Abstract
Objective
To investigate diagnosis‐specific sick leave as a risk marker for subsequent disability pension.
Design
A prospective population based cohort study. Exposure to a new medically certified sick leave episode of more than seven days by diagnosis during 1985 was examined in relation to incident cause‐specific disability pension through 1996.
Participants
The total non‐retired population of one Swedish county aged 16 to 49 years, alive and not in receipt of a disability pension at the end of 1985 (176 629 persons; 51% men).
Main results
To eliminate confounding by sick leaves that translate into a disability pension, the follow up period for disability pension was started five years after the assessment of sick leave. After adjustment for demographic characteristics, the risk of disability pension from mental disorders was 14.1 times higher (95% confidence interval (CI), 12.1 to 16.4) for those with sick leave for mental disorders than for those with no sick leave. The corresponding hazard ratio for sick leave and disability pension within diagnostic category was 5.7 (95% CI, 5.3 to 6.2) for musculoskeletal diseases and 13.0 (7.7 to 21.8) for gastrointestinal diseases. Irrespective of diagnoses, the hazard ratio for sick leave and disability pension was 3.0 (2.9 to 3.1).
Conclusions
Sick leave may provide an important risk marker for identifying groups at high risk of a disability pension, especially for psychiatric diagnoses.
Keywords: disability, pensions, ill health retirement, sickness absence, mental health
Owing to an upward trend in life expectancy, the demographic structure in industrialised countries is changing and it is projected that by 2020 the average life expectancy will be between 85 and 90 years.1 In contrast, the economically active proportion of the population has fallen, with particularly large decreases between the beginning of the 1980s and the mid‐1990s, especially among older age groups.2 These trends may result in a “pensions crisis”, with the number of persons in employment remaining below that required to provide the financial support expected by those out of the labour force.3,4 In this situation, the mounting costs of long term disability pensions (that is, incapacity benefits and ill health retirements) caused by increasing demands on healthcare services, the economy, and the future are unlikely to be sustainable.
Although the reduction of early exit from the labour force is considered an essential element in preventing the impending pensions crisis, little information is available about at‐risk groups to whom these interventions should be targeted.5 Recent studies have shown strong associations between rate of sickness absence and subsequent risk of disability pension.6,7,8,9,10,11 However, at least three issues compromise the value of this evidence. First, there is a lack of analyses on diagnosis‐specific associations between sick leave and disability pension—such information may assist prevention, as interventions are likely to be diagnosis‐specific and may be more effective for certain diagnoses. Second, in many studies the disability pension follow up began immediately after the sick leave assessment period, meaning that sick leaves that run into a disability pension (precipitating sick leaves) may have inflated observed associations. Third, most studies were based on selected or small samples.
We examined whether medically certified sick leave episodes of more than seven days can be used to predict subsequent receipt of a disability pension using data from a large population that included diagnoses for sick leaves and disability pensions. To determine whether sick leave represents a risk marker sufficiently distant to provide time to intervene and potentially prevent early disability, we focused on people aged less than 50 years at study entry, a population considerably younger than the official retirement age. Additionally, in some analyses, we began the disability pension follow up five years after the sick leave assessment period to minimise confounding by precipitating sick leave.
Methods
Study population
Data were drawn from an 11 year follow up of the entire working age population in the County of Östergötland, Sweden on 31 December 1984 (n = 245 704). The present study included all non‐retired persons aged 16 to 49 years at study entry, who were still alive and not in receipt of a disability pension at the end of 1985 (n = 176 629; 90 588 men and 86 041 women). Data on demographic characteristics, new medically certified sick leave episodes longer than seven days in 1985, and disability pensions from 1986 to 1996 were linked using participants' personal identification numbers (a unique number assigned to each Swedish inhabitant).
Sickness absence
All Swedish residents over 16, including the unemployed, qualify for sickness insurance entitling them to compensation for work incapacity because of disease or injury. Self certification is accepted for the first seven days, after which a sickness certificate from a physician is required. There is no limit to the duration of a sick leave episode.
The exposure of interest in the present study was the first medically certified sick leave episode of more than seven days that begun in 1985. For diagnosis‐specific analyses, the first medically certified sick leave episode of more than seven days was determined for each diagnostic category. Diagnoses for these episodes were manually retrieved from the sickness certificates and were categorised into 18 diagnostic groups from the International Classification of Diseases, 9th edition (ICD‐9). A validity check showed that coding of the diagnoses was correct in 98.4% of the cases.12
Disability pensions
Disability benefit schemes—for example, incapacity benefit in the United Kingdom and social security disability insurance in the USA—vary between countries. Under the Swedish system disability pensions can be granted to persons aged 16 to 65 if their work disability is long term or permanent. A disability pension should be considered after 12 months of sickness absence, but sick leave episodes preceding a disability pension are sometimes longer. For disability pension recipients, benefits amount to at least 65% of lost income. Dates and diagnoses for all disability pensions granted during the 1 January 1986 to the 31 December 1996 were obtained from the National Social Insurance Board. Disability pension diagnoses were also categorised according to ICD‐9.
Other measurements
Age on the 31 December 1984, sex, and marital status in 1985 were obtained from the Swedish National Social Insurance Board and were used as covariates. Dates of deaths up to the 31 December 1996 were obtained from the Swedish National Board of Health and Welfare.
Statistical analysis
Each individual in the study population was followed from the 1 January 1986 until either receipt of a disability pension, death, or the end of the study period on the 31 December 1996. Age was divided into four categories (16–19, 20–29, 30–39, 40–49 years). Differences in prevalence of sick leave by age group, sex, and marital status were tested by logistic regression models, and the corresponding differences in disability pension incidence with Cox proportional hazards models. In Cox models participants with no new sick leave episodes of more than seven days in 1985 were used as the reference category. Hazard ratios for the risk of a disability pension during 1986–1996 and during 1991–1996 (those with follow up less than five years excluded, n = 4835) were adjusted for age, sex, and marital status except in analyses using these variables for stratification. Stratified analyses were run by sex and age group (16–30 v 30–49), the first analyses being adjusted for age and marital status and the later analyses for sex and marital status. We illustrated the effect of sick leave on the probability of incident disability pension by sex and age group using Kaplan–Meier curves, tested with the log rank p value. The analyses were conducted using the SAS 9.1 program.
Results
Population characteristics
In 1985, 17.8% of participants had a new sick leave episode of more than seven days (table 1). Older participants, who were more likely to be married, and women had higher risks of a new sick leave episode. A disability pension was granted to 7.1% of participants during the mean follow up of 10.6 (SD 1.5) years. Risk of a disability pension similarly was greater among participants who were older, married, and women.
Table 1 Incidence of medically certified sick leave episodes of more than seven days and of disability pension by baseline characteristics in men and women aged 16 to 49 years at baseline.
| Baseline characteristic | No of participants | Incidence of sick leave in 1985 | Incidence of disability pension between 1986 and 1996 | ||
|---|---|---|---|---|---|
| No of cases | % | No of cases | Rate per 10 000 person years | ||
| Age group, years | |||||
| 16–19 | 22 967 | 2 236 | 9.7 | 261 | 10.4 |
| 20–29 | 51 762 | 9 676 | 18.7 | 1 588 | 28.3 |
| 30–39 | 56 092 | 10 604 | 19.0 | 3 894 | 65.4 |
| 40–49 | 45 808 | 8 904 | 19.4 | 6 797 | 145.7 |
| Sex | |||||
| Men | 90 588 | 13 948 | 15.4 | 4 951 | 51.2 |
| Women | 86 041 | 17 508 | 20.4 | 7 589 | 83.7 |
| Marital status | |||||
| Married | 79 099 | 14 323 | 18.1 | 7 083 | 85.0 |
| Other | 97 530 | 17 133 | 17.6 | 5 457 | 52.4 |
| All | 176 629 | 31 456 | 17.8 | 12 540 | 66.9 |
Diagnoses of sick leaves and disability pension
The most common diagnoses for sick leave were musculoskeletal diseases (28.2%), respiratory diseases (25.5%), injury and poisoning (16.7%), infectious and parasitic disease (9.2%), and mental disorders (8.0%) (table 2). Of these, musculoskeletal diseases and mental disorders were also common underlying causes for disability pension (rate per 10 000 person years, 35.9 and 13.1 respectively). The incidence of disability pension resulting from musculoskeletal diseases (per 10 000 person years) was 22.3 during the first five years of follow up and 48.4 during the subsequent follow up. The corresponding incidence estimates for disability pension for mental disorders were 10.9 and 15.1.
Table 2 Diagnoses of the first medically certified sick leave episodes of more than seven days in 1985 and incident disability pensions between 1986 and 1996 in men and women aged 16 to 49 years at baseline.
| Diagnosis | Incidence of sick leave in 1985 | Incidence of disability pension between 1986 and 1996 | ||
|---|---|---|---|---|
| No of | Per cent of all participants | No of | Rate per 10 000 person years | |
| cases* | (% of cases)* | cases | ||
| I Infectious and parasitic diseases | 2 883 | 1.6 (9.2) | 90 | 0.5 |
| II Neoplasms | 282 | 0.2 (0.9) | 243 | 1.3 |
| III Endocrine, nutritional, and metabolic diseases | 266 | 0.2 (0.9) | 251 | 1.3 |
| IV Diseases in blood and blood forming organs | 71 | 0.0 (0.2) | 10 | 0.1 |
| V Mental disorders | 2 518 | 1.4 (8.0) | 2 448 | 13.1 |
| VI Diseases of nervous system and sense organs | 1 194 | 0.7 (3.8) | 619 | 3.3 |
| VII Diseases of the circulatory system | 939 | 0.5 (3.0) | 758 | 4.0 |
| VIII Diseases of the respiratory system | 8 032 | 4.6 (25.5) | 331 | 1.8 |
| IX Diseases of gastrointestinal system | 2 275 | 1.3 (7.2) | 235 | 1.3 |
| X Diseases of genitourinary system | 516 | 0.3 (1.6) | 52 | 0.3 |
| XI Complications of pregnancy, childbirth, and the puerperium† | 2 903 | 1.6 (9.2) | 0 | 0.0 |
| XII Diseases of skin and subcutaneous tissue | 855 | 0.5 (2.7) | 170 | 0.9 |
| XIII Diseases of musculoskeletal system and connective tissue | 8 870 | 5.0 (28.2) | 6 727 | 35.9 |
| XVI Symptoms, signs, and ill defined conditions | 1 288 | 0.7 (4.1) | 99 | 0.5 |
| XVII Injury and poisoning | 5 241 | 3.0 (16.7) | 423 | 2.3 |
There were no sick leave episodes resulting from categories XIV (congenital anomalies) and XV (conditions originating in the perinatal period).
*Total percentage adds up >100% as the same persons can have more than one sick leave.
†Only for women (n = 86 041).
Sick leave as a predictor of disability pension
A medically certified sick leave episode for any cause was associated with a 3.3‐fold increased risk of a disability pension (all cause) during the entire follow up period. Greater excess risks of a disability pension were seen for those with sick leave because of the following diagnoses: mental disorders; musculoskeletal diseases; diseases of genitorurinary or gastrointestinal systems; symptoms, signs and ill defined conditions; and diseases of the nervous system and sense organs (the range of hazard ratios varied from 3.82 (95% confidence interval (CI), 3.4 to 4.3) to 6.19 (5.8 to 6.7)). The hazard ratios for a disability pension for sick leave resulting from other diagnoses were lower than that for all cause sick leave—for example, for respiratory diseases the hazard ratio was 3.00 (2.8 to 3.2).
The associations of all cause and diagnosis‐specific sick leave with incident all cause disability pension were stronger during the first five years of follow up (hazard ratio range 4.18 to 8.68) than subsequently (range 3.00 to 4.99) (table 3). This would be expected, as sick leaves that translate into a disability pension are likely to confound associations in the early rather than the late phases of follow up.
Table 3 Age, sex, and marital status adjusted Cox proportional hazards models of incident all cause disability pension with two follow up periods by sick leave of more than seven days at baseline*.
| Diagnosis for sick leave in 1985 | Disability pension during 1986–1990 | Disability pension during 1991–1996 | ||
|---|---|---|---|---|
| No of participants (No of disability pension cases) | Hazard ratio (95% CI) | No of participants (No of disability pension cases) | Hazard ratio (95% CI) | |
| Participants with no new sick leave | 145 173 (1 943) | 1.00 | 142 570 (5 283) | 1.00 |
| Participants with sick leave from a specific diagnosis | ||||
| V Mental disorders | 2 518 (358) | 8.68 (7.7 to 9.7) | 2 107 (421) | 4.99 (4.5 to 5.5) |
| XIII Diseases of musculoskeletal system and connective tissue | 8 870 (971) | 6.94 (6.4 to 7.5) | 7 840 (1 250) | 4.10 (3.9 to 4.4) |
| X Diseases of genitourinary system | 516 (33) | 4.25 (3.0 to 6.0) | 476 (74) | 4.16 (3.3 to 5.2) |
| IX Diseases of gastrointestinal system | 2 275 (150) | 4.57 (3.9 to 5.4) | 2 093 (292) | 3.87 (3.4 to 4.3) |
| XVI Symptoms, signs, and ill defined conditions | 1 288 (95) | 4.83 (3.9 to 5.9) | 1 184 (158) | 3.57 (3.0 to 4.2) |
| VI Diseases of nervous system and sense organs | 1 194 (93) | 4.71 (3.8 to 5.8) | 1 091 (153) | 3.42 (2.9 to 4.0) |
| All cause sick leave | 31 456 (1 966) | 4.18 (3.9 to 4.5) | 29 224 (3 348) | 3.00 (2.9 to 3.1) |
*Findings present only for sick leave categories that predicted disability pension more strongly than all cause sick leave. Analyses for each diagnostic category include participants with sick leave from the specific diagnosis (exposure group) and those with no new sick leave (the reference), but exclude participants with sick leave from other diagnoses.
CI, confidence interval.
Table 4 presents associations between diagnosis‐specific sick leaves and diagnosis‐specific disability pensions after excluding the first five years of follow up. Associations within the same diagnostic category were particularly strong for several diagnoses. For example, the hazard ratio for a disability pension because of a mental disorder was 14.0 times higher for those with sick leave for mental disorders than for those with no sick leave. The corresponding hazard ratios were 5.7 for musculoskeletal disorders, 13.0 for gastrointestinal diseases, and 7.7 for diseases of the nervous system and sense organs.
Table 4 Age, sex, and marital status adjusted hazard ratios for incident, cause specific disability pension during 1991–1996 associated with sick leave of more than seven days in 1985 of the same diagnosis*.
| No of participants (No of disability pension cases) | Hazard ratio (95% CI) | |
|---|---|---|
| Participants with no new sick leave | 142 570 (†) | 1.00 |
| Participants with sick leave from a specific diagnosis | ||
| V Mental disorders | 2 107 (207) | 14.05 (12.1 to 16.4) |
| XIII Diseases of musculoskeletal system and connective tissue | 7 840 (921) | 5.70 (5.3 to 6.2) |
| X Diseases of genitorurinary system | 476 (0) | – |
| IX Diseases of gastrointestinal system | 2 093 (17) | 12.99 (7.7 to 21.8) |
| XVI Symptoms, signs and ill defined conditions | 1 184 (2) | – |
| VI Diseases of nervous system and sense organs | 1 091 (19) | 7.72 (4.8 to 12.3) |
*Findings present only for sick leave categories that predicted disability pension more strongly than all cause sick leave. Analyses for each diagnostic category include participants with sick leave from the specific diagnostic category (exposure group) and those with no new sick leave (the reference), but exclude participants with sick leave from other diagnoses.
†937 for disability pension resulting from mental disorders, 2772 from diseases of musculoskeletal system and connective tissue, 90 from diseases of gastrointestinal system, and 296 from diseases of nervous system and sense organs.
CI, confidence interval.
The probability that an individual subsequently became the recipient of a disability pension because of a mental disorder was 18.2% for those with sick leave for mental disorders but only 1.0% for those with no sick leave (based on data covering the entire follow up period). The corresponding percentages were 18.9% and 2.5% for sick leaves and disability pensions for musculoskeletal diseases, 1.6% and 0.1% for gastrointestinal diseases, and 3.4% and 0.3% for diseases of the nervous system and sense organs.
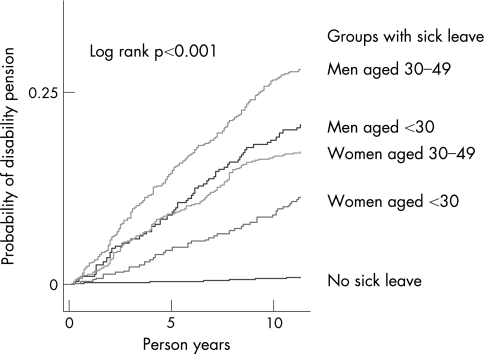
Analysis of mental disorders stratified by age and sex
Figure 1 shows that the time to first disability pension from mental disorders across the entire follow up period was strongly associated with sick leave due to mental disorders. Within those with such sick leaves, there was separation of the survival curves by sex and age. Among those aged 30–49 years, the association between sick leave and disability pension was significantly stronger among men (hazard ratio = 16.9 (95% CI, 13.2 to 21.6)) than among women (hazard ratio = 9.5 (7.2 to 12.4)) (p for interaction = 0.0007 with five year wash out period). For those under 30 years of age, no significant sex difference was found (hazard ratio = 22.2 (15.4 to 32.0) among men, and 14.8 (9.7 to 22.5) among women) (p for interaction = 0.18).
Figure 1 Cumulative hazard function for disability pension for mental disorders by sick leave for mental disorder, sex, and age.
Discussion
In the non‐retired population aged 16–49 of Östergötland, Sweden, sick leave for mental disorders predicted a 14‐fold excess risk of disability pension for mental disorders. The corresponding risk ratio for sick leave and disability pension was 13 for gastrointestinal diseases and less than 6 for musculoskeletal diseases. These excess risks were not attributable to disability pensions immediately precipitated by sick leave, because the increased risk was seen after excluding pensions during the first five years of follow up. To our knowledge, this is the first large scale investigation to examine cause‐specific sick leave as an early risk marker for disability pension across a range of diagnoses.
What this study adds
Although disability pensions make a significant contribution to the impending pensions crisis in industrialised countries, the early identification of groups at risk of a disability pension has been little studied.
Medically certified sick leave episodes of more than seven days were highly predictive of a disability pension five years later in a general population under 50 years of age.
The associations between sick leave and disability pension were particularly strong within diagnostic categories for mental disorders.
Previous work in this field suggests that the predictors of disability pension include societal factors, such as benefit rules and practices, individual factors such as age, social class, and unemployment, and health measures such as self rated health and previous sick leave. However, associations between previous sick leave and disability pension have generally been stronger than those for most of the other predictors, for which the risk ratios typically do not exceed 4.13,14,15,16,17,18 In common with our findings, this emphasises the primacy of sick leave as a risk marker for disability pension.
Policy implications
Use of sick leave for the detection of groups at high risk of a disability pension may provide time to implement successful interventions to reduce early exit from the workforce, especially for mental disorders.
Although the association between sick leave for mental disorders and disability pension for mental disorders was more pronounced among men than women aged 30–49, the association nevertheless was very strong in both sexes and all age groups. This finding is of particular importance given the existing need to reverse the increase in disability pensions granted for these diagnoses in Scandinavian and other European countries.19,20,21 The majority of cases of sick leave for mental disorders result from depression, which in most cases is amenable to suitable treatment. Thus the exceptionally high excess risk of disability pension among individuals with sick leave for mental disorders may indicate that measures to prevent early exit from the labour force on mental health grounds have not been optimal. Although primary prevention is the method of choice for reducing sick leave and disability pension incidence in the longer term, our findings suggest a current need to improve treatment and rehabilitation. Examples of potential interventions that deserve further research include enhanced coordination in the process of prevention, treatment, and rehabilitation, and changes in employees' and employers' attitudes towards increased recognition of the therapeutic role of work in the rehabilitation process.11,19,22,23,24
Musculoskeletal diseases were the most common diagnostic group for both sick leave and disability pension. The excess risk associated with an adjusted hazard ratio of just under 6 is roughly in agreement with some previous smaller scale studies, but considerably lower than the excess risks reported in studies that have included precipitating sickness absences.6,9 We found that the probability of a person with musculoskeletal sick leave becoming the recipient of a disability pension because of musculoskeletal disorders was about equal to the probability a person with sick leave for mental disorders becoming the recipient of a disability pension because of mental disorders. However, a greater proportion of those with no sick leave ended up on a disability pension for musculoskeletal disorders than for mental health disorders. Although sick leave for musculoskeletal disorders is less specific than for mental disorders as an identifier of subsequent disability pension for the same diagnosis, it could nonetheless offer opportunities for intervention given the predominance of musculoskeletal disability pensions. The use of the occurrence of musculoskeletal sick leaves as a risk marker of musculoskeletal disability may benefit substantially from complementary information on other risk factors, such as the duration of sick leave and the severity of musculoskeletal complaints.25
Finally, we found strong associations between sick leave and disability pension for diseases of the gastrointestinal system and those of the nervous system and sense organs. The size of these diagnostic groups is small and, while targeted interventions may help individuals, the overall burden of disability pensions from these diagnoses is low.
Methodology
This study benefited from a large population based sample with relatively long follow up that provided sufficient power for risk estimation, and the use of high quality national registry data. However, data on socioeconomic position and unemployment (two predictors of sick leave and disability pension) were unavailable in the present study. Major confounding is unlikely, however, as the predictive power of sick leave was substantially higher than that for either of these potential confounders.7,11,26
The measure of sick leave used in the present study had two limitations. First, we measured sick leave during one particular year. As sick leave can be very variable, a longer assessment period would probably have increased the sensitivity of sick leaves as a risk marker. Second, our records covered only new sick leave episodes and therefore sick leaves that began before study entry were misclassified into the category of no sick leave. Given these two drawbacks, our findings are likely to represent underestimations of the actual associations.
Although the present study was limited to one county in Sweden, Östergötland is representative of the southern part of Sweden, where over 80% of the population reside. However, replication in other countries would be important to determine whether the associations are generalisable across different pension schemes and population characteristics in contemporary settings.
Policy implications
Costs of disability pensions are steadily growing in many European countries and in the USA.4,20,27 In the UK, for example, expenditure on disability pensions accounted for 0.9% of gross domestic product (GDP) in 1980, but two decades later had reached 2.6% of GDP.4 Corresponding upward trends have been seen elsewhere, with particularly large relative increases in pensions for mental disorders.20,21 Growing numbers of younger disability pension recipients are a particular problem as they may be beneficiaries for decades.
Our findings from a population considerably younger than the official retirement age indicate that data on medically certified sick leave episodes can be used to identify effectively “at risk” groups for disability pension, in particular for mental disorder. The use of information on sick leave may improve the effectiveness of early interventions by policy makers, employers, and physicians.
Footnotes
Funding: This study was financially supported by the Swedish Council for Working Life and Social Research and AFA Insurance. MK and JV were supported by the Academy of Finland (projects 105195 and 117604) and the Finnish Work Environment Foundation. JEF was supported by the MRC (grant number G8802774).
Competing interests: None.
Ethical approval: The study was approved by the Swedish National Data Inspection Board and the local research ethics committee.
References
- 1.Oeppen J, Vaupel J W. Demography. Broken limits to life expectancy. Science 20022961029–1031. [DOI] [PubMed] [Google Scholar]
- 2.Blöndal S, Scarpetta S.The retirement decision in OECD countries. Paris: OECD Publishing, 1999, doi: 10. 1787/565174210530.
- 3.Martin P P, Weaver D A. Social security: a program and policy history. Soc Secur Bull 2005661–15. [PubMed] [Google Scholar]
- 4.OECD Transforming disability into ability: policies to promote work and income security for disabled people. Paris: OECD Publishing, 200316–176.
- 5.Poole C J, Bass C M, Sorrell J E.et al Ill‐health retirement: national rates and updated guidance for occupational physicians. Occup Med (Lond) 200555345–348. [DOI] [PubMed] [Google Scholar]
- 6.Borg K, Hensing G, Alexanderson K. Risk factors for disability pension over 11 years in a cohort of young persons initially sick‐listed with low back, neck, or shoulder diagnoses. Scand J Public Health 200432272–278. [DOI] [PubMed] [Google Scholar]
- 7.Gjesdal S, Ringdal P R, Haug K.et al Predictors of disability pension in long‐term sickness absence: results from a population‐based and prospective study in Norway 1994–1999. Eur J Public Health 200414398–405. [DOI] [PubMed] [Google Scholar]
- 8.Enthoven P, Skargren E, Carstensen J.et al Predictive factors for 1‐year and 5‐year outcome for disability in a working population of patients with low back pain treated in primary care. Pain 2006122137–144. [DOI] [PubMed] [Google Scholar]
- 9.Kivimäki M, Forma P, Wikstrom J.et al Sickness absence as a risk marker of future disability pension: the 10‐town study. J Epidemiol Community Health 200458710–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Virtanen M, Kivimäki M, Vahtera J.et al Sickness absence as a risk factor for job termination, unemployment, and disability pension among temporary and permanent employees. Occup Environ Med 200663212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alexanderson K, Norlund A. eds. Sickness absence ‐ causes, consequences, and physicians' sickness certification practices: A systematic review, Scand J Public Health 200432(suppl 63)1–263.14757541 [Google Scholar]
- 12.Alexanderson K.Sickness absence in a Swedish county, with reference to gender, occupation, pregnancy and parenthood [PhD thesis]. Linköpings Universitet 19953–103.
- 13.Mansson N O, Rastam L, Eriksson K F.et al Socioeconomic inequalities and disability pension in middle‐aged men. Int J Epidemiol 1998271019–1025. [DOI] [PubMed] [Google Scholar]
- 14.Mansson N O, Rastam L. Self‐rated health as a predictor of disability pension and death – a prospective study of middle‐aged men. Scand J Public Health 200129151–158. [PubMed] [Google Scholar]
- 15.Biering‐Sorensen F, Lund J, Hoydalsmo O J.et al Risk indicators of disability pension. A 15 year follow‐up study. Dan Med Bull 199946258–262. [PubMed] [Google Scholar]
- 16.Claussen B. Restricting the influx of disability beneficiaries by means of law: experiences in Norway. Scand J Soc Med 1998261–7. [DOI] [PubMed] [Google Scholar]
- 17.Holte H H, Tambs K, Bjerkedal T. Manual work as predictor for disability pensioning with osteoarthritis among the employed in Norway 1971–1990. Int J Epidemiol 200029487–494. [PubMed] [Google Scholar]
- 18.Sanderson P L, Todd B D, Holt G R.et al Compensation, work status, and disability in low back pain patients. Spine 199520554–556. [DOI] [PubMed] [Google Scholar]
- 19.Layard R. The case for psychological treatment centres. BMJ 20063321030–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moncrieff J, Pomerleau J. Trends in sickness benefits in Great Britain and the contribution of mental disorders. J Public Health Med 20002259–67. [DOI] [PubMed] [Google Scholar]
- 21.Salminen J K, Saarijarvi S, Raitasalo R. Depression and disability pension in Finland. Acta Psychiatr Scand 199795242–243. [DOI] [PubMed] [Google Scholar]
- 22.Henderson M, Glozier N, Holland Elliott K. Long term sickness absence. BMJ 2005330802–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Isometsä E T, Katila H, Aro T. Disability pension for major depression in Finland. Am J Psychiatry 20001571869–1872. [DOI] [PubMed] [Google Scholar]
- 24.Lund T, Labriola M, Christensen K B, Bultmann U, Villadsen E. Return to work among sickness‐absent Danish employees: prospective results from the Danish Work Environment Cohort Study/National Register on Social Transfer Payments. Int J Rehabil Res 200629229–235. [DOI] [PubMed] [Google Scholar]
- 25.Burdorf A, Frings‐Dresen M H, van Duivenbooden C.et al Development of a decision model to identify workers at risk of long‐term disability in the construction industry. Scand J Work Environ Health 200531(suppl 2)31–36. [PubMed] [Google Scholar]
- 26.Gjesdal S, Bratberg E. Diagnosis and duration of sickness absence as predictors for disability pension: results from a three‐year, multi‐register based and prospective study. Scand J Public Health 200331246–254. [DOI] [PubMed] [Google Scholar]
- 27.Holzmann R, Hinz R.Old age income support in the 21st century: an international perspective on pension systems and reform. Washington, DC: The World Bank, 20053–56.