Abstract
AIM: To establish which scolicidal agents are superior and more suitable for regular use.
METHODS: Echinococcus granulosus protoscoleces were obtained from 25 patients with liver hydatid cysts. Various concentrations of albendazole sulfone, albendazole sulfoxide, and albendazole sulfone and albendazole sulfoxide mixed together in concentrations of 50 μg/mL, and H2O2 in a concentration of 4%, NaCl 20%, and 1.5% cetrimide-0.15% chlorhexidine (10% Savlon-Turkey) were used to determine the scolicidal effects. Albendazole (ABZ) derivatives and other scolicidal agents were applied to a minimum of 100 scoleces for 5 and 10 min. The degree of viability was calculated according to the number of living scolices per field from a total of 100 scolices observed under the microscope.
RESULTS: After 5 min, ABZ sulfone was 97.3% effective, ABZ sulfoxide was 98.4% effective, and the combined solution was 98.6% effective. When sulfone, sulfoxide and the combined solutions were compared, the combined solution seemed more effective than sulfone. However, there was no difference when the combined solution was compared with sulfoxide. After 10 min, hypertonic salt water, sulfone, sulfoxide, and the combined solution compared to other solutions looked more effective and this was statistically significant on an advanced level. When sulfone, sulfoxide, and the combined solutions were compared with each other, the combined solution appeared more effective than sulfone. When the combined solution was compared with sulfoxide, there was no difference.
CONCLUSION: Despite being active, ABZ metabolites did not provide a marked advantage over 20% hypertonic saline. According to these results, we think creating a newly improved and more active preparation is necessary for hydatid cyst treatment.
Keywords: Hydatid disease, Albendazole, In vitro study, Combined solution, Scolicidal agents
INTRODUCTION
Treatments of hydatid disease have been suggested in many examples within the literature and text books, including systemic administration of various chemotherapeutic agents, surgery, and the percutaneous approach. The efficacy of systemic chemotherapy is limited[1–4]. Although surgery is the recommended treatment for liver hydatid cyst, percutaneous treatment has been introduced as an alternative treatment, especially in patients who cannot or do not want to undergo surgery[4,5]. There is no completely satisfactory surgical approach, but the operation is best performed by experts. The main object is to remove the cyst completely, without soiling and infecting the peritoneum and with complete obliteration of the resulting dead space. Complete removal of the cyst, with its adventitia, is ideal to avoid spilling the contents. The usual operation is cystectomy with removal of the germinal and laminated layers and preservation of the host derived ectocyst[6]. Instillation of a scolicidal agent into hepatic hydatid cysts to reduce the risk of spillage of viable protoscolices is an integral part of the surgical technique for many surgeons. For over 20 years, benzoimidazole derivatives have been widely used in the medical treatment of hydatidosis. The current literature suggests that amongst all of these, albendazole (ABZ) is the most effective and useful drug for the medical treatment of hydatid disease[7]. After oral administration, ABZ is oxidized to a sulfoxide, which is in part further oxidized to a sulfone, and ABZ sulfoxide is the main metabolite in vivo[8]. The metabolites of ABZ are characterized by their low solubility in water and poor absorption[9]. ABZ has a scolicidal effect via its biologically active metabolites ABZ sulfoxide and ABZ sulfone, the latter being more effective. The first aim of this in vitro study was to establish the use of ABZ sulfoxide, ABZ sulfone, and the combined solution as scolicidal agents on the hydatid cyst. The second aim was to compare their effectiveness with other scolicidal agents.
MATERIALS AND METHODS
Protoscolex collection
For this in vitro study, we used scolex solutions collected from 25 patients who underwent operations for liver hydatid disease at the Haseki Teaching and Research Hospital, Department of General Surgery from 2002 to 2004. All samples were examined and identified at the Istanbul University, Faculty of Medicine, Department of Microbiology and Clinical Microbiology. For this study, ABZ sulfone and ABZ sulfoxide were purchased from Unimark Remedies Ltd Company in India (Certificate of Analysis of working standard ABZ/IMP001/02-Date 17.04.2002).
Effectiveness of ABZ and other solutions in vitro
ABZ sulfone and ABZ sulfoxide dissolve poorly and slowly in water; however, in order to avoid the effects of other solvents, normal saline (0.9% NaCl) was used as a solvent, so that any scolocidal effect and tissue injury would be due only to ABZ sulfone and ABZ sulfoxide. Preparation of the ABZ sulfone and ABZ sulfoxide solutions was as follows: 10 mg ABZ sulfone and ABZ sulfoxide was dissolved in normal saline and brought to a final volume of 100 mL, and then the solution was mixed for 12 h at room temperature by a magnetic mixer. The solutions were further diluted by normal saline to obtain 50 μg/mL ABZ sulfone and ABZ sulfoxide in the final working solutions. We diluted another solution of ABZ sulfone and ABZ sulfoxide mixed together to a total of 50 μg/mL. All three solutions were sterilized by UV. Moreover, for comparison, we used H2O2 in 4% concentration, NaCl 20%, and 1.5% cetrimide-0.15% chlorhexidine (10% Savlon-Turkey) solution to determine the scolicidal effects.
The scolices were mixed with each solution for 5 and 10 min. The scolices were separated from the solutions and washed by normal saline. A few drops were smeared on an object glass and a drop of eosin was added; the slide was then covered with a cover glass and evaluated under the light microscope. For each different solution at both 5 and 10 min, the percentages of dead scolices were determined by counting a minumum of 100 scolices. With regard to the viability of cysts, the same criteria were used as defined in a previous report[10]. Scolices that lost their ellipsoid shape and became round, had rostellums rolled in, showed vacuolar degeneration, and took in eosin were considered dead; all four criteria had to be met for a scolex to be accepted as dead.
Statistical analysis
All statistical calculations were based on an analysis of comparing means by a paired samples t test. Differences were determined using the least significant differences, and P < 0.05 was considered to be significiant.
RESULTS
This in vitro study demonstrated that 50 μg/mL ABZ sulfone killed 97.3% of the scolices, ABZ sulfoxide killed 98.4% of the scolices, and the combined solution (sulfone + sulfoxide) killed 98.6% of the scolices in 5 min (Figure 1). The second part of the study showed that the three ABZ solutions respectively killed 98.6%, 99.5%, and 99.6% of the scolices in 10 min. Among the other solutions that were used, hypertonic salt water was seen to be most effective on scolices. Hypertonic saline solution respectively killed 98.2% and 99.5% of the scolices in 5 and 10 min (Table 1). In the first part of the study, the scolicidal effects of hypertonic salt water, the ABZ sulfone, ABZ sulfoxide, and the combined solution were seen to be statistically significant on an advanced level compared to cetrimide and peroxide. When sulfone, sulfoxide, and the combined solution were compared to hypertonic salt water, no statistical significance was seen (P > 0.05). When sulfone, sulfoxide, and the combined solutions were compared with each other, the combined solution was seen to be more effective. When comparing the combined solution to sulfoxide there was not any difference.
Figure 1.
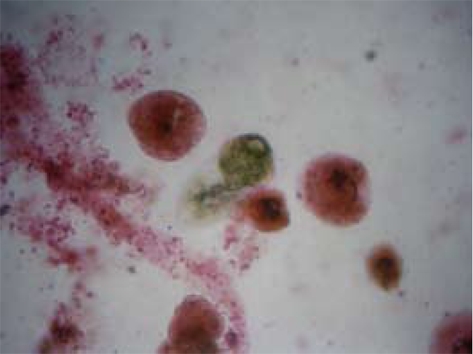
Light microscopy of Echinococcus granulosus microcysts incubated in vitro with ABZ.
Table 1.
The use of different scolicidal agents at the 5th and 10th min for the treatment of hydatid disease (in vitro results)
| Time | NaCl 20% | H2O2 | Cetrimide | Sulfone | Sulfoxide | Sulfone + Sulfoxide |
| 5th min | 98.2% | 90.3% | 86.9% | 97.3% | 98.4% | 98.6% |
| 10th min | 99.5% | 95.7% | 92.6% | 98.6% | 99.5% | 99.6% |
In the second part of the study, again hypertonic salt water, sulfone, and the combined solution were seen to be more effective compared to other solutions and were seen to be statistically significant on an advanced level as well. When sulfone, sulfoxide and the combined solution were compared to hypertonic salt water, hypertonic salt water was seen to be statistically significant compared to sulfone, but it was not seen to be significant compared to the others. When sulfone, sulfoxide and the combined solution were compared to each other, the combined solution was seen to be more effective compared to sulfone. Upon comparing the combined solution with sulfoxide, there was not any difference.
When each solution was compared based on 5 and 10 min timing in the first and the second part of the study, the scolicidal effects of each solution in the second part were statistically significant (P < 0.05).
DISCUSSION
There are currently three treatment options for hydatid disease of the liver: surgery, which remains the most efficent treatment, percutaneous aspiration and medical treatment. In general, hydatidosis is a public health problem, especially in our country, and the treatment often is selected depending on the social and medical professional’s conditions. Since the 1990s, percutaneous treatment has been used increasingly. Surgery remains the most effective treatment, which aims to treat concurrently the parasitic disease, the cavity, and often the biliary complications. Although surgery is technically demanding and often considered risky, the development of hepatic surgery permits safer performance of this therapeutic option.
Ideally, therapy of liver hydatid disease should be able to cure the disease with a low morbidity. Failure of treatment is defined as recurrence and complications related to the intervention. Protection of the operation field is mandatory before the planned operation on the cyst or before the cyst is emptied. Preoperative destruction of the cyst’s contents and preventing infection of the surrounding area has an important role for success of the operation; also, this procedure helps to prevent the illness from returning[11]. For sterilization of the cyst, several parasiticidal substances have been used. Scolicidal solutions remain indispensable in the treatment of hydatid cyst disease. Properties of an ideal solution would be inexpensiveness and the promotion of a rapid and complete scolicidal effect with an absence of local and systemic side effects. From this point of view, no ideal solution and agents have been described yet.
ABZ carbamate is one of the most important benzimidazole derivatives used against liver flukes, tapeworms, and lung and gastrointestinal roundworms. ABZ is normally not detectable in human plasma since it is rapidly metabolized to its major active metabolite as ABZ sulfoxide and ABZ sulfone. ABZ sulfoxide is the main metabolite in vivo[8,12–14]. ABZ leads to a decrease in the glycogen content of the cyst wall, inhibits acid phosphatase, ATP, pyruvate kinase, phosphoenolpyruvate kinase, and causes cellular autolysis and degeneration in the microthrics and the microtubuli[15].
Despite ABZ being used preoperatively and postoperatively for hydatid cyst treatment, today there is no comparative study in the literature, especially concerning ABZ metabolites’ preoperative scolicidal effectiveness (Table 2). In our study, the ABZ metabolites of ABZ sulfoxide, ABZ sulfone, and the combined form were applied directly on the scolices. In this case, the reason why we chose ABZ metabolites over ABZ was that ABZ was not effective directly on the body. Also, we determined how much time was needed for each of the metabolites to be effective and on how many scolices they were effective.
Table 2.
Different scolicidal agents in literature
| Author | Agents | Results |
| Caglar et al[26] (2008) | 20% silver nitra (20 min) | 100% death |
| 50% Dextroz (30 min) | 100% death | |
| 20% NaCl (45 min) | 100% death | |
| 20% Mannitol (45 min) | 100% death | |
| Frayha et al[27] (1981) | Cetrimide 0.5%-1% (10 min) | 100% death |
| Kayaalp et al[28] (2002) | 10%-30% NaCl (3, 6, 75 min | 100% death |
| Sonişik et al[11] (2002) | 10%-30% NaCl ( 3, 6 and 75 min) | 100% death |
| Besim et al[16] (1989) | 20% Saline (15 min) | 100% death |
| 95% Ethyl alcohol (15 min) | 100% death | |
| 10% Polyvinyl pirrolidone iodine (15 min) | 100% death | |
| 3% H2O2 (15 min) | 100% death | |
| Erzurumlu et al[20] (1998) | Albendazole sulfoxide 20 μg/mL | 5% death |
| Albendazole sulfoxide 50 μg/mL | 50% death | |
| Albendazole sulfoxide 100 μg/mL | 100% death | |
| Adas et al (our study) | 20% NaCL (5 min) | 98.2% death |
| (2008) | 3% H2O2 (5 min) | 90.3% death |
| Cetrimide (5 min) | 86.9% death | |
| Albendazole sulfone (5 min) | 97.3% death |
In both parts of the study, cetrimide was found to be the least effective in killing the scolices. This result showed a dissimilarity from other limited studies performed in the literature. Besim et al[16] reported that cetrimide-chlorhexidine was the most potent scolicidal agent in vitro. Half-percent cetrimide and 0.05% chlorhexidine combination for 5 min is an effective protoscolicidal agent in labaratory and clinical studies[16]. Sonişik et al[11] further supported the potent scolicidal effect of cetrimide with a clinical study. The disadvantages of cetrimide, namely metabolic acidosis and methemoglobinemia, have been reported[17]. In the literature, hypertonic salt water (20%) was 100% effective on scolices after 6 min, and this is probably the most widely used scolicidal agent in current practice because of its availability and effective scolicidal properties[17]. In our study, this treatment was found to be 98.2% effective at the end of min and 99.5% effective at the end of 10 min[17]. Hypertonic saline can cause acute hypernatremia. H2O2 was not found to be 100% effective on scolices in our study. Because of the side effects, it is not used in many fields today. Landa García et al[18] tested four scolicidal agents (10% H2O2, 10% providone iodine, praziquantel, 10% hypertonic saline) and reported that 10% H2O2 and 10% providone iodine were much more potent than the other agents. Even though 10% H2O2 was defined as a powerful scolicidal agent in vitro by Meymerian et al[19], fatal air embolism and anaphylactic shock have also been reported with 10% H2O2.
Today, ABZ and its metabolites are not used as scolicidals for the preoperative routine. ABZ is the most widely used substance for the medical treatment of hydatid cyst disease. It has a scolicidal effect via its biologically active metabolites sulfone and sulfoxide. ABZ sulfoxide is more effective than ABZ sulfone. There is no study examining whether one of the metabolites or combinations are more effective as a preoperative scolicidal. On this topic, there have been two experimental studies by Erzurumlu et al[20–22]. He demonstrated that 20 μg/mL ABZ sulfoxide killed 5% of the scolices in 15 min, scolicidal activity was 50% with a 50 μg/mL solution, and it was 100% for a 100 μg/mL solution[20]. The other study showed that 10%, 5% and 1% ABZ solutions had complete scolicidal effects[21]. ABZ was used experimentally for percutaneous treatment of hydatid cysts. Deger et al[3] demonstrated that ABZ sulfoxide injection as a scolicidal agent in the percutaneous treatment of cystic echinococcosis seems to be effective in sheep. Yetim et al[22] further supported percutaneous treatment with the idea that ABZ solutions are effective as scolicidal solutions on rabbits. Greater scolicidal effects and fewer side effects on the hepatobiliary system are the advantages of ABZ solution[22]. It is known that scolicidal solution injection in the cysts or the biliary system leads to a rise in liver enzyme level. It has also been shown that systemically administered ABZ can lead to the same changes[3,22,23].
When the first and the second part of the study were compared, it was seen that all of the solutions that were used were more effective at the end of 10 min. This result was statistically significant, as it showed us that 5 min of preoperative waiting time was not enough.
In conclusion, none of the solutions killed 100% of the scolices at the end of 5 and 10 min. With the aim of preventing the spread to the operations’ surrounding area and the peritoneum, it is necessary to strictly protect the surrounding area of the cyst. Despite the effectiveness of ABZ metabolites, no distinctive advantage was provided compared with 20% hypertonic saline. Its harder obtainability, harder preparation, and high cost are some of the important disadvantages. For this reason, it cannot be seen as an ideal scolicidal agent. An ideal scolicidal agent is defined as being potent in low concentrations, acting in a short period time, being stable in cyst fluid, not affected by dilution with the cyst fluid, being able to kill the scolex in the cyst, being non-toxic, having low viscosity, and being readily avaliable and easily prepared, as well as being inexpensive[24,25]. In conjunction with prevention of cystic fluid spillage, total evacuation and prevention of any contact of the germinative membrane with the peritoneal surface are essential because the germinative membrane can contain viable protoscoleces despite proper cyst fluid inactivation. Walling off the surgical field with laparotomy sponges soaked in scolicidal agents is the most important step in hydatid cyst surgery. If ABZ metabolites can be obtained for commercial use and can be inexpensive, the usage of them could be more common. Combined and sulfoxide solutions were found to be more effective than sulfone. In our clinical practice, it is usually the 20% hypertonic saline solution that is used. However, it presents serious intraoperative problems related to hypernatremia. Therefore, we need less harmful but more effective drugs in hydatid disease treatment. Our study sheds light on the fact that ABZ metabolites may well meet this requirement.
COMMENTS
Background
Using scolicidal agents is of great importance in hydatid disease. The aim of this study was to find the most effective and appropriate scolicidal agents.
Research frontiers
Albendazole (ABZ) metabolites are highly effective as scolicidal agents. When compared with each other, combined and sulfoxide solutions were found to be more effective than sulfone. When it comes to the comparison of ABZ metabolites with 20% hypertonic saline, no distinctive advantage was provided
Applications
ABZ metabolites, the most effective scolicidal agents, hydatid disease treatment, the comparison of various scolicidal agents.
Terminology
Hydatid disease is a potentially fatal parasitic disease that can affect many animals, including wildlife, commercial livestock and humans. ABZ is a broad spectrum anti-protozoal and anti-helminthic compound used as a drug indicated for the treatment of a variety of worm infestations. ABZ metabolites include sulfone, sulfoxide, and the combined solution.
Peer review
The manuscript deals with the topic with adequate methods and conclusive results. It’s very interesting.
Peer reviewer: Valentin Fuhrmann, MD, Department of Internal Medicine 4, Intensive Care Unit, Medical University Vienna, Waehringer Guertel 18-20, Vienna A-1090, Austria
S- Editor Li DL L- Editor Logan S E- Editor Zheng XM
References
- 1.Ramos G, Orduña A, García-Yuste M. Hydatid cyst of the lung: diagnosis and treatment. World J Surg. 2001;25:46–57. doi: 10.1007/s002680020007. [DOI] [PubMed] [Google Scholar]
- 2.Poston JG, Blumgart HL. Surgical Management of Hepatobiliary and Pancreatic Disorders. In: S Tagliacozzo., editor. Management of hydatid disease of the liver. Vol. 25. Taylor & Francis: London; 2003. pp. 215–235. [Google Scholar]
- 3.Deger E, Hokelek M, Deger BA, Tutar E, Asil M, Pakdemirli E. A new therapeutic approach for the treatment of cystic echinococcosis: percutaneous albendazole sulphoxide injection without reaspiration. Am J Gastroenterol. 2000;95:248–254. doi: 10.1111/j.1572-0241.2000.01652.x. [DOI] [PubMed] [Google Scholar]
- 4.Yorganci K, Sayek I. Surgical treatment of hydatid cysts of the liver in the era of percutaneous treatment. Am J Surg. 2002;184:63–69. doi: 10.1016/s0002-9610(02)00877-2. [DOI] [PubMed] [Google Scholar]
- 5.Akhan O, Ozmen MN. Percutaneous treatment of liver hydatid cysts. Eur J Radiol. 1999;32:76–85. doi: 10.1016/s0720-048x(99)00116-3. [DOI] [PubMed] [Google Scholar]
- 6.Sherlock S, Dooley J. Diseases of the liver and biliary system. Blackwell Science: London; 1997. pp. 515–520. [Google Scholar]
- 7.Erzurumlu K, Hökelek M, Gönlüsen L, Tas K, Amanvermez R. The effect of albendazole on the prevention of secondary hydatidosis. Hepatogastroenterology. 2000;47:247–250. [PubMed] [Google Scholar]
- 8.Redondo PA, Alvarez AI, Garcia JL, Larrodé OM, Merino G, Prieto JG. Presystemic metabolism of albendazole: experimental evidence of an efflux process of albendazole sulfoxide to intestinal lumen. Drug Metab Dispos. 1999;27:736–740. [PubMed] [Google Scholar]
- 9.García-Llamazares JL, Alvarez-de-Felipe AI, Redondo-Cardeña PA, Prieto-Fernández JG. Echinococcus granulosus: membrane permeability of secondary hydatid cysts to albendazole sulfoxide. Parasitol Res. 1998;84:417–420. doi: 10.1007/s004360050420. [DOI] [PubMed] [Google Scholar]
- 10.Urrea-París MA, Moreno MJ, Casado N, Rodriguez-Caabeiro F. In vitro effect of praziquantel and albendazole combination therapy on the larval stage of Echinococcus granulosus. Parasitol Res. 2000;86:957–964. doi: 10.1007/pl00008526. [DOI] [PubMed] [Google Scholar]
- 11.Sonişik M, Korkmaz A, Besim H, Karayalçin K, Hamamci O. Efficacy of cetrimide-chlorhexidine combination in surgery for hydatid cyst. Br J Surg. 1998;85:1277. doi: 10.1046/j.1365-2168.1998.00823.x. [DOI] [PubMed] [Google Scholar]
- 12.Ingold K, Bigler P, Thormann W, Cavaliero T, Gottstein B, Hemphill A. Efficacies of albendazole sulfoxide and albendazole sulfone against In vitro-cultivated Echinococcus multilocularis metacestodes. Antimicrob Agents Chemother. 1999;43:1052–1061. doi: 10.1128/aac.43.5.1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kitzman D, Cheng KJ, Fleckenstein L. HPLC assay for albendazole and metabolites in human plasma for clinical pharmacokinetic studies. J Pharm Biomed Anal. 2002;30:801–813. doi: 10.1016/s0731-7085(02)00382-5. [DOI] [PubMed] [Google Scholar]
- 14.Okelo GB, Hagos B, Ng'ang'a JN, Ogeto JO. Pharmacokinetics of albendazole in children with hydatid disease. East Afr Med J. 1993;70:643–645. [PubMed] [Google Scholar]
- 15.Lacey E. Mode of action of benzimidazoles. Parasitol Today. 1990;6:112–115. doi: 10.1016/0169-4758(90)90227-u. [DOI] [PubMed] [Google Scholar]
- 16.Besim H, Karayalçin K, Hamamci O, Güngör C, Korkmaz A. Scolicidal agents in hydatid cyst surgery. HPB Surg. 1998;10:347–351. doi: 10.1155/1998/78170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Urrea-París MA, Moreno MJ, Casado N, Rodriguez-Caabeiro F. In vitro effect of praziquantel and albendazole combination therapy on the larval stage of Echinococcus granulosus. Parasitol Res. 2000;86:957–964. doi: 10.1007/pl00008526. [DOI] [PubMed] [Google Scholar]
- 18.Landa García JI, Alonso E, Gonzalez-Uriarte J, Rodriguez Romano D. Evaluation of scolicidal agents in an experimental hydatid disease model. Eur Surg Res. 1997;29:202–208. doi: 10.1159/000129525. [DOI] [PubMed] [Google Scholar]
- 19.Meymerian E, Luttermoser GW, Frayha GJ, Schwabe CW, Prescott B. Host-parasite relationships in echinococcosis: x.laboratory evaluation of chemical scollcides as adjuncts to hydatid surgery. Ann Surg. 1963;158:211–215. doi: 10.1097/00000658-196308000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erzurumlu K, Hokelek M, Baris S, Sahin M, Birinci A, Amanvermez R, Tac K. Effect of albendazole sulfoxide solution on the scolices and the hepatobiliary system. Eur Surg Res. 1998;30:433–438. doi: 10.1159/000008610. [DOI] [PubMed] [Google Scholar]
- 21.Erzurumlu K, Ozdemir M, Mihmanli M, Cevikbaş U. The effect of intraoperative mebendazole-albendazole applications on the hepatobiliary system. Eur Surg Res. 1995;27:340–345. doi: 10.1159/000129418. [DOI] [PubMed] [Google Scholar]
- 22.Yetim I, Erzurumlu K, Hokelek M, Baris S, Dervisoglu A, Polat C, Belet U, Buyukkarabacak Y, Guvenli A. Results of alcohol and albendazole injections in hepatic hydatidosis: experimental study. J Gastroenterol Hepatol. 2005;20:1442–1447. doi: 10.1111/j.1440-1746.2005.03843.x. [DOI] [PubMed] [Google Scholar]
- 23.Gil-Grande LA, Rodriguez-Caabeiro F, Prieto JG, Sánchez-Ruano JJ, Brasa C, Aguilar L, García-Hoz F, Casado N, Bárcena R, Alvarez AI. Randomised controlled trial of efficacy of albendazole in intra-abdominal hydatid disease. Lancet. 1993;342:1269–1272. doi: 10.1016/0140-6736(93)92361-v. [DOI] [PubMed] [Google Scholar]
- 24.Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull World Health Organ. 1996;74:231–242. [PMC free article] [PubMed] [Google Scholar]
- 25.Puryan K, Karadayi K, Topcu O, Canbay E, Sumer Z, Turan M, Karayalcin K, Sen M. Chlorhexidine gluconate: an ideal scolicidal agent in the treatment of intraperitoneal hydatidosis? World J Surg. 2005;29:227–230. doi: 10.1007/s00268-004-7587-x. [DOI] [PubMed] [Google Scholar]
- 26.Caglar R, Yuzbasioglu MF, Bulbuloglu E, Gul M, Ezberci F, Kale IT. In vitro effectiveness of different chemical agents on scolices of hydatid cyst. J Invest Surg. 2008;21:71–75. doi: 10.1080/08941930701883640. [DOI] [PubMed] [Google Scholar]
- 27.Frayha GJ, Bikhazi KJ, Kachachi TA. Treatment of hydatid cysts (Echinococcus granulosus) by Cetrimide (R) Trans R Soc Trop Med Hyg. 1981;75:447–450. doi: 10.1016/0035-9203(81)90118-8. [DOI] [PubMed] [Google Scholar]
- 28.Kayaalp C, Balkan M, Aydin C, Ozgurtas T, Tanyuksel M, Kirimlioglu V, Akoglu M, Oner K, Pekcan M. Hypertonic saline in hydatid disease. World J Surg. 2001;25:975–979. doi: 10.1007/s00268-001-0065-9. [DOI] [PubMed] [Google Scholar]


