Abstract
Excessive wait times for magnetic resonance imaging (MRI) studies are a major problem in the Canadian healthcare system. To determine how requests for MRI studies are managed, the authors performed a survey of public MRI facilities in Canada. Ninety-six per cent had some method to triage MRI requests. However, only 42% had documented guidelines for prioritization, and none employed quality assurance methods to ensure that guidelines were followed. Target timelines for each prioritization category varied widely. Sixteen per cent of centres were not able to meet their target timelines for any prioritization category, and 45% of centres met target times only for some prioritization categories. Strategies for dealing with wait lists primarily involved attempts to increase capacity. No centres attempted to reduce wait times by decreasing inappropriate requests. There appears to be a need to standardize MRI wait list management given the variation in management practices and wait times observed.
Abstract
Les temps d'attente excessifs pour l'imagerie par résonance magéntique (IRM) constituent un grand problème pour le système de santé canadien. Afin de comprendre comment sont gérées les demandes d'examen par IRM, les auteurs ont mené un sondage auprès des centres d'IRM au Canada. Dans 96 % des centres, il existe une forme de triage des demandes d'IRM. Cependant, seulement 42 % sont munis de lignes directrices documentées pour établir la priorisation, et aucun d'entre eux n'emploie de méthodes d'assurance de la qualité afin d'assurer que les lignes directrices sont suivies. On observe une grande variation entre les calendriers ciblés pour chacune des catégories de priorité. Seize pour cent des centres ne peuvent respecter les temps visés, pour toute catégorie de priorité. Quarante-cinq pour cent des centres respectent les temps visés, uniquement pour certaines catégories de priorité. Les stratégies employées pour régler la question des listes d'attente consistent principalement en des tentatives pour accroître la capacité. Aucun centre n'a tenté de diminuer les temps d'attente en réduisant le nombre de demandes inappropriées. Étant donné les temps d'attente observés et la variation dans les modes de gestion, il semble y avoir un besoin de normaliser la gestion des listes d'attente pour l'IRM.
Excessive wait times for some healthcare interventions have caught the attention of governments, providers and the public (Sanmartin et al. 2000). Of particular interest to these groups are cardiac surgery, joint replacement surgery, cancer care and advanced diagnostic imaging, specifically magnetic resonance imaging (MRI). Wait times for diagnostic imaging are particularly important because they may result in delays in definitive treatment.
Efforts to reduce wait times for MRI have focused on increasing the number of diagnostic imaging devices, as Canada lags far behind other countries in this regard. For instance, Japan and the United States have 35.3 and 19.5 MRI units per million population, respectively, whereas Canada has only 4.6. (Stein 2005). The number of MRI scanners in Canada is lower than the median of 6.1 scanners per million for all countries within the Organisation for Economic Co-operation and Development (Stein 2005). The optimal number of MRI machines per capita has not been established, and the number of scanners does not indicate the number of patients scanned; however, it does provide an indication of capacity. While Canadian provinces have recently increased the number of imaging devices, it is unlikely that Canada will have such ready access to imaging as these other countries. Therefore, other approaches to wait time reduction are needed.
Improving the management of wait lists represents another approach to reducing wait times. This strategy might include the development of criteria for determining the appropriateness of imaging requests, which in turn could be used to help triage their relative urgency. A similar approach has been used for cardiac surgery (Naylor et al. 2000). In this setting, these criteria make wait list assignment more objective and equitable while also improving overall efficiency. Although the development of appropriateness criteria for MRI scanning has received some attention (Canadian Association of Radiologists 2005; ACR 2000), there is no evidence that these efforts have had an impact on practice. The role of standardized approaches to triaging requests for MRI has received almost no attention.
As part of a larger project to study wait time management, we set out to determine Canadian MRI facilities' self-reported wait times and their strategies for managing them. Specifically, we wanted to determine how facilities triaged requests for MRI (including the healthcare professionals who triaged requests and the methods by which they did so) and whether or not triaging included efforts to identify inappropriate requests. We also set out to ascertain other wait list management strategies, such as protocols for increasing capacity. If there are to be recommendations about how to improve the diagnostic imaging wait list system, it is imperative to understand how facilities are currently managing their requests for MRI.
Methods
We performed a cross-sectional study of all public MRI facilities in Canada. We identified eligible institutions using data from the Canadian Institute for Health Information (CIHI) for year 2005 and administered a telephone-based survey with the lead administrator at each centre between June 2006 and October 2006. The study was approved by the Health Research Ethics Board at the University of Alberta.
The survey contained 24 questions divided into four sections, which described facility characteristics, current MRI use and availability, prioritization methods and current wait times. To ensure the comprehensiveness of content and clarity of the questions, we prepared, iteratively, three successive drafts of our questionnaire. These were reviewed by six individuals including radiologists, radiology managers and researchers. We pilot tested the survey in six hospitals in Alberta and Ontario. We designed the survey to be completed within 15 minutes. The survey was mailed to the lead MRI administrator at each centre prior to a telephone interview. The final version of the survey was translated into French.
We treated hospitals operating under a common administrative structure (e.g., University Health Network in Toronto and Centre hospitalier de l'Université de Montréal) as single facilities. Survey responses were stored in a Microsoft Access database, and SAS v9 (Cary, NC) was used for all data manipulation and analyses. Not all centres were able to answer all questions, and thus the denominator differs slightly from question to question.
Results
Characteristics of responding centres
We identified 122 publicly funded facilities with MRI scanners in Canada. Seventynine (65%) institutions responded to our survey. This modest overall response rate reflected very high responses in the Western and Atlantic provinces (32/32 [100%] and 11/13 [85%], respectively) and lower responses from Ontario and Quebec (36/75 [48%]). Table 1 shows the characteristics of centres. Aside from region of the country, the characteristics of responding centres in terms of city size and teaching status were similar to those of non-responders.
TABLE 1.
Characteristics of centres
| Western | Central | Atlantic | ||
|---|---|---|---|---|
| Total number of centres | 32 | 75 | 13 | |
| Hospitals responding to survey | 32 (100%) | 36 (48%) | 11 (85%) | |
| City size | <100,000 | 8 (25%) | 8 (22%) | 4 (36%) |
| 100,000–1 million | 10 (31%) | 14 (39%) | 7 (64%) | |
| >1 million | 14 (44%) | 14 (39%) | 0 | |
| No. of beds | <200 | 5 (16%) | 4 (11%) | 3 (27%) |
| 200–500 | 19 (59%) | 23 (64%) | 6 (55%) | |
| >500 | 8 (25%) | 9 (25%) | 2 (18%) | |
| Teaching hospital | 17 (53%) | 16 (44%) | 4 (36%) | |
| Referral centre | 30 (94%) | 32 (88.9%) | 10 (91%) | |
| Cancer centre | 12 (38%) | 16 (44%) | 7 (64%) | |
MRI utilization
Of the 79 responding centres, 58 had one MRI scanner, 18 had more than one and three centres relied on portable scanners that visited on a regular basis. The median number of scanning hours per week was 93.5 (interquartile range [IQR]: 62.5–123.3). MRI scanners were routinely used on weekends in 46/79 (58%) of facilities. Only two centres (3%) routinely operated their MRI scanners on a 24/7 basis. The median number of studies performed annually was 6303.5 (IQR: 4157–8916), with approximately 90% of scans at each centre involving outpatients (median 91.5%, IQR: 86.5%–94.0%).
Approaches to prioritization
Almost all (75/78, 96%) centres used some method to triage requests for MRI studies to different priority levels. Ninety-six per cent (72/75) identified clinical urgency as the primary factor that determined priority. However, only 42% (33/79) had explicit, documented criteria to guide the prioritization process. Prioritization was usually based on implicit assessments by the radiologist, using a handwritten requisition submitted by an ordering physician.
In those sites that triage MRI requests, prioritization was performed solely by a radiologist in 81% (61/75) of centres. In one centre, prioritization was performed solely by a technologist. In the remaining 13 centres (17%), prioritization was done by a combination of people including MRI technologists, referring physicians, radiology clerical staff, radiology fellows and departmental managers. More than one radiologist was involved in prioritization in 72/75 (96%) of centres. In 24/72 (33%) of centres, subspecialty radiologists prioritized only requests for studies of the body part applicable to their area of expertise. Facilities triaged MRI requests into varying numbers of urgency categories, ranging from 1 to 6; 65% (49/75) of centres defined four categories. No centres reported the existence of a formal quality assurance mechanism for monitoring the triage process or ensuring that the prioritization occurred on a consistent basis.
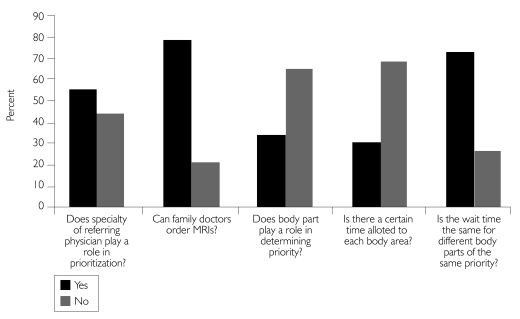
Several factors influenced triage decisions. All centres that triaged requests (75/75) identified inpatient status as probably or definitely playing a role in triage decisions. Other factors reported to influence prioritization included the results of prior imaging (51/75, 68%), the body part being imaged (27/75, 36%) and specialty of the referring physician (44/75, 59%). It is notable that 17/79 sites (22%) did not allow family doctors or general practitioners to order MRI scans, and an additional 11/79 sites (14%) allowed non-specialists to order only limited types of MRI scans (Figure 1).
FIGURE 1.
Factors affecting prioritization
Wait list length
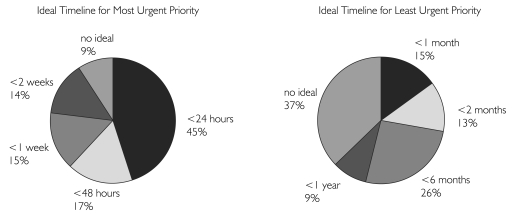
Ninety-seven per cent (76/78) of respondents stated that they had a list of patients awaiting MRI examinations. The two hospitals without waiting lists were both specialized cancer centres with limited referral bases. All centres knew the wait times for their most urgent prioritization category. Five per cent (4/78) of centres did not have documented target timelines for the completion of requests in any prioritization category, and 35% (26/74) did not have target timelines for elective or routine prioritization categories. In several centres, the timelines were considered only as a guide rather than a firm target. Those centres with documented timelines varied considerably in terms of target time for each category of priority (Figure 2). The target timeline for the highest-priority study varied from “immediately” to “within two weeks”. The target timeline for low-priority scans varied from two weeks to a year. Most centres also had a category for routine follow-up (e.g., yearly studies of a known lesion).
FIGURE 2.
Target timelines for scans prioritized as urgent and those prioritized as elective
When measured by the median number of days to scan or by the total numbers of patients waiting for scans, wait list size varied substantially. The median number of patients on the wait list was 1,000 (IQR: 444–1992). Wait times for the most urgent priority studies varied from less than 24 hours to more than one month. The wait times for the most elective category varied from 28 days to three years, with one centre stating that they were simply unable to scan cases prioritized as elective.
The ability to meet target wait times varied markedly. Despite being able to choose their own target wait times, 12/74 (16%) of centres did not meet their target wait times for any priority category, even the most urgent scans. Forty-five per cent of centres responded that they met target times only for some prioritization categories. Only 39% of centres reported meeting their wait time targets for all categories.
Strategies for dealing with wait lists were numerous and varied, making it difficult to characterize the different approaches quantitatively. The single most common response to excessive wait times consisted of attempting to increase the number of hours that an MRI scanner was utilized (64% of centres). The second most common strategy was to increase capacity by attempting to purchase another MRI scanner or to upgrade the current scanner to a faster model (20% of centres). Twelve centres (15%) said that they tried to hire more MRI technologists, a strategy that was limited by lack of funds and, in some cases, lack of qualified personnel. Eleven centres (14%) said they tried various means of increasing efficiency in order to scan more patients without having to increase total hours of operation. Finally, seven centres (9%) said that they contracted out MRI requests to private facilities during periods of excessively long wait lists.
Discussion
Our results document that most MRI facilities in Canada have a substantial wait list problem, with some centres reporting wait times of up to one month for urgent scans and up to several years for non-urgent scans. Despite the magnitude of these wait times and recognition of the problem by staff at the facilities, strategies used to manage wait lists and reduce wait times are diverse, uncoordinated and, judging by the number of patients on the wait lists, largely ineffective. Most facilities employ a categorization scheme for triaging MRI requests, but this is not applied in a rigorous manner. Few sites have documented criteria to guide the triaging decisions. No site had a method of quality assurance to determine whether or not the prioritization was being performed consistently. Thus, it is entirely possible that patients with the same medical indication for an MRI examination, at the same centre, could be placed in different prioritization categories, with very different wait times.
A large number of facilities lack documented target timelines for completion of MRIs in all prioritization categories. Of those with documented targets, there was a wide range of acceptable wait times within each category (e.g., the most urgent category varied from “scan immediately” to “scan within two weeks”). This inconsistency in defining prioritization categories and the considerable variation in the number of categories likely leads to significant inconsistencies in access to MRI from site to site even within a given province.
Facilities varied in their responses to long wait lists, but they generally consisted of attempts to increase capacity. Many centres reported running scanners for extended hours, hiring more technicians or purchasing more scanners, and some acknowledged contracting out to private facilities. Only 3% of centres routinely operated their MRI scanners 24 hours a day, seven days a week. This finding indicates that there is machine capacity to do more scans. This potential machine capacity was also found in another recent study (Ariste and Fortin 2007). Some centres stated that they tried to improve efficiency (i.e., increase the number of scans without increasing resources), but little information was provided in this area. Almost no effort was made to control demand (e.g., by identifying inappropriate requests for MRI scans). Some centres did not let family physicians order scans, though the justification for this practice (e.g., as a surrogate for appropriateness) was not provided. Placement of inappropriate requests in the lowest-priority category may also control demand to some extent, as one centre reported that staff were unable to scan cases in this category.
Development of effective prioritization guidelines for MRIs may be a challenging task, as was found by the Western Canada Waitlist Project (WCWL) (Hadorn et al. 2002) and others (Kahn et al. 1997). The WCWL used a panel of 14 clinicians and health administrators to produce comprehensive prioritization guidelines for MRI (Hadorn et al. 2002), but evaluation of the resulting tool showed poor inter-rater agreement. While not an easy task, developing a system for generating reproducible triage decisions nevertheless represents an important goal for the healthcare system. Measurement of wait times is routinely stratified by level of urgency, but these measurements have little meaning if priority judgments are inconsistent within and across institutions. The implementation of specific provincial prioritization guidelines with an audit process would help ensure consistency of prioritization among sites. Consistency could be further enhanced with a single point of referral, with all prioritization for a province or region performed at a single centre by a small number of people.
It is likely that a proportion of MRI studies are being ordered inappropriately. This has been a finding in studies of other healthcare interventions, including carotid endarterectomy (Kennedy et al. 2004) and gastrointestinal endoscopy (Kahn et al. 1988; Seematter-Bagnoud et al. 1999). We do not know the extent of the inappropriate overuse of MRI or whether overuse correlates with regional wait lists. It is also possible that inappropriate underuse may be greater than inappropriate overuse. A process to ensure the appropriate use of MRI, through the application of guidelines or other forms of decision support, could be used not only to discourage improper ordering but also to help solve the problems we have identified with the triage process.
There are several limitations to our study. The response rate to our questionnaire was 65%. We obtained a good representation of centres from all provinces as well as a good cross-section of types of hospitals. It is unlikely that a higher response rate would substantially alter the overall results. The questionnaire was discussed with a single administrator at each site; this procedure may have led to some bias in interpretation of the subjective questions. Some sites lacked adequate records to respond to some questions. Despite these limitations, our results have implications for those interested in measuring and reducing the problem of wait times for MRI in Canada. First, our results highlight the importance of standard prioritization schemes, consistent definitions of categories within these schemes and uniform guidelines for acceptable wait times for each level of priority. Additionally, classification schemes for prioritizing MRI requests should be based upon explicit, validated criteria that are applied in a consistent manner.
Conclusions
Magnetic resonance imaging remains a developing technology and indications for its use continue to grow, especially in the areas of abdominal, pelvic, cardiac and breast imaging. Many disease processes currently imaged by computerized tomography will in the future be primarily imaged by MRI because of concern over the use of ionizing radiation. The Institute of Clinical Evaluative Sciences, using administrative data, found a fivefold increase in the frequency of MRI scans in the 1990s and a 50% increase from 1999 to 2001 (Iron et al. 2003). It is likely that the demand for MRI scans will continue to grow rapidly. Given the constraints on our health budgets, access to MRI scanning may be even more limited in the future. Thus, it is critical to prioritize MRI requests effectively, to ensure that those most in need will benefit.
Improvement in wait list management is critical to reducing wait times to improve access, fairness and quality in the provision of MRI services in Canada. This study has shown several deficiencies in the current system and should help health system decision-makers and managers improve the provision of this important service.
Acknowledgements
This study was supported by an operating research grant from the Canadian Institutes of Health Research. Dr. Forster is a Career Scientist with the Ontario Ministry of Health and Long-Term Care. Dr. Shojania holds a Canada Research Chair in Patient Safety and Quality Improvement.
Contributor Information
Derek J. Emery, Associate Professor, Department of Radiology and Diagnostic Imaging, University of Alberta, Edmonton, AB.
Alan J. Forster, Associate Professor, Department of Medicine, University of Ottawa; Scientist, Ottawa Health Research Institute, Ottawa, ON.
Kaveh G. Shojania, Associate Professor, Department of Medicine, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, ON.
Stephanie Magnan, Medical Student, University of Alberta, Edmonton, AB.
Michelle Tubman, Research Project Coordinator, Department of Radiology and Diagnostic Imaging, University of Alberta, Edmonton, AB.
Thomas E. Feasby, Professor, Department of Clinical Neurosciences, University of Calgary, Calgary, AB.
References
- American College of Radiology (ACR) ACR Appropriateness Criteria 2000. Radiology. 2000;215(Suppl.):1–1511. [PubMed] [Google Scholar]
- Ariste R., Fortin G. Could MRI and CT Scanners Be Operated More Intensively in Canada? Healthcare Policy. 2007;3(1):1–8. [PMC free article] [PubMed] [Google Scholar]
- Canadian Association of Radiologists. Diagnostic Imaging Referral Guidelines: A Guide for Physicians. Ottawa: Author; 2005. [Google Scholar]
- Hadorn D.C. Steering Committee of the Western Canada Waiting List Project. Developing Priority Criteria for Magnetic Resonance Imaging: Results from the Western Canada Waiting List Project. Canadian Association of Radiologists Journal. 2002;53(4):210–18. [PubMed] [Google Scholar]
- Iron K., Przybysz R., Laupacis A. Access to MRI in Ontario: Addressing the Information Gap. Toronto: Institute for Clinical Evaluative Sciences; 2003. [Google Scholar]
- Kahn C.E., Jr, Michalski T.A., Erickson S.J., Foley W.E., Krasnow A.Z., Lofgren R.P., et al. Appropriateness of Imaging Procedure Requests: Do Radiologists Agree? American Journal of Roentgenology. 1997;169(1):11–14. doi: 10.2214/ajr.169.1.9207492. [DOI] [PubMed] [Google Scholar]
- Kahn K.L., Kosecoff J., Chassin M.R., Solomon D.H., Brook R.H. The Use and Misuse of Upper Gastrointestinal Endoscopy. Annals of Internal Medicine. 1988;109(8):664–70. doi: 10.7326/0003-4819-109-8-664. [DOI] [PubMed] [Google Scholar]
- Kennedy J., Quan H., Ghali W.A., Feasby T.E. Variations in Rates of Appropriate and Inappropriate Carotid Endarterectomy for Stroke Prevention in 4 Canadian Provinces. Canadian Medical Association Journal. 2004;171(5):455–59. doi: 10.1503/cmaj.1040170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor C.D., Szalai J.P., Katic M. Benchmarking the Vital Risk of Waiting for Coronary Artery Bypass Surgery in Ontario. Canadian Medical Association Journal. 2000;162(6):775–79. [PMC free article] [PubMed] [Google Scholar]
- Sanmartin C., Shortt S.E., Barer M.L., Sheps S., Lewis S., McDonald P.W. Waiting for Medical Services in Canada: Lots of Heat, But Little Light. Canadian Medical Association Journal. 2000;162(9):1305–10. [PMC free article] [PubMed] [Google Scholar]
- Seematter-Bagnoud L., Vader J.P., Wietlisbach V., Froehlich F., Gonvers J.J., Burnand B. Overuse and Underuse of Diagnostic Upper Gastrointestinal Endoscopy in Various Clinical Settings. International Journal for Quality in Health Care. 1999;11(4):301–8. doi: 10.1093/intqhc/11.4.301. [DOI] [PubMed] [Google Scholar]
- Stein L.A. Making the Best Use of Radiological Resources in Canada. Healthcare Papers. 2005;6(1):18–23. doi: 10.12927/hcpap..17719. [DOI] [PubMed] [Google Scholar]