Abstract
Background
Tuberculosis treatment outcome monitoring was introduced in England, Wales and Northern Ireland in 2002 based on cases reported in 2001.
Objective
To estimate the proportion of treatment success and to identify predictors of non‐completion for cases reported in 2001.
Method
At 12 months after the start of treatment, outcome was assessed according to a protocol based on standardised European recommendations.
Results
The proportion of cases completing treatment by 12 months was 79% if calculated for cases in whom outcome information was reported, and 62% of all cases regardless of whether information on outcome was reported or not. Of the new smear‐positive pulmonary cases for whom information on outcome was reported, 77% completed treatment. Non‐completion of treatment was associated with male sex, age ⩾65 years, recent entry into UK for those born abroad, residence outside London, pulmonary disease and drug resistance.
Conclusions
Despite the resources of an industrialised country with a low incidence of tuberculosis, the World Health Organization treatment success target of 85% was not achieved. This was partly due to the number of deaths in the elderly, and partly due to missing outcome information for 21% of the cases. As in other low‐incidence countries, additional outcome measures such as the proportion of those aged <65 years completing treatment would provide a more comparable indicator for assessment of treatment success. This first year of data collection has shown the importance of increasing the proportion of cases for whom outcome is ascertained, and of ensuring the validity of information provided.
Tuberculosis control aims to reduce mortality and morbidity due to tuberculosis, while preventing the development of drug resistance. It includes early diagnosis of cases and effective antituberculosis treatment. The proportion of cases with a successful outcome is therefore a key indicator to assess the effectiveness of national tuberculosis control programmes. The World Health Organization (WHO) has set a target of 85% of successful outcome for new sputum smear‐positive pulmonary cases.1
After decades of declining tuberculosis notification rates in England and Wales, rates began to increase in the late 1980s, and this trend has continued.2,3 By contrast, in many other western European countries, tuberculosis rates have continued to decline.4 In England, Wales and Northern Ireland, 6652 tuberculosis cases were reported in 2001, representing a rate of 12.4 per 100 000 population. However, higher rates are reported in some population subgroups and geographical areas. The tuberculosis rate in 2001 was 77 per 100 000 in people born abroad, that is, outside the UK, compared with 4 per 100 000 in people born in the UK. The rate was 38 per 100 000 in London, where 41% of all cases in England, Wales and Northern Ireland were reported in 2001.5
A working group published recommendations for the standardisation of tuberculosis treatment outcome monitoring across Europe in 1998.6 Since then, it has been increasingly implemented in Europe.4,7 However, in 2001, of the 15 European Union countries, only six provided national results on treatment outcome to EuroTB. The results were incomplete for three countries, and no information was available for six others.4 The late implementation of treatment outcome monitoring in well‐resourced countries with a relatively low incidence, such as the UK, may be explained partly by the structure of tuberculosis services, which are generally an integrated part of the overall healthcare system, rather than separate specialised services.8
In England, Wales and Northern Ireland, continuous monitoring of treatment outcome began in 2002 on cases reported in 2001, as part of the “enhanced tuberculosis surveillance” system. In this article, the first year of treatment outcome monitoring data was used to estimate the proportion of treatment completion and to identify predictors of non‐completion of treatment among reported tuberculosis cases.
Methods
Methods for tuberculosis treatment outcome monitoring in England, Wales and Northern Ireland have been based on the European recommendations6 adapted to the UK context, and have been agreed after consultation with clinicians, nurses and public health professionals. To provide information on probable transmission of infection, the WHO focuses on sputum smear‐positive pulmonary cases and has defined the treatment outcome monitoring cohort according to this priority.1 The European recommendations6 define the cohort as all culture‐confirmed pulmonary cases, to take into account the routine use of culture to confirm cases in an increasing number of European countries. Around 40% of tuberculosis cases diagnosed in the UK are, however, reported to have exclusively extrapulmonary disease.5 Although these cases do not present an immediate infectious threat to others, successful treatment is important for the health of the individual case, and treatment outcome results in this group contribute to an assessment of the quality of tuberculosis treatment services overall. In addition, the Chief Medical Officer's Action Plan for England recommends that information on treatment outcome should be collected for all patients with tuberculosis, and that at least 85% should successfully complete treatment.9
The cohort in which treatment outcome was determined consisted of all 6514 tuberculosis cases (pulmonary and extra‐pulmonary) reported between 1 January and 31 December 2001, including cases with a postmortem diagnosis, but excluding denotified cases (cases initially reported but subsequently found not to be tuberculosis cases). All tuberculosis cases were to be reported, whether or not they were culture confirmed (table 1).
Table 1 Tuberculosis case definitions used for surveillance purposes in England, Wales and Northern Ireland.
| Case classification | Description | |
|---|---|---|
| Culture‐confirmed case | Culture‐confirmed disease due to Mycobacterium tuberculosis complex (M tuberculosis, M bovis or M africanum) | |
| Other than culture‐confirmed case | In the absence of culture confirmation, cases meeting the following criteria: (a) a clinician's judgement that the patient's clinical or radiological signs are compatible with tuberculosis and (b) clinician's decision to treat the patient with a full course of antituberculosis treatment |
Pulmonary cases were defined as those with tuberculosis affecting the lung parenchyma and/or the tracheobronchial tree.
From January 2002, clinicians who had reported tuberculosis cases in 2001 were asked to complete a form classifying the patient's status at 12 months after the start of treatment (or diagnosis, or notification date where date of start of treatment was not available) into one of nine outcome categories (table 2). In England, Wales and Northern Ireland, the category “treatment completion” was used to indicate a successful outcome, as is increasingly the practice in Europe.4 This category includes all cases who had completed treatment at 12 months, whether or not microbiologically confirmed as “cured”.
Table 2 Tuberculosis treatment outcome definitions used in England, Wales and Northern Ireland.
| Outcome category | Description | |
|---|---|---|
| Treatment completed | Patient completed a full course of treatment at 12 months and was officially discharged by the attending doctor | |
| Cured | Patient completed a full course of treatment within 12 months, and there was a documented culture conversion in sputumculture‐positive patients during treatment | |
| Died | Patient died before or during treatment, including postmortem cases | |
| Still on treatment | Patient was still on treatment at 12 months | |
| Treatment stopped | Treatment was stopped, eg, due to an adverse drug reaction | |
| Transfer out | Responsibility of patient's care was transferred to another clinical team | |
| Lost to follow‐up | Patient was lost to follow‐up before the end of treatment | |
| Treatment not completed (no reason) | Patient was reported not to have completed treatment, but the reason was not known | |
| Outcome reported to be unknown | Information on patient's outcome was reported to be unknown |
The outcome category “cured” was defined as a subcategory of the outcome “treatment completed”. The international definition of the “cured” category was initially based on microscopy results.1 The definition has been adapted in Europe6 for countries routinely using culture. Information on cases reported was linked with data on mycobacterial isolates reported through MycobNet (the UK Mycobacterial Resistance Network of reference laboratories) to obtain information on culture results and drug susceptibility.
Statistical analysis
Data analysis was carried out on all cases included in the cohort for whom an outcome form was completed unless otherwise stated. Analysis was performed using software Epi‐Info TM V.6.01. Data were compared using χ2 or Fisher's exact tests. Statistical tests were used with 95% confidence interval (CI), and significance was taken to be p⩽0.01. Predictors of non‐completion of treatment were analysed using univariable and multivariable (logistic regression) methods.
Results
Of the 6652 tuberculosis cases reported in 2001, an outcome form was completed for 5277, 138 of whom had been denotified. Therefore, for 79% (5139 (5277–138)) of cases, an outcome status or postmortem diagnosis was reported.
The median age of cases for whom outcome was reported in 2001 was 37 years (interquartile range 26–58); 55% were male, 64% were born abroad, 59% had pulmonary tuberculosis, 41% had an extrapulmonary site of disease only and 59% were culture confirmed. The proportion of antituberculosis drug resistance among cases with drug susceptibility testing results was 6.2% for isoniazid (158/2537) and 0.7% for multidrug resistance (18/2656).
Proportion of cases with treatment completed
Overall, the proportion of cases who had completed treatment by 12 months was 79% if calculated for cases with outcome information reported (4033/5139), and 62% if calculated for all cases regardless of whether an outcome was reported (4033/6514). Further analyses are presented only for cases with outcome information reported (n = 5139).
The proportion of treatment completion was higher for patients with extrapulmonary tuberculosis than for pulmonary cases (82% vs 76%; p<0.001). For pulmonary cases with a positive culture, the proportion of treatment completion was 77% (1476/1927), of which 16.5% (317/1927) were classified as “cured” (table 3). For pulmonary cases with a sputum smear‐positive result, the proportion of treatment completion was 76% (822/1079) of all cases, and 77% (683/886) of new cases (with no previous tuberculosis diagnosis).
Table 3 Tuberculosis cases reported in England, Wales and Northern Ireland in 2001 by outcome category.
| Outcome category | All cases*, n (%) | All pulmonary†, n (%) | Pulmonary culture positive, n (%) | All extra‐ pulmonary‡, n (%) |
|---|---|---|---|---|
| Treatment completed | 4033 (78.5) | 2252 (75.7) | 1476 (76.6) | 1728 (82.3) |
| Of which cured | — | — | 317 (16.5) | — |
| Death | 427 (8.3) | 317 (10.7) | 198 (10.3) | 106 (5) |
| Lost to follow‐up | 207 (4) | 126 (4.2) | 78 (4) | 78 (3.7) |
| Still on treatment | 206 (4) | 120 (4) | 84 (4.4) | 84 (4) |
| Treatment stopped | 63 (1.2) | 36 (1.2) | 17 (0.9) | 26 (1.2) |
| Transfer out | 54 (1.1) | 34 (1.1) | 20 (1) | 20 (1) |
| Treatment not completed (no reason) | 13 (0.3) | 8 (0.3) | 4 (0.2) | 5 (0.2) |
| Outcome reported to be unknown | 136 (2.6) | 81 (2.7) | 50 (2.6) | 53 (2.5) |
| Total | 5139 (100) | 2974 (100) | 1927 (100) | 2100 (100) |
*Including 65 cases with site not reported.
†Pulmonary tuberculosis with or without extrapulmonary localisation.
‡Only extrapulmonary localisation.
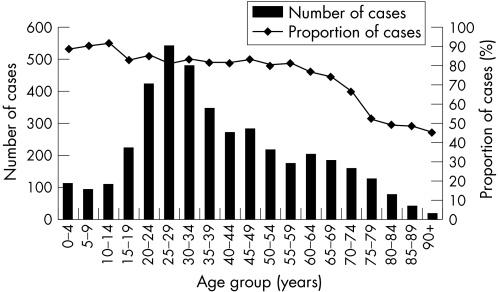
Treatment completion was strongly associated with age. The proportion of treatment completion decreased with age, ranging from ⩾80% in all age groups <60 years to <50% in those aged ⩾80 years (fig 1). The proportion of cases completing their treatment was significantly higher for women than in men (81% vs 77%, p<0.001).
Figure 1 Number and proportion of tuberculosis cases with treatment completed by age group for cases reported in England, Wales and Northern Ireland in 2001.
The proportion of treatment completion was higher for cases born abroad than for those born in the UK (82% vs 76%, p<0.001), and this difference remained, but was less marked, when standardised for age group (81% vs 78%, p<0.001). The proportion of treatment completion was higher for cases reported in London compared with those reported outside London (83% vs 75%, p<0.001).
Reasons and predictors of non‐completion of treatment
In all, 21% (1106/5139) of cases had not completed treatment at 12 months. These comprised 8.3% deaths (of which 37% were cases diagnosed postmortem), 4% lost to follow‐up, 4% still on treatment, 1.1% transferred out and 1.2% treatment stopped. Information on outcome was reported to be unknown for the remaining 2.6% of cases (table 3).
Of the 206 cases still on treatment, the regimen was initially planned to be >12 months for 40% of patients, and for 38% the initially planned course of treatment was changed; this was mainly due to drug resistance, an adverse reaction or poor clinical response. Treatment was prolonged due to an interruption in the regimen for 15% of cases, and for 7% the reason for still being on treatment was unknown.
Analysis of additional information supplied on the 63 cases who were reported to have stopped treatment showed that this was due to an adverse reaction in 24% of cases and to non‐compliance with the regimen in 13% of cases. In the remaining 63%, either no reason was given or the comments provided on the outcome form were not interpretable. Of the 427 cases who died, the relationship between tuberculosis and death was unknown for 46%, in 34% tuberculosis caused or contributed to death, and in 20% tuberculosis was incidental to death.
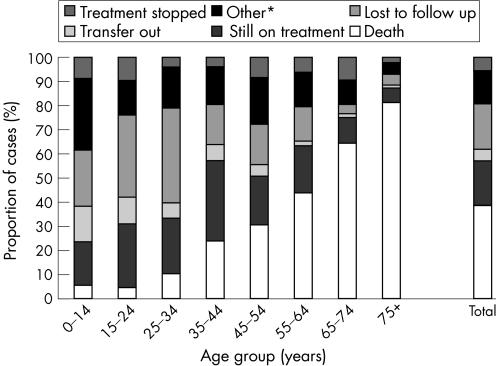
Death (irrespective of cause) was the main reason for non‐completion of treatment in the older age groups, representing the outcome in 69% of patients with treatment not completed aged ⩾65 years and in 78% in those aged ⩾75 years. By contrast, the main reasons of non‐completion in patients aged <40 years were being lost to follow‐up and being still on treatment, representing 33% and 26% of cases in this age group, respectively (fig 2).
Figure 2 Reasons for non‐completion of treatment by age group, for cases reported in England, Wales and Northern Ireland in 2001 (n = 1106). *Includes outcome categories “treatment not completed (no reason)” and “outcome reported to be unknown”.
From the multivariable analysis (table 4), the characteristics found to be significantly associated with non‐completion of treatment at 12 months were being:
Table 4 Predictors of non‐completion of treatment among cases reported in England, Wales and Northern Ireland in 2001 (univariable and multivariable analysis).
| Case characteristic | Number of cases | Univariable analysis for non‐completion of treatment | Multivariable analysis for non‐completion of treatment* | |||
|---|---|---|---|---|---|---|
| Not completed | Completed | OR (95%CI) | p Value | aOR† (95%CI) | p Value | |
| Total | 1106 | 4033 | — | — | — | — |
| Sex (n = 5134) | <0.001 | 0.011 | ||||
| Male | 657 | 2147 | 1.3 (1.1 to 1.5) | 1.2 (1.1 to 1.5) | ||
| Female | 449 | 1881 | 1 | 1 | ||
| Age (years; n = 5137) | <0.001 | <0.001 | ||||
| 0–14 | 33 | 305 | 0.5 (0.4 to 0.8) | 0.5 (0.3 to 0.8) | ||
| 15–44 | 479 | 2274 | 1 | 1 | ||
| 45–64 | 207 | 869 | 1.1 (0.9 to 1.4) | 1.0 (0.8 to 1.2) | ||
| ⩾65 | 387 | 583 | 3.2 (2.7 to 3.7) | 2.7 (2.1 to 3.4) | ||
| Place of birth (n = 4617) | <0.001 | <0.001 | ||||
| UK | 394 | 1260 | 1 | 1 | ||
| Abroad (entry <1 year) | 72 | 204 | 1.1 (0.8 to 1.5) | 1.7 (1.2 to 2.6) | ||
| Abroad (entry 1–4 years) | 127 | 713 | 0.6 (0.5 to 0.7) | 1 (0.7 to 1.3) | ||
| Abroad (entry >4 years) | 183 | 1019 | 0.6 (0.5 to 0.7) | 0.8 (0.6 to 1.1) | ||
| Abroad (entry date unknown) | 153 | 492 | 1 (0.8 to 1.2) | 1.4 (1 to 1.9) | ||
| Ethnic group (n = 4948) | <0.001 | 0.036 | ||||
| White | 448 | 1068 | 1 | 1 | ||
| Black Caribbean | 39 | 119 | 0.8 (0.5 to 1.1) | 1.4 (0.9 to 2.2) | ||
| Black African | 150 | 674 | 0.5 (0.4 to 0.7) | 1.2 (0.8 to 1.7) | ||
| Indian, Pakistani and Bangladeshi | 320 | 1616 | 0.5 (0.4 to 0.6) | 0.8 (0.6 to 1.1) | ||
| Other | 93 | 421 | 0.5 (0.4 to 0.7) | 1 (0.7 to 1.5) | ||
| Place of reporting (n = 5139) | <0.001 | <0.001 | ||||
| London | 393 | 1908 | 1 | 1 | ||
| Outside London | 713 | 2125 | 1.6 (1.4 to 1.9) | 1.5 (1.2 to 1.8) | ||
| Previous history of TB (n = 4344) | <0.001 | 0.284 | ||||
| Previous TB | 100 | 256 | 1.6 (1.2 to 2) | 1.2 (0.9 to 1.5) | ||
| No previous TB | 795 | 3193 | 1 | 1 | ||
| Culture result (n = 5139) | 0.613 | — | — | |||
| Culture positive | 656 | 2358 | 1 (0.9 to 1.2) | — | — | |
| Culture negative, not done, unknown | 450 | 1675 | 1 | — | — | |
| Site of disease (n = 5074) | <0.001 | 0.008 | ||||
| Pulmonary TB | 722 | 2252 | 1.5 (1.3 to 1.7) | 1.3 (1.1 to 1.5) | ||
| Extrapulmonary TB | 372 | 1728 | 1 | 1 | ||
| Isonaizid susceptibility results (n = 5139) | <0.001 | 0.004 | ||||
| Isoniazid resistant | 58 | 100 | 2.3 (1.6 to 3.2) | 2.2 (1.4 to 3.3) | ||
| Isoniazid susceptible | 482 | 1897 | 1 | 1 | ||
| Results not known | 566 | 2036 | 1.1 (1 to 1.3) | 1.3 (0.8 to 2.1) | ||
| MDR susceptibility results (n = 5139) | <0.001 | 0.004 | ||||
| MDR | 14 | 4 | 13 (4.2 to 39.5) | 7 (2 to 24.3) | ||
| Not MDR | 561 | 2077 | 1 | 1 | ||
| Results not known | 531 | 1952 | 1 (0.9 to 1.2) | 0.9 (0.6 to 1.6) | ||
Difference between totals (1106 and 4033) and totals by case characteristics are due to missing information.
*3941 cases were included in the multivariate analysis.
†Adjusted OR (aOR) on the variables included in the multivariable analysis corresponding to variables presented in the table with a significant association (p<0.01) with non‐completion of treatment on univariable analysis (no interaction between variables was found).
Male
Aged ⩾65 years
Born abroad (with entry into the UK <1 year before developing tuberculosis disease)
Reported outside London
A pulmonary tuberculosis case
A case resistant to isoniazid
A multidrug‐resistant case (resistant to at least isoniazid and rifampicin).
In the multivariable analysis performed only on cases positive by pulmonary culture, the significant risk factors associated with non‐completion of treatment were being aged ⩾65 years, and having isoniazid or multidrug‐resistant tuberculosis.
Discussion
These results show that treatment outcome can be effectively monitored, and provide a starting point to enable the monitoring of trends. This information makes it possible to identify groups or areas where treatment outcome was not completed and to target measures for improvement.
Of the 5139 tuberculosis cases reported in 2001 for whom outcome was reported, 79% had completed treatment within 12 months of starting. The proportion of cases with treatment completed (79%) was calculated for cases in whom outcome was reported. If calculated for all reported cases, the proportion was 62%, assuming that those cases with unknown information had not completed their treatment. From the available information, it was not possible to determine whether cases for whom the outcome was not reported were more or less likely to have a successful outcome. Cases with an outcome reported were similar to those without an outcome in terms of age and sex, but the proportion of extrapulmonary cases and people born abroad was higher in cases with no information on outcome. The two groups may also differ with regard to information not collected—for example, socioeconomic status—which could affect the treatment outcome.
The high proportion of missing information on outcome (21%) was mainly due to implementation difficulties in some areas as this was the first year of outcome monitoring (outcome was reported for <60% of cases in three regions, whereas in all other regions it was reported for 84–96%). In 2002, the preliminary estimate of the proportion with missing outcome information had reduced to 15%. The extent of the missing information may also reflect the approach to tuberculosis treatment in the UK, which, as in other industrialised countries, is based on individual clinician autonomy in case management rather than the structured national programmes seen in many countries with high tuberculosis burden. Additionally, in the UK, as in other low‐incidence countries, tuberculosis tends to be concentrated in urban areas and in some population subgroups, including “hard‐to‐reach” and highly mobile populations—for example, the homeless and recent immigrants who may return to their country of origin before the end of their treatment.8
Only 16.5% of pulmonary culture‐confirmed cases were reportedly “cured”. The outcome category “cured” is difficult to assess in this country and in many other industrialised countries where the bacteriological confirmation of cases is based on culture. In clinical practice, if the diagnosis has been based on culture, specimens are often not obtained to determine whether cases have become negative for culture during or after treatment. In addition, the use of culture is not always feasible for some disease sites (eg, intrathoracic lymph nodes) or in children. Therefore, the proportion of cases defined as “cured” does not accurately reflect the proportion with a successful outcome.
In line with the consensus for the cohort definition in England, Wales and Northern Ireland, both pulmonary and extrapulmonary cases were included in most of the analyses. Combining these two groups might have affected the results (eg, a higher proportion of extrapulmonary cases are foreign‐born) and could present some limitations in the conclusions that can be drawn from the results. Detailed analyses of pulmonary and extrapulmonary cases separately will therefore be an essential addition to the future assessment of treatment outcome.
The proportion of treatment completion among new sputum smear‐positive pulmonary cases with known outcome was 77%. This is comparable with other Western European countries with a similar tuberculosis incidence. For example, it was 76% in The Netherlands and 79% in Sweden in 2000.4 However, the WHO successful outcome target of 85% is not yet met in a number of western European countries.10 It might seem surprising that the proportion of treatment success of these low tuberculosis‐incidence countries is below that of some high‐burden countries.11 In the UK, this may in part be due to a high proportion of cases in the elderly (19% aged ⩾65 years in 2001) who form a much larger proportion of the population in industrialised countries. Death, and thus non‐completion of treatment, is more likely to occur in the elderly.12,13 If calculated for patients <65 years of age, the proportion of cases with treatment completed was 83%.
The inclusion of 157 postmortem cases (representing 37% of cases in the outcome category “death”) in the denominator may also affect the overall proportion of treatment completion. Tuberculosis is more likely to be diagnosed at postmortem in industrialised countries than in developing countries, because of the higher rate of postmortem examination. When postmortem cases were removed from the denominator, the proportion of cases who started a treatment and had a successful outcome was 81% of all cases reported, and 78% of sputum smear‐positive cases.
The proportion of treatment completion among all cases was significantly higher for people born abroad than for those born in the UK (82% vs 76%). This difference remained when adjusted for age. This may be partly explained by the fact that the proportion of extrapulmonary cases is twice as high in foreign‐born people compared with those born in the UK,5 and patients with extrapulmonary disease were found to be more likely to complete treatment (odds ratio (OR) 1.5, 95% confidence interval (CI) 1.3 to 1.7). However, in the multivariable analysis, when taking into account the year of entry into the UK, people who had recently arrived (<1 year) were more likely not to have completed their treatment by 12 months compared with those born in the UK.
The proportion of treatment completion was higher among cases reported in London compared with those reported outside London (83% vs 75%). This finding is supported by the multivariable analysis of predictors of non‐completion of treatment. Both the incidence of tuberculosis and factors that may complicate treatment—for example, antituberculosis drug resistance and HIV infection—are higher in London.5,14 A lower proportion of treatment completion might therefore be expected. Several factors could, however, explain these findings. The age structure and case characteristics of the cohort differed between regions. For example, the tuberculosis cases reported outside London were older and were more likely to have pulmonary tuberculosis than those reported in London (median age 42 (interquartile range 37–65) years vs 34 (interquartile range 25–49) years, OR for pulmonary tuberculosis 1.3, 95% CI 1.2 to 1.5). Further study is needed to understand the effect of these factors and to investigate possible biases in the information provided.
Other predictors associated with non‐completion of treatment were male sex, age ⩾65 years, having pulmonary tuberculosis and having an isoniazid‐resistant or multidrug‐resistant tuberculosis (multidrug resistant cases generally require a prolonged course of treatment). These findings are consistent with other studies showing that older patients with tuberculosis are more likely not to complete their treatment due to death,15,16 and that treatment failure is more likely for drug‐resistant cases than susceptible cases.17 The proportion of cases with successful outcome could be increased by earlier diagnosis and better treatment adherence in some subgroups of the population.18 With the current surveillance system, it is not possible to identify important contextual information about the reasons for non‐completion. Factors such as homelessness, unemployment, and drug or alcohol misuse have been found to be associated with non‐completion of treatment in some studies,15,19 but are difficult to collect through a routine national surveillance system. A cross sectional study carried out in London may help to improve understanding of the effect of these factors20 and contribute to the further development of continued enhanced surveillance of tuberculosis.
Continuous surveillance of treatment outcome is essential to assess tuberculosis control efforts. In the UK, and possibly in other low‐incidence countries with a similar epidemiological pattern of tuberculosis, although the age structure of cases may change over time, using additional outcome measures such as the proportion of treatment completion among those aged <65 years would provide a more comparable indicator for the assessment of treatment success. This first year of data collection on outcome has shown the importance of increasing the proportion of cases for whom treatment outcome is ascertained, and of ensuring the validity of information provided on individual cases. Further work, in the coming years, of treatment outcome monitoring data will include analyses of predictors of non‐completion of treatment excluding deaths, and more detailed study into causes of mortality among tuberculosis cases.
What is already known
Monitoring the treatment outcome of tuberculosis cases is an essential tool to assess the effectiveness of national tuberculosis control.
The World Health Organization has set as a target of 85% of successful outcome among infectious tuberculosis cases (new sputum smear‐positive pulmonary cases).
What this paper adds
As in some other European countries, the World Health Organization successful outcome target of 85% among infectious cases is not yet met in England, Wales and Northern Ireland.
This is mainly due to the effect of deaths among the elderly and to missing information on outcome.
Policy implications
Reporting information on treatment outcome is essential on all tuberculosis cases to provide an accurate assessment of the effectiveness of current treatment services.
The proportion of cases with successful outcome could be increased by earlier diagnosis and better treatment adherence in some subgroups of the population.
Acknowledgements
We thank all clinicians, nurses, microbiologists and other hospital, clinic and laboratory staff who provide information on tuberculosis cases. We acknowledge the National Public Health Service for Wales, and the Communicable Disease Surveillance Centre (Northern Ireland) for their assistance with co‐ordination of the Enhanced Tuberculosis Surveillance scheme and provision of their information. We also thank the Regional Tuberculosis Surveillance Co‐ordinators for their valuable work. We thank David Quinn for the management and the preparation of the database, André Charlett and David Gelb for their advice on the statistical analysis, and Pam Sonnenberg and Ibrahim Abubakar for their valuable comments on earlier drafts of this article.
Abbreviations
WHO - World Health Organization
Footnotes
Competing interests: None.
References
- 1.World Health Organization Treatment of tuberculosis: guidelines for national programmes. 3rd edn. WHO/CDS/TB/2003. 313. Geneva: 2003, http://www.who.int/tb/publications/global_report/en/ (accessed 4 Jan 2007)
- 2.Bhatti N, Law M R, Morris J K.et al Increasing incidence of tuberculosis in England and Wales: a study of the likely causes. BMJ 1995310967–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rose A M, Gatto A J, Watson J M. Recent increases in tuberculosis notifications in England and Wales—real or artefact? J Public Health Med 200224136–137. [DOI] [PubMed] [Google Scholar]
- 4.EuroTB, National coordinators for tuberculosis surveillance in the WHO European Region Surveillance of tuberculosis in Europe. Report on tuberculosis cases notified in 2001. Saint‐Maurice, InVS. http://www.eurotb.org/rapports/2001/etb_2001_full_report.pdf (accessed 30 Jan 2007)
- 5.CDSC HPA Annual report on tuberculosis cases reported in 2001 in England, Wales and Northern Ireland. London: 2004, 1–27. http://www.hpa.org.uk/infections/topics_az/tb/pdf/2001_Annual_Report.pdf (accessed 13 Jan 2007)
- 6.Veen J, Raviglione M C, Rieder H L.et al Standardized tuberculosis treatment outcome monitoring in Europe. Eur Respir J 199812510. [DOI] [PubMed] [Google Scholar]
- 7.EuroTB National coordinators for tuberculosis surveillance in the WHO European Region. Draft report on tuberculosis cases notified in 2002. http://www.eurotb.org/
- 8.Hayward A C, Darton T, Van Tam J N.et al Epidemiology and control of tuberculosis in Western European cities. Int J Tuberc Lung Dis 20037751–757. [PubMed] [Google Scholar]
- 9.Department of Health Stopping tuberculosis in England: an action plan from the Chief Medical Officer, 2004. http://www.dh.gov.uk/assetRoot/04/10/08/60/04100860.pdf (accessed 13 Jan 2007)
- 10.Faustini A, Hall A J, Perucci C A. Tuberculosis treatment outcomes in Europe: a systematic review. Eur Respir J 200526503–509. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization Global Tuberculosis control: Surveillance, Planning, financing. WHO Report 2004. WHO/HMT/TB/2004. 331, Geneva: 2004, 1–220. http://www.who.int/gtb/publications/globrep/index.html (accessed 13 Jan 2007)
- 12.Cullinan P, Meredith S K. Deaths in adults with notified pulmonary tuberculosis 1983–5. Thorax 199146347–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Humphries M J, Byfield S P, Darbyshire J H.et al Deaths occurring in newly notified patients with pulmonary tuberculosis in England and Wales. Br J Dis Chest 198478149–158. [PubMed] [Google Scholar]
- 14.Rose A M, Sinka K, Watson J M.et al An estimate of the contribution of HIV infection to the recent rise in tuberculosis in England and Wales. Thorax 200257442–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cayla J A, Caminero J A, Rey R.et al Current status of treatment completion and fatality among tuberculosis patients in Spain. Int J Tuberc Lung Dis 20048458–464. [PubMed] [Google Scholar]
- 16.Zellweger J P, Coulon P. Outcome of patients treated for tuberculosis in Vaud Country, Switzerland. Int J Tuberc Lung Dis 19982372–377. [PubMed] [Google Scholar]
- 17.Espinal M A, Kim S J, Suarez P G.et al Standard short‐course chemotherapy for drug‐resistant tuberculosis: treatment outcomes in 6 countries. JAMA 20002832537–2545. [DOI] [PubMed] [Google Scholar]
- 18.Falzon D, Le Strat Y, Belghiti F.et al Exploring the determinants of treatment success for tuberculosis cases in Europe. Int J Tuberc Lung Dis 200591224–1229. [PubMed] [Google Scholar]
- 19.Diel R, Niemann S. Outcome of tuberculosis treatment in Hamburg: a survey, 1997–2001. Int J Tuberc Lung Dis 20037124–131. [PubMed] [Google Scholar]
- 20.Story A, Roberts W, Hayward A.et al Tuberculosis in London: results of the 2003 TB case load profile. Int J Tuberc Lung Dis 20048(Suppl 1)S197–S198. [Google Scholar]