Abstract
Objective:
Research has consistently identified a family history of alcoholism as a risk factor for alcohol-related problems, and global positive expectancies have been found to moderate this association. High rates of comorbidity between alcohol use and anxiety disorders suggest that a family history of anxiety disorders may also increase risk. Further, expectations of negative reinforcement (e.g., tension reduction) have been found to moderate the influence of anxiety-related traits. The current study sought to extend previous research by examining the influence of parental history of alcoholism, anxiety disorders, and the combination, as predictors of alcohol-related problems. Expectancies of global positive changes and tension reduction were hypothesized to moderate the influence of parental history of alcoholism and anxiety, respectively.
Method:
Direct interviews with parents assessed their history of alcoholism and anxiety for 144 offspring (ages 18-32; 53.5% male) creating four groups: those with a parental history of alcoholism (27.80%), anxiety (22.20%), both alcoholism and anxiety (33.30%), and no history of psychopathology (16.70%). Established measures assessed the offsprings'alcohol expectancies, alcohol use, and alcohol-related problems.
Results:
Although expected interactions between parental alcoholism and global positive expectancies and between parental anxiety and tension-reduction expectancies were not found, global positive expectancies were associated with alcohol-related problems among the group with parental history of both alcoholism and anxiety.
Conclusions:
The results suggest that the relation between parental history of alcoholism and global positive expectancies observed in previous studies may be strongest among individuals with a comorbid parental history of alcohol and anxiety disorders. Incorporating expectancies into interventions targeting individuals with a comorbid parental history of alcohol and anxiety disorders may have utility.
Cross-sectional and longitudinal family and genetic studies of alcohol and anxiety disorders suggest that each diagnosis confers risk for the development of the other, with the likelihood of carrying either diagnosis increased two- to five-fold by the presence of the other (Burns and Teesson, 2005; Kushner et al., 1999; Merikangas et al., 1994; Zimmermann et al., 2003). As such, alcohol-use disorders (AUDs) often occur concurrently with the following anxiety disorders: agoraphobia (Davids et al., 2002), generalized anxiety disorder (Grant et al., 2005), obsessive-compulsive disorder, social anxiety disorder, panic disorder, and posttraumatic stress disorder (Ballie and Sannibale, 2007; Burns and Teesson, 2005). According to recent comorbidity estimates, approximately 12% and 23.5% of people meeting Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994), diagnostic criteria for alcohol abuse and dependence, respectively, concurrently experience an anxiety disorder (Grant et al., 2004). However, comorbidity estimates topping 55% have been reported (Conway et al., 2003). In addition, current research suggests that the co-occurrence of alcohol dependence and an anxiety disorder(s), particularly panic disorder, social phobia, or posttraumatic stress disorder, is related to increased severity of dependence symptoms and the experience of alcohol-related problems (Burns and Teesson, 2005).
Given the substantial rates of comorbidity, it is possible that genetic risk for one disorder may place an individual at risk for the other disorder. For example, research has demonstrated that a positive family history of alcoholism increases lifetime risk for developing an anxiety disorder to upwards of 55% (e.g., Conway et al., 2003; Davids et al., 2002; Merikangas et al., 1994). It has been well established that risk for developing an AUD is determined, at least in part, by genetics. Research suggests that, after controlling for sociodemographic and psychiatric variables, between 50% (Knopik et al., 2004; Liu et al., 2004) and 79% (Heath et al., 1999) of the variance in risk for AUDs and age at diagnosis can be attributed to genetic factors. Although the role of a positive family history of alcoholism in the development of AUDs and problems is well documented, comparatively little is known about the contribution of family history of anxiety. However, the argument for a dual-risk or comorbidity-driven risk model is bolstered by evidence for substantial genetic influence on the development of anxiety disorders.
Like AUDs, anxiety disorders appear to be transmitted from parent to child (Merikangas et al., 1994), with rates as high as 30% among children with positive family histories (Reich, 1986). Given the frequency of comorbidity and the possibility of shared genetic influence between AUDs and anxiety disorders, the variability in drinking behavior that is typically attributed to family history of alcoholism may actually be, in part, the result of risk for comorbid conditions. Thus, it is hard to establish the unique contribution of a parental history of alcoholism without assessing also the parental history of comorbid disorders.
The study of comorbid family history of anxiety among individuals with a positive family history of alcoholism may also be useful in understanding the mechanisms (particularly negative reinforcement mechanisms) through which alcohol-related problems develop in this high-risk group. Theoretical models on the etiology of AUDs have often focused on the principles of negative reinforcement, with the idea that drinking reduces the experience of negative emotions, specifically the experience of tension and anxiety (for a review, see Conger, 1951, 1956; Greeley and Oei, 1999). Consistent with these models, the focus on alcohol as a means to unwind or to drown one's sorrows has found its way into popular culture and media, and the self-medication or coping model depicting alcohol use as a means of dealing with stress (albeit an unsatisfactory and undesirable one) has been sustained in our cultural consciousness (e.g., Carrigan and Randall, 2003; Kuntsche et al., 2006a).
Although anecdotal evidence often supports the tension-reduction model, empirical evidence has been inconsistent (e.g., Greeley and Oei, 1999). Some researchers have suggested that the negatively reinforcing effects of alcohol may be primarily important for individuals with some underlying vulnerability, such as anxiety disorders, particularly social anxiety (e.g., Carrigan and Randall, 2003; Thomas et al., 2003; Zimmermann et al., 2003), and with high levels of anxiety sensitivity (e.g., Novak et al., 2003; Stewart and Zeitlin, 1995) and neuroticism (e.g., Kuntsche et al., 2006b; Stewart et al., 2001).
In support of an underlying vulnerability to drinking for negative reinforcement, anxiety sensitivity has been linked to increased risk for alcohol-related problems and AUDs (e.g., Schmidt et al., 2007), and a recent study demonstrated that a cognitive-behavioral intervention targeting anxiety sensitivity led to decreased drinking for conformity motives and overall reduced risk for hazardous drinking (Watt et al., 2006). In contrast, main effects of social anxiety on drinking behavior, in the absence of social anxiety disorder, have been inconsistently identified. In some cases, higher levels of social anxiety have been associated with lower levels of alcohol consumption (e.g., Eggleston et al., 2004). Inconsistent findings with respect to underlying trait vulnerability may be due, in part, to differences in expectations and motives for alcohol use. High trait anxiety is likely to be associated with heavier alcohol consumption only to the extent that individuals with this trait have strong expectations that drinking will reduce tension. Such expectations may lead to the development of negative reinforcement motives for drinking and the eventual development of alcohol-related problems.
A number of studies have demonstrated that alcohol expectancies, or the beliefs that individuals have about how alcohol will either positively or negatively affect their mood, emotion, and behavior (Leigh, 1989), impact a range of alcohol-related behaviors and outcomes. Alcohol-outcome expectancies result from both direct personal experience with alcohol and from modeling the drinking behavior of other individuals, and they have been shown to differ by family history status (Lundahl et al., 1997; Pastor and Evans, 2003). In general, expectations of positive outcomes of drinking, which include tension reduction, have been found to predict later drinking behavior and the development of alcohol-related problems (e.g., Borjesson and Dunn, 2001; Kassel et al., 2000; Leigh, 1999; Satre and Knight, 2001). In addition to expectancies, the related construct of alcohol motives has played an important role in tension-reduction models of alcohol use. Coping motives represent a significant risk factor for heavy drinking, and possibly even more so for the development of alcohol-related problems (e.g., Catanzaro and Laurent, 2004; Kassel et al., 2000; Neighbors et al., 2007; Rafnsson et al., 2006).
Although expectancies and motives have been shown to be consistent risk factors for alcohol use and abuse, the contention that these cognitions will characterize individuals with high levels of trait negative affect has found only modest support. For example, high levels of neuroticism, a personality trait commonly associated with the experience of anxiety, were found to relate to reliance on coping motives (Stewart and Devine, 2000). At the same time, a study of social anxiety found that individuals differing in levels of social anxiety (low, medium, high) did not differ in drinking motives, including coping motives (Ham et al., 2007). Thus, not all anxious drinkers expect or drink to receive tension reduction. Such findings have led to further refinements to the tension-reduction model whereby interactions between trait anxiety and alcohol-related cognitions (particularly for tension reduction) are hypothesized.
In support of revised tension-reduction model hypotheses, there is some evidence to suggest that the efficacy of tension-reduction expectancies and coping motives in predicting drinking behavior may be limited to individuals with high levels of trait anxiety, at either clinical or subclinical levels (Abrams and Kushner, 2004; Tran and Hagga, 2002; Tran et al., 1997). For example, Tran and Haaga (2002) found that, for individuals with comorbid alcohol abuse and social anxiety, tension-reduction expectancies were related to increased alcohol consumption. At the same time, anxious individuals who did not believe that alcohol would reduce anxiety drank less than their less anxious counterparts (Tran et al., 1997). A recent study conducted by Ham and colleagues (2007) found a similar relationship between social anxiety and motives. For highly and moderately anxious individuals, strong coping motives were related to heavier alcohol use and the experience of alcohol-related problems, whereas enhancement motives (but not coping motives) were associated with increased alcohol consumption for individuals low in social anxiety. Studies have also found interactions between trait levels of anxiety sensitivity and alcohol-related cognitions (Lawyer et al., 2002; Stewart and Zeitlin, 1995). For example, anxiety sensitivity appears to serve as an important factor in determining the relationship between tension-reduction expectancies, negative reinforcement motives like drinking to cope, and drinking outcomes (Lawyer et al., 2002; Stewart and Zeitlin, 1995).
In sum, the extant literature from both expectancy and motives perspectives indicates that strongly associating alcohol with coping and enhancement may result in increased risk among individuals with high levels of anxiety. It stands to reason that those with a genetic/biological predisposition toward anxiety disorders would also be at increased risk for experiencing alcohol-related problems when strong tension-reduction expectancies or coping motives for drinking are present. Examining parental history of anxiety disorders, which provides a very broad index of genetic risk for anxiety, may help begin to answer this question.
Although no study to date has examined alcohol-related cognitions (motives or expectancies) as a moderator of the relation between a parental history of anxiety and alcohol-related problems, there is evidence that expectancies may act as a moderator of biological risk for alcohol-related problems. Two recent studies have reported significant interactions between expectancies and parental history of alcoholism in relation to the experience of alcohol-related problems such that those with a positive parental history and stronger global positive expectancies were most likely to experience problems (Conway et al., 2003; Van Voorst and Quirk, 2003). However, in both cases the relationship between positive expectancies and the quantity and frequency of alcohol use was independent of family history status. These results are consistent with research on family history effects more generally, which has identified main effects for alcohol-related problems, but not for quantity or frequency of use (Hartford et al., 1987-88; Knowles and Schroeder, 1989; Muthén and Muthén, 2000; Pandina and Johnson, 1990). Thus, the experience of alcohol-related problems may be most relevant when considering main effects and interactions among family history status, expectancies, and alcohol-related outcomes.
Given the shared genetic vulnerability for alcohol use and anxiety disorders, it seems reasonable to predict that expectancies may interact with a family history of anxiety disorders, much as they do with a family history of alcoholism. At the same time, the types of expectancies that are important may well differ by family history status. Although global positive expectancies have been found to interact with family history of alcoholism, research on the tension-reduction model suggests that tension-reduction expectancies are a more likely moderator of family history of anxiety effects.
The current study was designed to assess the relative influence of parental history of alcoholism and anxiety, as well as the interactions between parental history status and alcohol expectancies on the experience of alcohol-related problems. We expected to find an interaction between parental history of alcoholism and global positive expectancies consistent with previous work. We also expected tension-reduction expectancies to interact with parental history of anxiety much in the way that these types of beliefs have been shown to interact with other indices of anxiety vulnerability (e.g., social anxiety and anxiety sensitivity). Finally, both types of expectancies were expected to be important predictors of alcohol-related problems among individuals with a comorbid parental history of alcohol and anxiety disorders.
Method
Participants
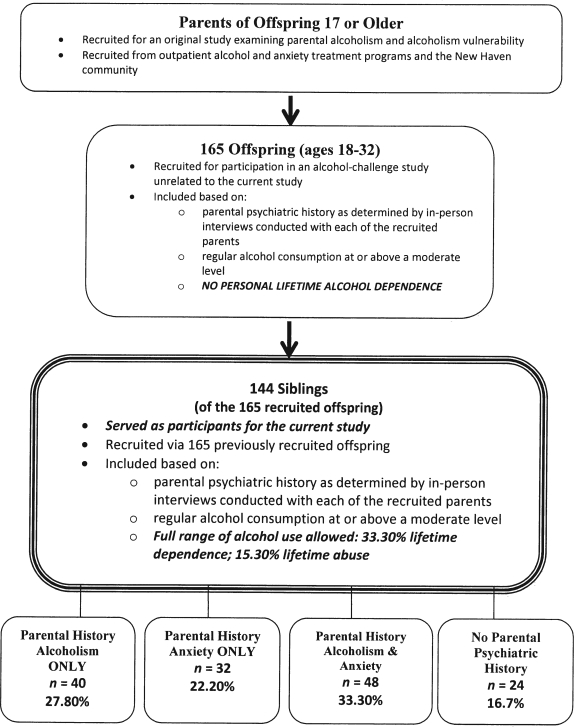
The sample for the current study comprised 144 siblings of a sample of 165 young adults originally recruited for an alcohol challenge study (Sinha et al., 1998); all participants were non-Hispanic white. The siblings (53.5% female; ages 18-32; mean [SD] = 24.04 [3.30]) were the focus of the current study because they reported a full range of alcohol-related problems and AUDs, with 33.3% meeting criteria for lifetime alcohol dependence and 15.3% for lifetime abuse. In contrast, a history of alcohol dependence was an exclusion criteria for the 165 young adults originally recruited for the alcohol challenge. Both the original alcohol challenge sample (n = 165) and the siblings (n = 144) who were the focus of the current study were recruited through their biological parents. Parents were recruited from outpatient community mental health programs for alcohol or anxiety disorders. Parents were also recruited from the broader New Haven, CT, community using random digit dialing from the telephone directory. Individuals who were white and had biological children between the ages of 18 and 30 living in or returning periodically to the area were invited to participate in a screening interview. Those who screened as potentially eligible were asked for permission to contact their offspring to ascertain their willingness to participate. If at least one adult child was willing to participate in the diagnostic study, the parent was invited to participate in the study. The following served as exclusion criteria for all offspring: parental or personal schizophrenia, schizoaffective disorder, organic psychosis, other psychotic disorders, mental retardation, or drug or alcohol dependence. Figure 1 provides a diagram of the recruitment strategy and the relation of the current study sample to the larger study from which the sample was drawn.
Figure 1.
Participant selection for the current study
For the current study, participants were categorized into four risk groups (see Table 1) based on the parent's lifetime diagnoses of alcoholism only (27.80%), anxiety only (22.20%), alcoholism/anxiety (33.30%), and no disorders (16.70%). The no-parental-history group included participants for whom neither parent carried any psychiatric diagnosis. Participants in the anxiety-only group had at least one parent diagnosed with an anxiety disorder and neither parent diagnosed with alcohol abuse/dependence. The alcoholism-only group comprised participants with at least one parent diagnosed with lifetime alcohol dependence lasting at least 2 years; parents could not carry diagnoses of anxiety or depression. To be included in the comorbid group, in addition to having at least one parent diagnosed with alcohol dependence, at least one parent (same or different) also had to carry a diagnosis of an anxiety disorder.
Table 1.
Demographics by parental history group
| Demographics | No PH (n = 24) | PHANX (n = 32) | PHALC (n = 40) | PHCOM (n = 48) |
| % Male | 33.33 | 50.00 | 35.00 | 60.40 |
| Age, mean (SD) | 24.71 (3.96) | 23.44 (4.13) | 24.44 (3.38) | 23.58 (3.71) |
| Weekly drinks, mean (SD) | 4.64 (10.81) | 2.87 (6.74) | 4.35 (11.79) | 14.14 (28.78) |
| Problems, mean (SD) | 3.04 (3.11) | 2.57 (2.72) | 5.45 (5.95) | 6.59 (8.61) |
Notes: No PH = no parental history; PHANX = parental history of anxiety; PHALC = parental history of alcoholism; PHCOM = parental history of anxiety and alcoholism combined.
Measures
Parental history status.
The Schedule for Affective Disorders and Schizophrenia for Lifetime Occurrences of Diagnoses (SADS-L) is a diagnostic interview that assesses general psychopathology (Endicott and Spitzer, 1978). A module from SADS-L determined lifetime AUD diagnoses in the sample of parents. Direct parental interviews were used to improve reliability and reduce the rate of false negatives/positives. All offspring also participated in the SADS-L interview to determine lifetime and current Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (American Psychiatric Association, 1987) alcohol-use and anxiety-disorder diagnoses.
Alcohol-associated behaviors.
The Michigan Alcoholism Screening Test (MAST) is a 25-item questionnaire used to screen for AUDs (Selzer, 1971). The MAST demonstrated good reliability (Cronbach's α = .84) in the current study. The Quantity-Frequency-Variability Index (QFVI) is a self-report measure designed to classify individuals into one of five groups (abstainer or infrequent, light, moderate, or heavy drinkers) based on the frequency of beer, wine, or distilled-spirits use and the modal maximum amount consumed (Cahalan et al., 1969). The final QFV classification is based on participants' beverage of choice. For the current study, a typical monthly consumption variable was created from the quantity and frequency items and was included in each statistical model.
Alcohol expectancies.
The Alcohol Expectancy Questionnaire (AEQ), a 90-item self-report measure, assesses individuals' beliefs about positive outcomes associated with alcohol consumption in six arenas: positive global change, sexual enhancement, social and physical pleasure, social assertion, relaxation and tension reduction, and arousal and feelings of power (Brown et al., 1987). Expectancies have been found to predict a range of alcohol-related outcomes including quantity and frequency of alcohol use and the experience of alcohol-related problems. The current study focused on global positive and tension-reduction expectancies. Reliability for the global positive and tension-reduction scales for the current sample were Cronbach's α = .87 and .82, respectively.
Statistical considerations
Examination of assumptions of normality.
Both typical monthly consumption and problems (MAST scores) were log-transformed owing to nonnormality. The log-transformed variables were used in all analyses.
Analytic approach.
Multiple regression and logistic regression were employed to test the study hypotheses using SPSS Version 15.0 (SPSS Inc., Chicago, IL). Multiple regressions assessed the main effects and interactions of parental history status and alcohol expectancies on a continuous measure of alcohol-related problems. These analyses were followed-up with logistic regression to examine clinically significant levels of alcohol problems as indicated by a score of 5 or greater on the MAST. The outcome variable in these analyses was dichotomous (yes/no clinically significant problems).
Multiple regression.
All continuous predictor variables were mean-centered, and age, gender, alcohol consumption, and participant anxiety status (i.e., diagnosis or no diagnosis) were included as covariates in all models. Three dummy-coded variables were created to contrast each of the parental history groups (alcoholism only, anxiety only, or comorbid alcoholism and anxiety) against the group with no parental history of alcoholism or anxiety.
Two separate regression models (one for each expectancy subscale) were run. In these models, the covariates (gender, age, drinking, and anxiety diagnosis) and one of the individual expectancy subscales were simultaneously entered in Block 1 as predictors of problems. Block 2 contained the three dummy-coded parental history status variables. A third block represented the two-way interactions between the given expectancy subscale and parental history status. The logistic regression models were identical to the multiple regression models with the exception of the outcome measure. Individuals scoring 5 or higher on the MAST were grouped into a high-risk group, with those scoring less than 5 considered a low-risk group.
Results
Parental history of alcoholism and anxiety and participant status
Chi-square analyses were conducted to examine the relationship between parental history of alcoholism and anxiety and participant anxiety-disorder diagnosis, monthly drinking, alcohol-dependence diagnosis, and the experience of alcohol-related problems (see Table 2). There was a statistically significant association between parental alcoholism status and participant alcohol dependence (χ2 = 14.26, 1 df, p < .001) and the experience of problems (χ2 = 8.23, 1 df, p < .01). Those with a positive parental history of alcoholism were more likely to carry a diagnosis of dependence and to experience alcohol-related problems. Parental alcoholism was not associated with participant's anxiety-disorder diagnoses or monthly drinking, and parental anxiety-disorder status was not associated with any of the anxiety or alcohol-related measures.
Table 2.
Parental history status by participant anxiety disorder, drinking, alcohol dependence, and problems
| Variable | Participant anxiety disorder (n = 128) |
Drinking (light vs heavy) (n = 143) |
Participant dependence (n = 128) |
Problems (low vs high) (n = 121) |
||||||||
| n | No | Yes | n | Light | Heavy | n | No | Yes | n | Low | High | |
| Parental alcoholism | ||||||||||||
| No | ||||||||||||
| n | 51 | 30 | 21 | 56 | 34 | 22 | 51 | 42 | 9 | 49 | 39 | 10 |
| % | 58.82 | 41.18 | 60.71 | 39.29 | 82.40 | 17.60 | 79.60 | 20.40 | ||||
| Yes | ||||||||||||
| n | 77 | 49 | 28 | 87 | 40 | 47 | 77 | 38 | 39 | 72 | 39 | 33 |
| % | 63.63 | 36.36 | 45.98 | 54.02 | 49.40 | 50.60 | 54.17 | 45.83 | ||||
| χ2 | χ2 = 0.30, 1 df, p = .58 | χ2 = 2.96, 1 df, p = .09 | χ2 = 14.26, 1 df, p <.001 | χ2= 8.23, 1 df, p < .01 | ||||||||
| Parental anxiety | ||||||||||||
| No | ||||||||||||
| n | 57 | 37 | 20 | 64 | 36 | 28 | 57 | 39 | 18 | 56 | 37 | 19 |
| % | 64.91 | 35.09 | 56.25 | 43.75 | 68.42 | 31.58 | 66.07 | 33.93 | ||||
| Yes | ||||||||||||
| n | 71 | 42 | 29 | 79 | 38 | 41 | 71 | 41 | 30 | 65 | 41 | 24 |
| % | 59.15 | 40.85 | 248.10 | 542.2 | 57.75 | 42.25 | 63.08 | 36.92 | ||||
| χ2 | χ2 = 0.44, 1 df, p = .51 | χ2 = 0.94, 1 df, p = .33 | χ2 = 1.54, 1 df, p = .22 | χ2 = 0.11, 1 df, p = .73 | ||||||||
Note: Bold indicates statistical significance.
Global positive expectancies
Multiple regression.
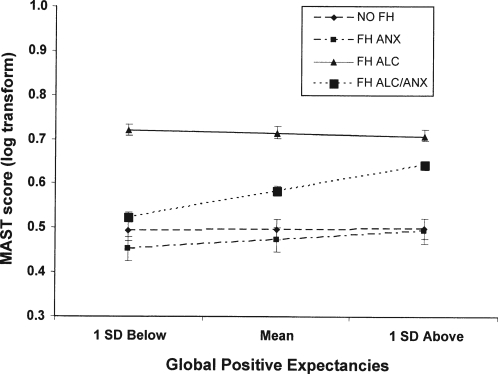
Block 1 variables for the global positive expectancies model accounted for significant variance in problems (F = 6.30, 5/97 df, p < .001; r 2 = .25). There was a significant main effect of global positive expectancies on problems (t = 3.76, 1 df, p < .001; n = 103), such that those with strong global positive expectancies experienced more problems. The variables entered at Block 2 did not account for significant variance, but the Block 3 variables were significantly associated with alcohol-related problems (F = 4.57, 3/91 df, p < .01; r 2 = .10), owing to an interaction between global positive expectancies and comorbid parental history status (t = 2.05, 1 df, p < .05; n = 95). Examination of simple main effects suggested that the interaction between comorbid status and global positive expectancies was the result of a strong relationship between expectancies and alcohol problems for those with a comorbid parental history (t = 5.39, 1 df, p < .001; n = 33) but not those without a parental history of psychopathology (t = 0.12, 1 df, p = .91; n = 21). (See Figure 2 for a graphic depiction of the interaction.)
Figure 2.
Parental history by global positive expectancy interaction. FH = family history; anx = anxiety; alc = alcoholism; MAST = Michigan Alcoholism Screening Test.
Logistic regression.
When compared with the constant-only model, variables entered in Block 1 reliably distinguished between individuals considered to be at either high or low risk (χ2 = 16.527, 5 df, p < .01; n = 144). Overall prediction success improved from 65.2% in the constant-only model to 71.30%, with 88.0% of those at low risk and 40.0% of those at high risk correctly identified. Despite the overall effect of the block of variables, Wald criterion for statistical significance indicated that none of the four predictor variables entered at Block 1 was significantly associated with problems. Addition of the dummy-coded parental-history status variables at Block 2 did not significantly add to the predictive ability of the model. However, the global positive expectancy by parental-history status variables entered in Block 3 were significant (χ2 = 8.98, 3 df, p < .05; n = 144). Overall prediction success improved to 76.5%, with 89.3% of those at low risk and 52.5% of those at high risk correctly identified. Of the three interactions, only the comorbid history and global positive expectancy interaction predicted alcohol-problem risk status (z = 4.38, p < .05). The associated odds ratio of 1.68 (95% confidence interval: 1.03-2.74) suggests that among individuals with a comorbid parental history of alcoholism and anxiety, a 1-point increase in global positive expectancies is associated with a 68.3% increase in the likelihood of experiencing alcohol-related problems.
Tension-reduction expectancies
Multiple regression.
Although Block 1 variables for the tension-reduction expectancies model accounted for significant variance in problems (F =3.33, 5/97 df, p < .01; r 2 = .15), there were no significant main effects associated with the covariates or tension-reduction expectancies. Addition of Block 2 and Block 3 variables did not account for significant variability in alcohol-related problems: All p values were greater than .05.
Logistic regression.
Results of the logic regression analysis mirrored those of the multiple regression model. When compared with the constant-only model, variables entered in Block 1 reliably distinguished between individuals considered to be at either high or low risk (χ2 = 14.37, 5 df, p < .05; n = 144). Overall prediction success improved from 65.2% in the constant-only model to 69.6%, with 86.7% of those at low risk and 37.5% of those at high risk correctly identified. According to the Wald criterion for statistical significance, none of the four predictor variables entered at Block 1 was significant. Variables entered at Blocks 2 and 3 did not significantly add to the predictive success of the model.
Discussion
Extending previous research, the current study examined relationships among family history of alcoholism, anxiety, expectancies, and alcohol-related problems. Contrary to study hypotheses and prior research, an interaction between parental history of alcoholism only and global positive expectancies was not found. Although individuals with parental history of alcoholism only were at increased risk for alcohol-related problems, this risk appeared to be independent of alcohol expectancies. However, global positive expectancies were strongly associated with alcohol-related problems for individuals with a positive parental history of both AUDs and anxiety disorders, suggesting that comorbidity may be an important factor in understanding the relationship between alcohol expectancies and alcohol outcomes.
The expected interaction between parental history of anxiety and tension reduction was not observed in this study. Neither the pure parental history of anxiety nor the comorbid parental history of anxiety and alcoholism group showed a significant relation between tension-reduction expectancies and alcohol-related problems. As already noted, global positive expectancies were an important predictor for the comorbid group, suggesting that positive reinforcement expectancies may be as much as or more important than negative reinforcement expectancies for individuals with a parental history of anxiety. Although not consistent with our study hypotheses, these results are consistent with theoretical models of anxiety and expectancies. Burke and Stephens (1999) proposed a social cognitive theory model of heavy drinking in college students with social anxiety. They suggested that expectancies for both anxiety reduction and social facilitation, in conjunction with low self-efficacy, might act as risk factors for heavy drinking among college students with high social anxiety. Consistent with the potential importance of positive reinforcement expectancies proposed in this model, Ham and colleagues (2005) found that socially anxious individuals had stronger expectancies of social assertion than those with lower levels of social anxiety. Moreover, expectancies of social assertion were related to alcohol problems in the socially anxious participants. Interestingly, they found no differences on other expectancies, including tension reduction. In a direct test of the social cognitive theory model, Gilles et al. (2006) also found that expectancies of social facilitation interacted with social anxiety and self-efficacy for avoiding heavy drinking in the prediction of drinking behavior.
Although more research is clearly needed to better understand the relationship between family history status, expectancies, and alcohol-related problems, the current results suggest potentially important implications for prevention and intervention, particularly those programs that target alcohol expectancies. Expectancy challenge studies have been shown to be moderately effective in altering drinking practices in college students (Darkes and Goldman, 1993, 1998; Wiers and Kummeling, 2004). Of particular import to the current study, Darkes and Goldman (1998) reported that challenges to both sociability and arousal expectancies resulted in reductions in alcohol consumption. The efficacy of expectancy challenges coupled with well-documented differences in expectancies by family history of alcoholism status (Brown et al., 1999; Lundahl et al., 1997; Wiers et al., 2000) might lead one to conclude that expectancy challenges could be particularly effective for individuals with a family history of alcoholism. However, the results of the current study suggest that this approach might have little or no impact among individuals with a pure parental history of alcoholism, for whom expectancies were unrelated to alcohol-related problems. Expectancy challenge might also have limited utility for individuals with a pure parental history of anxiety as they are generally at low risk and their expectancies are not strongly tied to their behavior. The individuals who might most benefit are those with a comorbid parental history of alcohol and anxiety disorders, perhaps because of the unique combination of traits of disinhibition and negative affect.
Although the current study yielded a number of interesting findings, several limitations must be considered. As is the case with all studies that rely on self-report data, the study is limited by the participants' willingness to honestly respond to the research questions. However past studies have demonstrated the validity and reliability of self-report measures (Del Boca and Noll, 2000; O'Malley et al., 2006) and have not provided strong evidence that collateral reports significantly improve the validity of data on alcohol use and related problems (Laforge et al., 2005).The analyses were also based on cross-sectional data, making it impossible to determine the direction of causation with respect to expectancies and drinking behavior. Thus, future studies with repeated measures of expectancies and drinking behavior are needed to improve our understanding of the relationships identified in the current study. Additionally, this study focused on positive expectancies and did not assess negative expectancies or include evaluations of the desirability of expectancies. Negative expectancies may serve as protective factors against the development of AUDs and may interact with family history in predicting problems. Future studies may benefit from using measures that assesses positive and negative expectancies and evaluations of each (Fromme et al., 1993).
Finally, it is important to note some of the unique characteristics of the current sample. The current study had a restricted range of participant ages (ages 18-32), and rates of alcohol dependence were quite high (33%). Although the prevalence of dependence in this sample may initially appear elevated, the estimates are only modestly discrepant from age-adjusted prevalence estimates obtained in the 1999 National Household Survey on Drug Abuse, which suggest that approximately 25% of men (ages 18-24 and 25-34) and 14% of women (ages 18-24 and 25-34) have experienced lifetime alcohol dependence (Substance Abuse and Mental Health Services Administration, 2000). Further, only 9 participants (17%) of those who did not have a parental history of alcoholism evidenced lifetime alcohol dependence. The rate of dependence in those with a parental history of alcoholism (50% in the current sample) is also consistent with the extant literature suggesting that offspring of alcohol-dependent parents are up to seven times more likely to develop an AUD themselves (Merikangas and Swendsen, 1997). In sum, the prevalence of alcohol dependence in the current sample is consistent with the literature identifying age and family history of alcoholism status as risk factors for heavy drinking and the onset of anxiety disorders and AUDs (mean age = 25). Nonetheless, characteristics of the current sample may limit the generalizability of the findings to the overall population.
Despite the aforementioned limitations, the current study extends our knowledge of the role of expectancies as moderators of the relations between parental history status and alcohol-related problems. Consistent with the social cognitive theory of drinking behavior (Burke and Stephens, 1999), the results suggest that it is critical to consider both positive and negative reinforcement expectancies when examining parental history effects. The results also highlight the importance of assessing both a parental history of alcoholism and a parental history of comorbid psychopathology with respect to alcohol expectancies and alcohol consumption. The mechanisms of risk may differ for those with pure versus comorbid parental histories, perhaps owing to unique personality traits associated with these parental histories. Although replication of the current results is needed, the rigorous direct family member interview methods used to assess parental history of alcoholism and anxiety lend confidence to the validity of the identified relationship. If future work confirms the pattern of results identified in the current study, it would suggest that incorporating expectancies into interventions targeting the subgroup of individuals with comorbid parental histories may have utility.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism grants R01AA008033 and K05AA014715 awarded to Stephanie S. O'Malley and by the MacArthur Foundation's Network on Health and Behavior.
References
- Abrams K, Kushner MG. The moderating effects of tension-reduction alcohol outcome expectancies on placebo responding in individuals with social phobia. Addict. Behav. 2004;29:1221–1224. doi: 10.1016/j.addbeh.2004.03.020. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) Washington, DC: 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Washington, DC: 1994. [Google Scholar]
- Baillie A, Sannibale C. Anxiety and drug and alcohol problems. In: Baker A, Velleman R, editors. Clinical Handbook of Co-Existing Mental Health and Drug and Alcohol Problems. New York: Routledge; 2007. pp. 197–217. [Google Scholar]
- Borjesson WI, Dunn ME. Alcohol expectancies of women and men in relation to alcohol use and perceptions of the effects of alcohol on the opposite sex. Addict. Behav. 2001;26:707–719. doi: 10.1016/s0306-4603(00)00154-4. [DOI] [PubMed] [Google Scholar]
- Brown SA, Christiansen BA, Goldman MS. The Alcohol Expectancy Questionnaire: An instrument for the assessment of adolescent and adult alcohol expectancies. J. Stud. Alcohol. 1987;48:483–491. doi: 10.15288/jsa.1987.48.483. [DOI] [PubMed] [Google Scholar]
- Brown SA, Tate SR, Vik PW, Haas AL, Aarons GA. Modeling of alcohol use mediates the effect of family history of alcoholism on adolescent alcohol expectancies. Exp. Clin. Psychopharmacol. 1999;7:20–27. doi: 10.1037//1064-1297.7.1.20. [DOI] [PubMed] [Google Scholar]
- Burke RS, Stephens RS. Social anxiety and drinking in college students: A social cognitive theory analysis. Clin. Psychol. Rev. 1999;19:513–530. doi: 10.1016/s0272-7358(98)00058-0. [DOI] [PubMed] [Google Scholar]
- Burns L, Teesson M. The prevalence and correlates of comorbid-ity between DSM-IV alcohol use disorders and anxiety disorders. In: Velotis CM, editor. Anxiety Disorder Research. Hauppauge, NY: Nova Science; 2005. pp. 293–311. [Google Scholar]
- Cahalan D, Cissin IH, Crossley HM. New Brunswick, NJ: American Drinking Practices: A National Study of Drinking Behavior and Attitudes, Rutgers Center of Alcohol Studies Monograph No. 6. 1969
- Carrigan MH, Randall CL. Self-medication in social phobia: A review of the alcohol literature. Addict. Behav. 2003;28:269–284. doi: 10.1016/s0306-4603(01)00235-0. [DOI] [PubMed] [Google Scholar]
- Catanzaro SJ, Laurent J. Perceived family support, negative mood regulation expectancies, coping, and adolescent alcohol use: Evidence of mediation and moderation effects. Addict. Behav. 2004;29:1779–1797. doi: 10.1016/j.addbeh.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Conger JJ. The effect of alcohol on conflict behavior in the albino rat. Q.J. Stud. Alcohol. 1951;12:1–29. [PubMed] [Google Scholar]
- Conger JJ. Alcoholism: Theory, problem and challenge: II. Reinforcement theory and the dynamics of alcoholism. Q.J. Stud. Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Conway KP, Swendsen JD, Merikangas KR. Alcohol expectancies, alcohol consumption, and problem drinking: The moderating role of family history. Addict. Behav. 2003;28:823–836. doi: 10.1016/s0306-4603(02)00265-4. [DOI] [PubMed] [Google Scholar]
- Darkes J, Goldman MS. Expectancy challenge and drinking reduction: Experimental evidence for a mediational process. J. Cons. Clin. Psychol. 1993;61:344–353. doi: 10.1037//0022-006x.61.2.344. [DOI] [PubMed] [Google Scholar]
- Darkes J, Goldman MS. Expectancy challenge and drinking reduction: Process and structure in the alcohol expectancy network. Exp. Clin. Psychopharmacol. 1998;6:64–76. doi: 10.1037//1064-1297.6.1.64. [DOI] [PubMed] [Google Scholar]
- Davids E, Müller MJ, Rollmann N, Burkart M, Regier-Klein E, Szegedi A, Benkert O, Maier W. Syndrome profiles in alcoholism and panic disorder with or without agoraphobia: An explorative family study. Prog. Neuro-Psychopharmacol. Biol. Psychiat. 2002;26:1079–1087. doi: 10.1016/s0278-5846(02)00225-7. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Noll JA. Truth or consequences: The validity of self-report data in health services research on addictions. Addiction. 2000;95(Suppl. No. 3):S347–S360. doi: 10.1080/09652140020004278. [DOI] [PubMed] [Google Scholar]
- Eggleston AM, Woolaway-Bickel K, Schmidt NB. Social anxiety and alcohol use: Evaluation of the moderating and mediating effects of alcohol expectancies. J. Anxiety Disord. 2004;18:33–49. doi: 10.1016/j.janxdis.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: The Schedule for Affective Disorders and Schizophrenia. Arch. Gen. Psychiat. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Fromme K, Stroot EA, Kaplan D. Comprehensive effects of alcohol: Development and psychometric assessment of a new expectancy questionnaire. Psychol. Assess. 1993;5:19–26. [Google Scholar]
- Gilles DM, Turk CL, Fresco DM. Social anxiety, alcohol expectancies, and self-efficacy as predictors of heavy drinking in college students. Addict. Behav. 2006;31:388–398. doi: 10.1016/j.addbeh.2005.05.020. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Ruan WJ, Goldstein RB, Smith SM, Saha TD, Huang B. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Med. 2005;35:1747–1759. doi: 10.1017/S0033291705006069. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Comp-ton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiat. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Greeley J, Oei T. Alcohol and tension reduction. In: Leonard KE, Blane HT, editors. Psychological Theories of Drinking and Alcoholism. 2nd Edition. New York: Guilford Press; 1999. pp. 14–53. [Google Scholar]
- Ham LS, Bonin M, Hope DA. The role of drinking motives in social anxiety and alcohol use. J. Anxiety Disord. 2007;21:991–1003. doi: 10.1016/j.janxdis.2006.10.014. [DOI] [PubMed] [Google Scholar]
- Ham LS, Carrigan MH, Moak DH, Randall CL. Social anxiety and specificity of positive alcohol expectancies: Preliminary findings. J. Psychopathol. Behav. Assess. 2005;27:115–121. [Google Scholar]
- Hartford TC, Haack MR, Spiegler DL. Positive family history for alcoholism. Alcohol Hlth Res. World. 1987-88;12:138–143. [Google Scholar]
- Heath AC, Madden PA, Bucholz KK, Dinwiddie SH, Slutske WS, Bierut LJ, Rohrbaugh JW, Statham DJ, Dunne MP, Whitfield JB, Martin NG. Genetic differences in alcohol sensitivity and the inheritance of alcoholism risk. Psychol. Med. 1999;29:1069–1081. doi: 10.1017/s0033291799008909. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Jackson SI, Unrod M. Generalized expectancies for negative mood regulation and problem drinking among college students. J. Stud. Alcohol. 2000;61:332–340. doi: 10.15288/jsa.2000.61.332. [DOI] [PubMed] [Google Scholar]
- Knopik VS, Heath AC, Madden PA, Bucholz KK, Slutske WS, Nelson EC, Stratham D, Whitfield JB, Martin NG. Genetic effects on alcohol dependence risk: Re-evaluating the importance of psychiatric and other heritable risk factors. Psychol. Med. 2004;34:1519–1530. doi: 10.1017/s0033291704002922. [DOI] [PubMed] [Google Scholar]
- Knowles EE, Schroeder DA. Familial and personality correlates of alcohol-related problems. Addict. Behav. 1989;14:537–543. doi: 10.1016/0306-4603(89)90074-9. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. ‘I drink spirits to get drunk and block out my problems…’ beverage preference, drinking motives and alcohol use in adolescence. Alcohol Alcsm. 2006a;41:566–573. doi: 10.1093/alcalc/agl046. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Who drinks and why? A review of socio-demographic, personality, and contextual issues behind the drinking motives in young people. Addict. Behav. 2006b;31:1844–1857. doi: 10.1016/j.addbeh.2005.12.028. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Erickson DJ. Prospective analysis of the relation between DSM-III anxiety disorders and alcohol use disorders. Amer. J. Psychiat. 1999;156:723–732. doi: 10.1176/ajp.156.5.723. [DOI] [PubMed] [Google Scholar]
- Laforge RG, Borsari B, Baer JS. The utility of collateral informant assessment in college alcohol research: Results from a longitudinal prevention trial. J. Stud. Alcohol. 2005;66:479–487. doi: 10.15288/jsa.2005.66.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawyer SR, Karg RS, Murphy JG, McGlynn FD. Heavy drinking among college students is influenced by anxiety sensitivity, gender, and contexts for alcohol use. J. Anxiety Disord. 2002;16:165–173. doi: 10.1016/s0887-6185(02)00092-0. [DOI] [PubMed] [Google Scholar]
- Leigh BC. Attitudes and expectancies as predictors of drinking habits: A comparison of three scales. J. Stud. Alcohol. 1989;50:432–440. doi: 10.15288/jsa.1989.50.432. [DOI] [PubMed] [Google Scholar]
- Leigh BC. Thinking, feeling, and drinking: Alcohol expectancies and alcohol use. In: Peele S, Grant M, editors. Alcohol and Pleasure. Ann Arbor, MI: Edwards Brothers; 1999. pp. 215–231. [Google Scholar]
- Liu I-C, Blacker DL, Xu R, Fitzmaurice G, Lyons MJ, Tsuang MT. Genetic and environmental contributions to the development of alcohol dependence in male twins. Arch. Gen. Psychiat. 2004;61:897–903. doi: 10.1001/archpsyc.61.9.897. [DOI] [PubMed] [Google Scholar]
- Lundahl LH, Davis TM, Adesso VJ, Lukas SE. Alcohol expectancies: Effects of gender, age, and family history of alcoholism. Addict. Behav. 1997;22:115–125. doi: 10.1016/s0306-4603(96)00022-6. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Risch NJ, Weissman MM. Comorbidity and co-transmission of alcoholism, anxiety and depression. Psychol. Med. 1994;24:69–80. doi: 10.1017/s0033291700026842. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Swendsen JD. Genetic epidemiology of psychiatric disorders. Epidemiol. Rev. 1997;19:144–155. doi: 10.1093/oxfordjournals.epirev.a017937. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. The development of heavy drinking and alcohol-related problems from ages 18 to 37 in a U.S. national sample. J. Stud. Alcohol. 2000;61:290–300. doi: 10.15288/jsa.2000.61.290. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Lee CM, Lewis MA, Fossos N, Larimer ME. Are social norms the best predictor of outcomes among heavy-drinking college students? J. Stud. Alcohol Drugs. 2007;68:556–565. doi: 10.15288/jsad.2007.68.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak A, Burgess ES, Clark M, Zolensky MJ, Brown RA. Anxiety sensitivity, self-reported motives for alcohol and nicotine use and level of consumption. J. Anxiety Disord. 2003;17:165–180. doi: 10.1016/s0887-6185(02)00175-5. [DOI] [PubMed] [Google Scholar]
- O'Malley PM, Johnston LD, Bachman JG, Schulenberg JE, Kumar R. How substance use differs among American secondary schools. Prev. Sci. 2006;7:409–420. doi: 10.1007/s11121-006-0050-5. [DOI] [PubMed] [Google Scholar]
- Pandina RJ, Johnson V. Serious alcohol and drug problems among adolescents with a family history of alcoholism. J. Stud. Alcohol. 1990;51:278–282. doi: 10.15288/jsa.1990.51.278. [DOI] [PubMed] [Google Scholar]
- Pastor AD, Evans SM. Alcohol outcome expectancies and risk for alcohol use problems in women with and without a family history of alcoholism. Drug Alcohol Depend. 2003;70:201–214. doi: 10.1016/s0376-8716(03)00007-3. [DOI] [PubMed] [Google Scholar]
- Rafnsson FD, Jonsson FH, Windle M. Coping strategies, stressful life events, problem behaviors, and depressed affect. Anxiety Stress Coping. 2006;19:241–257. [Google Scholar]
- Reich J. The epidemiology of anxiety. In: Muñoz RA, editor. Treating Anxiety Disorders. San Francisco, CA: Jossey-Bass; 1986. pp. 11–30. [Google Scholar]
- Satre DD, Knight BG. Alcohol expectancies and their relationship to alcohol use: Age and sex differences. Aging Ment. Hlth. 2001;5:73–83. doi: 10.1080/13607860020020672. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Buckner JD, Keough ME. Anxiety sensitivity as a prospective predictor of alcohol use disorders. Behav. Modificat. 2007;31:202–219. doi: 10.1177/0145445506297019. [DOI] [PubMed] [Google Scholar]
- Selzer ML. The Michigan Alcoholism Screening Test: The quest for a new diagnostic instrument. Amer. J. Psychiat. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Sinha R, Robinson J, O'Malley S. Stress response dampening: Effects of gender and family history of alcoholism and anxiety. Psycho-pharmacology. 1998;137:311–320. doi: 10.1007/s002130050624. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Devine H. Relations between personality and drinking motives in young adults. Pers. Indiv. Diff. 2000;29:495–511. [Google Scholar]
- Stewart SH, Loughlin HL, Rhyno E. Internal drinking motives mediate personality domain: Drinking relations in young adults. Pers. Indiv. Diff. 2001;30:271–286. [Google Scholar]
- Stewart SH, Zeitlin SB. Anxiety sensitivity and alcohol use motives. J. Anxiety Disord. 1995;9:229–240. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (Office of Applied Studies) Rockville, MD: Substance Abuse and Mental Health Services Administration; Summary of Findings From the 1999 National Household Survey on Drug Abuse, DHHS Publication No. (SMA) 00-3466. 2000
- Thomas SE, Randall CL, Carrigan MH. Drinking to cope in socially anxious individuals: A controlled study. Alcsm Clin. Exp. Res. 2003;27:1937–1943. doi: 10.1097/01.ALC.0000100942.30743.8C. [DOI] [PubMed] [Google Scholar]
- Tran GQ, Haaga DAF. Coping responses and alcohol outcome expectancies in alcohol abusing and non-abusing social phobics. Cog. Ther. Res. 2002;26:1–17. [Google Scholar]
- Tran GQ, Haaga DAF, Chambless DL. Expecting that alcohol use will reduce social anxiety moderates the relation between social anxiety and alcohol consumption. Cog. Ther. Res. 1997;21:535–553. [Google Scholar]
- VanVoorst WA, Quirk SW. Are relations between parental history of alcohol problems and changes in drinking moderated by positive expectancies? Alcsm Clin. Exp. Res. 2003;27:25–30. doi: 10.1097/01.ALC.0000046338.20896.EE. [DOI] [PubMed] [Google Scholar]
- Watt M, Stewart S, Birch C, Bernier D. Brief CBT for high anxiety sensitivity decreases drinking problems, relief alcohol outcome expectancies, and conformity drinking motives: Evidence from a randomized controlled trial. J. Mental Hlth. 2006;15:683–695. [Google Scholar]
- Weirs RW, Hartgers C, van den Brink W, Gunning WB, Sargeant JA. A confirmatory analysis of the hierarchical structure of positive and negative dose-related alcohol expectancies in alcoholics and the associations with family history of alcoholism. J. Stud. Alcohol. 2000;61:177–186. doi: 10.15288/jsa.2000.61.177. [DOI] [PubMed] [Google Scholar]
- Wiers RW, Kummeling RHC. An experimental test of an alcohol expectancy challenge in mixed gender groups of heavy young drinkers. Addict. Behav. 2004;29:215–220. doi: 10.1016/s0306-4603(03)00081-9. [DOI] [PubMed] [Google Scholar]
- Zimmermann P, Wittchen HU, Hofler M, Pfister H, Kessler RC, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: A 4-year community study of adolescents and young adults. Psychol. Med. 2003;33:1211–1222. doi: 10.1017/s0033291703008158. [DOI] [PubMed] [Google Scholar]