Abstract
Background
This study investigated the stiffness and strength of bridge plating with uni-cortical and bi-cortical locking plate constructs relative to a conventional, non-locked construct in the osteoporotic femoral diaphysis.
Methods
Four bridge plating configurations were applied to a validated model of the osteoporotic femoral diaphysis. A non-locked conventional configuration served as baseline. Locked configurations included bi-cortical locked plating, uni-cortical locked plating and mix-mode locked plating, which combined uni and bi-cortical locking screws. For all configurations, an 11-hole plate was applied with 4.5-mm screws placed in the 1st, 3rd, and 5th plate hole. Five specimens of each configuration were dynamically loaded until failure in torsion, axial compression, and bending to determine construct stiffness, strength and failure modes.
Findings
In torsion and bending, locked plating constructs provided a significantly lower stiffness and strength than the conventional construct. The uni-cortical locked construct was 69% weaker (P<0.001) in torsion than the conventional construct, but its torsional strength improved 73% (P<0.001) by adding one bi-cortical locked screw. In axial compression, construct stiffness varied by less than 10% between the four groups. However, the bi-cortical and mixed-mode locked constructs provided a significant increase in strength of 12% (P = 0.001) and 11% (P=0.002), respectively, compared to the conventional construct.
Interpretations
Locked plating in the osteoporotic diaphysis can improve fixation strength under axial loading, but may reduce fixation strength in bending and torsion compared to conventional plating. Adding one bi-cortical locked screw to an otherwise uni-cortical construct is recommended to improve torsional strength.
Keywords: Locked plating, stiffness, strength, diaphysis, osteoporotic bone
Introduction
The incidence of osteoporotic fractures increases each year as our population ages (Ebeling, 2004). These fractures provide unique problems for fracture fixation. Bridge plate fixation with non-locked screws in diaphyseal and metaphyseal osteoporotic bone is complicated by high rates of fixation failure at the screw-bone interface, resulting in construct failure (Cornell, 2003; Hausman and Panozzo, 2004). Locking plates hold the promise of stronger fixation in osteoporotic bone and, presumably, lower rates of fixation failure for these challenging fractures (Kolodziej et al., 1998; Perren, 2002; Ring et al., 2004). Locking plates have threaded screw holes that support rigid engagement of threaded locking screw heads with the plate. The resulting locking plate constructs derive fixation strength by fixed-angle stabilization rather than by plate-to-bone compression required with conventional, non-locked plating constructs.
Several early locked plating outcome studies have noted lower failure rates in the metaphysis, but fixation failure rates as high as 5–18% in the diaphysis (Button et al., 2004; Kregor et al., 2004; Sommer et al., 2004; Sommer et al., 2003). Mechanical studies suggest that fixed-angle stabilization with uni-cortical locking screws provides a distinct advantage over non-locked screws for fixation in the osteoporotic metaphysis (Kubiak et al., 2006; Marti et al., 2001). However, it remains inconclusive if a similar advantage exists for bi-cortical and uni-cortical fixation in osteoporotic diaphyseal bone (Gardner et al., 2005).
Mechanical studies of bone-plate stability in diaphyseal bone mostly apply to conventional, non-locking plate constructs. These constructs appear to be most stable when long plates with widely spaced screws are used (Gautier and Sommer, 2003; Stoffel et al., 2003). However, the mechanics of locking plates are fundamentally different from conventional plates, meaning the recommendations for optimal screw placement for conventional plates are not readily transferable to locking plate constructs. The clinical use of locking plates requires a revised understanding of the bone-plate construct stability (Gautier and Sommer, 2003).
This study was designed to investigate the stiffness and strength of bridge plate fixation with uni-cortical and bi-cortical locked plating constructs relative to conventional, non-locking plates in a validated osteoporotic diaphyseal long bone model. We hypothesized that uni-cortical and bi-cortical locked plating constructs were at least as stable mechanically as conventional non-locking constructs.
Materials and Methods
Four bridge plating configurations were applied to a validated model of the osteoporotic femoral diaphysis. A non-locked conventional plating (CP) configuration served as baseline. Locked configurations included bi-cortical locked plating (BLP), uni-cortical locked plating (ULP) and mixed-mode locked plating (MLP) which combined uni and bi-cortical locking screws. Each configuration was dynamically loaded until failure in torsion, axial loading, and bending to determine construct stiffness, strength and failure mode.
Specimens
Bridge plating constructs were tested on a validated model of the osteoporotic femoral diaphysis (Sommers et al., 2007). This model consisted of a cortex shell and a trabecular core. The cortex shell of 27 mm diameter and 2 mm thickness was custom machined from 3rd generation composite bone cylinders (Pacific Research Laboratories, Inc., Vashon, WA). The trabecular core was machined from 10 pcf (0.16 g/cm3) solid rigid polyurethane foam (Pacific Research Laboratories, Inc., Vashon, WA) and was bonded to the inside of the cortex shells. Prior research demonstrated that five structural properties of this bone surrogate (torsional rigidity and strength, bending rigidity and strength, and screw pull-out strength) matched the lower 16% of the cumulative range reported for cadaveric femurs (Sommers et al., 2007). Therefore, this osteoporotic bone surrogate reflected the diminished structural properties seen in osteoporotic femora.
Implants
Generic implants were dimensioned to nominally replicate standard 4.5 mm osteosynthesis plates and screws commercially available from several manufacturers. The generic implants were designed with screw holes in the exact same position for locked and non-locked plates, and with identical screw threads and diameters for locked and non-locked screws. These attributes are not available in most commercially available implants, but were deemed crucial for direct comparison between locked and non-locked constructs in absence of confounding factors due to geometric differences. Eleven-hole 4.5 mm osteosynthesis plates in locked and non-locked configurations were manufactured from Ti-6Al-4V surgical grade Titanium. Plates were 5.5 mm thick, 17.5 mm wide, had a curvature of 30 mm radius along the plate width, and had a hole spacing of 18 mm. Generic 4.5 mm screws with a four-fluted self-tapping feature were manufactured from the same material in locked and non-locked configurations. Screw heads of conventional screws had a spherical undersurface as defined by ASTM standard F543-02 (ASTM, 2002). Locking screws had a double-helix thread at the screw head for engagement with the threaded holes of the locking plate. Plates and screws were manufactured in medical grade quality by a company specialized in production of orthopaedic implants (Thortex, Portland, Oregon).
Fixation Constructs
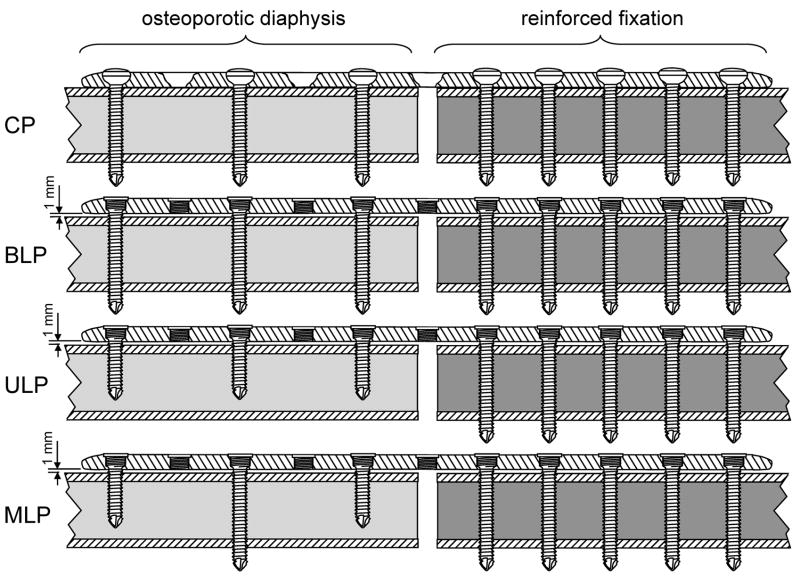
All four implant configurations were tested in a bridge plating construct with a 10 mm fracture gap. On one side of the construct, the plate was applied to the osteoporotic bone surrogate with three screws placed in the 1st, 3rd, and 5th plate hole (Figure 1). This construct side served for evaluation of CP, BLP, ULP, and MLP configurations in an osteoporotic diaphysis. On the opposite side, the plate was rigidly fixed with five bi-cortical screws to a bone surrogate that was reinforced by filling its intramedullary lumen with bone cement. Therefore, construct failure was isolated to the osteoporotic diaphyseal side of each construct, making results applicable to both purely diaphyseal fractures and diaphyseal-metaphyseal fractures with a well-fixed metaphyseal component. For the CP configuration, three non-locking screws were tightened with a torque wrench (Sturtevant, Franklin Park, Il) to 2.8 Nm, corresponding to 80% of their stripping torque as determined in a pilot study on five specimens. In the locked configurations, three locking screws were tightened to 4 Nm and the plate remained 1 mm elevated from the surrogate surface using temporary spacers to account for biological preserving submuscular plating technique recommended for locked plating (Stoffel et al., 2007). In the MLP configuration, two uni-cortical locking screws in the 1st and 5th plate hole were complimented by one bi-cortical locking screw in the 3rd plate hole to improve rotational stability relative to the uni-cortical (ULP) construct.
Figure 1.
Bridge plating constructs, representing four diaphyseal fixation configurations: conventional non-locked plating (CP), bi-cortical locked plating (BLP), uni-cortical locked plating (ULP), and mixed-mode (uni- and bi-cortical) locked plating (MLP). Construct failure was isolated to the osteoporotic diaphyseal side of each construct.
Loading
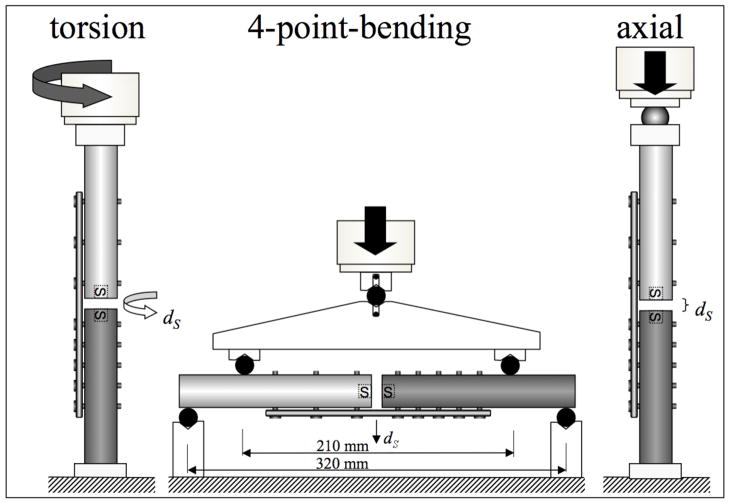
All four plating configurations were tested under progressive dynamic loading to failure (Marti et al., 2001) in torsion, axial compression, and bending with a bi-axial material testing system (Instron 8874, Canton, MA) (Figure 2). Five specimens were tested in each loading mode and implant configuration, requiring a total of 60 tests. Torsion was applied around the diaphyseal shaft axis. Axial compression was applied through a ball bearing at the osteoporotic diaphyseal side of the construct, while the reinforced surrogate portion was rigidly fixed (Stoffel et al., 2007). Bending was applied in a four-point-bending setup to generate a constant bending moment across the entire plate length. The upper and lower cylindrical supports were separated by 210 mm and 320 mm, respectively. The plate was located on the tension side to induce bending in a gap-closing mode. After application of a static pre-load LPRE, sinusoidal loading with a load amplitude of LDYN was applied at 2 Hz. Every 100 loading cycles, this load amplitude was increased stepwise by LDYN until construct failure occurred. For torsion, axial compression, and bending, preloads LPRE of 1 Nm, 50 N and 1 Nm and stepwise load amplitudes LDYN of 1 Nm, 100 N, and 1 Nm were selected, respectively. This stepwise load increase enabled dynamic loading to failure while ensuring that failure was attained for each configuration within a reasonable number of load cycles (Marti et al., 2001). Construct failure was defined either by catastrophic fracture or by a subsidence threshold at the fracture site, whichever occurred first. Subsidence dS represents the non-recoverable collapse at the fracture site after load removal and is caused by implant bending or implant loosening (Gosling et al., 2004). A dS threshold of 5 degrees in torsion (Hasenboehler et al., 2006), 1 mm in compression, and 1 mm mid-point deflection in bending was deemed indicative of the onset of construct failure in absence of a catastrophic fracture. Subsidence by 5 degrees nominally correlated to a 1 mm shear displacement between cortices at the fracture site. Subsidence was assessed with two miniature electromagnetic motion sensors (PcBird, Ascension Technology, Burlington, VT). These sensors were centered in the medullary canal at each side of the fracture gap. They recorded the motion of the bone ends at the fracture site in six-degrees-of-freedom with a resolution of 0.1 mm and 0.1 degrees after filtering of raw data acquired at 100 Hz sampling rate. To eliminate errors in electromagnetic motion sensing due to interference from ferro-magnetic objects, all testing components in the vicinity of the test specimen were machined from non-magnetic materials.
Figure 2.
Construct testing under three distinct loading conditions: four-point bending in gap-closing direction; torsions; and axial compression. Interfragmentary motion in response to progressive dynamic loading was recorded by motion sensors (S).
Outcome Evaluation
The performance of each configuration was described by its stiffness, strength, and failure modes under the three loading conditions. Initial construct stiffness was calculated from the displacement amplitudes in response to loading amplitudes of 1 Nm torsion, 1 kN compression, and 1 Nm bending in addition to application of pre-load LPRE. Construct strength was characterized in terms of the ultimate load to construct failure, defined as the peak load LMAX achieved during dynamic loading. Failure modes were visually analyzed for presence of hardware failure, fixation failure or bone fracture. An analysis of variance (ANOVA) was used to assess the influence of construct type on stiffness and failure loads using a statistical software package (SPSS Inc, Chicago, IL). When significance was detected at a level of significance of α=0.05, Tukey post hoc tests were performed between individual constructs to determine corresponding p-values.
Results
Stiffness
In torsion, CP constructs provided the highest torsional rigidity of 0.72 (SD 0.02) Nm2/° (Figure 3, Table 1a). Compared to the CP construct, the torsional rigidity of the BLP and ULP constructs was reduced by 19% (P < 0.001) and 33% (P < 0.001), respectively. Replacing one uni-cortical locking screw of the ULP construct with a bi-cortical locking screw yielded a 10% increase (P = 0.003) of torsional rigidity in the MLP construct. However, the torsional rigidity of MLP constructs remained significantly below that of CP or BLP constructs. Axial stiffness varied by less than 10% between the four groups, ranging from 3.1 (SD 0.1) kN/mm for MLP constructs to 3.4 (SD 0.2) kN/mm in CP constructs. In bending, the CP construct was significantly stiffer than the three locked plating constructs. Compared to the CP construct, the bending rigidity of the BLP, ULP, and MLP constructs was reduced by 20% (P = 0.01), 21% (P = 0.005), and 30% (P < 0.001), respectively. There was no significant difference in bending rigidity between the three locked constructs.
Figure 3.
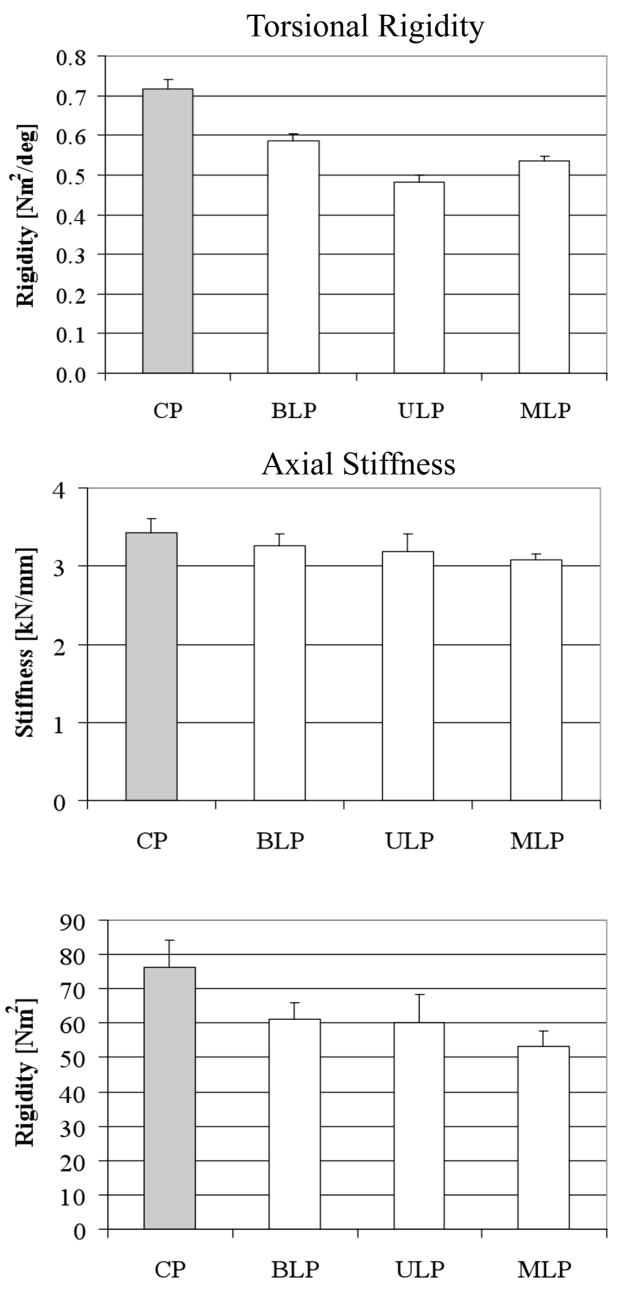
Construct stiffnesses in torsion, axial compression and four-point-bending. Asterisks (*) denote significant differences between groups.
Table 1.
Stiffness, strength, and failure modes of plating configurations. P- values are depicted relative to the CP baseline configuration. CP = conventional plating; BLP = bi-cortical locked plating; ULP = uni-cortical locked plating; MLP = mixed-mode locked plating.
| a | Stiffness | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Torsional Rigidity [Nm2/°] | Axial Stiffness [kN/mm] | Bending Rigidity [Nm2] | |||||||
| Configuration | Mean | Stdev | P-value | Mean | Stdev | P-value | Mean | Stdev | P-value |
| CP | 0.72 | 0.02 | 3.4 | 0.2 | 76.4 | 7.7 | |||
| BLP | 0.58 | 0.02 | < 0.001 | 3.3 | 0.1 | 0.352 | 61.3 | 4.6 | 0.010 |
| ULP | 0.48 | 0.02 | < 0.001 | 3.2 | 0.2 | 0.145 | 60.1 | 8.3 | 0.005 |
| MLP | 0.53 | 0.01 | < 0.001 | 3.1 | 0.1 | 0.024 | 53.1 | 4.5 | < 0.001 |
| b | Strength | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Torsion [Nm] | Axial [kN] | Bending [Nm] | |||||||
| Configuration | Mean | Sthev | P-value | Mean | Sthev | P-value | Mean | Sthev | P-value |
| CP | 25.5 | 1.9 | 3.9 | 0.2 | 34.5 | 2.6 | |||
| BLP | 19.6 | 1.0 | < 0.001 | 4.4 | 0.1 | 0.001 | 29.8 | 2.0 | 0.006 |
| ULP | 7.9 | 0.7 | < 0.001 | 4.0 | 0.1 | 0.833 | 25.8 | 1.7 | <0.001 |
| MLP | 13.7 | 0.7 | < 0.001 | 4.4 | 0.2 | 0.002 | 25.5 | 1.0 | < 0.001 |
| c | Failure Modes | ||
|---|---|---|---|
| Configuration | Torsion | Axial | Bending |
| CP | screw loosening (4); spiral fracture (1) | screw migration (5) | fracture at plate end (5) |
| BLP | screw breakage (5) | screw migration and bending (5) | fracture at plate end (5) |
| ULP | screw loosening (5) | screw migration (5) | fracture at plate end (5) |
| MLP | screw loosening and bending (5) | screw migration and bending (5) | fracture at plate end (5) |
Strength
In torsion, CP constructs provided the highest strength with a failure torque of 25.5 (SD 1.9) Nm (Figure 4, Table 1b). Compared to the CP construct, the torsional strength of the BLP and ULP was reduced by 23% (P < 0.001) and 69% (P < 0.001), respectively. Replacing one uni-cortical locking screw of the ULP construct with a bi-cortical locking screw yielded a 73% improvement (P < 0.001) of strength in the MLP constructs compared to ULP constructs. However, MLP constructs remained 30% weaker than BLP constructs and 46% weaker than CP constructs in torsion. In axial loading, CP constructs failed at 3.9 (SD 0.2) kN. BLP constructs were significantly stronger than CP constructs and failed at 4.4 (SD 0.1) kN (P = 0.001). ULP constructs were not significantly stronger than CP constructs and failed at 4.0 (SD 0.1) kN (P = 0.81). MLP constructs were significantly stronger than CP constructs (P = 0.002) and their failure load of 4.4 (SD 0.2) kN was comparable to that of BLP constructs. In bending, the CP construct tolerated the highest bending moment of 34.5 (SD 3) Nm. Compared to the CP construct, the bending strength of the BLP and ULP constructs was reduced by 14% (P = 0.006) and 25% (P < 0.001), respectively. There was no significant difference (P = 0.99) in bending strength between the ULP and MLP constructs.
Figure 4.
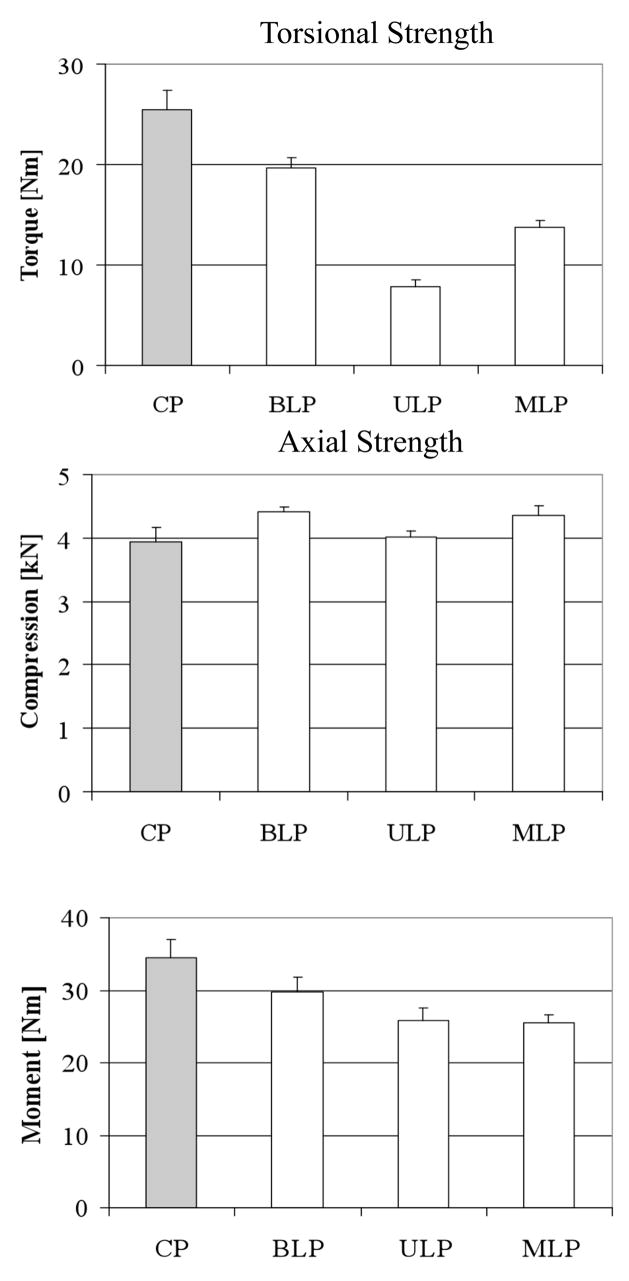
Construct failure loads in torsion, axial compression, and four-point-bending. Asterisks (*) denote significant differences between groups.
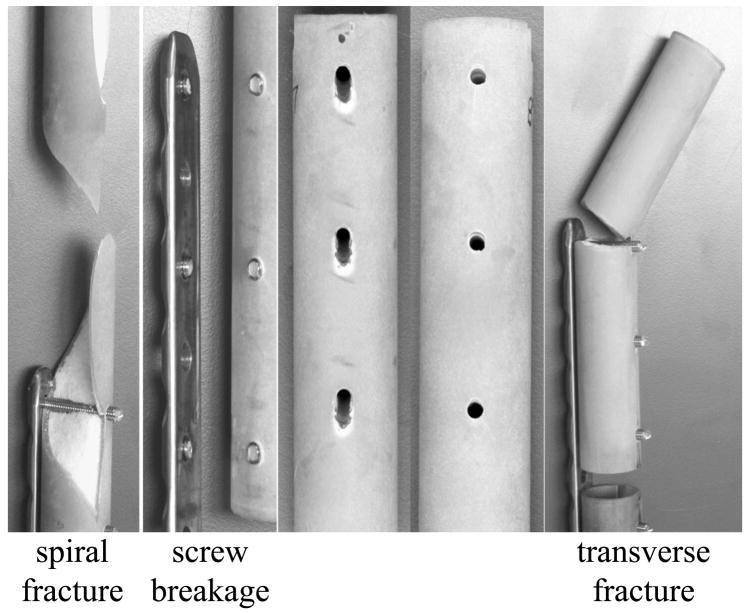
Failure Mode
In torsion, CP constructs failed by screw loosening (4) or by spiral fracture (1) through the screw hole at the plate end (Figure 5, Table 1c). All BLP constructs failed by screw breakage between the elevated plate and the bone due to repetitive bending during cyclic torsion. ULP constructs failed by screw loosening in the near cortex. MLP constructs failed by a combination of screw loosening of uni-cortical screws and screw breakage of the bi-cortical screw. In axial compression, all constructs failed by screw migration in the near cortex, resulting in elongation of the near cortex holes and progressive loss of fixation. In CP constructs, migration caused screw rotation about a pivot point in the far cortex of the bone. For bi-cortical locking screws, migration caused screw bending while uni-cortical locking screws migrated in the near cortex without screw bending. In bending, all specimens failed by fracture through the screw hole at the plate end, regardless of the plating configuration.
Figure 5.
Failure modes of constructs: a) in torsion, failures included spiral fracture at the plate end (CP) and screw breakage between the elevated plate and the bone; b) in axial compression, all constructs failed by screw migration, resulting in elongation of the near cortex screw holes; c) in bending, all constructs failed by transverse fracture through the screw hole at the plate end.
Discussion
The superior fixation strength of locking screws compared to conventional screws has been well established for metaphyseal fracture fixation in osteoporotic bone, whereby long uni-cortical screws act as columns capable of supporting fracture fragments at a fixed angle to the plate (Kubiak et al., 2006). However, for fixation in the osteoporotic diaphysis, controversy remains concerning the indications for use and optimal configuration of locked plating.
Early biomechanical studies using locking plates focused on the mechanics of uni-cortical locking screw constructs. Marti et al. (2001) compared the Less Invasive Stabilization System (LISS) with a Condylar Buttress Plate in cadaveric femoral diaphyseal bone. They found less irreversible deformation under axial load using the all uni-cortical locking LISS plate relative to the non-locking Condylar Buttress Plate. Stoffel et al. (2003) evaluated the axial and torsional stiffness of uni-cortical locked constructs using titanium plates in non-osteoporotic surrogate bone specimes. They found that axial stiffness and torsional rigidity were affected by the distance of the first screw to the fracture site, whereby placing the screw further from the fracture site decreased axial stiffness. Bong et al. (2002) evaluated fixation of supracondylar femur fractures in cadaveric specimens using a retrograde nail or a LISS plate. They found the retrograde nail to be more stable in comminuted fracture patterns, especially in torsion. Kowalski et al. (1996) evaluated the stiffness of fixation of early locking plate constructs relative to non-locking plates and external fixators in a surrogate tibia model and found the locking plates to be as rigid as non-locking plates as long as the plate-bone distance was no greater than 5 mm. In the cadaveric radial diaphysis, Gardner et al. (2005) reported a subtle mechanical superiority of bi-cortical locked plating compared to conventional plating under torsional loading. They concluded that the few differences found between the constructs mandated further investigations. In a subsequent study on sawbone humeri, they found that locked or hybrid constructs retained torsional stiffness under dynamic loading better than non-locked constructs (Gardner et al., 2006). They simulated screw purchase in osteoporotic bone by over-drilling of screw holes. The present study employed for the first time a validated model of the osteoporotic femoral diaphysis to investigate the stiffness and strength of locked plating constructs relative to a non-locked construct under all three principal loading modes.
Stiffness represents the initial fixation characteristics of the plate-bone construct. In the current study, all of the locked plate constructs had a significantly lower stiffness in torsion and bending than the conventional plate construct. This reduced stiffness of locked plating constructs can be attributed to plate elevation over the cortex, which eliminates the stabilizing effect of the plate-bone interface provided in the conventional plating construct. In axial compression, locked plating constructs were comparable in stiffness to the conventional non-locked construct. These stiffness results correlate to results of Stoffel et al. (2007) obtained in a bridge plating model of supracondylar femur fractures in osteopenic femurs. They reported that locked constructs had a 26% lower torsional rigidity than non-locked constructs while the axial stiffness did not significantly differ between locked and non-locked constructs.
Dynamic load to failure is often used as a measure of construct strength (Gardner et al., 2005; Marti et al., 2001). In axial loading, the bi-cortical locking construct was superior in strength compared to the non-locked construct, which can be attributed to the fixed-angle stabilization provided by locking screws. This finding is in agreement with previous laboratory studies using cadaveric and synthetic specimens (Marti et al., 2001; Snow et al., 2008; Stoffel et al., 2007). Furthermore, the present research demonstrated that for fixation in the osteoporotic diaphysis, the conventional construct was significantly stronger in torsion and bending than any of the locked plating constructs. The reduced strength of locked constructs in torsion may again be explained by plate elevation. In the case of bi-cortical locking screws, torsion-induced toggle of the elevated plate around its plane of fixation resulted in fatigue fracture of the screw shaft between the plate and the bone. This failure mode correlates with the results of Stoffel et al. (2007). They found that LISS locking plates applied to synthetic and cadaveric femurs at 1 mm elevation failed in torsion as a result of screw breakage. They furthermore found that bi-cortical non-locked constructs could tolerate on average higher torsional loads than could bi-cortical locked constructs, although the differences were not statistically significant. Consequently, the present findings are limited to locked plating with plate elevation. In absence of plate elevation, Gardner et al. (2005, 2006) found that locked plating constructs exhibited a higher torsional strength and stability than non-locked constructs. However, eliminating plate elevation may adversely affect periosteal perfusion and biological fixation intended with locked plating. Nevertheless, the effect of plate elevation versus plate-to-bone contact on torsional strength of locked constructs in the osteoporotic diaphysis should be investigated in a future study. For uni-cortical screws in the present study, plate toggle resulted in screw loosening attributed to the smaller working length of the screw in thin walled, osteoporotic bone. Gautier et al. (2003) previously recognized the importance of cortical thickness on fixation of uni-cortical locked screws, especially in osteoporotic bone. They recommended avoiding the use of all uni-cortical fixation in osteoporotic bone, especially if torsional loading is expected. Similarly, Roberts et al. (2007) reported that locked uni-cortical constructs exhibited inferior torsional rigidity, which could be improved by 58% when adding a single bi-cortical screw. However, their study only reported construct stiffness but not strength. The present study found that adding a single bi-cortical screw to a uni-cortical construct can improve its torsional strength by 73%.
In bending, it is interesting that the non-locked construct tolerated a higher bending load than any of the locking constructs. This reduced bending strength of locked constructs relative to the conventional construct is likely caused by stress concentrations at the end screw, leading to periprosthetic fracture at the end screw hole. Periprosthetic fracture at the plate end is a well-recognized complication associated with conventional plate fixation in osteoporotic bone with an incident rate of 1–3% (Beaupre et al., 1992; Davenport et al., 1988). A case series on locked plating reported a 2.6% incidence of periprosthetic fractures at the plate end (Sommer et al., 2003). It is possible that the fixed angle nature of the locked screws can create higher stress concentrations at the screw-bone interface leading to earlier failures relative to the conventional screws which would be more likely to toggle and create a lower stress concentration. Furthermore, both constructs with uni-cortical end screws (ULP and MLP) failed earlier than the bi-cortical locked construct, potentially because the uni-cortical locking screws concentrated load transfer on the near cortex, while bi-cortical locking screws may have allowed for load sharing between the near and far cortex at the plate end.
Although improved strength under dynamic loading is certainly advantageous, the benefit of high construct stiffness for locking plates is less clear. Conventional non-locked compression plating theory requires the absolute stability provided by interfragmentary compression to allow primary bone healing (Allgower and Spiegel, 1979). However, locking plate theory does not aim for interfragmentary compression but instead relies on secondary bone healing by callus formation, which can be promoted by interfragmentary motion (Egol et al., 2004; Uhthoff et al., 2006). Locking plate constructs may therefore benefit from a low stiffness that facilitates interfragmentary motion to promote secondary bone healing by callus formation.
We chose to utilize a thoroughly validated model of the osteoporotic femoral diaphysis to remove the variability in mechanical characteristics seen in cadaveric femora. The published mechanical properties of cadaveric femora are inconsistent, with torsional strength ranging from 42 Nm to 318 Nm (Hubbard, 1973; Martens et al., 1980; Mensch et al., 1976) and bending strength ranging from 52 – 605 Nm (Funk et al., 2004; Stromsoe et al., 1995). When used for biomechanical testing, this considerable variation in the strength of cadaveric bone results in data sets with large standard deviations and limits the sensitivity to detect significant differences between implant configurations. While paired testing of contralateral specimens can compensate for some of the inherent variability in bone quality, it is limited to direct comparison between two groups and cannot accommodate simultaneous comparison between four plating configurations used in the present study. As is the case for any bone model one must recognize its inherent limitations. Although the model is representative of the weak bone range for five key structural properties of bone, there are other mechanical behaviors that have not been validated. Crack propagation and fatigue under dynamic loading were not quantified since comparable values for these properties are not available in the literature. However, the spiral fracture in torsion and the transverse fractures in bending closely correlated with fracture patterns seen clinically. Nevertheless, absolute results obtained in the bone model do not allow for a direct correlation to the clinical setting. However, the relative relationship in outcome parameters between the plating constructs should retain its clinical relevance.
Furthermore, this study isolated the three forces that a fracture construct might experience, namely torsion, axial loading and bending, in an attempt to better define the specific role of each of these forces in the failure modes of the bone-plate construct. In clinical applications, every fracture construct is loaded with some combination of these forces, making the true failure mechanism more complex than described in this study. However, to develop a complete understanding of the relative strengths and weakness of locked plating, it was vital that the individual forces be isolated to these loading modes. This allowed the identification of problem areas of fixation, such as the relative weakness of uni-cortical screws in torsion and the improvement of this weakness by the addition of a single bi-cortical screw, which may not be identified in a combined loading model. Additionally, isolating the loads makes the data portable, meaning that with the prior knowledge of the loading characteristics of a specific bone, the data can be applied to a large range of fracture scenarios. Finally, the results of this study only describe differences in structural properties between the fixation constructs. In vivo, locked plating is believed to enable less-invasive and more biological fixation by plate elevation, which may promote periosteal perfusion and fracture healing (Perren, 2002).
In conclusion, we found that in axial loading, bi-cortical and mixed-mode locked bridge plating can offer significantly improved strength of fixation under dynamic axial loading in the osteoporotic femoral diaphysis while providing comparable construct stiffness. However, non-locking constructs exhibited higher strength in bending and torsion compared to locking constructs applied at 1 mm plate elevation. In torsion, the all-uni-cortical constructs perform poorly relative to non-locking and bi-cortical locked constructs. We recommend the addition of a single bi-cortical locking screw to any all-uni-cortical locking screw construct used for fracture fixation in osteoporotic bone when torsional loading is expected. We urge further mechanical studies aimed at more clinically applicable combined loading scenarios to support the clinical utility of these findings. In addition, future studies should address the effects of plate elevation on the strength of locked plating constructs.
Acknowledgments
The authors thank Sebastian Boldhaus for his technical support. Financial support for this research was provided by the Legacy Foundation and NIH/NIAMS Grant R21 AR053611.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allgower M, Spiegel PG. Internal fixation of fractures: evolution of concepts. Clin Orthop Relat Res. 1979:26–9. [PubMed] [Google Scholar]
- Astm. Standard Specification and Test Methods for Metallic Medical Bone Screws. ASTM International. 2002:F543–02. [Google Scholar]
- Beaupre GS, Giori NJ, Caler WE, Csongradi J. A comparison of uni-cortical and bi-cortical end screw attachment of fracture fixation plates. J Orthop Trauma. 1992;6:294–300. doi: 10.1097/00005131-199209000-00005. [DOI] [PubMed] [Google Scholar]
- Bong MR, Egol KA, Koval KJ, Kummer FJ, Su ET, Iesaka K, Bayer J, Di Cesare PE. Comparison of the LISS and a retrograde-inserted supracondylar intramedullary nail for fixation of a periprosthetic distal femur fracture proximal to a total knee arthroplasty. J Arthroplasty. 2002;17:876–81. doi: 10.1054/arth.2002.34817. [DOI] [PubMed] [Google Scholar]
- Button G, Wolinsky P, Hak D. Failure of less invasive stabilization system plates in the distal femur: a report of four cases. J Orthop Trauma. 2004;18:565–70. doi: 10.1097/00005131-200409000-00015. [DOI] [PubMed] [Google Scholar]
- Cornell CN. Internal fracture fixation in patients with osteoporosis. J Am Acad Orthop Surg. 2003;11:109–19. doi: 10.5435/00124635-200303000-00005. [DOI] [PubMed] [Google Scholar]
- Davenport SR, Lindsey RW, Leggon R, Miclau T, Panjabi M. Dynamic compression plate fixation: a biomechanical comparison of uni-cortical vs bi-cortical distal screw fixation. J Orthop Trauma. 1988;2:146–50. [PubMed] [Google Scholar]
- Ebeling PR. Idiopathic or hypogonadal osteoporosis in men: current and future treatment options. Treat Endocrinol. 2004;3:381–91. doi: 10.2165/00024677-200403060-00006. [DOI] [PubMed] [Google Scholar]
- Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488–93. doi: 10.1097/00005131-200409000-00003. [DOI] [PubMed] [Google Scholar]
- Funk JR, Kerrigan JR, Crandall JR. Dynamic bending tolerance and elastic-plastic material properties of the human femur. Annu Proc Assoc Adv Automot Med. 2004;48:215–33. [PMC free article] [PubMed] [Google Scholar]
- Gardner MJ, Brophy RH, Campbell D, Mahajan A, Wright TM, Helfet DL, Lorich DG. The mechanical behavior of locking compression plates compared with dynamic compression plates in a cadaver radius model. J Orthop Trauma. 2005;19:597–603. doi: 10.1097/01.bot.0000174033.30054.5f. [DOI] [PubMed] [Google Scholar]
- Gardner MJ, Griffith MH, Demetrakopoulos D, Brophy RH, Grose A, Helfet DL, Lorich DG. Hybrid locked plating of osteoporotic fractures of the humerus. J Bone Joint Surg Am. 2006;88:1962–7. doi: 10.2106/JBJS.E.00893. [DOI] [PubMed] [Google Scholar]
- Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003;34(Suppl 2):B63–76. doi: 10.1016/j.injury.2003.09.026. [DOI] [PubMed] [Google Scholar]
- Gosling T, Schandelmaier P, Marti A, Hufner T, Partenheimer A, Krettek C. Less invasive stabilization of complex tibial plateau fractures: a biomechanical evaluation of a unilateral locked screw plate and double plating. J Orthop Trauma. 2004;18:546–51. doi: 10.1097/00005131-200409000-00011. [DOI] [PubMed] [Google Scholar]
- Hasenboehler E, Smith WR, Laudicina L, Philips GC, Stahel PF, Morgan SJ. Fatigue behavior of Ilizarov frame versus tibial interlocking nail in a comminuted tibial fracture model: a biomechanical study. J Orthop Surg. 2006;1:16. doi: 10.1186/1749-799X-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausman M, Panozzo A. Treatment of distal humerus fractures in the elderly. Clin Orthop Relat Res. 2004:55–63. doi: 10.1097/01.blo.0000131485.47685.8c. [DOI] [PubMed] [Google Scholar]
- Hubbard MJ. The fixation of experimental femoral shaft torque fractures. Acta Orthop Scand. 1973;44:55–61. doi: 10.3109/17453677308988672. [DOI] [PubMed] [Google Scholar]
- Kolodziej P, Lee FS, Patel A, Kassab SS, Shen KL, Yang KH, Mast JW. Biomechanical evaluation of the schuhli nut. Clin Orthop Relat Res. 1998:79–85. [PubMed] [Google Scholar]
- Kowalski MJ, Schemitsch EH, Harrington RM, Chapman JR, Swiontkowski MF. A comparative biomechanical evaluation of a noncontacting plate and currently used devices for tibial fixation. J Trauma. 1996;40:5–9. doi: 10.1097/00005373-199601000-00002. [DOI] [PubMed] [Google Scholar]
- Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18:509–20. doi: 10.1097/00005131-200409000-00006. [DOI] [PubMed] [Google Scholar]
- Kubiak EN, Fulkerson E, Strauss E, Egol KA. The evolution of locked plates. J Bone Joint Surg Am. 2006;88(Suppl 4):189–200. doi: 10.2106/JBJS.F.00703. [DOI] [PubMed] [Google Scholar]
- Martens M, Van Audekercke R, De Meester P, Mulier JC. The mechanical characteristics of the long bones of the lower extremity in torsional loading. J Biomech. 1980;13:667–76. doi: 10.1016/0021-9290(80)90353-x. [DOI] [PubMed] [Google Scholar]
- Marti A, Fankhauser C, Frenk A, Cordey J, Gasser B. Biomechanical evaluation of the less invasive stabilization system for the internal fixation of distal femur fractures. J Orthop Trauma. 2001;15:482–7. doi: 10.1097/00005131-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Mensch JS, Markolf KL, Roberts SB, Finerman GM. Experimental stabilization of segmental defects in the human femur. A torsional study. J Bone Joint Surg Am. 1976;58:185–90. [PubMed] [Google Scholar]
- Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093–110. doi: 10.1302/0301-620x.84b8.13752. [DOI] [PubMed] [Google Scholar]
- Ring D, Kloen P, Kadzielski J, Helfet D, Jupiter JB. Locking compression plates for osteoporotic nonunions of the diaphyseal humerus. Clin Orthop Relat Res. 2004:50–4. doi: 10.1097/01.blo.0000131484.27501.4b. [DOI] [PubMed] [Google Scholar]
- Roberts JW, Grindel SI, Rebholz B, Wang M. Biomechanical evaluation of locking plate radial shaft fixation: uni-cortical locking fixation versus mixed bi-cortical and uni-cortical fixation in a sawbone model. J Hand Surg [Am] 2007;32:971–5. doi: 10.1016/j.jhsa.2007.05.019. [DOI] [PubMed] [Google Scholar]
- Snow M, Thompson G, Turner P. A Mechanical Comparison of the Locking Compression Plate (LCP) and the Low Contact Dynamic Compression Plate (DCP) in an Osteoporotic Bone Model. J Orthop Trauma. 2008;22:121–125. doi: 10.1097/BOT.0b013e318160c84c. [DOI] [PubMed] [Google Scholar]
- Sommer C, Babst R, Muller M, Hanson B. Locking compression plate loosening and plate breakage: a report of four cases. J Orthop Trauma. 2004;18:571–7. doi: 10.1097/00005131-200409000-00016. [DOI] [PubMed] [Google Scholar]
- Sommer C, Gautier E, Muller M, Helfet DL, Wagner M. First clinical results of the Locking Compression Plate (LCP) Injury. 2003;34(Suppl 2):B43–54. doi: 10.1016/j.injury.2003.09.024. [DOI] [PubMed] [Google Scholar]
- Sommers MB, Fitzpatrick DC, Madey SM, Vande Zanderschulp C, Bottlang M. A surrogate long-bone model with osteoporotic material properties for biomechanical testing of fracture implants. J Biomech. 2007;40:3297–304. doi: 10.1016/j.jbiomech.2007.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoffel K, Dieter U, Stachowiak G, Gachter A, Kuster MS. Biomechanical testing of the LCP--how can stability in locked internal fixators be controlled? Injury. 2003;34(Suppl 2):B11–9. doi: 10.1016/j.injury.2003.09.021. [DOI] [PubMed] [Google Scholar]
- Stoffel K, Lorenz KU, Kuster MS. Biomechanical considerations in plate osteosynthesis: the effect of plate-to-bone compression with and without angular screw stability. J Orthop Trauma. 2007;21:362–8. doi: 10.1097/BOT.0b013e31806dd921. [DOI] [PubMed] [Google Scholar]
- Stromsoe K, Hoiseth A, Alho A, Kok WL. Bending strength of the femur in relation to non-invasive bone mineral assessment. J Biomech. 1995;28:857–61. doi: 10.1016/0021-9290(95)95274-9. [DOI] [PubMed] [Google Scholar]
- Uhthoff HK, Poitras P, Backman DS. Internal plate fixation of fractures: short history and recent developments. J Orthop Sci. 2006;11:118–26. doi: 10.1007/s00776-005-0984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]