Abstract
Objective
To assess the socioeconomic variations in call rates to the Quitline (Victoria, Australia) and in the impact of anti‐tobacco television advertising on call rates.
Design
The outcome measure was the number of calls to the Quitline in Victoria for each week for each socioeconomic group for the period January 2001 to March 2004. Socioeconomic status (SES) was derived from the caller's postcode using the Index of Socioeconomic Disadvantage provided by the Australian Bureau of Statistics. The exposure measure was weekly Target Audience Rating Points (TARPs, a standard measure of television advertising weight) for anti‐tobacco advertising broadcast in Victoria over the same period. Negative binomial regression was used to examine the interaction of SES and TARPs in their effect on the number of Quitline calls.
Results
SES and call rates were positively associated. Adjusted call rate was 57% (95% CI 45% to 69%) higher in the highest than the lowest SES quintile. SES differences in call rates were stable over time. In the study period, the effect of the presence or increasing levels of antismoking TARPs on call rates did not vary across categories of SES.
Conclusions
In the study period, different SES groups had a similar level of responsiveness to antismoking television advertisements, at least as measured by the rate of calls to the Quitline. However, the present media campaigns are not likely to diminish SES differences in call rates, and more needs to be done to encourage disadvantaged groups to call the Quitline.
Mass media antismoking advertising campaigns play an important role as part of a comprehensive tobacco control programme and are associated with increases in smoking cessation and declines in adult smoking prevalence.1,2 One of the first evaluated mass media antismoking campaigns was conducted in Australia during the 1980s. Those exposed to the campaign were found to have higher quit rates,3,4 which occurred equally across adults of different levels of educational attainment.5 This led the investigators to suggest that antismoking advertising may offer a valuable population‐wide intervention to reduce the education gap in smoking prevalence. Another study reported that antismoking televised public service announcements in the US in the mid 1980s resulted in a higher percentage of telephone calls to the Cancer Information Service from callers who had received only high school education or less.6 A mass media campaign in Scotland in the early 1990s resulted in a higher percentage of telephone calls to Smokeline from lower socioeconomic groups and contributed to an accelerated decline in smoking prevalence.7 In the modern‐day tobacco control climate of more frequent use of mass media antismoking campaigns, there have been no studies to examine whether such campaigns can influence all population subgroups.
The relationship between socioeconomic status (SES) and smoking is well established, with lower socioeconomic groups having a markedly higher prevalence of smoking.8,9,10,11,12 There is also evidence that the socioeconomic differentials in smoking are increasing in many countries.13,14,15 The evidence in Australia, however, is equivocal. While an analysis of national data from 1980 to 2001 revealed a slight widening of the gap in smoking prevalence across SES categories,16 another national report showed that the gap has remained stable in the period between 1997 and 2000.17
Many observers of the widening SES differentials in smoking suggest that lower socioeconomic groups are resistant to antismoking advice18 and that, while interventions have been successful in reducing the overall prevalence of smoking, they have been less effective in addressing social inequalities in smoking prevalence.19 Given the importance of reducing social inequalities in health,20,21 the issue of whether mass media antismoking campaigns might equally influence all smokers is critical. In this study, we aim to assess socioeconomic variations in mass‐media‐prompted seeking of help to quit in the state of Victoria, Australia.
Context of the study
Mass media antismoking campaigns have been part of the Australian state of Victoria's tobacco control efforts since the early 1980s. During the late 1980s, hypothecated tobacco tax was used to fund Quit Victoria, increasing the frequency and reach of campaigns. During the 1990s and up to the present day, Quit Victoria's antismoking advertising used a variety of messages, especially those featuring the health effects of smoking, to motivate adult smokers to quit. From 1992, television advertisements were tagged with a free‐call telephone Quitline number, which provided access to pre‐recorded advice about quitting. In 1997, the first coordinated large‐scale Australia‐wide antismoking campaign was launched. The Australian National Tobacco Campaign (NTC) developed hard‐hitting television advertisements featuring the health risks of smoking.22 Like the Quit Victoria advertisements, smoking cessation telephone services (Quitlines with live counsellors) were promoted consistently through the NTC advertisements and there were substantial investments in these services to ensure they could accommodate the increased demand. Since 1998, advertisements have been broadcast that model the behaviour of calling the Quitline. They are designed to encourage smokers to call the Quitline and portray the service as accessible, friendly, professional, effective and acceptable.22 Callers to Quitlines are offered a “Quit Pack”, which includes a 30‐page full‐colour A6 book (Quit Because You Can), leaflets about services provided by Quit Victoria and a business card‐sized fact sheet with strategies to resist craving. Through the Quitline, smokers can also access more intensive smoking cessation services, such as call‐back counselling.
Attempts have been made to tailor the anti‐tobacco and Quitline television advertisements to reach lower socioeconomic groups.23 These include deliberate placement of advertising around television programs that are more likely to be watched by these groups, and choice of images and messages that resonate with them. Furthermore, the campaign advertising material is pretested in focus groups on smokers from lower educational backgrounds.
Quitline services are identified as a valuable component of any large‐scale comprehensive tobacco control programme,24,25 and callers often represent smokers with a higher level of nicotine dependence and a greater need for assistance in quitting.26,27 The efficacy of Quitline counselling has been documented both in clinical trials and “real‐world” settings.28,29
Studies have shown a clear relationship between mass media antismoking advertising and the number of calls to telephone Quitlines.6 In Australia, as reported by Miller and associates, a correlation coefficient of 0.93 was reported between the weekly volume of television antismoking advertising and the number of calls to the Quitline.29 This study seeks to investigate whether the effect of advertising on calls varies by SES.
Methods
The data used in this study come from two sources. The outcome measure was Victorian Quitline call volume between January 2001 and March 2004, which came from the administrative records of Quit Victoria. SES was determined using postcodes provided by Quitline callers who requested a smoking Quit Pack be sent to them. About 80% of callers requested a Quit Pack. The socioeconomic distribution of callers who asked for a Quit Pack was very similar to that of other callers. The percentage of males was larger among those who asked for a Quit Pack compared to other callers (45% vs 38%). The number of households in postcodes in Victoria ranges from 22 to 19 230, with an average of 2566. Postcodes were classified using the Index of Socioeconomic Disadvantage, an area‐based socioeconomic index complied at the Collection District level by the Australian Bureau of Statistics.30 The index is derived from information about the income, education, occupation, housing, household composition and English fluency of the district's residents. SES is classified into quintiles, with low quintiles indicating high disadvantage (low SES). Callers with an unidentifiable postcode were excluded from the analysis (representing 6% of the total calls). In order to examine the degree of homogeneity within SES quintiles, we computed the intraclass correlation for postcode median income across SES quintiles. This statistic was 0.42 (p<0.001), which indicates a high level of homogeneity within each quintile.
The exposure measure was weekly antismoking Target Audience Rating Points (TARPs) for all Victorians (smokers and non‐smokers) aged ⩾18 years, which was provided by ACNielsen (Sydney, New South Wales, Australia). TARPs are a standard measure of television advertising weight and are used to indicate the number of people within a certain demographic group that were exposed to an advertisement within a given period of time. A value of 100 TARPs for one week is equal to an average of one exposure per person in the target population within that week of the campaign. Based on the distribution of TARPs over the period, the weekly sum of TARPs for Victorians aged ⩾18 for the Quit Victoria antismoking advertisements were grouped into three categories: No TARPs, medium (1–161 TARPs) and high (162–748 TARPs). This grouping was used on the basis that it enabled analysis of calls and SES when there was no advertising, and it produced two approximately even‐sized groups for analysing the effects of medium and high levels of advertising. The adverts shown during this period were mainly related to illustrating the health risks of smoking, although one advertisement highlighted the deceptive behaviour of the tobacco industry, and all were accompanied by advertisements to promote the Quitline. They included advertisements developed by the NTC22 which continued to be broadcast in Victoria, and other advertisements listed on the Quit Victoria website (http://www.quit.org.au/index.html).
Poisson regression is normally suited for modelling the effect of covariates on a count variable such as the number of Quitline calls; however, we employed negative binomial regression because the data were overdispersed (ie, the Poisson model underestimated the variance of the outcome). We used the log of the population count of smokers aged >15 as the offset term. General population estimates for each quintile of SES in Victoria were provided by the Australian Bureau of Statistics CData, base on the 2001 Census of Population.31 The proportion of smokers aged >15 in each quintile were derived form the 2001 National Drug Strategy Household Survey32; they were 0.24, 0.22, 0.21, 0.21 and 0.16, in the most disadvantaged to the least disadvantaged quintiles, respectively. Our regression models adjusted for TARPs for nicotine replacement therapy (NRT) advertisements bought by pharmaceutical companies, coded as: no TARPs, medium (1–160 TARPs) and high (161–445 TARPs). We used week as a covariate to de‐trend the data. All statistical analyses were performed with Stata V.8.0.
Results
Within the 169 weeks of the study, there were 47 520 calls to the Quitline in Victoria from identifiable postcodes. The percentage of calls from the first, second, third, fourth and fifth quintile of SES, were 25.8, 18.1, 14.8, 17.0 and 24.3, respectively. There were no anti‐tobacco television advertisements during 88 weeks of the study period. There was a medium volume of TARPs in 42 weeks and a high volume in 39 weeks.
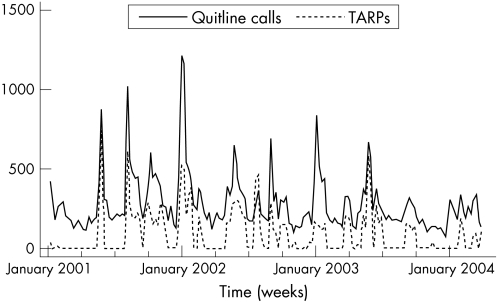
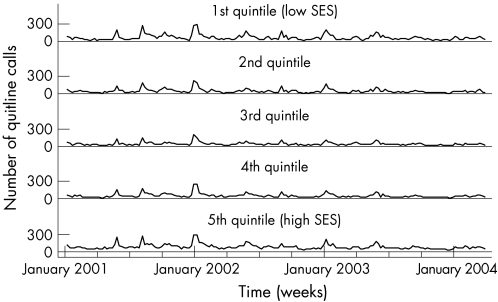
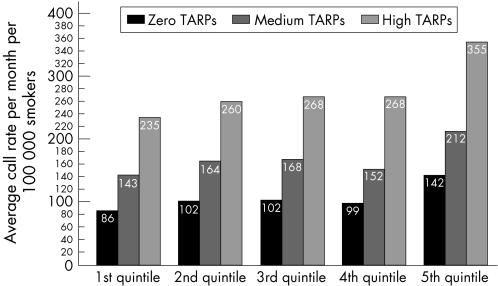
Figure 1 shows that higher weekly TARPs correspond closely with a larger overall volume of calls. Figure 2 shows the trend in calls by SES. The trend appears to be very similar across SES categories, indicating no interaction between TARPs and SES in their effect on the volume of calls. Figure 3 shows the amount of increase in call rates due to increasing levels of TARPs, across SES groups. The call rates gradient appears to be very similar across SES groups.
Figure 1 Quitline calls and antismoking Target Audience Rating Points (TARPs).
Figure 2 Trends in Quitline calls by socioeconomic status (SES).
Figure 3 The effect of Target Audience Rating Points (TARPs) on smokers'call rates by socioeconomic status.
In order to statistically assess the interaction effect of SES and TARPs on call rates and examine the interaction of these two covariates, we estimated a negative binomial regression, as described above. Table 1 presents the rate ratios, which are the exponentiated regression coefficients. SES and call rates were inversely associated. Adjusted call rate was 57% (95% CI 45% to 69%) higher in the highest than the lowest SES quintile. Anti‐smoking and NRT TARPs were positively associated with call rates. Week had a rate ratio smaller than unity, indicating a decreasing trend over time in rates of calls to the Quitline. Likelihood ratio tests for the interaction of antismoking TARPs (p = 0.934), NRT TARPs (p = 0.995) revealed no evidence of an interaction. We further examined the interaction of time with SES and found no evidence of an interaction (p = 0.336), suggesting that SES differentials in call rates were stable in the study period.
Table 1 Rate ratios and 95% CI from negative binomial regression of log of number of Quitline calls on covariates.
| Covariates | Crude RR (95% CI) | p Value | Adjusted RR (95% CI) | P Value |
|---|---|---|---|---|
| Socioeconomic status (SES) | <0.001 | <0.001 | ||
| 1st quintile (high disadvantage) | 1.00 | 1.00 | ||
| 2nd quintile | 1.14 (1.02 to 1.28) | 1.15 (1.07 to 1.24) | ||
| 3rd quintile | 1.17 (1.04 to 1.31) | 1.17 (1.08 to 1.27) | ||
| 4th quintile | 1.22 (1.00 to 1.26) | 1.23 (1.04 to 1.21) | ||
| 5th quintile (low disadvantage) | 1.54 (1.38 to 1.73) | 1.57 (1.45 to 1.69) | ||
| Antismoking TARPs | <0.001 | <0.001 | ||
| Zero | 1.00 | 1.00 | ||
| Medium | 1.58 (1.48 to 1.69) | 1.58 (1.49 to 1.68) | ||
| High | 2.62 (2.44 to 2.80) | 2.52 (2.37 to 2.69) | ||
| Nicotine replacement therapy TARPs | ||||
| Zero | 1.00 | <0.001 | 1.00 | <0.001 |
| Medium | 1.11 (1.02 to 1.22) | 1.14 (1.07 to 1.21) | ||
| High | 1.42 (1.29 to 1.56) | 1.23 (1.16 to 1.32) | ||
| Week | 1.00 (1.00 to 1.00)* | <0.006 | 1.00 (1.00 to 1.00) | <0.001 |
*The rate ratio and confidence limits for week are slightly smaller than unity.
Discussion
We examined socioeconomic variations in Quitline call rates (Victoria, Australia) and found that they were lower among lower socioeconomic groups. We also showed that, in the study period (2001–2004), there was no socioeconomic variation in the effect on call rates of anti‐tobacco television advertising that predominantly featured hard‐hitting advertisements on the health risks of smoking, and promotion of a telephone Quitline. That is, the amount of increase in the number of Quitline calls as a response to a given increase in the volume of advertising was the same across socioeconomic groups. Furthermore, we found that socioeconomic differences in call rates were stable throughout the study period. The findings indicate that, in the study period, antismoking media campaigns prompted help seeking for quitting smoking (at least as measured by call rates to the Quitline) equally among people of lower and higher SES. The existing stable SES differences in call rates have historical reasons that are unrelated to the current antismoking media campaigns. While the lower SES bias of the choice of media placement and images (as discussed above) existed since the early 1990s, Quitline services have been extensively promoted and advertised only in recent years. If lower SES groups are less likely to call the Quitline in the absence of Quitline promotion and advertisement, then this could help explain the SES differences in call rates in the period before this study. More research is required to investigate the origins and causes of these initial differences. The present media campaigns are unlikely to diminish SES variations in call rates, and more needs to be done to encourage smokers from disadvantaged groups to call the Quitline. However, it needs to be noted that the implementation of tobacco control policies that apply to the whole of the population (eg, the recently legislated clean‐air laws in pubs and bars, and graphic warnings on cigarette packs), which provide a more supportive environment for smoking cessation, might enhance the effect of media campaigns on lowering the smoking prevalence among disadvantaged groups.
What is already known
Previous research has shown that mass media antismoking advertising campaigns are associated with increases in calls to telephone helplines for quitting smoking.
What this paper adds
The present study showed that area socioeconomic status (SES) was positively associated with rates of calls to Quitline in Victoria, Australia. SES variations in call rates were stable in the study period, 2001–2004. We also examined the effect of anti‐tobacco television advertising that predominantly featured hard‐hitting advertisements on the health risks of smoking, and promotion of a telephone Quitline, on SES variations in call rates. We found no effect such that the amount of increase in Quitline call rates as a response to a given increase in the volume of advertising was the same across SES groups.
Policy implications
The present media campaigns in Australia are unlikely to diminish socioeconomic status variations in call rates, and more needs to be done to encourage smokers from disadvantaged groups to call the Quitline. However, the implementation of tobacco control policies that apply to the whole of the population (eg, the recently legislated clean‐air laws in pubs and bars, and graphic warnings on cigarette packs), which provide a more supportive environment for smoking cessation, might enhance the effect of media campaigns on lowering the smoking prevalence among disadvantaged groups.
Some study limitations need to be noted. Our method of estimating the size of the smoking population in each SES quintile may have been crude. Ideally, we would require the smoking prevalence within each postcode from a source such as a population census (as is the case in New Zealand where all residents are asked to state their smoking status) or a large population survey. Such data are not available in Australia.
We examined the effect of campaigns that use mainly hard‐hitting advertisements about serious health effects of smoking in combination with Quitline promotion. Advertisements with a different motivational message, which might depict, for example, the social acceptability of smoking or how smoking may cause non‐serious outcomes such as wrinkling or bad breath, might not result in the same pattern of findings we have reported.
Calling the Quitline is not the only outcome of an anti‐tobacco television campaign.25 Mass media campaigns are also associated with an improvement in the knowledge of the harms of smoking, increased intentions to quit smoking,33 frequency of negative thoughts about smoking, cessation activity,34 and smoking prevalence.1,3 Future research might further explore SES differentials in the effect of campaigns and levels of TARPs on these outcomes.
Acknowledgements
We thank Todd Harper for useful comments on a previous draft of this paper.
Abbreviations
NRT - nicotine replacement therapy
NTC - National Tobacco Campaign
SES - socioeconomic status
TARP - Target Audience Rating Point
Footnotes
Funding: MS and MW are funded by fellowships from the Victorian Health Promotion Foundation (VicHealth).
Competing interests: None.
The collection of Quitline data has been approved by the Human Research Ethics Committee at the Cancer Council Victoria.
References
- 1.McVey D, Stapleton J. Can anti‐smoking television advertising affect smoking behaviour? Controlled trial of the health education authority for England's anti‐smoking TV campaign. Tob Control 20009273–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hyland A, Wakefield M, Higbee C.et al Anti‐tobacco television advertising and indicators of smoking cessation in adults: a cohort study. Health Educ Res 200621296–302. [DOI] [PubMed] [Google Scholar]
- 3.Pierce J P, Macaskill P, Hill D. Long‐term effectiveness of mass media led anti‐smoking campaigns in Australia. Am J of Public Health 199080565–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pierce J P, Dwyer T, Frape G.et al Evaluation of the Sydney “quit for life” anti‐smoking campaign. Med J Aust 1986144341–347. [PubMed] [Google Scholar]
- 5.Macaskill P, Pierce J P, Simpson J M.et al Mass media‐led antismoking campaign can remove the education gap in quitting behaviour. Am J Public Health 19928296–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pierce J P, Anderson D M, Romano R M.et al Promoting smoking cessation in The United States: effect of public service announcements on the cancer information service telephone line. J Natl Cancer Inst 199284677–683. [DOI] [PubMed] [Google Scholar]
- 7.Platt S, Tannahill A, Watson J.et al Effectiveness of antismoking telephone helpline: a follow up survey. BMJ 19973141371–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huisman M, Kunst A E, Mackenbach J P. Inequalities in the prevalence of smoking in the European Union: comparing education and income. Prev Med 200540756–764. [DOI] [PubMed] [Google Scholar]
- 9.Siahpush M, Borland R. Sociodemographic variations in smoking status among Australians aged 18 years and over: multivariate results from the 1995 National Health Survey. Aust N Z J Public Health 200125438–442. [PubMed] [Google Scholar]
- 10.Barbeau E M, Krieger N, Soobader M J. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health 200494269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pampel F C. Patterns of tobacco use in the early epidemic stages: Malawai and Zambia, 2000–2002. Am J Public Health 2005951009–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sorensen G, Gupta P C, Pednekar M S. Social disparities in tobacco use in Mumbai, India: the roles of occupation, education, and gender. Am J Public Health 2005951003–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giskes K, Kunst A E, Benach J.et al Trends in smoking behaviour between 1985 and 2000 in nine European countries by education. J Epidemiol Commun Health 200559395–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Evandrou M, Falkingham J. Smoking behaviour and socio‐economic status: a cohort analysis, 1974 to 1998. Health Stat Q 20021430–38. [Google Scholar]
- 15.Federico B, Kunst A E, Vannoni F.et al Trends in educational inequalities in smoking in northern, mid and southern Italy, 1980–2000. Prev Med 200439919–926. [DOI] [PubMed] [Google Scholar]
- 16.White V, Hill D, Siahpush M.et al How has the prevalence of cigarette smoking changed among Australian adults? Trends in smoking prevalence between 1980 to 2001. Tob Control 20031267–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siahpush M, Borland R. Trends in sociodemographic variations in smoking prevalence, 1997–2000. Australia's National Tobacco Campaign: evaluation report vol 3. Canberra: Commonwealth Department of Health and Aged Care, 2004
- 18.Lawlor D, Frankel S, Shaw M.et al Smoking and ill health: does lay epidemiology explain the failure of smoking cessation programs among deprived populations? J Public Health 200393266–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sorensen G, Barbeau E, Hunt M K.et al Reducing social disparities in tobacco use: a social‐contextual model for reducing tobacco use among blue‐collar workers. Am J Public Health 200494230–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kawachi I, Kennedy B P.The health of nations: why inequality is harmful to your health. New York: The New Press, 2002
- 21.Graham H. ed. Understanding health inequalities. Buckingham: Open University Press, 2001
- 22.Hill D, Carroll T. Australia's National Tobacco Campaign. Tob Control 200312ii9–NaN14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hassard K. ed. Australia's National Tobacco Campaign: evaluation report. Vol 1 Canberra: Commonwealth Department of Health and Aged Care, 1999
- 24.Zhu S‐H, Anderson C M, Johnson C E.et al A centralised telephone service for tobacco cessation: the Californian experience. Tob Control 20009ii48–ii55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wakefield M, Borland R. Saved by the bell: the role of telephone helpline services in the context of mass‐media anti‐smoking campaigns. Tob Control 20009117–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Owen N, Roberts L, Wakefield M. The South Australian Quit advisory service: characteristics of callers and cessation outcomes. Health Promot J Austr 1995549–50. [Google Scholar]
- 27.Balanda K P, Lowe J B, O'Connor‐Fleming M ‐ L. Comparison of two self‐help smoking cessation booklets. Tob Control 1999857–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu S ‐ H, Anderson C M, Tedeschi G J.et al Evidence of real‐world effectiveness of a telephone Quitline for smokers. N Eng J Med 20023471106–1109. [DOI] [PubMed] [Google Scholar]
- 29.Miller C L, Wakefield M, Roberts L. Uptake and effectiveness of the Australian telephone Quitline service in the context of a mass media campaign. Tob Control 200312ii53–ii58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Australian Bureau of Statistics Socio‐economic indexes for areas, Australia, 2001. Cat. No. 2039. 0. Canberra: AGPS, 2003
- 31.Australian Bureau of Statistics CDATA 2001 ‐ full GIS. Available from, http://www.abs.gov.au (accessed 13 Jan 2007)
- 32.Australian Institute of Health and Welfare and Commonwealth Department of Health and Aged Care National drug strategy household survey, 2001. Canberra: Social Science Data Archive, The Australian National University, 2002
- 33.Wakefield M, Freeman J, Donovan R. Recall and response of smokers and recent quitters to the Australian National Tobacco Campaign. Tob Control 200312ii15–ii22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Borland R, Balmford J. Understanding how mass media campaigns impact on smokers. Tob Control 200312ii45–ii52. [DOI] [PMC free article] [PubMed] [Google Scholar]