Abstract
Background:
Little is known about inter-facility patient transfers in populations. In 2003, detailed information about inter-facility patient transfers began to be systematically collected in Ontario.
Methodology:
The authors undertook a descriptive examination of inter-facility patient transfers using a newly created population-based information system.
Results:
Approximately 1,000 inter-facility patient transfers occur in Ontario each day, and every day and a half, the total distance travelled for these transfers equals the distance around the earth's circumference. The annual cost for patient transfers is approximately $283 million. Most common were routine and non-urgent inter-facility patient transfers. Eighty-five thousand patients (24.3% of transferred patients) were transported between healthcare facilities for dialysis appointments, appointments with physicians and return trips home. Patients with circulatory conditions were the most commonly transferred diagnostic group. Although 70% of all transfers were within 25 kilometres, some were for longer distances: for example, those involving pregnant women and newborn babies required travelling a median distance of 40.3 kilometres for continued care. Cardiac patients (54,000 patient transfers per year) travelled a median of 24.2 kilometres to reach a catheterization lab for treatment and further investigation. There was considerable lateral movement between academic health sciences centres (AHSCs). Over 16,000 patients per year (4.7% of all transfers) were transferred from one AHSC to another, predominantly for cardiac care.
Discussion:
Patients in Ontario are often transferred between healthcare facilities. Most transfers are for routine, non–life-threatening reasons, using the Emergency Medical Services (EMS) system. This practice diverts resources from more emergent requests. Although patient transportation is a necessary part of any healthcare system, the results of this study highlight the current demands on a system that was not intended for the volume of inter-facility patient transfers it is supporting. These results call into question the use of sophisticated, highly trained, expensive patient transfer resources to provide routine medical services in Ontario.
Abstract
Contexte :
On connaît peu de choses au sujet du transfert de patients entre établissements dans une population donnée. En 2003, l'Ontario commençait à recueillir systématiquement une information détaillée à propos de tels transferts.
Méthodologie :
À l'aide d'un nouveau système d'information axé sur les populations, les auteurs ont mené un examen descriptif des transferts de patients entre établissements.
Résultats :
Environ 1000 transferts de patients entre établissements ont lieu chaque jour en Ontario. À chaque 36 heures, la distance totale parcourue au cours de ces transferts est égale à la circonférence de la terre. Le coût annuel pour le transfert de patients est d'environ 283 millions de dollars. Les transferts de routine, ou non urgents, sont les plus fréquents. Quatre-vingt-cinq mille patients (24,3 %) sont transportés entre des établissements de santé pour des dialyses, des rendez-vous avec le médecin ou le retour au foyer. Les patients qui ont des problèmes du système circulatoire constituent le groupe où les transferts sont les plus fréquents. Bien que 70 % de tous les transferts s'effectuent sur une distance de 25 kilomètres ou moins, certains d'entre eux – notamment pour les femmes enceintes et les nouveaux-nés – se font sur une distance médiane de 40,3 kilomètres, pour la continuité des soins. Les patients qui ont un problème cardiaque (54 000 transferts par année) parcourent une distance médiane de 24,2 kilomètres pour se rendre dans un centre de cathétérisation afin d'y recevoir un traitement ou d'y passer un examen. Il y a un mouvement latéral considérable entre les centres universitaires des sciences de la santé (CUSS). Plus de 16 000 patients par année (4,7 % de tous les transferts) sont transférés d'un CUSS à l'autre pour recevoir des soins, principalement pour des problèmes cardiaques.
Commentaire :
En Ontario, les patients sont souvent transférés entre les établissements de santé. La plupart de ces transferts ont un caractère routinier, où la vie des patients n'est pas en jeu, et font appel aux services médicaux d'urgence. Cette pratique détourne les ressources au détriment de situations plus urgentes. Bien que le transport de patients soit nécessaire dans tout système de santé, les résultats de cette étude mettent en relief la pression actuelle sur un système qui n'a pas été conçu pour un tel volume de transferts de patients entre établissements. Les résultats remettent en question l'utilisation d'une ressources perfectionnée et onéreuse, où le personnel est solidement formé, afin d'offrir aux patients ontariens des services médicaux de routine.
Beginning in 1996 with the Ontario Health Services Restructuring Commission, the landscape of Ontario's healthcare began to change. As a result of restructuring and regionalization of healthcare services, Ontario patients are often moved through the healthcare system from facility to facility for care. Patients can no longer expect to have all their healthcare needs met at a single facility. Emergency medical services (EMS) in Ontario are provincially mandated and regulated but locally administered, most often by municipal governments.
The structure of emergency services varies greatly from province to province. For example, pre-hospital emergency services in British Columbia are wholly administered by the province. Alberta is centralizing its EMS structure to transfer responsibility to Alberta Health Services by April 2009. At the other end of the spectrum, emergency services in Nova Scotia are regulated by the Department of Health but managed by a private company, Emergency Medical Care. The diversity of governance structures and administration of EMS across Canada makes sharing data and drawing comparisons difficult.
Ambulance services and other patient transportation are non-insured services under the Canada Health Act, and coverage is left up to the discretion of the provinces. In 2001, when Ontario municipalities assumed responsibility for ambulance services, they also accepted responsibility to provide 50% of the funding necessary to run them jointly with the Ministry of Health and Long-Term Care. Since then, it is widely acknowledged (Armstrong 2004, D'Angelo 2004) that costs have not been equally balanced, as municipalities now cover more than 50% of ambulance costs. The majority of patient transportation in Ontario is completed through the public system; however, some inter-facility patient transfers are completed through contracts with private companies as a way for some hospitals to trim their costs and improve efficiency.
More often than not, transferred patients are transported between healthcare facilities by fully equipped ambulances that are staffed by highly trained and well-paid paramedics – the same system used for emergency 911 calls. Inter-facility patient transfers can be emergent or routine in nature.
In 2003, in reaction to outbreaks of severe acute respiratory syndrome (SARS) in Toronto, the Provincial Transfer Authorization Centre (PTAC) was established to authorize all inter-facility patient transfers in the province of Ontario (MacDonald et al. 2004). Today, a patient transfer between two healthcare facilities may not proceed until authorization has been received from PTAC. All data pertaining to patient transfers are stored in the PTAC database.
The objective of this study was to provide a cross-sectional view of patient transfers in Ontario. Prior to this study, total numbers of patient transfers were known, but detailed descriptive data about these transfers were not available. An examination of demographics, patterns and volume of patient movement can assist policy makers who face resource allocation decisions and must plan for future needs and growth. To the best of our knowledge, ours is the first population-based analysis of inter-facility patient transfers in a Canadian province.
Methodology
As can be expected with any new data set, the PTAC database was not without its own challenges. First, the data set had to be validated against a “gold standard.” A validation study (Robinson et al. 2006) determined that the PTAC data had a high level of validity (i.e., sensitivity values for data variables ranged from 0.87 to 1.0). Second, the data set required additional coding and recoding of variables. This process is discussed in subsequent sections.
Study population
The study population was a random sample of 5,000 inter-facility land transfers in Ontario, Canada drawn from one year's worth of data (349,342 transfers). Inter-facility patient transfers that were completed by air were excluded.
Data
The Provincial Transfer Authorization Centre is operated by Ornge (formerly Ontario Air Ambulance), which has stewardship over all data collected through PTAC. Data were abstracted from the PTAC database for a one-year period from June 1, 2004 to May 31, 2005. These data were collected during the PTAC authorization process for inter-facility patient transfers.
There are several steps in the authorization process. First, sending facilities are required to complete a patient transfer authorization form. Once the form has been submitted to PTAC, the request is processed using a decision algorithm, primarily screening for infectious disease. If the transfer request meets the predetermined criteria, it is approved and assigned a transfer authorization number. Authorization is normally obtained quickly. If the transfer is non-urgent, authorization can be requested and granted in advance to avoid delays. When a request does not meet the criteria, a physician reviews it and often contacts the sending facility to obtain more information. Patient transfer requests are processed consecutively except for emergency transfers, which are processed immediately.
Once a transfer request is approved, the sending facility contacts its regional Central Ambulance Communication Centre (CACC) or local ambulance service provider to proceed with the transfer.
Inter-facility patient transfers have three levels of priority: emergent, urgent and non-urgent. An emergent transfer involves a life-threatening situation, is time-sensitive and receives priority by PTAC. (See Appendix A for a full description at http://www.longwoods.com/product.php?productid=20478.) An urgent transfer is not as serious as an emergent transfer, but may still be time-sensitive and should be completed within a specific timeframe. A non-urgent transfer is considered routine and does not involve an immediate threat to life or limb, or care that is time-sensitive.
Research ethics approval for this study was granted by the University of Toronto and Sunnybrook and Women's Health Sciences Centre Research Ethics Boards.
Analysis
Because of the need for recoding, a random sample of 5,000 transfers was selected using the random sampling function in the statistical software program SPSS (SPSS Inc. n.d.). A sample size of 4,113 provides a 99% confidence interval of +/−2% on proportions. The sample size was rounded up to 5,000.
Several variables had to be either recoded or created in order to analyze the PTAC data set properly. From a free text variable, two variables were created to describe the reason for the inter-facility transfer, one of the most important aspects of the analysis. The first was the diagnosis based on an International Classification of Disease (ICD) version 10 code. The second was a modified version of the Canadian Classification of Health Interventions (CCHI) and was used to describe the procedure or issue to be addressed at the receiving facility. The CCHI was modified with the addition of several variables specific to inter-facility patient transfers. A validation process concluded that the coding sensitivity (true positive result) was 0.96.
Hospitals in Ontario are classified by the Ministry of Health and Long-Term Care according to their size and function. A slightly modified version of this classification system was used in the study.
Distances between facilities were calculated by converting postal codes first into geographical units of latitude and longitude and then using a specific equation that calculates distances between two points.
A detailed description of the coding and recoding process for the reason-for-transfer variables, the facility classification variables and the geographical coding variables appears in Appendix B (http://www.longwoods.com/product.php?productid=20478). The equation used to calculate patient transfer distances appears in Appendix C (http://www.longwoods.com/product.php?productid=20478).
Once all the data were coded, cleaned and checked for accuracy, they were imported into SPSS (v. 15) for analysis. A series of descriptive analyses were performed including calculation of means, medians, t-tests, chi-squares and Mann–Whitney U tests to examine differences between groups and also linear and multiple regressions to examine associations among data variables.
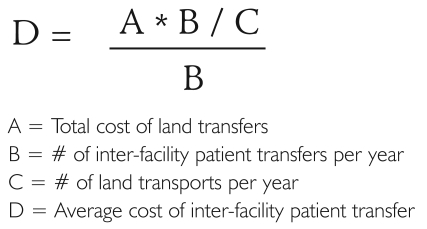
Using costing data publicly available through the Ministry of Health and Long-Term Care and the Ontario Auditor General (2005) and a simple proportions equation (Figure 1), we estimated the average direct cost of a one-way inter-facility patient transfer. This average inter-facility patient transfer cost was applied to transfer numbers to provide financial context to the analyses. Detailed costing information will be presented in a subsequent paper.
FIGURE 1.
Equation for estimating the average cost of inter-facility patient transfers, 2005
Results
On a typical day there are over 1,000 inter-facility patient transfers within the province of Ontario, for a total of almost 400,000 transfers annually. Ontario ambulances providing these transfers travel a distance equal to the circumference of the earth every day and a half – that is, approximately 10.5 million kilometres.
The majority of all inter-facility patient transfers are non-urgent (80.4%; see Table 1) and occur between Monday and Thursday. The main reasons for non-urgent transfers are physician's appointments, dialysis and returning to home facility or residence (81,000 transfers per year; see Table 2). The majority of inter-facility patient transfers concern the circulatory, musculoskeletal and connective tissue, or genitourinary systems.
TABLE 1.
General descriptive statistics of inter-facility transfers by transfer priority
| Transfer priority (% of all transfers) | ||||
|---|---|---|---|---|
| Emergent | Urgent | Non-urgent | All transfers | |
| All transfers by priority | 10.4 | 9.2 | 80.4 | 100.0 |
| Sex | ||||
| Female | 47.3 | 50.9 | 56.8 | 55.6 |
| Male | 52.7 | 49.1 | 43.7 | 44.4 |
| Day of week | ||||
| Monday | 15.2 | 14.5 | 18.8 | 18.0 |
| Tuesday | 14.1 | 19.7 | 18.8 | 18.5 |
| Wednesday | 16.0 | 15.2 | 17.5 | 17.1 |
| Thursday | 11.9 | 14.6 | 18.2 | 17.2 |
| Friday | 14.9 | 16.6 | 10.4 | 11.4 |
| Saturday | 14.3 | 10.3 | 5.2 | 6.6 |
| Sunday | 13.7 | 9.0 | 11.1 | 11.1 |
TABLE 2.
Top reasons for inter-facility patient transfers, classified by ICD 10 and CCHI, and their estimated cost to the Ontario healthcare system
| ICD 10 chapter | Percentage of all transfers (%) | Number of transfers per year | Median distance travelled per transfer (km) | Median distance inter-quartile range (km) | Estimated cost per year (in millions) | |
|---|---|---|---|---|---|---|
| 1 | Circulatory | 15.5 | 54,162 | 17.0 | 6.8–50.0 | $38.0 |
| 2 | Musculoskeletal and connective tissue | 12.7 | 44,378 | 10.5 | 5.4–39.4 | $31.0 |
| 3 | Genitourinary | 12.1 | 42,281 | 9.2 | 3.3–25.5 | $29.8 |
| 4 | Digestive | 5.3 | 18,520 | 10.5 | 3.7–35.5 | $13.0 |
| 5 | Neoplasms | 5.0 | 17,472 | 14.0 | 6.3–63.1 | $12.3 |
| 6 | Mental and behavioural disorders | 4.9 | 17,122 | 10.5 | 3.7–26.9 | $12.1 |
| 7 | Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 4.6 | 16,074 | 10.3 | 3.4–27.1 | $11.3 |
| 8 | Respiratory | 4.6 | 16,074 | 7.9 | 2.8–23.8 | $11.3 |
| 9 | Nervous | 4.3 | 15,026 | 10.5 | 3.7–40.7 | $10.6 |
| 10 | Injury, poisoning and certain other consequences of external causes | 2.7 | 9,435 | 11.7 | 4.8–51.0 | $6.6 |
| Canadian Classification of Health Interventions (CCHI) | Percentage of all transfers (%) | Number of transfers per year | Median distance travelled per transfer (km) | Median distance inter-quartile range (km) | Estimated cost per year (in millions) | |
|---|---|---|---|---|---|---|
| 1 | Pre-scheduled physician's appointment | 8.9 | 31,099 | 10.5 | 5.3–23.2 | $21.9 |
| 2 | Dialysis appointment | 7.7 | 26,906 | 9.5 | 3.9–25.8 | $18.9 |
| 3 | Physical/physiological therapeutic intervention | 6.9 | 24,111 | 10.5 | 5.4–42.7 | $17.0 |
| 4 | Admission | 6.7 | 23,412 | 10.5 | 5.0–40.7 | $16.5 |
| 5 | Diagnostic imaging intervention | 6.2 | 21,665 | 10.5 | 3.0–41.7 | $15.3 |
| 6 | Returning to sending facility/home | 5.9 | 20,617 | 8.3 | 3.6–18.3 | $14.5 |
| 7 | Catheterization lab | 3.2 | 11,182 | 24.2 | 8.2–70.9 | $7.9 |
| 8 | Consultation | 1.7 | 5,940 | 10.5 | 5.5–36.5 | $4.2 |
The median age for inter-facility transferred patients is 75 years. There are significant differences in median age by priority status. For example, emergent inter-facility transfer patients are considerably younger, with an overall median age of 56 years. Almost 70% of transferred patients are over the age of 65, and less than 5% of transfers are of children under the age of 18.
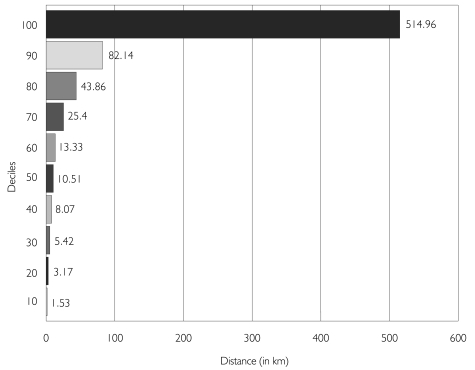
Within an urban setting, the majority of inter-facility patient transfers are over short distances. The median distance travelled is 10.5 kilometres, with an inter-quartile range of 4.3 to 33.3 kilometres (kurtosis 20.0, standard error 0.07). Of all non-urgent patients who are transferred for dialysis, physician's appointments and returning to home facilities or residences, 77.7% of them travel within a radius of 25 kilometres. Among all transferred patients, 20% travel over 44.0 kilometres to receive care (Figure 2).
FIGURE 2.
Overall distance travelled presented by decile (in km)
Pregnant women, women transferred for childbirth and neonates travel a median distance of 40.3 kilometres; over half (52.9%) of these transfers are emergent or urgent.
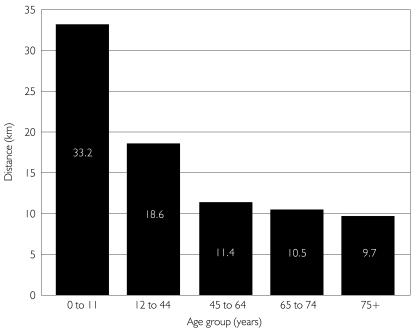
There are significant differences in travel distances between emergency, urgent and non-urgent transfers (MWU, p < .0005). Non-urgent and urgent transfers travel the same median distance as the overall average (10.5 kilometres), but emergent transfers travel a median distance of 33.8 kilometres. Differences also exist between age groups. Young children (0–11 years) are transferred a median distance that is 22.6 kilometres longer compared to older adults (65–74 years) (MWU, p<0.0005)(Figure 3).
FIGURE 3.
Median inter-facility patient transfer distance travelled by age group
Group A, or academic health sciences centres (AHSCs), are large, tertiary care teaching hospitals. Group B hospitals are large non-teaching hospitals with no fewer than 100 beds. Group C hospitals are small non-teaching hospitals with fewer than 100 beds. Transfers among Group A, B and C hospitals (see Appendix B) represent 39.8% of all transfers. Among these, there is significant lateral movement of patients. Approximately 16,454 (4.7%) patient transfers occur between one AHSC and another, and approximately 32,207 (9.2%) patient transfers occur between Group B hospitals (Table 3). Transfers laterally between AHSCs are primarily for cardiac-related services, followed by musculoskeletal and digestive services. Transfers laterally between Group B hospitals are also primarily for cardiac-related reasons, followed by genitourinary and musculoskeletal services. Almost all emergent and urgent patient transfers are to an AHSC, Group B or Group C hospital.
TABLE 3.
Movement between facilities by hospital classification
| Most travelled route* | Percentage of transfers per year | Actual number of transfers per year |
|---|---|---|
| Group B to LTC | 12.1% | 42,631 |
| LTC to Group B | 9.8% | 34,244 |
| Group B to Group B | 9.2% | 32,148 |
| Group C to Group B | 7.8% | 27,256 |
| Group B to AHSC | 7.5% | 26,207 |
| LTC to AHSC | 4.8% | 16,773 |
| AHSC to AHSC | 4.7% | 16,423 |
See Appendix B for a description of facilities.
The total direct cost of providing inter-facility patient transfers in Ontario for one year was $242.88 million in 2005. The average cost for an individual, one-way inter-facility patient transfer was $704. An approximation of cost totals by diagnostic category, based on applying this value to transfer numbers, is presented in the last column of Table 2.
Discussion
This study represents the first population-based analysis of inter-facility patient transfers in Ontario. Regionalized healthcare in Ontario has necessitated the movement of patients from facility to facility and for many patients in Ontario this has become the new pattern of care. From 2005 to 2008, inter-facility patient transfers increased 40%, from an average of 1,000 transfers per day to 1,375 (PTAC data).
A patient transportation system is a necessary part of any healthcare system, especially a highly regionalized one like Ontario's. Regionalization of certain services has been found to improve outcomes (Halm et al. 2002), namely, mortality and morbidity, while maintaining a certain level of quality and efficiency in the healthcare system. An unanticipated effect, however, at least in Ontario, is the amount of patient movement required to maintain continuity of care, and the consequent impact on emergency services when a high volume of routine transport is assumed by the ambulance system.
The results of this study indicate that the majority of patient transfers are for non-urgent reasons, and for short distances. Planning for specialized services is often done with major interventions in mind (e.g., definitive surgery), but without full consideration of the impact of service centralization on consultations, routine treatments and follow-up care. Transfers for highly specialized care, however, represent only a small proportion of all inter-facility patient transfers in Ontario; the majority of patient transfers are routine. Therefore, other options should be explored to make the patient transportation system more efficient and accessible. For example, inter-facility patient transfer trends for dialysis appointments may indicate the need for additional dialysis facilities.
Some municipalities have reported an inability to cope with the current demand for ambulance use because of inter-facility patient transfers (Auditor General of Ontario 2005). As a result, their provincially mandated response times for 911 ambulance calls have suffered, and patient transfers are often delayed (Auditor General of Ontario 2005). According to the Association of Municipal Emergency Services of Ontario, increasing inter-facility patient transfer volume “results in hundreds of hours of lost availability to the EMS providers, which has a very negative impact on emergency response time. Delays currently experienced in respect to low-priority inter-facility patient transfers has an extremely negative impact on the healthcare system as a whole” (Armstrong 2004).
Having a patient transportation system dedicated, at least in part, to the transfer of non-urgent, routine patients makes intrinsic sense. Yet, since the offloading of EMS to municipalities in 2001, the Ontario Ministry of Health and Long-Term Care appears to have given patient transportation low priority. Patient transfer volumes have increased without a corresponding increase in government funding to meet the 50/50 funding formula. This shortfall leaves municipalities to cover upwards of 65% of EMS costs (D'Angelo 2004, Armstrong 2004).
At the urging of many interested groups, the ministry commissioned a consulting firm, IBI Group, to examine the inter-facility patient transfer issue in Ontario. The findings confirmed the concerns and possible solutions raised by municipalities, EMS groups and others across the province; however, the ministry refused to make the results of the study public. The findings were made known through a Freedom of Information request.
An important finding from the current study was the amount of lateral movement between AHSCs and between Group B facilities. Such lateral transfers may be symptomatic of hospital crowding, lack of available beds, staffing shortages at healthcare facilities and a lack of comprehensive services, even at AHSCs.
Although this study did not specifically examine wait times for inter-facility patient transfers, these are well documented elsewhere (Auditor General of Ontario 2005; Stolte et al. 2006) and have considerable impacts on patient care. The Ontario Auditor General (2005) reported that over 40% of non-urgent inter-facility patient transfers were delayed more than 20 minutes from the scheduled time. Patients can be “in the queue” for an inter-facility transfer but may have to wait a long time because of priority calls or offloading issues from previous transfers. Such delays can cause missed appointments and tardy medication administration and treatment (Stolte et al. 2006), as well as higher stress levels due to waiting, prolonged length of stay in acute facilities and lack of care continuity – all factors that can result in compromised patient care and increased healthcare costs.
Study limitations
Although this study was population-based, a random sample was taken from one year of data, and recoding was completed on this sample. Because variables were recoded, coding errors are possible; but as coding was completed by one researcher (VR) and the process was checked for accuracy, the chance for error was small. Some records (8% of the sample) lacked information about the reason for a transfer, possibly because this information was not available at the time. Even though the analyses used sampled data, drawing the sample from an entire year's data should have minimized seasonal effects.
As well, a small percentage of patient transfers were completed by private patient transportation companies, taxis or family members, and it was not possible to exclude these from the analyses.
Conclusions
This population-based study of inter-facility patient transportation for an entire province highlights issues that may exist in other parts of Canada and around the world.
Although there may be a public perception that ambulances are used to transport patients solely during emergencies to healthcare facilities, the results of this study challenge this perception.
In Ontario, the large volume of inter-facility patent transfers is overwhelming many EMS systems throughout the province. One in every three patients admitted to hospital in Ontario can expect to be transferred for continued care (Jaakkimainen et al. 2006). The typical inter-facility patient transfer in Ontario involves a non-urgent appointment with a cardiologist or a dialysis treatment and covers 10.5 kilometres. Round trip transfers costs average $1,408. The use of emergency medical services to transfer non-urgent inter-facility patients may represent an inappropriate use of resources.
The results of this study suggest a need for change in the way patients are transferred throughout the province. Policy makers now have more detailed information to inform decisions about how to implement that change.
Future studies involving PTAC data might include more detailed trend analyses of transfers and patient outcomes analyses, including morbidity and mortality, through data linkages with hospitals and other databases.
Acknowledgements
Victoria Robinson is supported by a CIHR Doctoral Research Award and financial assistance from Ornge, formally the Ontario Air Ambulance Services Corporation. This research was also supported by funding from Ornge. Doug Manuel holds a CIHR/PHAC Chair in Applied Public Health Sciences.
Appendices
Appendix A: Priority Status Descriptions of Inter-Facility Patient Transfers
Emergent Transfer
The medically necessary criteria for an emergency transfer are defined by the Ontario Ministry of Health and Long-Term Care as:
One or more body systems are abnormal and rapidly deteriorating in association with an acute illness or injury. Intense monitoring and medical interventions are required to correct and stabilize the patient's condition. Condition requires immediate specialty care for any one of the following that cannot be provided in sending health care facility:
Abnormal or deteriorating neurological status
Life-threatening emergencies
Significant or life-threatening traumatic injuries
Threat to maternal or fetal life
Airway compromise or severe respiratory distress
Acute paediatric illness requiring specialized care
Ontario Ministry of Health and Long Term Care
Urgent Transfer
An urgent transfer is not as serious in nature as an emergent transfer but may still be time-sensitive and should be completed within a specific timeframe.
Non-Urgent Transfer
A non-urgent transfer is considered routine, is not an immediate threat to life or limb and does not involve time-sensitive care.
Appendix B: Description of Coding and Recoding Process for Reason-for-Transfer Variables, Facility Classification Variables and the Geographical Coding Variables
Several variables from the PTAC database had to be either created or recoded in order to permit a proper analysis of the data set.
Reason-for-Transfer Variables
From a free text variable, two variables were created to describe the reason for the inter-facility patient transfer. The first is the diagnosis based on an International Classification of Disease (ICD) version 10 code. The second is a modified version of the Canadian Classification of Health Interventions (CCHI) and was used to describe the procedure or issue to be addressed at the receiving facility. The CCHI was modified with the addition of several variables specific to inter-facility patient transfers. For example, additional values included dialysis appointment, scheduled doctor's appointment, admission to facility, cardiac catheterization or return to home facility. Transfers were coded as “multiple,” when there were multiple body systems highlighted in the free text and determination of the system most responsible for the transfer was not possible.
One researcher (VR) conducted all coding. Validation of a sample of 100 from the 5,000 was completed to determine the accuracy of the initial coding done. The other members of the research team coded this sample independently. These codes were then compared to the initial coding. Sensitivity (true positive result) was initially calculated to be 0.76. The majority of discrepancies were identical and systemic. These errors were corrected through discussions among the research team. Specific examples of inter-facility patient transfers were then coded by the team; any outstanding disagreements were discussed, and a decision was made about how they would be coded. A coding manual was also prepared by VR and reviewed by the team to standardize coding. Examples of transfers that occurred in the database were put in the coding manual for easy reference during the coding process. When the discrepancies and system errors were corrected, the sensitivity for the coding was 0.96. Once the coding was completed, considerable time was taken reviewing and checking the coding for errors. As a result, the overall error rate was expected to be very small.
Health Facility Classification Variable
Hospitals in Ontario are classified by the Ministry of Health and Long-Term Care according to their size and function. The largest of the hospitals are academic health sciences centres (AHSCs), or Group A hospitals. AHSCs are general hospitals and teaching sites that are affiliated with universities that have a medical school. The next in size are Group B hospitals, large non-teaching hospitals with no fewer than 100 beds. Small non-teaching hospitals that have fewer than 100 beds are classified as Group C hospitals. Other facilities are classified primarily by their function (e.g., chronic, psychiatric, rehabilitative or long-term care). Table 4 lists facility classifications and their description.
TABLE 4.
Health facility classification
| Facility reclassification | ||
|---|---|---|
| Variable | Facility classification | Description |
| 1 | Group A or AHSC | Tertiary care facility, Academic Health Sciences Centre (teaching) + cancer treatment |
| 2 | Group B | Large non-teaching (no fewer than 100 beds) + cancer treatment |
| 3 | Group C | Small non-teaching (fewer than 100 beds) + ambulatory care + private hospitals |
| 4 | Rehab | Rehab hospitals + special rehab hospitals |
| 5 | Chronic care | Large and small chronic care hospitals + continuing care centres |
| 6 | Psychiatric | Psychiatric hospitals (teaching) + psychiatric hospitals (non-teaching) + psych for youth + mental health outpatient |
| 7 | Long-term care | Long term care + home for the aged |
| 8 | Community services | Community services: assisted living, child and family centre, developmental services, hospice + abortion clinic + drug and alcohol treatment hospitals and clinics + dialysis |
| 9 | Out of province | Out of province (Quebec, Manitoba, US) |
| 10 | Other | Other + private residence + medical clinic |
Geographical Coding Variables
Each healthcare facility was coded according to its geographical latitude and longitude, using the street address and postal code and the website geocoder.ca (http://geocoder.ca). The creators of geocoder.ca state that their program has a mean error of approximately 9 metres.
Distance between facilities was calculated using an approach employed by Ng et al. (1993). Using the same equation, distances between facilities were calculated to determine the distance travelled for each inter-facility patient transfer. (See Appendix C.) Since this was an aerial (straight line) distance, a conversion factor of 1.373487 was calculated using the Google Maps™ driving directions function and was applied to all aerial distances to approximate driving distance between facilities.
A number of sending and receiving facilities were coded as “facility unknown.” Although an extensive list of facilities exists within the PTAC database, some facilities may have been overlooked, or a particular facility may not have been located within the database by the data entry clerk. As a result, an assumption was made that the majority of these facilities were within the median distance (8 kilometres) of all the transfers. Transfers occurring within the same facilities were recorded as 1 kilometre in distance.
Appendix C: Equation Used to Calculate Inter-Facility Patient Transfer Distances Using the Latitude and Longitude of Sending and Receiving Facilities
D = 6,370,997 ∗ arcos[sin(LAT1) ∗ sin(LAT2) + cos(LAT1) ∗ cos(LAT2) ∗ cos(LONG1 − LONG2)]
where
D = distance (in metres)
LAT1 = latitude of point 1 (in radians)
LONG1 = longitude of point 1 (in radians)
LAT2 = latitude of point 2 (in radians)
LONG2 = longitude of point 2 (in radians)
arcos = arc cosine
cos = cosine
sin = sine
and 6,370,997 is the radius of the sphere (in metres)
Footnotes
Appendices are available online at: http://www.longwoods.com/product.php?productid=20478.
Contributor Information
Victoria Robinson, Institute of Medical Science, Faculty of Medicine, University of Toronto, Toronto, ON.
Vivek Goel, President and CEO, Ontario Agency for Health Protection and Promotion; Professor, Dalla Lana School of Public Health, University of Toronto, Toronto, ON.
Russell D. MacDonald, Medical Director, Research Program, Ornge (formerly Ontario Air Ambulance); Assistant Professor, Department of Medicine, University of Toronto, Toronto, ON.
Doug Manuel, Senior Scientist, Ottawa Health Research Institute, University of Ottawa; Associate Professor, Dalla Lana School of Public Health, University of Toronto, Toronto, ON.
References
- Armstrong R. Role of Municipalities.. Patient Transportation Services: Who's Accountable?; Address to the Ontario Hospital Association Conference; Toronto, Ontario. 2004. Jun 18, [Google Scholar]
- Auditor General of Ontario. Auditor General's Report. Chapter 3.02: Ambulance Services – Land. 2005 Retrieved January 19, 2009. < http://www.auditor.on.ca/en/reports_2005_en.htm>.
- D'Angelo C. The Oxford Solution – Non-Emergency Inter-Facility Patient Transfers.. Patient Transportation Services: Who's Accountable?; Address to the Ontario Hospital Association Conference; Toronto, Ontario. 2004. Jun 18, [Google Scholar]
- Halm E., Lee C., Chassin M. Is Volume Related to Outcome in Health Care? A Systematic Review and Methodologic Critique of the Literature. Annals of Internal Medicine. 2002;137:511–20. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- Jaakkimainen L., Upshur R., Klein-Geltink J., Leong A., Maaten S., Schultz S., Wang L. Primary Care in Ontario ICES Atlas. 2006. Nov,
- MacDonald R.D., Farr B., Neill M., Loch J., Sawadsky B., Mazza C., Daya K., Olynyk C., Chad S. An Emergency Medical Services Transfer Authorization Center in Response to the Toronto Severe Acute Respiratory Syndrome Outbreak. Prehospital Emergency Care. 2004;8:223–31. doi: 10.1016/j.prehos.2003.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng E., Wilkins R., Perras A. How Far Is It to the Nearest Hospital? Calculating Distances Using the Statistics Canada Postal Code Conversion File. Statistics Canada, Health Reports. 1993;5(2):179–88. [PubMed] [Google Scholar]
- Ontario Ministry of Health and Long-Term Care. Patient Transfer Authorization Procedure. Retrieved January 19, 2009. < http://www.health.gov.on.ca/english/providers/program/pubhealth/sars/docs/xfer_form_051203.pdf>.
- Robinson V.A., MacDonald R.D., Manuel D., Goel V. Validation of the Provincial Transfer Authorization Centre Database: A Comprehensive Database Containing Records of All Inter-Facility Patient Transfers in the Province of Ontario. BMC Health Services Research. 2006;6(129) doi: 10.1186/1472-6963-6-129. Retrieved January 19, 2009. < http://www.biomedcentral.com/1472-6963/6/129>. [DOI] [PMC free article] [PubMed]
- SPSS Inc. SPSS for Windows Standard Version 15.0. Chicago: Author; n.d. [Google Scholar]
- Stolte E., Iwanow R., Hall C. Capacity-Related Interfacility Patient Transports: Patients Affected, Wait Times Involved and Associated Morbidity. Canadian Journal of Emergency Medicine. 2006;8(4):262–68. doi: 10.1017/s1481803500013816. [DOI] [PubMed] [Google Scholar]