Abstract
To map out area effects on health research, this study had the following aims: (1) to inventory multilevel investigations of area effects on self rated health, cardiovascular diseases and risk factors, and mortality among adults; (2) to describe and critically discuss methodological approaches employed and results observed; and (3) to formulate selected recommendations for advancing the study of area effects on health. Overall, 86 studies were inventoried. Although several innovative methodological approaches and analytical designs were found, small areas are most often operationalised using administrative and statistical spatial units. Most studies used indicators of area socioeconomic status derived from censuses, and few provided information on the validity and reliability of measures of exposures. A consistent finding was that a significant portion of the variation in health is associated with area context independently of individual characteristics. Area effects on health, although significant in most studies, often depend on the health outcome studied, the measure of area exposure used, and the spatial scale at which associations are examined.
Keywords: small area analysis, neighbourhood, multilevel analysis, scoping study
A brief search of published reports on area effects on health shows a striking increase over the past decade in the number of studies adopting a multilevel approach to the study of social determinants of health. The impetus for such research probably results from a convergence of conceptual and methodological innovations, including an appreciation of the importance of the social environment to health and greater accessibility of multilevel modelling techniques and software. However, multilevel investigations of area effects on health abound with conceptual and methodological challenges which have given rise to numerous debates. Debated issues are summarised in table 1.
Table 1 Conceptual and methodological issues raised in published reports on area effects on health.
| Conceptual and methodological challenges | Description | |
|---|---|---|
| Conceptualising causal pathways2,3,4,5,6,7,8,9,10 | Absence of fully articulated theoretical frameworks and formulation of testable hypotheses. | |
| Designating the ecologic unit of analysis1,11,12 | Ecologic units of analysis have been referred to as neighbourhood, small area, local area, and place. These labels have been used interchangeably without concern for differences in conceptual and operational definitions even though some have argued that there are substantive reasons for appropriately defining the nature of the ecological unit of analysis. | |
| Defining the spatial contours of the ecological unit of analysis1,5,8,13,14,15 | Spatial contours of small areas are mostly delimited by existing administrative and statistical spatial units. However, these areas may be of limited value in examining the association between area level exposures and health outcomes, because they may lack any intrinsic meaning in relation to health, they may not correspond to the spatial distribution of environmental features (ecologic exposures) associated with health, and they may be inconsistent with how residents define and experience their residential area. | |
| Defining ecologic exposures5,7,13,15,17,18,19,20,21,22 | Little attention has been devoted to conceptually and operationally defining ecological exposures as researchers have tended to aggregate data from individuals to create meaningful area variables. | |
| Controlling for individual‐level variables2,5,13,15,18,23 | Lack of consistency in controlling for individual level variables and further lack of consensus on whether individual variables should be conceptualised as confounders, moderators, or mediators of the associations between ecological exposures and health outcomes. | |
| Power, sample size, and representativeness5,13,15,25 | Usual considerations surrounding statistical power and sample size have been neglected. | |
| Use of multilevel modelling techniques4,13,15,23,24,26,27,28 | Appropriate use of multilevel modelling techniques has been applied suboptimally, thus limiting novel perspectives that might ensue from their judicious application: results are mainly reported for fixed effects whereas the potentials of discussing conceptual and methodological ramifications of random effects have been ignored. | |
| Disentangling context from composition7,8,13,18,27,29,30,31,32,33,34 | Some investigators argue for disentangling the portion of the between area variation in health that is attributable to areas in which people live (contextual effect) from the portion attributable to individuals' characteristics (compositional effect), whereas others argued that this is a “false” issue as context and composition are inextricably intertwined. | |
| Dearth of longitudinal and experimental studies8,18,34,35 | Few studies have relied on research designs other than cross sectional. This limits ascertaining the duration and timing of ecological exposures, addressing selection bias, and ascribing causality. Furthermore, as people, areas, and the relation between the two may change over time, using longitudinal designs is of accrued importance. |
In a previous review of social determinant studies examining effects of area socioeconomic status (SES) on health, 23 of 25 studies reported significant associations between at least one measure of area SES and health, while controlling for individual SES.1 The investigators concluded that data supported the existence of modest small area effects on health but that extant data were replete with methodological problems. More specifically, they stated: “It is clear from our review that investigations of the role of neighbourhood level [small area] social factors on health are characteristics of preliminary, exploratory studies in epidemiology. Certain aspects of study design are in need of improvement before the field can advance […] We hope that this review will show what has already been achieved and point the way to more sophisticated studies of societal determinants of health” (pp 120–121).
In an effort to map out multilevel research on social determinants of health, to identify the types of evidence available, and to gauge whether or not “more sophisticated studies” are being conducted, we undertook a scoping study of research of area effects on health published between July 1998 and December 2005. Unlike the more familiar systematic review, a scoping study addresses broad research topics where many different study designs are applied, with the aim of comprehensively examining the extent, range, and nature of research activity and to identify key concepts and results.36,37
Given the broad diversity of studies, we restricted the scoping review to multilevel investigations of area effects on self rated health (SRH), cardiovascular disease and risk factors, and mortality among adults. These health indicators were selected because of their relevance to understanding the broader socio‐spatial patterning of health. SRH is a highly predictive measure of morbidity and mortality, independent of other medical, behavioural, or psychosocial factors,38 and cardiovascular disease is one of the leading causes of mortality in developed countries.
We further restricted study selection to multilevel investigations allowing for estimation of between‐area variation (random effects). As pointed out by Merlo and colleagues,24 “clustering of individual health within neighbourhoods (areas) is not a statistical nuisance that only needs to be considered for obtaining correct statistical estimations, but a key concept in social epidemiology that yields important information by itself” (p 443). As measures of variation provide information on the portion of health differences among people that may be attributable to the areas in which they live, they are central to understand the significance of specific contexts for health.24
In keeping with the framework for conducting a scoping study proposed by Arksey and O'Malley,36 the specific objectives of the scoping study were: (1) to provide an inventory of multilevel investigations of area effects on SRH, cardiovascular disease and risk factors, and mortality; (2) to describe and critically discuss the methodological approaches employed and results observed; and (3) to formulate selected recommendations for advancing the study of area effects on health.
Methods
The scoping study involved three steps.
First step
In the first step, the identification of studies published between July 1998 and December 2005 ensued from a comprehensive search strategy using the Medline database. We first used “neighbourhood/neighbourhood or area” and “multilevel/multi‐level or hierarchical” as words in the title or abstract of articles; this search yielded 634 entries. Inclusion criteria for studies were: publication in the English language, peer reviewed journals, data from adult populations in industrialised countries, use of a multilevel design with at least two units of analysis including individuals and areas, and measurement and analysis of health indicators at the individual level. Studies exploring between country variation in health were excluded, though areas operationalised by subregions of a country—for example, states—were included. Of the 634 studies, 67 meet the inclusion criteria.
We conducted additional searches using “contextual effects”, “place effects”, “census tracts”, and “community” as words in title or abstract, and “residence characteristics and small area analysis” as medical subject headings (MeSH), again limiting the search to studies referring to multilevel methods in their title or abstract. Three additional studies were identified. References lists of all studies compiled and of other sources were reviewed, yielding an additional 16 studies. In all, 86 studies meeting inclusion criteria were retained. In two studies, the investigators reported findings for both self rated health and cardiovascular disease risk factors; these studies appear in both categories.39,40 Overall the sample of the scoping study comprised 88 multilevel investigations of area effects on health.
Second step
In the second step, studies were coded by one of us (MR) along the following dimensions: citation and study location; health indicator/analytical variable; research design, year of data collection for individual sample; individual sample size and sex/age distribution; individual characteristics adjusted for; area sample size and operational definition; area level exposures; crude between‐area variation; adjusted between‐area variation (for individual level variables); and summary of significant findings of adjusted area effects. LG and TAB cross validated half the studies. The coding scheme and abbreviations are summarised in table 2.
Table 2 Coding scheme and abbreviations.
| Coding dimensions | Explanations | Abbreviations | |||
|---|---|---|---|---|---|
| Citation/location | • Surname of first author and year of publication; country where study undertaken. | Studies reporting data for both SRH and CVD risk factors indicated by asterisks. | |||
| Health indicator/analytic variable | • Self rated health: How would you describe your overall state of health: excellent, very good, good, fair, or poor?• Risk factors for CVD: physical activity, diet, smoking, alcohol consumption, body mass index, overweight and obesity, diabetes, hypertension.• Mortality: all cause and cause specific mortality where individual level data available.• Analytic variable: treatment of the outcome variable was treated. | BMI, body mass index; CVD, cardiovascular disease; CHD: coronary heart disease; HBP, high blood pressure; N'hood, neighbourhood; PA, physical activity.Analytical variables: dichotomous/binomial, 0/1; ordinal/ordered categorical, ord; continuous, cont. | |||
| Design/year of data collection (individual level) | • Cross sectional, longitudinal (follow up), or case–control research design.• Year of data collection at the individual level. | ||||
| Sample size individuals (sex/age range) | • Sample size of individual data (full dataset) and sex distribution and age in years (y) range of the sample. | y, year | |||
| NR, not reported | |||||
| Individual characteristicsadjusted for | • Individual level characteristics adjusted for in multilevel models. | A, age; E, education; ES, employment status (eg, employed, unemployed, retired); I, income; MS, marital status; N'hood, neighbourhood; OS, occupational status (type of work, eg blue collar, professional); PA, physical activity; R/E, race/ethnicity; S, sex; SC, social class; SES, socioeconomic status; SN, social network/support. All other characteristics are nominally identified. | |||
| Sample size of areas | • Sample size and operational definition of areas | ||||
| Area level exposures | • Area level exposure and type—ie, whether they are derived/aggregated from individual level data (eg, census data), or integral—ie, only measurable at the area level (eg, number of parks). | d, Derived variable | |||
| i, Integral variable | |||||
| N'hood, neighbourhood | |||||
| Crude between‐area variation | • Significant between‐area variation unadjusted for individual level characteristics unless otherwise specified.• Reported by variance component and standard error, intraclass correlation coefficient for continuous and dichotomous outcomes, and plausible value range; all others are nominally identified. | ICC, intraclass correlation coefficient; p, p value; SE, standard error; PP, predicted probability; PVR, plausible value range; VC, variance component; NR, not reported; Sign, significant; NS, not significant; SNR, significance not reported. | |||
| (Note: variance component is significant when >1.96 * SE). | |||||
| Adjusted between‐area variation | • Significant between‐area variation adjusted for individual level characteristics unless otherwise specified. | Same as above | |||
| Same as above | |||||
| Significant adjusted area effects | • Significant area effects on health in models adjusting for individual and area level variables (final models) unless otherwise specified.• Cross level interaction: differential area effects across subgroup of individuals. In some cases, authors reported the association of an individual effect on a health indicator in a subset of areas. This was also considered to be a cross level interaction.• Area level interaction: differential effect of an area exposure on a health outcome conditional on another area exposure. | ||||
Third step
In the third step, in order to gauge the accuracy of data compiled, we established interauthor agreement in a random sample of about 25% of studies (n = 21) where the coding of one us (MR) was compared with that of another (TAB) for all coding dimensions except “citation/location” and “summary findings of area effects”. For every dimension, each source of information was equated with one observation. Discrepancies in values reported were considered a disagreement. Overall interauthor agreement was 92.0% (43 disagreements in 513 observations), with agreement ranging between 81.0% and 100% across dimensions. Finally, summary statistics were compiled using the total sample of investigations (n = 88) as the unit of analysis.
Results
Results of study coding appear in the supplementary table, which can be viewed on the journal website (http://www.jech.com/supplemental). Studies are listed alphabetically by surname of first author within each category of health indicator—that is, self rated health (n = 39), cardiovascular morbidity and risk factors (n = 32), and mortality (n = 17). Table 3 presents summary statistics for research design, operational definition of area contours, and exposure as a function of health indicator and time period.
Table 3 Summary statistics for research design and operational definition of area contours and exposure as a function of health indicator and time period.
| Coding dimensions | Self rated health | Cardiovascular morbidity and risk factors | Mortality | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1998–2002 | 2003–2005 | 1998–2005 | 1998–2002 | 2003–2005 | 1998–2005 | 1998–2002 | 2003–2005 | 1998–2005 | 1998–2005 | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Design | ||||||||||
| Cross sectional | 16 (41.0) | 23 (59.0) | 39 (100.0) | 10 (31.3) | 17 (53.1) | 27 (84.4) | 2 (11.8) | 3 (17.6) | 5 (29.4) | 71 (80.7) |
| Longitudinal | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (3.1) | 3 (9.4) | 4 (12.5) | 3 (17.6) | 8 (47.1) | 11 (64.7) | 15 (17.0) |
| Case–control | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (3.1) | 1 (3.1) | 0 (0.0) | 1 (5.9) | 1 (5.9) | 2 (2.3) |
| Total | 16 (41.0) | 23 (59.0) | 39 (100.0) | 11 (34.4) | 21 (65.6) | 32 (100.0) | 5 (29.4) | 12 (70.6) | 17 (100.0) | 88 (100.0) |
| Area definition | ||||||||||
| Administrative/statistical | 14 (35.9) | 19 (48.7) | 33 (84.6) | 11 (34.4) | 20 (62.5) | 31 (96.9) | 5 (29.4) | 10 (58.8) | 15 (88.2) | 79 (89.8) |
| Other | 2 (5.1) | 4 (10.3) | 6 (15.4) | 0 (0.0) | 1 (3.1) | 1 (3.1) | 0 (0.0) | 2 (11.8) | 2 (11.8) | 9 (10.2) |
| Total | 16 (41.0) | 23 (59.0) | 39 (100.0) | 11 (34.4) | 21 (65.6) | 32 (100.0) | 5 (29.4) | 12 (70.6) | 17 (100.0) | 88 (100.0) |
| Area exposures | ||||||||||
| Derived | 15 (26.3) | 20 (35.1) | 35 (89.7) | 8 (21.1) | 17 (44.7) | 25 (78.1) | 5 (22.7) | 12 (54.5) | 17 (100.0) | 77 (87.5) |
| Integral | 5 (8.8) | 13 (22.8) | 18 (46.2) | 3 (7.9) | 8 (29.6) | 11 (34.4) | 2 (9.1) | 3 (13.6) | 5 (29.4) | 34 (38.6) |
| None | 1 (1.8) | 3 (5.3) | 4 (10.3) | 0 (0.0) | 2 (5.3) | 2 (6.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 6 (6.8) |
| Total* | 21 (36.8) | 36 (63.2) | 39 (100.0) | 11 (28.9) | 27 (70.1) | 32 (100.0) | 7 (31.8) | 15 (68.1) | 17 (100.0) | 88 (100.0) |
*Percentages do not add up to 100% because some studies used both derived and integral measures of area exposures.
Year of publication and location of studies
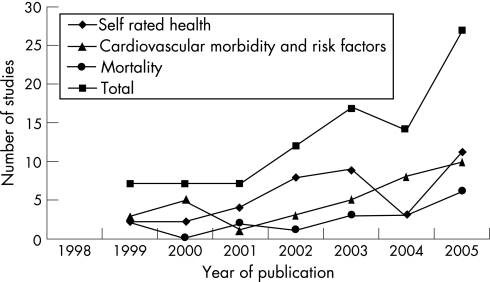
There has been a marked increase in the number of studies published on area effects on self rated health, cardiovascular disease and risk factors, and mortality over the 1998–2005 time period, which almost doubled from 2004 to 2005 (fig 1). Most results are from area effects examined in the USA (n = 37) and the United Kingdom (n = 14), although several studies involved data collected in Canada (n = 10), the Netherlands (n = 8), and Sweden (n = 8).
Figure 1 Trends in publication of multilevel investigations of area effects on self rated health, cardiovascular morbidity and risk factors, and mortality.
Research design and analytical variables
As shown in table 3, a majority of studies (80.7%) had cross sectional designs, whereas others adopted longitudinal designs (17.0%) wherein a majority of studies involved data from a cohort that were matched with vital statistics records to examine associations with mortality and cardiovascular disease at a later time (designated as “follow up” in the supplementary table). Linear multilevel models for continuous and logistic multilevel models for dichotomous outcomes were the most commonly used statistical models, although some analyses were done on models for ordinal outcomes.45,48,57,64,67,76
Individual data: sample size and variables
Sample size of individuals ranged between 57792 and 2 637 628,101 with a median of 8606 individuals. Sixteen per cent of studies had a sample size over 100 000 individuals, but the majority of studies (61%) had a sample size under 10 000.
Most studies controlled for age, sex, SES, and marital status, but some controlled for other individual characteristics such as health related behaviours, medical conditions, perception of area characteristics, social network, and years of residency in the area. Seven studies did not control for individual SES.56,103,104,112,116,121,124 Most studies targeted general populations, but some restricted their focus to men,96,118 older adults,64,88,92 and racial/ethnic groups.54,55,59,80,83,95
Area data: operational definition, sample size, and exposures
As shown in table 3, the majority of studies (89.8%) operationalised areas using statistical (for example, census tracts) or administrative spatial units (for example, city defined neighbourhoods, boroughs, local authorities), or both. One study delimited areas using geographical information systems,107 and others clustered statistical/administrative spatial units based on similarities in terms of SES, demographic composition, and type of area.41,45,46,47,48,76,110,116 Most studies had a two level structure, with individuals nested within areas, though some had more complex structures, including cross classification,110 and three level structures—for example, individuals nested within households within areas63 or individuals nested within several hierarchically structured area units.39,44,58,85,111,119,121
Six studies did not report area level sample size. Among studies for which data were reported, sample size ranged from 956 to 12 344 areas.111 Average within‐area sample size ranged from 1100 to 36 387 individuals.117 Half the studies (52.4%) had an average within‐area sample size of 50 individuals; for 10% of the studies, the within‐area sample size was less than five individuals.
Area level indicators of SES such as deprivation, education, and unemployment were generally aggregates of individual level variables derived from censuses and survey data. Others derived measures of area social context (for example, social cohesion, social capital) by aggregating individuals' perceptions or by the application of ecometric procedures.45,46,48 Over one third of the studies (38.6%) operationalised area exposures using integral measures—that is, features of areas only measurable at an ecological level (table 4). The most commonly used integral measure was income inequality, but other studies relied on characteristics of the social and built environment,50,67,75,92,112 urban sprawl,87 and availability of services and parks.81,88,92,95,106,107
Summary of findings about area effects
Among 47 studies that reported on between‐area variation after adjusting for individual characteristics (minimally age, sex, and SES), 27 studies (57.4%) reported significant between‐area variation for at least one subgroup (defined either by individual or area level characteristics). Although several studies reported one or the other, several did not report variance components for both unadjusted and adjusted models.
Of the 88 studies, six focused on between‐area variation in health only56,60,63,73,89,94 and 82 examined main area effects. Of these studies, six did not report significant direct area effects on health.51,75,93,96,120,122 All other studies reported significant associations between at least one measure of area exposure and at least one health indicator. Significant cross level interactions were observed, indicating that subgroups of individuals may be differentially influenced by certain area characteristics, and by interacting area characteristics. More specifically, effects of area deprivation on poor health, unhealthy behaviours, and risk of mortality were often greater among low SES individuals and among women.
Self rated health
Thirty nine studies examined area effects on self rated health. Four studies focused on between‐area variation only, and 35 were cross sectional investigations of associations between area SES and SRH. In all but two studies,51,75 significant associations were observed between at least one measure of area SES and SRH. More specifically, less favourable area socioeconomic conditions were associated with poorer SRH. Area affluence, positive perceptions of area environment, and higher area levels of collective efficacy and social capital were predictive of better SRH, although area residential stability was associated with poorer health.46,48 One study reported associations between poor SRH and unfavourable area level opportunity structures and social functioning, such as poor physical quality of residential environment, lower political engagement, and lower transport wealth.50 Several studies reported significant effects of social processes, characteristics of the built environment, and perceptions of area characteristics as potential mediating pathways of the association between area deprivation/inequality and SRH.46,48,51,53,76
Cardiovascular morbidity and risk factors
Thirty two studies were investigations of cardiovascular disease and risk factors, of which two examined between‐area variation only.89,94 Some studies employed follow up96,101,102 and case–control research designs,99 but most were cross sectional.
Twenty three studies examined the direct main effect of area deprivation on cardiovascular disease and risk factors. In all studies, at least one measure of area deprivation was associated with a greater risk for cardiovascular disease and with at least one but not all of the risk factors investigated. In general, greater levels of area deprivation and inequality were associated with a greater likelihood of unhealthy dietary habits, smoking, overweight and obesity, and physical inactivity. However, positive associations between affluence and smoking and drinking behaviours were also observed,78,79,104 and in one study, greater state inequality was associated with lower body mass index among white women.80 A greater likelihood of walking was observed in more deprived areas,88,106 but also in more socially cohesive areas.88
In studies where area exposures were operationalised with integral variables, results showed that in less sprawling areas, the risk of being overweight or obese was lower and levels of walking were higher.87 Involvement in physical activity and walking was more likely in areas characterised by greater availability, accessibility, and density of selected services and green spaces.87,88,92,106,107 Dietary habits were associated with the presence of supermarkets and full service restaurants in the area,95 and greater mean distance to alcohol outlets was associated with lower alcohol consumption.98 High convenience store density and lower distance to convenience store were associated with smoking, although this association was not significant in models controlling for area SES.81
Mortality
Seventeen studies examined area effects on mortality, most of which reported results from matching of cohort data with vital statistics.
In all but two studies,120,122 results showed that at least one measure of area SES was associated with all cause and cause specific mortality, such that greater area deprivation and income inequality were significantly associated with greater risk of mortality. When adjusting for area SES, greater area religious affiliation was associated with lower risk of all cause mortality,113 and areas with higher social capital were associated with lower risk of all cause mortality and mortality from heart disease,116 while lower levels of social cohesion were associated with higher risk of all cause mortality.118 Area SES confounded the association between air pollution and all cause and cause specific mortality.115
Discussion
Results of the scoping study showed that the typical methodological approach for multilevel investigations of area effects remains a cross sectional two level study wherein individuals are nested within areas delimited by administrative/statistical spatial units, area level indicators are operationalised using aggregates of individual variables, and direct associations between area exposures and individual level outcomes are adjusted for selected individual characteristics. Various large datasets produced several publications, and it should be noted that findings emanating from the same dataset clearly are not independent.
Over‐reliance on cross sectional research designs raises the critical issue of “self selection”—that is, the fact that people will be selected into residential areas based on individual attributes which are themselves related to health.2 To deal with this issue, one frequently used strategy consists of controlling for individual level variables that are potential confounders of associations between area characteristics and health outcomes. Although useful, this modelling strategy does not overcome problems associated with misspecification resulting from omitted or mismeasured individual level variables, or with lack of statistical power. Addressing these methodological issues rests on crafting longitudinal studies, assessing individual characteristics over the life course, and endeavouring to study cross level interactions and mediating pathways. In this regard, several investigators have emphasised the value of innovative methodological approaches.125
In multilevel studies, there are at least two units of analysis: individuals and areas. However, the attention that is usually devoted to measuring individual attributes is infrequently carried over to areas. For example, in six studies area sample size was not reported, and most studies provided little information on the validity and reliability of area level measures of exposure. When measuring exposure, most studies relied on indicators of area SES derived from censuses and other surveys. Although easily accessible, such measures provide only truncated information about the context of areas,7,17 and may in fact be endogenous to the composition of the areas as they are determined by individual characteristics of residents.2,35 To this end, some studies have tapped into measuring area exposures by means of ecometric procedures.20,23,45,46,48
Most studies employed administrative or statistical spatial units to define area contours, despite their recognised limitations—that is, their potential lack of intrinsic meaning in relation to health.1,5,8,13,14,15 Such limitations are evidenced by variations in the strength and magnitude of area effects on health according to the operational definition of areas.44,58,65,111 We view as particularly innovative recent initiatives to define area contours by delimiting a radius around individual residential location and post codes.107,126,127
Between‐area variation was reported using a variety of statistical parameters including variance components and standard error coefficients, intraclass correlation coefficients for continuous and dichotomous outcomes, plausible value ranges, and others, which precludes comparisons across studies. Furthermore, several studies did not report variance components for either unadjusted or adjusted models. This is unfortunate given the importance of measures of variation for understanding the socio‐spatial patterning of health. There is clearly a need for more detailed and consistent reporting of between‐area variation.24
Power estimation in multilevel studies is complicated by the need to account for the nested structure of the data.128 Only one study reported power calculations.91 Routine reporting of a priori power estimates and post hoc effect size calculations is warranted in multilevel studies.
Although significant area effects were reported in a majority of studies, critical examination of findings revealed inconsistencies within and across studies. For example, one study examined associations between area deprivation and SRH for different operational definitions of area; significant area effects were observed for one type of area only.65 Others have examined effects of area deprivation on several cardiovascular disease risk factors, but observed significant effects only for some of them.78,83 Within individual studies, associations between health and several indicators of area SES were frequently investigated. Although there is probably multicolinearity between measures of area exposures,44,81,119,124 often only certain indicators were significantly associated with the health outcome. This suggests that indicators of area SES such as average income, educational attainment, and income inequality may be tapping into different aspects of the social environment and may be differently associated with specific health outcomes. In addition, a few studies reported no significant area effects. Of concern, findings of the scoping study show that area effects on a specific health indicator may be dependent on the measure of area exposure and the spatial level (area unit) at which associations are investigated. This clearly underscores the importance of conceptualising plausible causal pathways in the search for new knowledge.
The diversity in research designs employed and in the reported results calls attention to the need to move toward a set of reporting guidelines for multilevel investigations of area effects on health. This could include, but not be exclusive to, the following: first, greater details accorded to the description of the nested structure of the database with systematic reporting of sample size at both individual and area levels, and a more explicit discussion of the validity and reliability of area level measures of exposures; second, description of the analytical strategy in such a way that would allow replication of analyses; and third, better description of the between‐cluster variation in health outcomes, both in unadjusted and adjusted models for individual characteristics.24
What is already known
A significant portion of the variation in health is associated with area context independently of individual characteristics.
Limitations
The main limitation of our scoping study pertains to inclusion criteria for studies. A first issue concerns keyword and MeSH searches in the Medline database. Because the area of research emerged only recently, keywords listed by authors do not necessarily correspond to keywords used for searching the literature in the MeSH system. Rather, when searching for “neighbourhood” and “area”, MeSH uses the terms “residence characteristics” and “small area analysis”. Thus if these MeSH terms were not used to classify an article, and if the selected keyword—that is, “neighbourhood”, “area”, “multilevel”, and “hierarchical”—were not specified either in the title or in the abstract of an article, then it would not have been identified. To overcome this problem, more encompassing terms were used and reference lists of all identified articles were reviewed to identify studies. Nonetheless, we acknowledge that some studies may not have been identified with our search strategy.
What this paper adds
This paper is a scoping study of 86 multilevel investigations of area effects on self rated health, cardiovascular morbidity and risk factors, and mortality among adults. Area effects on health, although significant in most studies, often depend on the health outcome studied, the measure of area exposure used, and the spatial scale at which associations are examined.
This highlights the importance conceptualising causal pathways linking area context to health outcomes and devising appropriate methodological strategies in future research.
A second limitation pertains to the exclusion of the literature on area effects on mental health, non‐cardiovascular disease morbidity, paediatric populations, maternal health, and health services utilisation. Several of these studies have used innovative methodological approaches and analytical procedures which could provide the reader with other perspectives on area effects on health.126,127,129,130 It seems relevant to undertake a review of these studies as well to ascertain similarities and differences in the range and types of investigations conducted.
Policy implications
Various health outcomes are influenced by area context although the specific processes through which such influences occur remain unclear. The implementation and evaluation of policy interventions aimed at changing area exposures represents an opportunity to fill this knowledge gap.
Conclusions
The results of the scoping study raise several important issues. One issue pertains to whether or not “true” area effects are concealed by less than adequate methodologies. This may indeed be the case. Several studies showed significant between‐area variation and area effects independently of individual characteristics. These are quite considerable findings given that most studies suffered from methodological limitations and lack of precision when operationalising and measuring context. Significant results garnered with such measurement error probably underestimate effect sizes.
In recent years, increased attention has been directed towards formulating and testing theoretically based pathways between more specific area level measures of exposures and more specific health indicators, such as the effect of the density of food stores on dietary habits, or the effect of urban form on physical activity involvement. These measures of area exposures may be more proximal to influence everyday health related behaviours, thus operating on the pathways between area SES and broader health outcomes.
A second issue is whether or not widely used methodologies for studying areas and health are well suited to the task. Multilevel modelling, without being a panacea, is a suitable statistical procedure that can be used to analyse data with nested sources of variability, while accounting for the non‐independence of within‐cluster observations—that is, addressing the non‐random processes situating people with similar characteristics into certain types of areas.25 As operationalisation of area contours essentially falls back on using readily available spatial units such as census tracts, space is fragmented into seemingly independent area units, therefore ignoring spatial associations between areas. As pointed out by Chaix and colleagues,126 multilevel modelling procedures are based on the assumption that spatial correlations can be reduced to within‐area correlation. For this reason, multilevel approaches may provide only limited information on the spatial distribution of health outcomes and ecological exposures, both when modelling variations and when investigating associations.126 Further debates underscore limitations of multilevel models in detecting causal effects of area exposures on health outcomes.2,15,35,131
Another issue relates to the most promising approaches in this area of research. In recent years, didactic and conceptual tutorials linking social epidemiological concepts to multilevel analysis have been published.24,26,28,132 Innovative methodological approaches and analytical procedures have been applied to examining area effects on health, such as geographical information systems used to operationalise area contours and ecological exposures,107,126,127 development of measurement technology (for example, ecometrics20,22,45,46,48), geostatistical modelling and spatial analysis,47,115,126,133 multilevel path analyses,92 and multilevel structural equation modelling to test potential mediating pathways between area exposures and health outcomes.53,88 Others have underscored the value of developing experimental research designs such as randomised community trials,35 and natural134 and social experiments.135
What seems to emerge from the accumulating evidence on area effects on health is a “specific” research agenda. As argued by other investigators,17,133,136 we espouse the view that the adoption of a specific research approach to examine area effects on health—that is, one that would conceptualise, operationalise, and measure associations between specific health outcomes and specific area exposures—across specific spatial area units may yield more informative evidence of area effects. Adopting a specific approach shows the greatest promise for advancing theoretically based pathways, providing a basis for more precise definitions and measures of ecological exposures, and improved delimitations of area contours.
The supplementary table can be viewed on the journal website, http://www.jech.com/supplemental
Supplementary Material
Acknowledgements
MR is recipient of a Canada graduate scholarships doctoral award and TAB is recipient of a postdoctoral fellowship, both from the Canadian Institutes of Health Research. Both are working under the supervision of LG.
We thank Steven Cummins for his helpful comments on an earlier draft of the manuscript.
Abbreviations
MeSH - medical subject heading
SES - socioeconomic status
SRH - self rated health
Footnotes
The supplementary table can be viewed on the journal website, http://www.jech.com/supplemental
References
- 1.Pickett K E, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health 200155111–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diez Roux A V. Estimating neighborhood health effects: the challenges of causal inference in a complex world. Soc Sci Med 2004581953–1960. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan G A. What's wrong with social epidemiology, and how can we make it better? Epidemiol Rev 200426124–135. [DOI] [PubMed] [Google Scholar]
- 4.Bingenheimer J B. Multilevel models and scientific progress in social epidemiology. J Epidemiol Communiy Health 200559438–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diez Roux A V. Multilevel analysis in public health research. Annu Rev Public Health 200021171–192. [DOI] [PubMed] [Google Scholar]
- 6.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol 200130668–677. [DOI] [PubMed] [Google Scholar]
- 7.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise and measure them? Soc Sci Med 200255125–139. [DOI] [PubMed] [Google Scholar]
- 8.O'Campo P. Invited commentary: advancing theory and methods for multilevel models of residential neighborhoods and health. Am J Epidemiol 20031579–13. [DOI] [PubMed] [Google Scholar]
- 9.Susser M, Susser E. Choosing a future for epidemiology. I. Eras and paradigms. Am J Public Health 199686668–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Susser M, Susser E. Choosing a future for epidemiology: II. From black box to Chinese boxes and eco‐epidemiology. Am J Public Health 199686674–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berkman L F, Kawachi I.Social epidemiology. New York: Oxford University Press, 2000
- 12.Galster G. On the nature of neighbourhood. Urban Stud 2001382111–2124. [Google Scholar]
- 13.Subramanian S V, Jones K, Duncan C. Multilevel methods for public health research. In: Kawachi I, Berkman LF, editors. Neighborhoods and health. New York: Oxford University Press, 200365–111.
- 14.Coulton C J, Korbin J, Chan T.et al Mapping resident's perceptions of neighborhood boundaries: a methodological note. Am J Community Psychol 200129371–383. [DOI] [PubMed] [Google Scholar]
- 15.Subramanian S V. The relevance of multilevel statistical methods for identifying causal neighborhood effects. Soc Sci Med 2004581961–1967. [DOI] [PubMed] [Google Scholar]
- 16.Harris R J, Longley P A. Creating small measures of urban deprivation. Environ Plan A 2002341073–1093. [Google Scholar]
- 17.Cummins S, Macintyre S, Davidson S.et al Measuring neighbourhood social and material context: generation and interpretation of ecological data from routine and non‐routine sources. Health Place 200511249–260. [DOI] [PubMed] [Google Scholar]
- 18.Diez Roux A V. Investigating neighborhood and area effects on health. Am J Public Health 2001911783–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diez Roux A V. The study of group‐level factors in epidemiology: rethinking variables, study designs, and analytical approaches. Epidemiol Rev 200426104–111. [DOI] [PubMed] [Google Scholar]
- 20.Gauvin L, Richard L, Craig C L.et al From walkability to active living potential. An “ecometric” validation study. Am J Prev Med 200528(suppl 2)126–133. [DOI] [PubMed] [Google Scholar]
- 21.Macintyre S, Ellaway A. Ecological approaches: rediscovering the role of the physical and social environment. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press, 2000332–348.
- 22.Raudenbush S W, Sampson R J. Ecometrics: toward a science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociol Methodol 1999291–41. [Google Scholar]
- 23.Sampson R J, Morenoff J D, Gannon‐Rowley T. Assessing “neighborhood effects”: social processes and new directions in research. Annu Rev Sociol 200228443–478. [Google Scholar]
- 24.Merlo J, Chaix B, Yang M.et al A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health 200559443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Snijders T A B, Bosker R J.Multilevel analysis: an introduction to basic and advanced multilevel modelling, 1st edition. Thousand Oaks, CA: Sage, 1999
- 26.Merlo J, Yang M, Chaix B.et al A brief conceptual tutorial on multilevel analysis in social epidemiology: investigating contextual phenomena in different groups of people. J Epidemiol Community Health 200559729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bingenheimer J B, Raudenbush S W. Statistical and substantive inferences in public health: issues in the application of multilevel models. Annu Rev Public Health 20042553–77. [DOI] [PubMed] [Google Scholar]
- 28.Merlo J, Chaix B, Yang M.et al A brief conceptual tutorial on multilevel analysis in social epidemiology: interpreting neighbourhood differences and the effect of neighbourhood characteristics on individual health. J Epidemiol Community Health 2005591022–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blakely T A, Woodward A J. Ecological effects in multi‐level studies. J Epidemiol Community Health 200054367–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Curtis S, Jones I R. Is there a place for geography in the analysis of health inequalities? Sociol Health Illness 199820645–672. [Google Scholar]
- 31.Diez‐Roux A V. The examination of neighbourhood effects on health: conceptual and methodological issues related to the presence of multiple levels of organisations. In: Kawachi I, Berkman LF, editors. Neighborhoods and health. New York: Oxford University Press, 200325–64.
- 32.Duncan C, Jones K, Moon G. Context, composition and heterogeneity: using multi‐level models in health research. Soc Sci Med 19984697–117. [DOI] [PubMed] [Google Scholar]
- 33.Macintyre S, Ellaway A. Neighborhoods and health: an overview. In: Kawachi I, Berkman LF, editors. Neighborhoods and health. New York: Oxford University Press, 200320–42.
- 34.Yen I H, Syme S L. The social environment and health: a discussion of the epidemiologic literature. Annu Rev Public Health 199920287–308. [DOI] [PubMed] [Google Scholar]
- 35.Oakes J M. The (mis)estimation of neighbourhood effects: causal inference for a practicable social epidemiology. Soc Sci Med 2004581929–1952. [DOI] [PubMed] [Google Scholar]
- 36.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005819–32. [Google Scholar]
- 37.Mays N, Roberts E, Popay J. Synthesising research evidence. In: Fulop N, Allen P, Clarke A, Black N, editors. Studying the organisation and delivery of health services: research methods London: Routledge, 2001
- 38.Idler E, Benyamini Y. Self‐rated health and mortality: a review of twenty‐seven community studies. J Health Soc Behav 19973821–37. [PubMed] [Google Scholar]
- 39.Reijneveld S A. Neighbourhood socioeconomic context and self reported health and smoking: a secondary analysis of data on seven cities. J Epidemiol Community Health 200256935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stafford M, Marmot M. Neighbourhood deprivation and health: does it affect us all equally? Int J Epidemiol 200332357–366. [DOI] [PubMed] [Google Scholar]
- 41.Béland F, Birch S, Stoddart G. Unemployment and health: contextual‐level influences on the production of health in populations. Soc Sci Med 2002552033–2052. [DOI] [PubMed] [Google Scholar]
- 42.Blakely T A, Kennedy B P, Glass R.et al What is the lag time between income inequality and health status? J Epidemiol Community Health 200054318–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Blakely T A, Kennedy B P, Kawachi I. Socioeconomic Inequality in Voting Participation and Self‐Rated Health. Am J Public Health 20019199–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blakely T A, Lochner K, Kawachi I. Metropolitan area income inequality and self‐rated health – a multi‐level study. Soc Sci Med 20025465–77. [DOI] [PubMed] [Google Scholar]
- 45.Browning C R, Cagney K A. Neighborhood structural disadvantage, collective efficacy, and self‐rated physical health in an urban setting. J Health Soc Behav 200243383–399. [PubMed] [Google Scholar]
- 46.Browning C R, Cagney K A. Moving beyond poverty: neighborhood structure, social processes, and health. J Health Soc Behav 200344552–571. [PubMed] [Google Scholar]
- 47.Browning C R, Cagney K A, Wen M. Explaining variation in health status across space and time: implications for racial and ethnic disparities in self‐rated health. Soc Sci Med 2003571221–1235. [DOI] [PubMed] [Google Scholar]
- 48.Cagney K A, Browning C R, Wen M. Racial disparities in self‐rated health at older ages: what difference does the neighbourhood make? J Gerontol 200560BS181–S190. [DOI] [PubMed] [Google Scholar]
- 49.Craig N. Exploring the generalisability of the association between income inequality and self‐assessed health. Soc Sci Med 2005602477–2488. [DOI] [PubMed] [Google Scholar]
- 50.Cummins S, Stafford M, Macintyre S.et al Neighbourhood environment and its association with self rated health: evidence from Scotland and England. J Epidemiol Community Health 200559207–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Drukker M, van Os J. Mediators of neighbourhood socioeconomic deprivation and quality of life. Soc Psychiatry Psychiatr Epidemiol 200338698–706. [DOI] [PubMed] [Google Scholar]
- 52.Drukker M, Kaplan C, van Os J. Residential instability in socioeconomically deprived neighbourhoods, good or bad? Health Place 200511121–129. [DOI] [PubMed] [Google Scholar]
- 53.Franzini L, Caughy M, Spears W.et al Neighborhood economic conditions, social processes, and self‐rated health in low‐income neighborhoods in Texas: a multilevel latent variables model. Soc Sci Med 2005611135–1150. [DOI] [PubMed] [Google Scholar]
- 54.Gee G C. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health 200292615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gee G C, Takeuchi D T. Traffic stress, vehicular burden and well‐being: a multilevel analysis. Soc Sci Med 200459405–414. [DOI] [PubMed] [Google Scholar]
- 56.Hopman W M, Berger C, Joseph L.et al Is there regional variation in the SF‐36 scores of Canadian adults? Can J Public Health 200293233–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hou F, Chen J. Neighbourhood low income, income inequality and health in Toronto. Health Rep 20031421–34. [PubMed] [Google Scholar]
- 58.Hou F, Myles J. Neighbourhood inequality, neighbourhood affluence and population health. Soc Sci Med 2005601557–1569. [DOI] [PubMed] [Google Scholar]
- 59.Karlsen S, Nazroo J Y, Stephenson R. Ethnicity, environment and health: putting ethnic inequalities in health in their place. Soc Sci Med 2002551647–1661. [DOI] [PubMed] [Google Scholar]
- 60.Lindstrom M, Moghaddassi M, Merlo J. Individual self‐reported health, social participation and neighbourhood: a multilevel analysis in Malmo, Sweden. Prev Med 200439135–141. [DOI] [PubMed] [Google Scholar]
- 61.Malmstrom M, Sundquist J, Johansson S E. Neighborhood environment and self‐reported health status: a multilevel analysis. Am J Public Health 1999891181–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McCulloch A. Ward‐level deprivation and individual and economic outcomes in the British Household Panel Survey. Environ Plan A 200133667–684. [Google Scholar]
- 63.Pampalon R, Duncan C, Subramanian S V.et al Geographies of health perception in Quebec: a multilevel perspective. Soc Sci Med 1999481483–1490. [DOI] [PubMed] [Google Scholar]
- 64.Patel K V, Eschbach K, Rudkin L L.et al Neighborhood context and self‐rated health in older Mexican Americans. Ann Epidemiol 200313620–628. [DOI] [PubMed] [Google Scholar]
- 65.Reijneveld S A, Verheij R A, Bakker D H. The impact of area deprivation on differences in health: does the choice of the geographical classification matter? J Epidemiol Community Health 200054306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Robert S A, Lee K Y. Explaining race differences in health among older adults: the contribution of community socioeconomic context. Res Aging 200224654–683. [Google Scholar]
- 67.Stafford M, Bartley M, Mitchell R.et al Characteristics of individuals and characteristics of areas: investigating their influence on health in the Whitehall II study. Health Place 20017117–129. [DOI] [PubMed] [Google Scholar]
- 68.Stafford M, Martikainen P, Lahelma E.et al Neighbourhoods and self rated health: a comparison of public sector employees in London and Helsinki. J Epidemiol Community Health 200458772–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stafford M, Cummins S, Macintyre S.et al Gender differences in the associations between health and neighbourhood environment. Soc Sci Med 2005601681–1692. [DOI] [PubMed] [Google Scholar]
- 70.Subramanian S V, Kawachi I, Kennedy B P. Does the state you live in make a difference? Multilevel analysis of self‐rated health in the US. Soc Sci Med 2001539–19. [DOI] [PubMed] [Google Scholar]
- 71.Subramanian S V, Kim D J, Kawachi I. Social trust and self‐rated health in US communities: a multilevel analysis. J Urban Health 200279(suppl 4)S21–S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Subramanian S V, Kawachi I. The association between state income inequality and worse health is not confounded by race. Int J Epidemiol 2003321022–1028. [DOI] [PubMed] [Google Scholar]
- 73.Subramanian S V, Kim D, Kawachi I. Covariation in the socioeconomic determinants of self rated health and happiness: a multivariate multilevel analysis of individuals and communities in the USA. J Epidemiol Community Health 200559664–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Subramanian S V, Acevedo‐Garcia D, Osypuk T L. Racial residential segregation and geographic heterogeneity in black/white disparity in poor self‐rated health in the US: a multilevel statistical analysis. Soc Sci Med 2005601667–1679. [DOI] [PubMed] [Google Scholar]
- 75.Veenstra G. Location, location, location: contextual and compositional health effects of social capital in British Columbia, Canada. Soc Sci Med 2005602059–2071. [DOI] [PubMed] [Google Scholar]
- 76.Wen M, Browning C R, Cagney K A. Poverty, affluence, and income inequality: neighborhood economic structure and its implications for health. Soc Sci Med 200357843–860. [DOI] [PubMed] [Google Scholar]
- 77.Xi G, McDowell I, Nair R.et al Income inequality and health in Ontario: a multilevel analysis. Can J Public Health 200596206–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chaix B, Chauvin P. Tobacco and alcohol consumption, sedentary lifestyle and overweightness in France: a multilevel analysis of individual and area‐level determinants. Eur J Epidemiol 200318531–538. [DOI] [PubMed] [Google Scholar]
- 79.Chaix B, Guilbert P, Chauvin P. A multilevel analysis of tobacco use and tobacco consumption levels in France. Are there any combination risk groups? Eur J Public Health 200414186–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chang V W, Christakis N A. Income inequality and weight status in US metropolitan areas. Soc Sci Med 20056183–96. [DOI] [PubMed] [Google Scholar]
- 81.Chuang Y C, Cubbin C, Ahn D.et al Effects of neighbourhood socioeconomic status and convenience store concentration on individual level smoking. J Epidemiol Community Health 200559568–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cubbin C, Winkleby M A. Protective and harmful effects of neighborhood‐level deprivation on individual‐level health knowledge, behavior changes, and risk of coronary heart disease. Am J Epidemiol 2005162559–568. [DOI] [PubMed] [Google Scholar]
- 83.Diez‐Roux A V, Nieto F J, Caulfield L.et al Neighbourhood differences in diet: the Atherosclerosis Risk in Communities (ARIC) Study. J Epidemiol Community Health 19995355–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Diez‐Roux A V, Link B G, Northridge M E. A multilevel analysis of income inequality and cardiovascular disease risk factors. Soc Sci Med 200050673–687. [DOI] [PubMed] [Google Scholar]
- 85.Duncan C, Jones K, Moon G. Smoking and deprivation: are there neighbourhood effects? Soc Sci Med 199948497–505. [DOI] [PubMed] [Google Scholar]
- 86.Ecob R, Macintyre S. Small area variations in health related behaviours; do these depend on the behaviour itself, its measurement, or on personal characteristics? Health Place 20006261–274. [DOI] [PubMed] [Google Scholar]
- 87.Ewing R, Schmid T L, Killingsworth R.et al Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot 20031847–57. [DOI] [PubMed] [Google Scholar]
- 88.Fisher K J, Li F, Michael Y.et al Neighborhood‐level influences on physical activity among older adults: a multi‐level analysis. J Aging Phys Act 20041245–63. [DOI] [PubMed] [Google Scholar]
- 89.Kairouz S, Nadeau L, Siou G L. Area variations in the prevalence of substance use and gambling behaviours and problems in Québec: a multilevel analysis. Can J Psychiatry 200550591–598. [DOI] [PubMed] [Google Scholar]
- 90.Kavanagh A M, Goller J L, King T.et al Urban area disadvantage and physical activity: a multilevel study in Melbourne, Australia. J Epidemiol Community Health 200559934–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Leyland A H. Socioeconomic gradients in the prevalence of cardiovascular disease in Scotland: the roles of composition and context. J Epidemiol Community Health 200559799–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li F, Fisher K J, Brownson R C.et al Multilevel modelling of built environment characteristics related to neighbourhood walking activity in older adults. J Epidemiol Community Health 200559558–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lindstrom M, Moghaddassi M, Merlo J. Social capital and leisure time physical activity: a population based multilevel analysis in Malmo, Sweden. J Epidemiol Community Health 20035723–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lindstrom M, Moghaddassi M, Bolin K.et al Social participation, social capital and daily tobacco smoking: a population‐based multilevel analysis in Malmo, Sweden. Scand J Public Health 200331444–450. [DOI] [PubMed] [Google Scholar]
- 95.Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents' diets: the Atherosclerosis Risk in Community Study. Am J Public Health 2002921761–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Morris R W, Whincup P H, Lampe F C.et al Geographic variation in incidence of coronary heart disease in Britain: the contribution of established risk factors. Heart 200186277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Robert S A, Reither E N. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Soc Sci Med 2004592421–2434. [DOI] [PubMed] [Google Scholar]
- 98.Scribner R A, Cohen D A, Fisher W. Evidence of a structural effect for alcohol outlet density: a multilevel analysis. Alcohol Clin Exp Res 200024188–195. [PubMed] [Google Scholar]
- 99.Stjärne M K, de Leon A P, Hallqvist J. Contextual effects of social fragmentation and material deprivation on risk of myocardial infarction: results from the Stockholm Heart Epidemiology Program (SHEEP). Int J Epidemiol 200433732–741. [DOI] [PubMed] [Google Scholar]
- 100.Sundquist J, Malmstrom M, Johansson S E. Cardiovascular risk factors and the neighbourhood environment: a multilevel analysis. Int J Epidemiol 199928841–845. [DOI] [PubMed] [Google Scholar]
- 101.Sundquist K, Malmstrom M, Johansson S E. Neighbourhood deprivation and incidence of coronary heart disease: a multilevel study of 2.6 million women and men in Sweden. J Epidemiol Community Health 20045871–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sundquist K, Winkleby M, Ahlen H.et al Neighborhood socioeconomic environment and incidence of coronary heart disease: a follow‐up study of 25,319 women and men in Sweden. Am J Epidemiol 2004159655–662. [DOI] [PubMed] [Google Scholar]
- 103.Tonne C, Schwartz J, Mittleman M.et al Long‐term survival after acute myocardial infarction is lower in more deprived neighbourhoods. Circulation 20051113063–3070. [DOI] [PubMed] [Google Scholar]
- 104.Twigg L, Moon G, Jones K. Predicting small‐area health‐related behaviour: a comparison of smoking and drinking indicators. Soc Sci Med 2000501109–1120. [DOI] [PubMed] [Google Scholar]
- 105.van Lenthe F J, Mackenbach J P. Neighbourhood deprivation and overweight: the GLOBE study. Int J Obes 200226234–240. [DOI] [PubMed] [Google Scholar]
- 106.van Lenthe F J, Brug J, Mackenbach J. Neighbourhood inequalities in physical inactivity: the role of neighbourhood attractiveness, proximity to local facilities and safety in the Netherlands. Soc Sci Med 200560763–775. [DOI] [PubMed] [Google Scholar]
- 107.Wendel‐Vos G C W, Sschuit A J, De Niet R.et al Factors of the physical environment associated with walking and bicycling. Med Sci Sports Exerc 200436725–730. [DOI] [PubMed] [Google Scholar]
- 108.Borrell C, Rodriguez M, Ferrando J.et al Role of individual and contextual effects in injury mortality: new evidence from small area analysis. Inj Prev 20028297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bosma H, van de Mheen H D, Borsboom G J J M.et al Neighborhood socioeconomic status and all‐cause mortality. Am J Epidemiol 2001153363–371. [DOI] [PubMed] [Google Scholar]
- 110.Curtis S, Southall H, Congdon P.et al Area effects on health variation over the life‐course: analysis of the longitudinal study sample in England using new data on area of residence in childhood. Soc Sci Med 20045857–74. [DOI] [PubMed] [Google Scholar]
- 111.Franzini L, Spears W. Contributions of social context to inequalities in years of life lost to heart disease in Texas, USA. Soc Sci Med 2003571847–1861. [DOI] [PubMed] [Google Scholar]
- 112.Hembree C, Galea S, Ahern J.et al The urban built environment and overdose mortality in New York City neighbourhoods. Health Place 200511147–156. [DOI] [PubMed] [Google Scholar]
- 113.Jaffe D H, Eisenbach Z, Neumark Y D.et al Does living in a religiously affiliated neighborhood lower mortality? Ann Epidemiol 200515804–810. [DOI] [PubMed] [Google Scholar]
- 114.Jaffe D H, Eisenbach Z, Neumark Y D.et al Individual, household and neighborhood socioeconomic status and mortality: a study of absolute and relative deprivation. Soc Sci Med 200560989–997. [DOI] [PubMed] [Google Scholar]
- 115.Jerrett M, Burnett R T, Ma R.et al Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology 200516727–736. [DOI] [PubMed] [Google Scholar]
- 116.Lochner K A, Kawachi I, Brennan R T.et al Social capital and neighborhood mortality rates in Chicago. Soc Sci Med 2003561797–1805. [DOI] [PubMed] [Google Scholar]
- 117.Marinacci C, Spadea T, Biggeri A.et al The role of individual and contextual socioeconomic circumstances on mortality: analysis of time variations in a city of North West Italy. J Epidemiol Community Health 200458199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Martikanen P, Kauppinen T M, Valkonen T. Effect of the characteristics of neighbourhoods and the characteristics of people on cause specific mortality: a register based follow up study of 252 000 men. J Epidemiol Community Health 200357210–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mohan J, Twigg L, Barnard S.et al Social capital, geography and health: a small‐area analysis for England. Soc Sci Med 2005601267–1283. [DOI] [PubMed] [Google Scholar]
- 120.Roos L L, Magoon J, Gupta S.et al Socioeconomic determinants of mortality in two Canadian provinces: multilevel modelling and neighborhood context. Soc Sci Med 2004591435–1447. [DOI] [PubMed] [Google Scholar]
- 121.Subramanian S V, Chen J T, Rehkopf D H.et al Racial disparities in context: a multilevel analysis of neighborhood variations in poverty and excess mortality among black populations in Massachusetts. Am J Public Health 200595260–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Veugelers P J, Yip A M, Kephart G. Proximate and contextual socioeconomic determinants of mortality: multilevel approaches in a setting with universal health care coverage. Am J Epidemiol 2001154725–732. [DOI] [PubMed] [Google Scholar]
- 123.Waitzman N J, Smith K R, Stroup A. The direct and indirect effects of metropolitan area inequality on mortality a hierarchical analysis. Ann NY Acad Sci 1999896347–349. [DOI] [PubMed] [Google Scholar]
- 124.Yen I H, Kaplan G A. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County Study. Am J Epidemiol 1999149898–907. [DOI] [PubMed] [Google Scholar]
- 125.Oakes J M, Johnson P H. Propensity score matching for social epidemiology. In: Oakes JM, Kaufman JS, editors. Methods in social epidemiology. San Francisco: Jossey‐Bass, 2006364–386.
- 126.Chaix B, Merlo J, Subramanian S V.et al Comparison of a spatial perspective with the multilevel analytical approach in neighborhood studies: the case of mental and behavioral disorders due to psychoactive substance use in Malmö, Sweden, 2001. Am J Epidemiol 2005162171–182. [DOI] [PubMed] [Google Scholar]
- 127.Propper C, Jones K, Bolster A.et al Local neighbourhood and mental health: evidence from the UK. Soc Sci Med 2005612065–2083. [DOI] [PubMed] [Google Scholar]
- 128.Raudenbush S W, Bryk A.Hierarchical linear models: applications and data analysis methods, 2nd edition. Newbury Park, CA: Sage, 2002
- 129.Frohlich K L, Potvin L, Gauvin L.et al. Youth smoking initiation: disentangling context from composition, Health Place 20028155–166. [DOI] [PubMed] [Google Scholar]
- 130.Drukker M, Kaplan C, Feron F.et al Children's health‐related quality of life, neighbourhood socio‐economic deprivation and social capital: a contextual analysis. Soc Sci Med 200357825–841. [DOI] [PubMed] [Google Scholar]
- 131.Oakes M J. Causal inference and the relevance of social epidemiology. Soc Sci Med 2004581969–1971. [DOI] [PubMed] [Google Scholar]
- 132.Merlo J, Chaix B, Ohlsson H.et al A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health 200660290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chaix B, Rosvall M, Lynch J.et al Disentangling contextual effects on cause‐specific mortality in a longitudinal 23‐year follow‐up study: impact of population density or socioeconomic environment? Int J Epidemiol 200635633–643. [DOI] [PubMed] [Google Scholar]
- 134.Cummins S, Pettirew M, Higgins C.et al Large scale food retailing as an intervention for diet and health: quasi‐experimental evaluation of a natural experiment. J Epidemiol Community Health 2005591035–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Levental T, Brooks‐Gunn J. Moving to opportunity: an experimental study of neighborhood effects on mental health. Am J Public Health 2003931576–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Galea S, Ahern J. Invited commentary: Considerations about specificity of associations, causal pathways, and heterogeneity in multilevel thinking. Am J Epidemiol 20061631079–1082. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.