used in this study permits the effect of contextual deprivation to be investigated, adjusting for individual socioeconomic level.29
We measured neighbourhood deprivation by area male unemployment because this indicator has been reported to be one of the best measures of deprivation in our country,30,31 and has been used in the majority of deprivation indexes constructed.32 We have found an area effect in AIDS mortality, which is much more important in neighbourhoods of high unemployment: those in the centre of the city where there is a concentration of marginalised populations, poverty, drug use and social unrest. Also, this marginality could increase because of the fact that these neighbourhoods concentrate most of the resources focused on these groups. All these characteristics may influence the incidence of AIDS and AIDS mortality, apart from individual socioeconomic level. This non‐linear relationship between neighbourhood deprivation and AIDS mortality has been described previously at an ecological level.31,33 Moreover, it has to be mentioned that the RR of death related to deprivation was higher in the post‐HAART period.
The cross‐sectional design of our study cannot discard residential mobility (people with AIDS moving to deprived neighbourhoods) and also taking into account the highest level of resources in deprived areas. We tried to study residential mobility from two points of view. First, when we compared the neighbourhood from the mortality register (census based) with the neighbourhood in the registry of AIDS cases (self‐reported), the agreement between them was very high (κ = 0.81). Second, we studied the AIDS‐related deaths that were included in the census at the moment of registering the death (implying that these people were not included in the municipal census before dying). In total, they represented 6.4% of deaths, a percentage that did not change in the five groups of neighbourhoods included in this study (groups defined by the level of deprivation). Both facts oppose residential mobility as an explanation of the results found.
Other papers have reported inequalities in AIDS mortality at the area level, before and after the introduction of HAART. For example, one study compared AIDS cases between 20 US counties with the largest proportional increases in incidence rates of AIDS and 20 US counties with the smallest increases. Counties with the largest increases in the incidence of AIDS had lower levels of income, education and literacy.34 Zierler et al5 described how the incidence of AIDS before the HAART period in census blocks of the state of Massachusetts (USA) increased with economic deprivation of the small areas. Wallace9 showed that decreases in AIDS mortality after the introduction of HAART in areas of New York (USA), defined by zip code, were related to an array of socioeconomic and community stress variables, the areas with indicators of less deprivation (white population, college degree, higher income) having a greater decrease, whereas more deprived areas had a smaller decrease. In San Franciso (USA),35 people living in poorer neighbourhoods had poorer AIDS survival in the HAART period.35 A study carried out in Rome (Italy)10 described how after the introduction of HAART treatment (1996–7), the risk of death was greater for people with lower neighbourhood socioeconomic status, after having adjusted for age, sex, intravenous drug use, CD4 cell count diagnosis, AIDS defining disease and hospital diagnosis. The explanations that the authors discuss are related to poor healthcare access, medical management or poor adherence to treatment.
Policy implications
This study has shown that there are inequalities in AIDS mortality in terms of individual variables as well as a community‐level variable both before and after the introduction of highly active antiretroviral therapy (HAART).
These socioeconomic inequalities in AIDS mortality must be considered when prevention and treatment strategies are implemented.38,39,40,41
These strategies should be targeted to the whole population and particularly to the most deprived neighbourhoods.
Although Barcelona had programmes designed to assist drug users,42 recently, a drug consumption room has been opened in the most deprived area of the city, where drug users can be offered methadone maintenance programmes, syringe exchange and direct treatment of AIDS and other diseases. Therefore, the services offered can reduce the acquisition of AIDS and also the mortality of this disease among this population.
The community‐level effect before HAART found in our study can be related to the higher incidence rates of AIDS in these neighbourhoods, which are related to the higher percentages of marginalised populations and drug users. The increase in the community‐level effect in the post‐HAART period can be explained by the lower access and adherence to HAART in the population living in areas with more deprivation. Probably, this fact is related to the marginalisation of this population, implying that apart from educational level, other factors related to poverty and living conditions are important. In this sense, as has been stated before, a high percentage of IDUs who are HIV positive have never taken HAART.19
Limitations
One of the limitations of this study is that we only included death from AIDS as the underlying cause of death in the mortality register. In the pre‐HAART period, most deaths of people with AIDS were AIDS related, this cause of death having high validity,36 but after the introduction of HAART the causes of death have changed among HIV‐infected individuals, diminishing the AIDS‐related deaths as has been described by other authors.37 We have to take into account that this study did not consider deaths due to other causes. A second limitation is that it is not possible to obtain as part of the population at risk, IDUs and members of the homosexual/bisexual population of Barcelona. For this reason, we used the population of Barcelona as the denominator of AIDS mortality. A third limitation is the presence of some missing values in our variables (table 1), even though these missing values were not related to the other variables, except in the HIV transmission group, which had more missing values for the years 2000 and 2001. Because of this fact, not including missing values does not bias our estimations. Finally, it is necessary to mention the low number of cases in the post‐HAART period, mainly in women.
What this paper adds
Social factors are critical to understanding infectious disease patterns.
Several studies have shown that AIDS mortality is higher in areas with greater neighbourhood deprivation and in people belonging to disadvantaged socioeconomic groups, before the introduction of highly active antiretroviral therapy (HAART) as well as after.
This study has shown that there are inequalities in AIDS mortality in terms of individual and community‐level variables using a multilevel approach.
Apart from individual socioeconomic level, area deprivation also has an effect, which is more important after the introduction of HAART than before.
Acknowledgements
This study was partially funded by the Red de Centros de Investigación en Epidemiología y Salud Pública of the Fondo de Investigaciones Sanitarias (FISS C03/09) and by a grant from the Fundación para la investigación y la prevención del SIDA en España (grant number 2425/01).
Abbreviations
HAART - highly active antiretroviral therapy
IDU - injecting drug user
Footnotes
Competing interests: None declared.
References
- 1.Poundestone K E, Strathdee S A, Celentano D D. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev 20042622–35. [DOI] [PubMed] [Google Scholar]
- 2.Wallace R, Fullilove M, Fullilove R.et al Will AIDS be contained within US minority urban populations? Soc Sci Med 1994391051–1062. [DOI] [PubMed] [Google Scholar]
- 3.Fournier A M, Carmichael C. Socioeconomic influences on the transmission of human immunodeficiency virus infection. The hidden risk. Arch Fam Med 19987214–217. [DOI] [PubMed] [Google Scholar]
- 4.Moatti J P, Souteyrand Y. AIDS social and behavioral research: past advances and thoughts about the future [editorial]. Soc Sci Med 2000501519–1532. [DOI] [PubMed] [Google Scholar]
- 5.Zierler S, Krieger N, Tang Y.et al Economic deprivation and AIDS incidence in Massachusetts. Am J Public Health 2000901064–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borrell C, Pasarín M I, Plasència A.et al Widening inequalities in mortality: the case of a southern European city (Barcelona). J Epidemiol Community Health 199751659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diaz T, Chu S Y, Buchler J W.et al Socioeconomic differences among people with AIDS: results from a multistate surveillance project. Am J Prev Med 199410217–222. [PubMed] [Google Scholar]
- 8.Fonseca M G, Travassos C, Bastos F I.et al Social distribution of AIDS in Brazil, according to labor market participation, occupation and socioeconomic status of cases from 1987 to 1998. Cad Saude Publica 2003191351–1363. [DOI] [PubMed] [Google Scholar]
- 9.Wallace R G. AIDS in the HAART era: New York's heterogeneous geography. Soc Sci Med 2003561155–1171. [DOI] [PubMed] [Google Scholar]
- 10.Rapiti E, Porta D, Forastiere F.et al Socioeconomic status and survival of persons with AIDS before and after the introduction of highly active antiretroviral therapy. Epidemiology 200011496–501. [DOI] [PubMed] [Google Scholar]
- 11.EuroHIV HIV/AIDS surveillance in Europe. End‐year report 2003Number 70. Saint‐Maurice: Institut de Veille Sanitaire, 2004
- 12.Arribas P, Cirera E, Tristán M. Buscando una aguja en un pajar: las técnicas de conexión de registros en los sistemas de información sanitaria. Med Clin (Barc) 2004122(Suppl 1)16–20. [DOI] [PubMed] [Google Scholar]
- 13.Diez‐Roux A V. Multilevel analysis in public health research. Annu Rev Public Health 200021171–192. [DOI] [PubMed] [Google Scholar]
- 14.Raudenbush S, Bryck A, Cheong Y F.et alHierarchical linear and nonlinear modelling. Lincolnwood: Scientific Software International, USA, 2000
- 15.Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol 200516181–88. [DOI] [PubMed] [Google Scholar]
- 16.Brugal M T, Borrell C, Diaz de Quijano E.et al Deprivation and AIDS in a southern European city: different patterns across transmission group. Eur J Public Health 200313259–261. [DOI] [PubMed] [Google Scholar]
- 17.Borrell C, Rodríguez‐Sanz M, Pasarín M I.et al AIDS mortality before and after the introduction of highly active antiretroviral therapy: does it vary with socioeconomic level in a country with a National Health System?Eur J Public Health 200616601–608. [DOI] [PubMed] [Google Scholar]
- 18.Regidor E, Calle M E, Navarro P.et al The size of educational differences in mortality from specific causes of death in men and women. Eur J Epidemiol 200318395–400. [DOI] [PubMed] [Google Scholar]
- 19.Bravo M J, Royuela L, Barrio G.et al Prevalencia de prácticas indirectas de compartir material para inyectarse drogas en Galicia, Madrid, Seviila y Valencia. Gac Sanit 200418472–478. [DOI] [PubMed] [Google Scholar]
- 20.Dray‐Spira R. Social health inequalities during the course of chronic HIV disease in the era of highly active antiretroviral therapy. AIDS 200317283–290. [DOI] [PubMed] [Google Scholar]
- 21.Wood E, Montaner J S G, Tyndall M W.et al Prevalence and correlates of untreated human immunodeficiency virus type 1 infection among persons who have died in the era of modern antiretroviral therapy. J Infect Dis 20031881164–1170. [DOI] [PubMed] [Google Scholar]
- 22.Wood E, Montaner J S G, Chan K.et al Socioeconomic status, access to triple therapy and survival from HIV‐disease since 1996. AIDS 2002162065–2072. [DOI] [PubMed] [Google Scholar]
- 23.Galdós H, Caylà J A, García‐de‐Olalla P.et al Factors predicting non‐completion of tuberculosis treatment among HIV‐infected patients in Barcelona (1987–1996). Int J Tuberc Lung Dis 2000455–60. [PubMed] [Google Scholar]
- 24.Jefferys M. Social inequalities in health. Do they diminish with age? [editorial]. Am J Public Health 199686473–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beckett M. Converging health inequalities in later life, an artifact of mortality selection? J Health Soc Behavior 200041106–119. [PubMed] [Google Scholar]
- 26.Reijneveld S A, Gunning‐Schepers L J. Age, health and the measurement of socio‐economic status of individuals. Eur J Public Health 19955187–192. [Google Scholar]
- 27.Zierler S, Krieger N. Reframing women's risk: social inequalities and HIV infection. Annu Rev Public Health 199718401–436. [DOI] [PubMed] [Google Scholar]
- 28.Aranda‐Naranjo B, Davis R. Psychosocial and cultural considerations. In: Anderson JR, ed. A guide to the clinical care of women with HIV. Rockville, MD: US Department of Health and Human Services, Health Resources and Services Administration 2001275–287.
- 29.Diez Roux A V. The examination of neighborhood effects on health: conceptual and methodological issues related to the presence of multiple levels of organization. In: Kawachi I, Berkman LF, eds. Neighborhoods and health. New York: Oxford University Press, 200345–64.
- 30.Domínguez‐Berjón M F, Borrell C, Benach J.et al Medidas de privación material en los estudios de áreas geográficas pequeñas. Gac Sanit 200115(Suppl 4)23–33.12069713 [Google Scholar]
- 31.Pasarín M I, Borrell C, Plasència A. Dos patrones de desigualdades sociales en mortalidad en Barcelona? Gac Sanit 199913431–440. [DOI] [PubMed] [Google Scholar]
- 32.Gordon D. Area‐based deprivation measures—a UK perspective. In: Kawachi I, Berkman LF, eds. Neighborhoods and health. New York: Oxford University Press, 200345–64.
- 33.Pasarin M I, Borrell C, Brugal M T.et al Weighing social and economic determinants related to inequalities in mortality. J Urban Health 200481349–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peterman T A, Lindsey C A, Selik R M. This place is killing me: a comparison of counties where the incidence rates of AIDS increased the most and the least. J Infect Dis 2005191(Suppl 1)S123–S126. [DOI] [PubMed] [Google Scholar]
- 35.McFarland W, Chen S, Hsu L.et al Low socioeconomic status is associated with a higher rate of death in the era of highly active antiretroviral therapy, San Francisco. J Acquir Immune Defic Syndr 20033396–103. [DOI] [PubMed] [Google Scholar]
- 36.Montellà N, Ricart I, Borrell C.et al Comparación de las defunciones del registro de casos de sida y de las defunciones por sida del registro de mortalidad. Barcelona 1991–1992. Rev San Hig Pub 19956949–57. [PubMed] [Google Scholar]
- 37.Krentz H B, Kliewer G, Gill M J. Changing mortality rates and causes of death for HIV‐infected individuals living in Southern Alberta, Canada from 1984 to 2003. HIV Med 2005699–106. [DOI] [PubMed] [Google Scholar]
- 38.Auerbach J D, Coates T J. HIV prevention research: accomplishments and challenges for the third decade of AIDS. Am J Public Health 2000901029–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wolffers I. Biomedical and development paradigms in AIDS prevention. Bull World Health Organ 200076267–273. [PMC free article] [PubMed] [Google Scholar]
- 40.Bamberger J D, Unick J, Klein P.et al Helping the urban poor stay with antiretroviral HIV drug therapy. Am J Public Health 200090699–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Farmer P, Leandre F, Mukherjee J S.et al Community‐based approaches to HIV treatment in resource‐poor settings. Lancet 2001358404–409. [DOI] [PubMed] [Google Scholar]
- 42.Manzanera R, Torralba Ll, Brugal M T.et al Afrontar los estragos de la heroína: diez años del Plan de Acción sobre Drogas de Barcelona. Gac Sanit 20001458–66. [DOI] [PubMed] [Google Scholar]