Abstract
AIM: To retrospectively collect inpatient and outpatient data and to assess the use of endoscopic procedures during the years 1991, 1997 and 2003 to analyse for trends.
METHODS: This retrospective survey was conducted in a University-associated Gastroenterology Unit offering secondary and tertiary health care services for a population of approximately 182 000 people in Southern New Zealand. Data collected included patient contacts (in- and outpatients), gastroscopic and colonoscopic investigations.
RESULTS: We observed a significant increase in the absolute numbers of patient contacts over the years (1991: 2308 vs 1997: 2022 vs 2003: 2783, P < 0.0001) with inflammatory bowel disease, other diseases of the colon, anus and rectum and iron studies related disorders decreasing significantly but liver disease and constipation increasing linearly over time. The use of endoscopy services remained relatively stable but colonoscopic investigations for a positive family history of colorectal cancer increased significantly while more gastroscopies were performed for unexplained anaemia.
CONCLUSION: The whole spectrum of gastroenterology contacts was studied. A substantial proportion of colonoscopies and outpatient consultations were undertaken to screen for colorectal cancer. This proportion is likely to grow further. Our findings have implications for the recruitment and training of the next generation of gastroenterologists.
Keywords: Colonoscopy, Colorectal cancer, Disease trends, Endoscopy, Gastroenterology, Hepatitis, Inflammatory bowel disease, Recruitment, Workforce
INTRODUCTION
The worldwide demand for gastroenterological services is growing. In order to adapt a training curriculum for future gastroenterologists and to allocate health resources, disease trends and the workload of gastroenterologists need to be monitored closely[1–3]. The literature on this topic is sparse. In 1973, Switz first described the practice of gastroenterologists in Virginia, USA[4] but only a few studies followed, mainly focussing on specific procedures or diagnoses. Manning et al (1980) surveyed the practice of a single gastroenterologist[5] and in 1984 an analysis of the working patterns of 500 members of the American Gastroenterological Association was published, focussing mainly on functional disorders[6]. A more general profile of a district hospital gastroenterology service in the United Kingdom was obtained by Holmes et al in 1987; there was little change over a 12 year period[7]. The most recent survey of practice patterns was conducted in the USA by Russo et al and was published in 1999[8].
However, each of these surveys had limitations and was therefore not suitable for generalisation. The Southern Island of New Zealand is mostly rural with approximately 182 000 people scattered over an area of about 32 000 sq km and is therefore comparable to many other regions outside the large population centres of Asia, Europe and the Americas. A difficult and often unmet task is to ringfence health resources (funding, staffing and facilities) prospectively so that the health needs of the population can be met. Long distances and a borderline population size make the justification for investments difficult. Projected data for disease and demand trends are of utmost importance. There is no published New Zealand data on the workload of gastroenterologists and the use of endoscopy procedures.
The goals of this study were (1) to retrospectively collect inpatient and outpatient data and (2) to assess the use of endoscopic procedures during the years 1991, 1997 and 2003 to examine the demographics of patients seen by the service and to analyse trends in diseases seen during these periods.
MATERIALS AND METHODS
Study population
This survey was conducted in the Dunedin Public Hospital Gastroenterology Unit. The hospital serves as the only secondary and tertiary public referral centre for a population of approximately 182 000 people mainly in the Otago Region of the South Island of New Zealand. The majority of people in this area identify themselves as European in ethnic origin, with 5.9% identifying themselves as Maori, 3.1% as Asian, and 1.5% as Pacific Islanders[9]. These numbers were relatively stable over the observed period. The next advanced public health care centres are to the north or to the south and approximately 4 h by car.
The Gastroenterology Unit is usually staffed by one full-time consultant, two part time (0.5) consultants and one full-time registrar. Patients have access through referrals from local general practitioners and hospital specialists. The unit offers in- and outpatient specialist consultations and diagnostic procedures such as upper and lower diagnostic and therapeutic endoscopies, endoscopic retrograde cholangio-pancreatico-graphy (ERCP), trans-abdominal ultrasound, liver biopsy, and pH telemetry. Patients in general have the possibility to access private services but transfer to a public centre out of area is not possible.
Prior to the commencement of this study, ethical approval was obtained from the Lower South Regional Ethics Committee. The data collection was performed in two phases by two separate groups of final year medical students as part of their health-care evaluation projects during their attachment to the Department of Preventive and Social Medicine. Each phase included data from the same years: 1991, 1997 and 2003.
Data collection
The absolute number of patient contacts (i.e. individual patients might have been seen more than once) including inpatients (IP; first and subsequent admissions) and outpatients (OP; as new or follow-up visits) was determined for the years concerned. Disease trends were determined based on the diagnosis on first presentation of the disease. Excluded from analysis were deceased patients as their files had been destroyed, and those with missing files. At the time of our analysis in 2005/2006, 23.9% of all patients first seen in 1991 were deceased, compared to 10.4% and 4.1% first seen in 1997 and 2003, respectively. The proportion of missing data ranged from 1% to 4% for the three years combined.
Data was obtained via the hospital computerised patient management system. In addition, OP diagnoses were obtained by retrieving the relevant clinic letters from the hospital’s medical record filing system.
Diagnostic data were in the form of International Classification of Disease Version 9 (ICD-9) codes (1991 and 1997) and ICD-10 codes (2003), providing all the diagnoses recorded during each admission. The ICD-9 codes were matched electronically to the ICD-10 codes so as to simplify analysis. When more than one gastrointestinal diagnosis was present in the raw data, it was ranked numerically by clinical coders but not necessarily in order of relevance to the clinical presentation (primary vs secondary diagnosis). Therefore, two investigators went through all the diagnoses listed for each admission, and chose the most likely primary and secondary diagnoses for that presentation. This resulted in more diagnoses than patients or patient contacts. If numbers for an entity were too small for analysis, codes were combined into broader diagnosis groups.
Endoscopic data were collected for all patients using the gastroenterology database and the computerised patient management system. Data on ERCP (n = 309), abdominal ultrasound and pH telemetry were not included in this analysis due to the small numbers of these procedures.
Statistical analysis
Differences between years for qualitative variables were tested using a chi-squared test or, in the case of small expected counts, Fisher’s exact test. If the chi-squared test was statistically significant, linear trends were investigated using the Cochrane-Armitage (C-A) test for trend. Quantitative data was compared using analysis of variance (ANOVA). The level of significance for all tests was set at 5% and all tests were 2-sided. All statistical analyses were performed in STATA (Version 9.2) or XLSTAT (Version 2008).
RESULTS
In- and outpatient demographic features
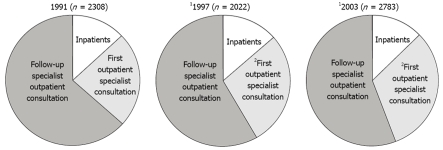
There was a statistically significant increase in the absolute numbers of patient contacts (IP-first admissions and subsequent admissions and OP-new patients and follow-up visits) over the years (Figure 1: 1991: 2308; 1997: 2022; 2003: 2783; C-A test P < 0.0001). Also, first hospital admissions and first specialist consultations (patients not seen before by this service) showed a statistically significant increase over the thirteen years between 1991 and 2003 (C-A test P < 0.001 for both, Table 1). For the three years combined, more females were seen as both in- and outpatients (58% inpatients and 61% outpatients were female, P < 0.001 for both). Overall, there was no statistically significant difference in the percentage of females seen in the in- and outpatient setting (P = 0.123). The mean age of inpatients was higher than that of outpatients (P < 0.001).
Figure 1.
Total numbers of patients seen as in- and outpatients. There is a significant increase in the total number of patients (1C-A P < 0.0001) and in the number of new patients seen (2C-A P < 0.0001). The number of follow-up patients and inpatients remained statistically unchanged.
Table 1.
Patient numbers and demographics
|
Yr |
|||
| 1991 | 1997 | 2003 | |
| Inpatients | |||
| No. of admissions1 | 173 | 310 | 391 |
| Rate per 10 000 population2 | 9 | 16 | 20 |
| Age mean (SD)3 | 54.1 (19.7) | 55.9 (18.9) | 53.4 (19.1) |
| Female n (%) | 97 (56) | 196 (63) | 210 (54) |
| Outpatients | |||
| No. of admissions1 | 553 | 469 | 756 |
| Rate per 10 000 population2 | 30 | 25 | 39 |
| No. of patients with information available | 399 | 404 | 716 |
| Age mean (SD)3 | 49.0 (19.3) | 47.0 (18.0) | 50.1 (18.5) |
| Female n (%) | 246 (62) | 256 (63) | 421 (59) |
First hospital admissions and first specialist consultations showed a statistically significant linear increase over the years (P < 0.001 for both);
Estimates of the Otago population obtained from the Ministry of Social Development website: http://www.socialreport.msd.govt.nz/regional/r-councils/otago.html;
There was a statistically significant difference in the mean age of inpatients and outpatients (P < 0.001).
Diagnoses of in- and outpatients
In the IP (Table 2) setting, the top 5 diagnostic groups over all the years studied were: liver disease and abnormal liver function tests (LFTs; 20.8%), biliary disease (16.1%), inflammatory bowel disease (IBD; 11.7%), malignancy (8.7%) and other diseases of the colon/anus/rectum (5.0%). In comparison, the top 5 diagnoses in OP (Table 2) were: liver disease and abnormal LFTs (11.4%), other functional disease (11.1%), abdominal pain of unknown cause (10.0%), constipation (7.3%) and oesophagitis/gastro-oesophageal reflux disease (GORD; 6.5%). The detailed results are presented in Table 2. The data excludes patients referred by open access for endoscopy.
Table 2.
Number (percentage) of diagnoses seen in the inpatient and outpatient setting1
| Diagnosis | 1991 | 1997 | 2003 | Total |
| Inpatient | ||||
| Liver disease (including Hepatitis)and Abnormal LFTs4 | 33 (15.1) | 90 (20.3) | 124 (23.5) | 247 (20.8) |
| Biliary disease | 22 (10.1) | 91 (20.5) | 78 (14.8) | 191 (16.1) |
| Inflammatory bowel disease3 | 38 (17.4) | 47 (10.6) | 54 (10.2) | 139 (11.7) |
| Malignancy | 23 (10.6) | 34 (7.7) | 47 (8.9) | 104 (8.7) |
| Other diseases of colon/anus/rectum3 | 13 (6.0) | 30 (6.8) | 17 (3.2) | 60 (5.0) |
| Abdominal pain unknown cause | 12 (5.5) | 9 (2.0) | 35 (6.6) | 56 (4.7) |
| Iron studies related disorders3 | 14 (6.4) | 18 (4.1) | 7 (1.3) | 39 (3.3) |
| Constipation4 | 4 (1.8) | 5 (1.1) | 29 (5.5) | 38 (3.2) |
| Pancreatic disease | 7 (3.2) | 11 (2.5) | 17 (3.2) | 35 (2.9) |
| Infective | 5 (2.3) | 14 (3.2) | 8 (1.5) | 27 (2.3) |
| Oesophagitis/GORD | 4 (1.8) | 9 (2.0) | 8 (1.5) | 21 (1.8) |
| Peptic ulcer disease | 0 (0) | 4 (0.9) | 10 (1.9) | 14 (1.2) |
| Irritable bowel syndrome | 3 (1.4) | 2 (0.5) | 1 (0.2) | 6 (0.5) |
| Haemorrhoids | 0 (0) | 1 (0.2) | 1 (0.2) | 2 (0.2) |
| Other functional disease | 0 (0) | 1 (0.2) | 0 (0) | 1 (0.1) |
| Other gastroenterological diagnosis2 | 31 (14.2) | 67 (15.1) | 82 (15.6) | 180 (15.1) |
| Non-Gastroenterological diagnosis | 9 (4.1) | 11 (2.5) | 9 (1.7) | 29 (2.4) |
| Total | 218 (100) | 444 (100) | 527 (100) | 1189 (100) |
| Outpatient | ||||
| Liver disease (including Hepatitis) and Abnormal LFTs4 | 29 (6.4) | 61 (13.5) | 108 (12.9) | 198 (11.4) |
| Other functional disease3 | 70 (15.5) | 60 (13.3) | 63 (7.6) | 193 (11.1) |
| Abdominal pain unknown cause3 | 82 (18.2) | 36 (8.0) | 55 (6.6) | 173 (10.0) |
| Constipation4 | 23 (5.1) | 26 (5.8) | 78 (9.4) | 127 (7.3) |
| Oesophagitis/GORD | 27 (6.0) | 22 (4.9) | 64 (7.7) | 113 (6.5) |
| Irritable bowel syndrome | 26 (5.8) | 24 (5.3) | 60 (7.2) | 110 (6.3) |
| Family history of bowel cancer4 | 13 (2.9) | 25 (5.5) | 70 (8.4) | 108 (6.2) |
| Other diseases of colon/rectum/anus | 23 (5.1) | 39 (8.6) | 46 (5.5) | 108 (6.2) |
| Inflammatory bowel disease | 19 (4.2) | 23 (5.1) | 47 (5.6) | 89 (5.1) |
| Haemorrhoids | 16 (3.5) | 15 (3.3) | 47 (5.6) | 78 (4.5) |
| Iron studies related disorders4 | 10 (2.2) | 4 (0.9) | 41 (4.9) | 55 (3.2) |
| Infective (excluding Hepatitis) | 8 (1.8) | 26 (5.8) | 10 (1.2) | 44 (2.5) |
| Biliary disease | 8 (1.8) | 12 (2.7) | 14 (1.7) | 34 (2.0) |
| Malignancy | 4 (0.9) | 3 (0.7) | 12 (1.4) | 19 (1.1) |
| Peptic ulcer disease | 9 (2.0) | 1 (0.2) | 8 (1.0) | 18 (1.0) |
| Pancreatic disease | 2 (0.4) | 4 (0.9) | 7 (0.8) | 13 (0.8) |
| Other gastroenterological diagnosis2 | 73 (16.2) | 52 (11.5) | 78 (9.4) | 203 (11.7) |
| Non-Gastroenterological diagnosis | 9 (2.0) | 18 (4.0) | 26 (3.1) | 53 (3.0) |
| Total | 451 (100) | 451 (100) | 834 (100) | 1736 (100) |
Number of diagnoses adds to more than the number of inpatients as a patient could have more than one diagnosis. The top 5 diagnostic categories per year and overall are highlighted;
This is a grouping of all the other minor diagnostic categories seen;
A statistically significant linear decrease over the years [Inpatient: Inflammatory bowel disease, other diseases of colon/anus/rectum and iron studies related disorders (P = 0.015, 0.040 and < 0.001, respectively); Outpatient: Abdominal pain of unknown cause and other functional disease (P < 0.001 for both)];
A statistically significant linear increase over the years [Inpatient: Liver disease and constipation (P = 0.010 and 0.001, respectively); Outpatient: Liver disease, family history of bowel cancer, constipation and iron studies related disorders (P = 0.001, < 0.001, 0.003 and 0.002, respectively)].
Disease trends
The number (percentage) of diagnoses seen in the inpatient setting is presented in Table 2. Disease trends in IP showed a statistically significant linear decline over time for inflammatory bowel disease, other diseases of the colon, anus and rectum and for iron studies related disorders as a proportion of all diagnoses (C-A tests P = 0.015, 0.040 and < 0.001, respectively). Conversely, liver disease and constipation increased linearly over time (C-A tests P = 0.010 for both). The proportion of patients seen with biliary disease spiked in 1997 but then decreased again in 2003 to levels similar to those seen in 1991, therefore, the difference across the years for biliary disease was not statistically significant (chi-square test P = 0.502). There was no statistically significant difference in the proportions of malignant disease (chi-squared test P = 0.457).
The number (percentage) of diagnoses seen in the OP setting is presented in Table 2. The OP diagnosis of abdominal pain of unknown cause and other functional disease showed a statistically significant linear decrease over the years (C-A tests P < 0.001 for both). Conversely, liver disease and abnormal LFTs, family history of bowel cancer, constipation and iron studies related disorders showed a statistically significant linear increase (C-A tests P = 0.001, < 0.001, 0.003 and 0.002, respectively) (Table 2). All other diagnoses in the in- and outpatient settings showed no statistically significant linear trend over the years studied.
Use of endoscopies
The number of procedures and the patient demographics are presented in Table 3. Over the three years studied, a total of 6705 procedures were performed; 4795 (71.5%) were gastroscopies and 1910 (28.5%) were colonoscopies.
Table 3.
Procedure numbers and patient demographics
|
Yr |
|||
| 1991 | 1997 | 2003 | |
| Colonoscopy | |||
| No. of procedures | 638 | 580 | 692 |
| Rate per 10 000 population1 | 34 | 31 | 36 |
| Age mean (SD) | 57.3 (14.5) | 58.2 (15.0) | 59.4 (14.7) |
| Female n (%)2 | 319/632 (50) | 295/537 (55) | 349/692 (50) |
| Gastroscopy | |||
| No. of procedures | 1439 | 1812 | 1544 |
| Rate per 10 000 population1 | 77 | 96 | 80 |
| Age mean (SD) | 58.9 (17.9) | 58.1 (17.5) | 58.4 (18.6) |
| Female n (%)2 | 726/1432 (51) | 824/1595 (52) | 793/1540 (51) |
Estimates of the Otago population obtained from the Ministry of Social Development website: http://www.socialreport.msd.govt.nz/regional/r-councils/otago.html;
Denominator given as data on sex was not available for all patients.
There was no statistically significant linear trend across the years for either procedure (C-A tests P = 0.379 and 0.392, respectively). Overall, there were no gender differences for both colonoscopies and gastroscopies (P = 0.132 and 0.078, respectively). The age distribution for colonoscopies changed over time (P = 0.027) while the age distribution for gastroscopies did not change (P = 0.527).
Indications and findings
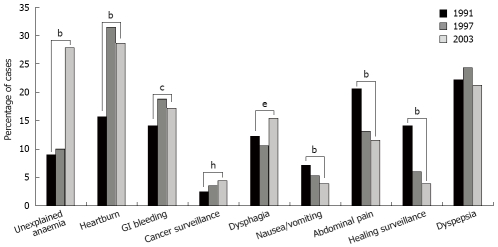
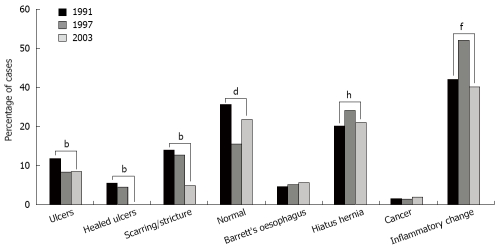
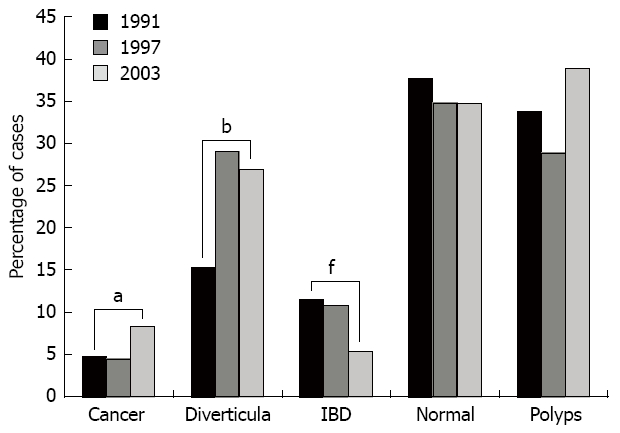
The patient indications and findings following the colonoscopies are illustrated in Figures 2 and 3, respectively. The indications and findings following the gastroscopies are illustrated in Figures 4 and 5, respectively. Some patients had more than one finding so the percentages added up to more than 100% for each of the years.
Figure 2.

Indications for colonoscopies over the three years studied. There was a significant increase in colonoscopies in patients with a past medical history of colorectal cancer (aP = 0.015) and in patients with a positive family history of colorectal cancer and/or polyps (dP < 0.001). But there was a significant decrease in colonoscopies for rectal bleeding (fP < 0.001), change in bowel habit (hP < 0.001), and IBD surveillance (iP < 0.019).
Figure 3.
Colonoscopic findings. Over the 13 years studied, significant increases in cancer (aP = 0.008) and diverticulae (bP < 0.001) were seen. In contrast, findings of inflammatory bowel disease decreased (fP < 0.001).
Figure 4.
Indications for gastroscopies over the three years studied. There was a significant increase in gastroscopies performed for unexplained anaemia and heartburn (bP < 0.001), as well as for suspected upper gastrointestinal bleeding (cP < 0.034), dysphagia (eP = 0.014) and cancer surveillance (hP = 0.01).
Figure 5.
Gastroscopic findings. The number of ulcers, healed ulcers and scarring/strictures (bP < 0.001) for all) and the proportion of normal findings (dP = 0.006) decreased significantly over the years. Findings of inflammatory changes and hiatus hernia fluctuated significantly across the years (chi-squared fP < 0.001 and hP < 0.005, respectively) (fP = 0.148 and hP = 0.478, respectively).
Indications for colonoscopy
Most colonoscopies were performed to investigate rectal bleeding or as part of the surveillance for colorectal cancer and polyps in patients with a positive family history. Interestingly, while there was a further statistically significant increase in colonoscopies performed for cancer surveillance and for patients with a family history of cancer (C-A tests P = 0.014 and P < 0.001, respectively), there was a statistically significant decrease in the frequency of colonoscopies performed for rectal bleeding (C-A test P < 0.001), change in bowel habit (C-A test P < 0.001), and IBD surveillance/ulcerative colitis (C-A test P = 0.018) over the years studied. There was a tendency towards an increase in colonoscopies for unexplained anaemia (chi-squared test P = 0.057). The remaining indications showed no statistically significant linear trend (Figure 2).
Colonoscopy findings
Most colonoscopies were either reported as normal or showed polyps or diverticulae. Over the study timeframe, statistically significant increases in cancer (C-A test P = 0.007) and diverticulae (C-A test P < 0.001) were seen. In contrast, IBD decreased (C-A test P < 0.001), and there was a tendency towards an increase in polyps (C-A test P = 0.057). The proportion of normal findings did not change across the years (chi-squared test P = 0.493) (Figure 3).
Indications for gastroscopy
Over the study timeframe, significantly more gastroscopies were performed for unexplained anaemia and heartburn (C-A test P < 0.001 for both), GI bleeding (C-A test P = 0.034), dysphagia (C-A test P = 0.014) and cancer surveillance (C-A test P = 0.010). Conversely, the frequency of gastroscopies carried out for nausea/vomiting, abdominal pain and healing surveillance decreased (C-A test P < 0.001 for all). There were no significant changes in the proportion of gastroscopies performed for dyspepsia (chi-squared test P = 0.114) (Figure 4).
Gastroscopy findings
Most gastroscopies showed only inflammatory changes. The number of ulcers, healed ulcers and scarring/strictures (C-A test P < 0.001) for all) and the proportion of normal findings (C-A test P = 0.005) decreased significantly over the years. There was no significant difference in Barrett’s oesophagus (chi-squared test P = 0.313) and cancer (chi-squared test P = 0.424) observed over time. Findings of inflammatory changes and hiatus hernia differed significantly across the years (chi-squared P < 0.001 and 0.005, respectively), but there was no significant linear trend across the years (C-A test P = 0.148 and 0.478, respectively) (Figure 5).
DISCUSSION
Our retrospective analysis over 13 years (1991-2003) aimed to collect data on in- and outpatient demographics, disease trends and endoscopic procedures in a secondary and tertiary but rural referral centre in southern New Zealand. This analysis has produced data which can be used for prospective planning in order to allocate health resources and in curriculum development for the future gastroenterological workforce.
Our study has several interesting findings, demonstrating that the working pattern for gastroentero-logists over the last 13 years has changed dramatically in several aspects. This was not only true for absolute numbers of patient contacts, but also for indications and findings. These results may permit speculation on possible trends. However, this analysis was not aimed at explaining observed disease trends in the wider context as this is very complex and needs to take both contractual arrangements as well as local characteristics into account.
The absolute numbers of patient contacts by this service increased significantly over time, despite a stable workforce both inside and outside the hospital (e.g. consultants and general practitioners). This was mainly seen for in- and outpatient contacts, while the number of investigations remained stable over the years studied. Our results show distinct differences in the types of conditions seen in inpatient versus outpatient settings (Table 2). The gastroenterology service continues to see consistently more females (60%) than males (inpatients and outpatients; P < 0.001), in contrast to the 50:50 ratio seen in the study by Bohra in Ireland[10]. Age distributions have also remained stable over the thirteen year observation period, with a mean age of 48.9 years for outpatients and 54.4 years for inpatients (P < 0.001).
Excluding endoscopies, the gastroenterology service sees approximately 660 patients for a first specialist assessment each year. The top five OP diagnoses (liver diseases, functional disorders, abdominal pain, constipation and reflux) were similar across the three years studied. This is largely in agreement with statistics published by Russo et al ranking abdominal pain, reflux, gastroenteritis, gastritis, haemorrhoidal disease and irritable bowel disease first but with liver disease in 16th place[11]. A survey among 376 members of the American Gastroenterological Association revealed Irritable Bowel Syndrome (19%) as the most common diagnosis, followed by oesophageal reflux and peptic disorders (17% and 10%, respectively), IBD (14%) and liver diseases (11%)[8]. If we summarise abdominal pain and constipation as a likely presentation of a functional disorder, this indication made up 27.3% and is therefore very much in agreement with the above survey by Russo et al[8]. However, in contrast to the view by Powell[1], but in agreement with others[5–7], there were significantly fewer patients with functional disorders compared with the beginning of the period. It is difficult to speculate on a reason for this finding, however, due to long waiting times of up to 6 mo for non-urgent referrals it is likely that only treatment-resistant cases are seen by this service.
Patients with liver disorders made up 8.5% of our outpatients and over 20% of the inpatient population with a significant increase seen over time. This might be a reflection of treatment options for Hepatitis C (testing available since 1992 in NZ), and the understanding of the significance of non-alcoholic fatty liver disease (NAFDL). However, most of these patients are admitted as day cases for liver biopsies and are therefore not truly reflecting inpatients. Such a trend was suspected by Powell[1] and in part confirmed by Russo et al[8].
We found that the absolute number of endoscopies (gastroscopies and colonoscopies) performed in our centre remained largely the same over the study period, approaching 80/10 000 gastroscopies and 36/10 000 colonoscopies in 2003 with 77/10 000 and 34/10 000 in 1991, respectively. This was largely due to contractual constraints. Scott and Atkinson in their 5-year review found that the annual number of gastroscopies doubled in the early 80’s and was expected to reach 120/10 000 in the 90’s with a similar trend expected for colonoscopies[2,12]. The Working Party of the Clinical Services Committee of the British Society of Gastroenterology stated in 1991 that an annual requirement of 100/10 000 gastroscopies and 20/10 000 colonoscopies were needed for a district general hospital[13].
In a study by Westbrook, gastroscopies were recorded at 179/10 000 population in 1997/98 in New South Wales, Australia[14]. Our almost stable lower numbers for endoscopic services can have several explanations and might not necessarily reflect the actual demand. Due to a strictly limited budget, the service in Dunedin can offer open access for gastroscopy but not for colonoscopy. Colonoscopy referrals undergo rigorous evaluation before an investigation is granted. Throughout the years the percentage of normal colonoscopies remained stable at approximately 35%. While it is relatively easy to judge the appropriateness of an investigation retrospectively, prospectively this task is difficult. It has been reported that the indication for up to 24.5% of colonoscopies[15] and 15-39% of gastroscopies[16–18] might not be appropriate. In contrast, we observed a significant increase in the number of cases of colorectal cancer at colonoscopy. This has to be seen on the background of more than a doubling of the incidence of colorectal cancer between 1956 and 1996 from 32/100 000 to 80/100 000 in male New Zealanders[19]. A significant relative increase in colonoscopies performed for cancer surveillance and for a positive family history of colorectal cancer (from 20 in 1991 to 168 in 2003) and also for unexplained anaemia was also observed reflecting our increasing understanding of preventative measures in medicine.
The relative increase in gastroscopies performed for unclear anaemia is probably a result of our greater understanding of the changing face of coeliac disease[20,21]. The awareness of the significance of Barrett’s oesophagus in the development of oesophageal cancer[22] is possibly reflected in the increased number of endoscopies performed for dysphagia and cancer surveillance. However, we did not find an increased incidence of Barrett’s oesophagus (approximately 5.5%-6.8%)[16] or cancer of the upper gastrointestinal tract (1.5%-1.2%) over the years.
In summary, we have presented data that reflect changes in the working pattern of a rural tertiary gastroenterology service over 13 years. Most of our findings are in agreement with those of previous studies. However, this analysis is unique in that we studied the whole spectrum of gastroenterology contacts in a hospital providing secondary and tertiary services. This study provides dynamic information to aid allocation of health resources and emphasises the importance of preventive medicine and also workforce development. A substantial proportion of colonoscopies and outpatient consultations are already undertaken to screen for colorectal cancer in an at-risk population. This proportion is likely to grow further, and New Zealand is no exception. In the United States, about 13% of the population is over 65 years, and projections estimate this figure may rise to 20% over the next twenty years[23]. Our study showed that the median age of patients undergoing endoscopy in Dunedin Public Hospital was almost 60 years, and our aging population means that more patients will require endoscopic procedures in the coming years.
A larger workforce will probably be necessary to meet these increasing demands. A recent review of the gastroenterology workforce available in the United States suggests that there will be a significant shortfall in gastroenterologists by 2010[24]. The baby boom generation is not only providing more patients, but those gastroenterologists who are also part of that era are now nearing retirement. In 1997, about 30% of American gastroenterologists were within 5-10 years of retirement[23]. All of this has huge implications for the recruitment and training of the next generation of gastroenterologists.
COMMENTS
Background
The field of gastroenterology in line with other areas in medicine is rapidly changing. New insight into disease progression and pathomechanisms translate into daily medicine. In order to obtain a high standard of patient care, gastroenterological training as well as recruitment has to adapt to these changes.
Innovations and breakthroughs
This analysis is unique in that the whole spectrum of gastroenterology contacts in a hospital setting providing secondary and tertiary services was studied. The Dunedin Public Hospital is located in the Otago region which is in general, sparsely populated. Nevertheless, advanced gastroenterological services are expected to meet the demand of the people. Most data is provided by large specialised centres, not suitable for units based in rural settings. However, it is these centres that need to consider trends to carefully plan training and staffing.
Applications
This study provides dynamic information to aid allocation of health resources and emphasises the importance of preventive medicine and also workforce development. Our findings have implications for the recruitment and training of the next generation of gastroenterologists and a larger workforce will be necessary to meet these increasing demands.
Peer review
This clinical study gives a well structured survey about gastroenterological diagnoses in the University-associated Hospital in Southern New Zealand. The manuscript is well written and all data are statistically verified.
Acknowledgments
The work for this project was carried out as a trainee intern healthcare evaluation project in the Department of Preventive and Social Medicine using departmental funding. In addition to the named authors, the following people greatly contributed to the planning, data retrieval and interpretation of results: Aaron Zhang, Aimée Rondel, Chris Hopkins, Marie-Michelle Ernesta, Philippa Ho, Rachel Balfour, Alice Pan, Hannah Ross, Edward Bebb, Peter Caswell-Smith and Ben Hayward. We thank Professor Gilbert O Barbezat, Dr. Martin Schlup and Dr. Ralf Lübcke for their clinical input and critical review of the manuscript.
Peer reviewer: Nikolaus Gassler, Professor, Institute of Pathology, University Hospital RWTH Aachen, Pauwelsstrasse 30, 52074 Aachen, Germany
S- Editor Cheng JX L- Editor Webster JR E- Editor Lin YP
References
- 1.Powell DW. What will the gastroenterologist do all day in the new millennium? J Clin Gastroenterol. 1999;29:295–296. doi: 10.1097/00004836-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Scott B. Endoscopic demands in the 90's. Gut. 1990;31:125–126. doi: 10.1136/gut.31.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sung JJ. Changing role of endoscopy in the new millennium. Bushell Lecture, Asia-Pacific Digestive Week 2001. J Gastroenterol Hepatol. 2002;17:369–373. doi: 10.1046/j.1440-1746.2002.02695.x. [DOI] [PubMed] [Google Scholar]
- 4.Switz DM. What the gastroenterologist does all day. A survey of a state society's practice. Gastroenterology. 1976;70:1048–1050. [PubMed] [Google Scholar]
- 5.Manning AP, Long TT, Tyor MP. Analysis of patients referred to a gastroenterologist practicing in a community hospital. Gastroenterology. 1980;79:566–570. [PubMed] [Google Scholar]
- 6.Mitchell CM, Drossman DA. Survey of the AGA membership relating to patients with functional gastrointestinal disorders. Gastroenterology. 1987;92:1282–1284. doi: 10.1016/s0016-5085(87)91099-7. [DOI] [PubMed] [Google Scholar]
- 7.Holmes KM, Salter RH, Cole TP, Girdwood TG. A profile of district hospital gastroenterology. J R Coll Physicians Lond. 1987;21:111–114. [PMC free article] [PubMed] [Google Scholar]
- 8.Russo MW, Gaynes BN, Drossman DA. A national survey of practice patterns of gastroenterologists with comparison to the past two decades. J Clin Gastroenterol. 1999;29:339–343. doi: 10.1097/00004836-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 9.2001 New Zealand Census Data.Otago District Healthboard Area. Available from: URL: http://www.stats.govt.nz/census/2001-census-data/default.htm.
- 10.Bohra S, Byrne MF, Manning D, Smyth C, Patchett SE, Murray FE. A prospective analysis of inpatient consultations to a gastroenterology service. Ir Med J. 2003;96:263–265. [PubMed] [Google Scholar]
- 11.Russo MW, Wei JT, Thiny MT, Gangarosa LM, Brown A, Ringel Y, Shaheen NJ, Sandler RS. Digestive and liver diseases statistics, 2004. Gastroenterology. 2004;126:1448–1453. doi: 10.1053/j.gastro.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 12.Scott B, Atkinson M. Gastroenterology services: a regional review of changes over a five year period (1981-86) Gut. 1989;30:695–700. doi: 10.1136/gut.30.5.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Provision of gastrointestinal endoscopy and related services for a district general hospital. Working Party of the Clinical Services Committee of the British Society of Gastroenterology. Gut. 1991;32:95–105. doi: 10.1136/gut.32.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Westbrook JI. Trends in the utilization of diagnostic upper GI endoscopy in New South Wales, Australia, 1988 to 1998. Gastrointest Endosc. 2002;55:847–853. doi: 10.1067/mge.2002.124634. [DOI] [PubMed] [Google Scholar]
- 15.Minoli G, Meucci G, Bortoli A, Garripoli A, Gullotta R, Leo P, Pera A, Prada A, Rocca F, Zambelli A. The ASGE guidelines for the appropriate use of colonoscopy in an open access system. Gastrointest Endosc. 2000;52:39–44. doi: 10.1067/mge.2000.106683. [DOI] [PubMed] [Google Scholar]
- 16.Froehlich F, Repond C, Mullhaupt B, Vader JP, Burnand B, Schneider C, Pache I, Thorens J, Rey JP, Debosset V, et al. Is the diagnostic yield of upper GI endoscopy improved by the use of explicit panel-based appropriateness criteria? Gastrointest Endosc. 2000;52:333–341. doi: 10.1067/mge.2000.107906. [DOI] [PubMed] [Google Scholar]
- 17.Chan YM, Goh KL. Appropriateness and diagnostic yield of EGD: a prospective study in a large Asian hospital. Gastrointest Endosc. 2004;59:517–524. doi: 10.1016/s0016-5107(04)00002-1. [DOI] [PubMed] [Google Scholar]
- 18.Rossi A, Bersani G, Ricci G, Defabritiis G, Pollino V, Suzzi A, Gorini B, Alvisi V. ASGE guidelines for the appropriate use of upper endoscopy: association with endoscopic findings. Gastrointest Endosc. 2002;56:714–719. doi: 10.1067/mge.2002.129222. [DOI] [PubMed] [Google Scholar]
- 19.Cancer Control in New Zealand. Cancer in New Zealand-trends and projections. Public Health Intelligence Occasional Bulletin No. 15. Vol. 56. New Zealand Ministry of Health: Wellington; 2002. [Google Scholar]
- 20.Dewar DH, Ciclitira PJ. Clinical features and diagnosis of celiac disease. Gastroenterology. 2005;128:S19–S24. doi: 10.1053/j.gastro.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Lo W, Sano K, Lebwohl B, Diamond B, Green PH. Changing presentation of adult celiac disease. Dig Dis Sci. 2003;48:395–398. doi: 10.1023/a:1021956200382. [DOI] [PubMed] [Google Scholar]
- 22.Flejou JF. Barrett's oesophagus: from metaplasia to dysplasia and cancer. Gut. 2005;54 Suppl 1:i6–i12. doi: 10.1136/gut.2004.041525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hall KE, Proctor DD, Fisher L, Rose S. American gastroenterological association future trends committee report: effects of aging of the population on gastroenterology practice, education, and research. Gastroenterology. 2005;129:1305–1338. doi: 10.1053/j.gastro.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 24.Meyer GS, Jacoby I, Krakauer H, Powell DW, Aurand J, McCardle P. Gastroenterology workforce modeling. JAMA. 1996;276:689–694. [PubMed] [Google Scholar]