Abstract
There is increasing evidence of the efficacy of dose-dense therapy in the management of platinum-resistant/refractory ovarian cancer. We report our experience of extended weekly carboplatin and paclitaxel in this population group. Twenty patients with platinum-resistant/refractory ovarian cancer received carboplatin AUC 3 and paclitaxel 70 mg m−2 on day 1, 8, 15 q 4 weekly for six planned cycles. Toxicity was assessed using Common Toxicity Criteria. Response was evaluated using radiological and CA125 criteria. Median age was 61 years (range 40–74 years). Median number of prior therapies is three (range 1–8). Response rate was 60% by radiological criteria (RECIST) and 76% by CA125 assessment. Grade 3 toxicities consisted of neutropenia (29% of patients) and anaemia (5%). One patient experienced grade 4 neutropenia. No grade 3/4 thombocytopaenia was reported. Fatigue, nausea and peripheral neuropathy were the most frequent non-hematological side effects. Median progression-free survival was 7.9 months and overall survival was 13.3 months. The dynamics of response to dose-dense therapy were as rapid as with front-line therapy within the same patient. This dose-dense regimen can be extended to at least 18 weekly cycles over 6 months and is well tolerated with high response rates in heavily pre-treated, platinum-resistant ovarian cancer. It forms a highly active and tolerable cytotoxic scaffold to which molecular-targeted therapies can be added in platinum-resistant ovarian cancer.
Keywords: ovarian cancer, resistance, relapse, carboplatin, paclitaxel, weekly
Ovarian cancer is the leading cause of death from gynecologic malignancies in the United Kingdom, and is the fourth most common cause of cancer mortality in women (Piver et al, 1991). Despite relatively high response rates to first-line platinum-based therapies, the majority of patients with epithelial ovarian cancer will experience disease relapse and will require further chemotherapy (Neijt et al, 1991). Several therapeutic options are available and the decision as to which therapy to commence is dependent on the time from last platinum chemotherapy to decision to treat, known as the platinum-free interval (PFI) (Markman et al, 1991; van der Burg et al, 1991). The PFI is a predictor of response not only to second-line treatment with platinum-based chemotherapy but also other active agents including the taxanes, topoisomerase I inhibitors and anthracyclines (Eisenhauer et al, 1994). The probability of response to platinum rechallenge increases with the PFI, from >60% in patients relapsing >12 months since last platinum therapy to below 10% in patients relapsing within 6 months (Markman et al, 1991). This entity of platinum-resistant ovarian cancer, therefore, represents a different clinical scenario with lower response rates between 10 and 15% to a range of chemotherapy agents (Gordon et al, 2004; Mutch et al, 2007; Ferrandina et al, 2008). However, there is increasing evidence that by administering platinum in a ‘dose-dense’ manner involving increased schedule frequency and increased dose intensity, resistance can be overcome resulting in significant improvements in response (van der Burg et al, 2005).
Thus, dose density refers to increasing dose frequency while the dose per cycle and overall dose remains the same, thereby increasing the dose intensity and shortening overall treatment time (Simon and Norton, 2006). A number of different ‘dose-dense’ carboplatin and paclitaxel regimens have been developed for the treatment of recurrent ovarian cancer initially pioneered by van der Burg et al (2002). They reported a response rate of 46% in patients with a PFI of <4 months with weekly cisplatin (50–70 mg m−2) and daily oral etoposide for 6 weekly cycles, followed by maintenance oral etoposide. On the basis of finding that weekly paclitaxel is also very active in platinum-resistant disease, cisplatin and carboplatin have both been tolerably combined with paclitaxel in short duration weekly schedules. de Jongh et al (2002) and Van der Burg et al (2004) have reported on weekly induction regimens of cisplatin 70 mg m−2 or carboplatin AUC 4 with paclitaxel 90 mg m−2 for 6 weeks, followed by a return to three weekly schedules. The authors report a response rate of 60% in platinum-resistant disease and progression-free survival of 8–11 months. However, if the dose-dense regimen is likely to be the more active component of this regimen, there is a clear rationale for continuing with weekly treatment rather than reverting to a three weekly ‘maintenance’ schedule to which patients had prior resistance. In practice, with these Rotterdam regimens, the limitation in the dose-dense phase was toxicity.
Weekly dosing was also investigated earlier as part of the ‘Leuven’ dose regimen in which patients received continuous weekly carboplatin AUC 4 and paclitaxel 90 mg m−2 on day 1 and 8 every 21days for 6 cycles (Cadron et al, 2007). The authors reported a response rate of 38% in platinum-resistant patients with a progression-free survival of 6.8 months and an overall survival of 8 months; these results were achieved with significant haematological toxicity. Havrilesky et al (2003) investigated weekly carboplatin AUC 2 and paclitaxel 80 mg m−2 on day 1, 8 and 15 every 28 days until disease progression; thus not delivering dose-dense platinum, as the platinum dose intensity in this regimen is below that achieved with conventional schedules. For this regimen, a median of 5.5 cycles (477 pulses) was administered with a similar response rate of 38% reported in platinum-resistant patients and a progression-free survival of 3.2 months, and an overall survival of 11 months. Although these studies suggest that weekly platinum and taxane is an effective and well-tolerated approach in recurrent ovarian cancer, neither the optimal schedule nor its duration has been determined. This is important from the perspective not just of response rate and maximal tolerated dose but also from the perspective of potential durability of response in platinum-resistant disease.
Here, we report our experience of dose dense weekly carboplatin AUC 3 and paclitaxel 70 mg m−2 on day 1, 8, 15 q 4 weekly administered in patients with heavily pre-treated platinum-refractory and/or platinum-resistant ovarian cancer delivered for an intended six blocks of therapy (18 cycles). It shows excellent feasibility, tolerability and activity of this regime in a very difficult patient group. The importance and novelty of this regime is its feasibility and tolerability, and its potential for extended duration therapy allows us to contemplate its use as a scaffold for the safe integration of targeted therapies that may enhance the efficacy of platinum rechallenge in a platinum-resistant scenario.
Methods
This is a retrospective report of our experience of patients with a diagnosis of epithelial ovarian cancer who had relapsed within a platinum-resistant interval (⩽6 months) treated with dose-dense carboplatin and paclitaxel. Carboplatin AUC 3 and paclitaxel 70 mg m−2 were administered on day 1, 8, 15 q 4 weekly, with the intent to deliver six cycles of chemotherapy. Baseline CT imaging of the chest, abdomen and pelvis was carried out prior to the commencement of therapy and after every two cycles. Carboplatin dose was calculated by ethylenediaminetetraacetic acid clearance. Blood samples for full blood count, biochemistry, liver function tests and serum CA125 test were taken prior to the commencement of therapy and before each treatment. Patients were reviewed weekly during treatment for safety assessment. All safety evaluations were graded according to the NCI-CTC v5.0. Tumour response was assessed after every two cycles with repeat CT chest, abdomen and pelvis (RECIST criteria) and by CA125 (GCIG criteria) (Therasse et al, 2000; Rustin, 2003). Data regarding the planned and delivered weekly dose intensity of treatment, the overall treatment dose delivered, toxicity and clinical outcome were collected.
Survival
Progression-free survival was measured from the date of first treatment until either progression or death, the median OS was defined as the period of time between the start of the treatment and death and was censored at last follow-up. Survival curves were generated using Kaplan–Meier methodology. Univariate survival analyses were performed using the Kaplan–Meier method and log rank tests. The relationship between subgroup variability and response to treatment was analysed using either χ2-test or Fisher's exact test. Analysis was performed using SPSS software version 11.5 (SPSS Inc., Chicago, IL, USA).
Results
Patients
Twenty-three patients received dose-dense carboplatin/paclitaxel between August 2006 and August 2008. Two patients were excluded from analysis as one initially received cisplatin/etoposide and one received two cycles of three weekly carboplatin immediately prior to dose-dense therapy. All patients had histologically proven epithelial ovarian cancer. All patients had been treated earlier with carboplatin, and 18 (86%) patients had previous conventional schedule taxane exposure. Patient characteristics are shown in Table 1. The median age of the evaluable patients was 61 years (range 40–74 years). The majority of patients had a performance status of one (71%). Patients had received an average of three (range 1–8) prior chemotherapeutic regimens. Seven patients had platinum refractory disease following front-line therapy. The mean PFI was 5.1 months (range 0.5–13.9 months). The mean taxane-free interval was 16.8 months (range 1.2–75.1 months). Three patients had no prior exposure to taxanes. All patients had relapsed within a platinum-resistant time period and median time to relapse following platinum-based therapy is 5.4 months (range 0–6.7). However, three patients received treatment with non-platinum conventional chemotherapy regimens (two received liposomal doxorubicin and one received topotecan). Six patients symptomatically relapsed but were not treated within 6 months either because of prolonged hospitalisation or because patients elected to delay treatment. The mean treatment-free interval was 4.7 months (range 0.5–12.1 months).
Table 1. Patient demographics (N=21).
| Patient demographics | No of patients (%) |
|---|---|
| Age, years | |
| Median | 62 |
| Range | 41–75 |
| WHO performance status | |
| 0 | 6 (29) |
| 1 | 15 (71) |
| 2 | 0 |
| Tumour histology | |
| Serous | 19 (90) |
| Endometrioid | 2 (10) |
| Mucinous | 0 |
| Clear cell | 0 |
| Tumour differentiation grade | |
| 1 | 0 |
| 2 | 4 (20) |
| 3 | 16 (76) |
| Unknown | 1 (5) |
| Number of prior chemotherapeutic regimens | |
| 1 | 7 (33) |
| 2 | 6 (29) |
| 3 | 5 (24) |
| ⩾4 | 3 (14) |
| Time to relapse following last chemotherapy | |
| Median | 0.7 months |
| Range | 0–6.7 |
| Platinum-free interval, months | |
| <6 | 12 |
| ⩾6 | 9a |
| Taxane-free interval, months | |
| <6 | 8 |
| ⩾6 | 11 |
| No prior taxane | 3 |
Six patients relapsed within a platinum-resistant time period (<6 months) but elected to delay treatment. Three patients received alternative chemotherapy for the treatment of platinum-resistant disease.
An average of four blocks of dose-dense chemotherapy was administered (range 1–6). The mean delivered dose intensity of carboplatin per week was AUC 2.1 (range 0.5–2.25) against a planned dose intensity of AUC 2.25. The median ratio of carboplatin delivered vs planned dose was 95% (range 23–100). Although no dose reduction in paclitaxel dosing was required, a reduction in dose intensity was observed that was attributable to dose delay. The mean delivered dose intensity of paclitaxel was 50 mg m−2 per week (range 11.8–52.5) against a planned dose intensity of 52.5 mg m−2 per week. The median ratio of paclitaxel delivered vs planned dose was 91% (range 22–100).
Treatment efficacy
One patient was not assessed radiologically because of death prior to assessment. Therefore, 20 patients were assessed for radiological response. Confirmed partial tumour responses (RECIST) were reported in 12 patients (60%). No complete responses were reported. Four patients (20%) had stable disease and four (20%) patients had progressive disease on treatment. All patients were assessable for response by GCIG CA125 criteria. In all, 16 patients (76%) achieved a response (Table 2).
Table 2. Overall response rates to dose-dense carboplatin/paclitaxel.
| Response type | No. of patients (%) |
|---|---|
| Radiologic response | |
| Complete response | 0 |
| Partial response | 12 (60) |
| Stable disease | 4 (20) |
| Progressive disease | 4 (20) |
The rate of decline in CA125 was assessed in 18 patients compared with their rate of CA125 decline with first-line therapy. Three patients commenced their first-line treatment in other institutions and therefore their initial serum CA125 results were not available. In patients receiving dose-dense therapy the median half-life of serum CA125 was 16.5 days (range 0–41). The median half-life of serum CA125 in this population at the time of front-line treatment was longer at 18 days (range 0–42) (Table 3). Analysis of patients whose CA125 half-life response to dose-dense therapy was faster compared with front-line therapy revealed longer overall survival (mean overall survival 20.2 months (95% CI 12.5–27.9) vs 8.8 months (95% CI 6.1–11.6), P=0.018) but no difference in progression-free survival (PFS). No association was observed between CA125 half-life response to dose-dense therapy and PFI or exposure to prior taxane therapy.
Table 3. Half-life of serum CA125 (days) during front-line chemotherapy treatment and subsequent half-life with dose-dense chemotherapy.
| Subject number | First-line chemotherapy: half-life CA125 (days) | Dose-dense therapy: half-life CA125 (days) |
|---|---|---|
| 1 | 21 | 30 |
| 2 | 17 | 11 |
| 3 | 7.3 | 15 |
| 4 | 24 | 21 |
| 5 | 12 | 10 |
| 6 | 33 | 14 |
| 7 | 30 | 41 |
| 8 | — | 18 |
| 9 | — | R |
| 10 | 37 | R |
| 11 | 20 | 33 |
| 12 | 13 | R |
| 13 | R | 37 |
| 14 | — | 30 |
| 15 | 12 | 12 |
| 16 | 17 | 23 |
| 17 | 42 | 35 |
| 18 | 10 | 10 |
| 19 | 19 | 23 |
| 20 | 12 | 28 |
| 21 | 19 | 18 |
| Median | 18 | 18 |
R=Refractory.
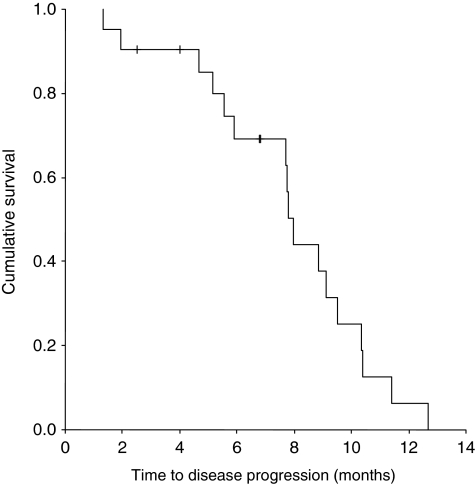
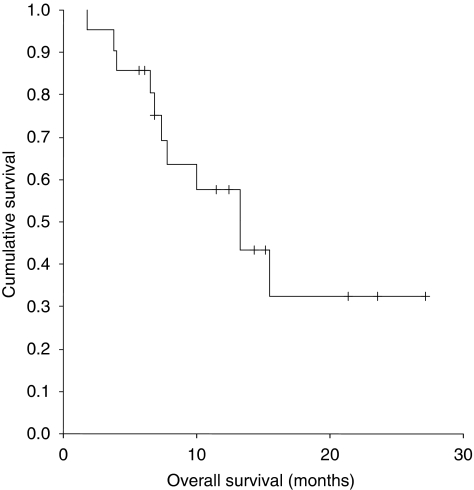
In the 16 patients who had been exposed to a taxane prior to weekly carboplatin/paclitaxel, the CA125 response rate was 81% and the radiologic response rate was 83%. There was no correlation between the response rate to dose-dense therapy, by either RECIST or GCIG criteria, and platinum-free interval, taxane-free interval or treatment-free interval. At the time of analysis, 11 patients had died. The median PFS was 7.9 months (95% CI 7.59–8.35) (Figure 1). The median overall survival was 13.3 months (95% CI 7.81–18.79) (Figure 2).
Figure 1.
Kaplan–Meier curve for time to disease progression in patients receiving dose-dense carboplatin and paclitaxel for platinum-resistant ovarian cancer.
Figure 2.
Kaplan–Meier curve for overall survival patients receiving dose-dense carboplatin and paclitaxel for platinum-resistant ovarian cancer.
Toxicity
Overall dose-dense carboplatin/paclitaxel was well tolerated (Table 4). Six patients (29%) experienced grade 3 neutropenia and one patient experienced grade 4 neutropenia. Two patients required admission for neutropenic sepsis (10%). One patient (5%) died as a result of sepsis. One patient experienced non-neutropenic line sepsis (5%). One patient (5%) experienced symptomatic grade 3 anaemia. Importantly, grade 3/4 thrombocytopenia or grade 4 anaemia were not observed.
Table 4. Haematologic and non-haematologic toxicity of dose-dense therapy.
| Grade no (%) | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Anaemia | 2 (10) | 13 (62) | 1 (5) | 0 |
| Neutropenia | 4 (19) | 5 (24) | 6 (29) | 1 (5) |
| Thrombocytopaenia | 1 (5) | 1 (5) | 0 | 0 |
| Lethargy | 3 (14) | 8 (38) | 0 | 0 |
| Nausea and vomiting | 4 (19) | 2 (10) | 0 | 0 |
| Oral mucositis | 2 (10) | 0 | 0 | 0 |
| Arthralgia | 1 (5) | 1 (5) | 0 | 0 |
| Neurotoxicity | 4 (19) | 1 (5) | 3 (14) | 0 |
| Renal toxicity | 1 (5) | 1 (5) | 0 | 0 |
| Otoxicity | 1 (5) | 1 (5) | 0 | 0 |
Three patients required dose reductions secondary to neutropenia (14%), and one patient required two additional dose reductions because of persistent neutropenia. Eight patients required dose delays (38%), predominantly because of neutropenia; however, we dose delayed patients rather than administer granulocyte-colony stimulating factor (G-CSF). Only three patients received G-CSF therapy (14%). G-CSF was administered 300 μg subcutaneously daily from day 3 to day 5. Three patients (14%) experienced treatment delays because of Unit holidays.
The most common non-haematologic toxicity was grade 2 lethargy (33%). Two patients (10%) experienced grade 2 nausea and vomiting. Three patients developed worsening of pre-existing peripheral neuropathy leading to the cessation of treatment. Three patients (14%) developed hypersensitivity reaction secondary to carboplatin infusion. One patient was managed effectively with pre-treatment with hydrocortisone 100 mg intravenously and chlorphenamine 10 mg intravenously prior to carboplatin infusion. Two patients ceased therapy because of hypersensitivity reactions to carboplatin.
Discussion
Several chemotherapeutic agents such as topotecan, gemcitabine, liposomal doxorubicin, paclitaxel and etoposide have been used in the treatment of platinum-resistant disease with unexciting response rates in the range 10–15% in this patient group (Swisher et al, 1997; Gordon et al, 2001). Our data show that the use of extended dose-dense chemotherapy results in a response rate of 60% in this poor prognosis group, which is consistent with previous published studies (de Jongh et al, 2002; Van der Burg et al, 2004). Extended dose-dense therapy affords the opportunity to effectively and tolerably treat conventionally platinum-resistant patients with platinum again, and this study shows the feasibility and tolerability of delivering up to six blocks (18 cycles) of this treatment. This finding is of importance as platinum resistance ultimately becomes the dominant problem for most patients with ovarian cancer. The approach described here holds promise in that it may be coupled to molecularly targeted therapies that can either reverse acquired platinum resistance or enhance intrinsic platinum sensitivity (Gordon et al, 2005; Schilder et al, 2005; Alvero et al, 2006; Appleton et al, 2007; Cannistra et al, 2007; Chien et al, 2007). This approach may feasibly enhance efficacy to the point that survival gains may become worthwhile. The regimen described in this report, therefore, needs to be tested in a phase III setting against the community standard for this population, pegylated liposomal doxorubicin.
The mechanism by which dose-dense therapy induces responses in patients with platinum-resistant disease is unclear. It is assumed that a fixed proportional cell kill is achieved at shorter time intervals, improving the overall impact of therapy, as it allows less time and opportunity for the emergence and proliferation of surviving cells. Furthermore, for S phase-specific drugs, more frequent dosing may expose more cells to the drug during the sensitive phase of the cell cycle. In addition, the use of weekly paclitaxel may have additional anti-angiogenic effects when used in a fractionated schedule (Belotti et al, 1996; Lau et al, 1999).
As outlined in the introduction, dose dense weekly schedules of carboplatin and paclitaxel have been investigated by a number of groups. These studies all differ in the dose intensity of carboplatin and paclitaxel administered, the duration of dose-dense therapy and the concurrent toxicity (Bolanos et al, 2001; Katsumata et al, 2001; Dunton, 2003; Havrilesky et al, 2003; Van der Burg et al, 2004; Kikuchi et al, 2005; Rose et al, 2005; Watanabe et al, 2005; Cadron et al, 2007). However, only four of the nine identified published studies enrolled patients with platinum-resistant disease (Table 5). The results from our study (a response rate of 60% and a PFS of 7.9 months in resistant or refractory disease) are comparable with these previously reported data, although the extended duration to six blocks (12 cycles total) has only been shown in the Leuven study, which with an AUC 4/taxol 90 mg m−2 dosing could be delivered only as 2 weeks on and 1 week off, with significant haematological toxicity, which therefore could make integration of additional biotherapies difficult (Cadron et al, 2007).
Table 5. Studies of weekly carboplatin and paclitaxel in platinum-resistant recurrent ovarian cancer.
| Study | Regimen | Platinum sensitivity | N | RR (%) | CR (%) | PFS (months) | OS (months) | Anaemia | Neutropaenia | Thrombocytopaenia | Neurotoxicity | Alopecia | Hypersensitivity |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cadron et al (2007) | T 90 mg m−2 per week | Total number | 29 | 66 | 21 | 9 | 18 | 24 | 94 | 25 | 3 | 0 | 9 |
| C AUC 4 per week | <6 months | 10 | 38 | 13 | 6.8 | 8 | |||||||
| Days 1, 8, q 3 weekly | 6–12 months | 11 | 73 | 18 | 10.5 | NR | |||||||
| 6 courses | >12 months | 8 | 80 | 30 | 12.8 | NR | |||||||
| 2.6 | |||||||||||||
| Van der Burg et al (2004) | T 90 mg m−2 per week | Total number | 62 | 74 | 24 | 11 | NR | 40 | 8 | 0 | 23 | ||
| C AUC 4 per week | <6 months | 23 | 61 | 13 | |||||||||
| Days 1, 8, 15, 29, 36, 49 | 6–12 months | 19 | 84 | 42 | |||||||||
| +6xTC q 3 weekly | >12 months | 20 | 80 | 20 | |||||||||
| Havrilesky et al (2003) | T 80 mg m−2 per week | Total number | 29 | 83 | 55 | 11.5 | 11 | 32 | 14 | 0 | 0 | 21 | |
| C AUC 2 per week | <6 months | 8 | 38 | 13 | 3.2 | 11.4 | |||||||
| Days 1, 8, 15 q 28 days until progression/CR+8 courses | >6 months | 21 | 100 | 71 | 13.7 | ||||||||
| Katsumata et al (2001) | T 80 mg m−2 per week | Total number | 45 (33) | 67 | 39 | 61 | 15 | 21 | 6 | ||||
| C AUC 2 per week | <6 months | 11 | 55 | (+ grade 2) | |||||||||
| for 18 weeks | >6 months | 16 | 73 | ||||||||||
| Current study | T 70 mg m−2 per week | Total number | 21 | 60 | 0 | 7.9 | 13.3 | 5 | 30 | 0 | 15 | NR | 14 |
| C AUC 3 per week | Refractory | 5 | 25 | 8.9 | 6.8 | ||||||||
| Days 1, 8, 15 q 4 weekly | <6 months | 7 | 25 | 5.5 | — | ||||||||
| 4–6 courses | >6 months | 9 | 50 | 7.8 | 10.0 |
N=number of patients; RR=response rate; CR=complete remission; PFS=progression-free survival; OS=overall survival; T=paclitaxel; C=carboplatin; NR=not reached.
Toxicity is grade ⩾3 and expressed in percentage. Adapted from Cadron et al (2007).
We calculated the half-life of serum CA125, and have shown a more rapid decline in CA125 after dose-dense therapy in platinum-resistant disease compared with CA125 decline in front-line therapy for individual patients. Furthermore, we have shown that patients whose CA125 half-life response to dose-dense therapy was faster compared with front-line therapy had an improved overall survival when compared with those with a slower response. This is consistent with previously published front-line studies, which suggest that a shorter half-life is associated with improved prognosis (Riedinger et al, 2008) (Mano et al, 2005) (Gadducci et al, 2004). No study, however, has compared the decline in CA125 within patients with subsequent treatments and the impact on clinical outcomes. Although interesting, these results are based on a small sample size and need confirmation in a larger patient population.
Although all the patients relapsed within a platinum-resistant interval, treatment was delayed in nine patients such that these patients did not receive a platinum regimen within 6 months. Despite this, no differences were observed in response rates for this group; however, it is possible that this subgroup may have been more sensitive (resensitised) to platinum. A significant minority of patients were not prior taxane exposed, which may also have affected response to weekly therapy, although the small sample size for this subgroup precluded statistical evidence for this. Nevertheless, this is overall one of the largest reports of dose dense weekly therapy in the resistant patient population and further supports this approach to treatment in a difficult clinical scenario. The ‘3 weeks on, 1 week off’ regimen described here differs from those published earlier in its tolerability and, therefore, potential for extension of therapy for at least 18 cycles, over 24 weeks and possible use for treatment to progression (which is not a standard approach in the United Kingdom, but may be more acceptable in other countries).
We have shown that dose-dense carboplatin/paclitaxel regimen can be administered safely with minimal toxicity in heavily pre-treated platinum-resistant patients. In particular, we report a negligible incidence of thrombocytopenia, the most important and unaddressable dose limiting factor in this approach, and a low incidence of grade 3/4 neutropenia (30%) in contrast to other published studies. In particular, the study by Cadron et al (2007) investigating carboplatin AUC 4 and paclitaxel 90 mg m−2 on day 1 and 8 every q 4 weekly reported an incidence of grade 3/4 neutropenia in 94% and thrombocytopenia in 25% of patients. These toxicities would have curtailed the extended duration of the use of this regimen and feasibility for integration with other molecularly targeted therapies. Only one previous study examining carboplatin AUC 2 and paclitaxel 80 mg m−2 reports a comparable rate of neutropenia; however, the authors report a higher incidence of grade 3/4 thrombocytopenia, and this study does not deliver dose-dense platinum, indeed the dose intensity of platinum is less than that of conventional therapy (Havrilesky et al, 2003). Furthermore, we report a low incidence of anaemia compared with the previous reports. We did observe a significant number of dose delays because of neutropenia. As described above, we tended to dose delay rather than administer G-CSF in myelosuppression and this may have compromised the dose intensity of delivered chemotherapy. In future studies, we propose the addition of G-CSF 300 μg daily from day 3 to 5 to avoid neutropenia and maintain dose intensity, and it will be interesting to observe whether this will impact thrombocytopenia adversely. Interestingly, we also did not observe a high rate of neurotoxicity despite the majority of patients having had prior treatment with a taxane. Because of the impact of neurotoxicity on patient quality of life, we plan to formally assess neuropathy prior to and post dose-dense therapy in future studies. A major limitation to the use of dose-dense therapy is the development of hypersensitivity to platinum. Previous studies do report hypersensitivity occurring in 6–23% of patients treated. We report 14% of patients developing hypersensitivity. Although one patient was effectively managed with the use of hydrocortisone and anti-histamines, two patients had to cease treatment. Desensitisation to platinum agents is an active area of research and this may impact favourably on the deliverability of platinum agents in the future.
This regimen is therefore a safe and effective regimen for the management of platinum-resistant relapse, and efforts are underway to explore this regimen in randomised clinical trials against the current standard of care in platinum-resistant ovarian cancer. Translational research efforts are also showing that inhibition of several molecular targets can reverse acquired clinical platinum resistance in vitro, and adaptations of this regimen will be explored as a platinum scaffold to incorporate inhibitors to such targets in order to maximise clinical benefit to patients with platinum-resistant ovarian cancer (Stronach et al, 2008).
Acknowledgments
This work was supported by Imperial College Biomedical Research Centre Experimental Cancer Medicine Centre.
References
- Alvero AB, O’Malley D, Brown D, Kelly G, Garg M, Chen W, Rutherford T, Mor G (2006) Molecular mechanism of phenoxodiol-induced apoptosis in ovarian carcinoma cells. Cancer 106: 599–608 [DOI] [PubMed] [Google Scholar]
- Appleton K, Mackay HJ, Judson I, Plumb JA, McCormick C, Strathdee G, Lee C, Barrett S, Reade S, Jadayel D, Tang A, Bellenger K, Mackay L, Setanoians A, Schatzlein A, Twelves C, Kaye SB, Brown R (2007) Phase I and pharmacodynamic trial of the DNA methyltransferase inhibitor decitabine and carboplatin in solid tumors. J Clin Oncol 25: 4603–4609 [DOI] [PubMed] [Google Scholar]
- Belotti D, Vergani V, Drudis T, Borsotti P, Pitelli MR, Viale G, Giavazzi R, Taraboletti G (1996) The microtubule-affecting drug paclitaxel has antiangiogenic activity. Clin Cancer Res 2: 1843–1849 [PubMed] [Google Scholar]
- Bolanos M, Borrega P, Gonzalez-Beca R, Arranz JA, Velasco A, Perez MM, Gomez-Bernal A, Martinez-Prado P, Pedro de Alcantara HS (2001) Weekly paclitaxel/carboplatinum as first-line chemotherapy in late relapses of epithelial ovarian cancer. A preliminary report on side effects. Proc Am Soc Clin Oncol 20, (abstr 870) [Google Scholar]
- Cadron I, Leunen K, Amant F, Van Gorp T, Neven P, Vergote I (2007) The ‘Leuven’ dose-dense paclitaxel/carboplatin regimen in patients with recurrent ovarian cancer. Gynecol Oncol 106: 354–361 [DOI] [PubMed] [Google Scholar]
- Cannistra SA, Matulonis UA, Penson RT, Hambleton J, Dupont J, Mackey H, Douglas J, Burger RA, Armstrong D, Wenham R, McGuire W (2007) Phase II study of bevacizumab in patients with platinum-resistant ovarian cancer or peritoneal serous cancer. J Clin Oncol 25: 5180–5186 [DOI] [PubMed] [Google Scholar]
- Chien JR, Aletti G, Bell DA, Keeney GL, Shridhar V, Hartmann LC (2007) Molecular pathogenesis and therapeutic targets in epithelial ovarian cancer. J Cell Biochem 102: 1117–1129 [DOI] [PubMed] [Google Scholar]
- de Jongh FE, de Wit R, Verweij J, Sparreboom A, van den Bent MJ, Stoter G, van der Burg ME (2002) Dose-dense cisplatin/paclitaxel. a well-tolerated and highly effective chemotherapeutic regimen in patients with advanced ovarian cancer. Eur J Cancer 38: 2005–2013 [DOI] [PubMed] [Google Scholar]
- Dunton CJ (2003) Phase II study of weekly paclitaxel and weekly carboplatinum in recurrent platinum sensitive ovarian cancer. Proc Am Soc Clin Oncol 22, (abstr 1876) [Google Scholar]
- Eisenhauer EA, ten Bokkel Huinink WW, Swenerton KD, Gianni L, Myles J, van der Burg ME, Kerr I, Vermorken JB, Buser K, Colombo N (1994) European-Canadian randomized trial of paclitaxel in relapsed ovarian cancer: high-dose versus low-dose and long versus short infusion. J Clin Oncol 12: 2654–2666 [DOI] [PubMed] [Google Scholar]
- Ferrandina G, Ludovisi M, Lorusso D, Pignata S, Breda E, Savarese A, Del Medico P, Scaltriti L, Katsaros D, Priolo D, Scambia G (2008) Phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in progressive or recurrent ovarian cancer. J Clin Oncol 26: 890–896 [DOI] [PubMed] [Google Scholar]
- Gadducci A, Cosio S, Fanucchi A, Negri S, Cristofani R, Genazzani AR (2004) The predictive and prognostic value of serum CA 125 half-life during paclitaxel/platinum-based chemotherapy in patients with advanced ovarian carcinoma. Gynecol Oncol 93: 131–136 [DOI] [PubMed] [Google Scholar]
- Gordon AN, Finkler N, Edwards RP, Garcia AA, Crozier M, Irwin DH, Barrett E (2005) Efficacy and safety of erlotinib HCl, an epidermal growth factor receptor (HER1/EGFR) tyrosine kinase inhibitor, in patients with advanced ovarian carcinoma: results from a phase II multicenter study. Int J Gynecol Cancer 15: 785–792 [DOI] [PubMed] [Google Scholar]
- Gordon AN, Fleagle JT, Guthrie D, Parkin DE, Gore ME, Lacave AJ (2001) Recurrent epithelial ovarian carcinoma: a randomized phase III study of pegylated liposomal doxorubicin versus topotecan. J Clin Oncol 19: 3312–3322 [DOI] [PubMed] [Google Scholar]
- Gordon AN, Tonda M, Sun S, Rackoff W (2004) Long-term survival advantage for women treated with pegylated liposomal doxorubicin compared with topotecan in a phase 3 randomized study of recurrent and refractory epithelial ovarian cancer. Gynecol Oncol 95: 1–8 [DOI] [PubMed] [Google Scholar]
- Havrilesky LJ, Alvarez AA, Sayer RA, Lancaster JM, Soper JT, Berchuck A, Clarke-Pearson DL, Rodriguez GC, Carney ME (2003) Weekly low-dose carboplatin and paclitaxel in the treatment of recurrent ovarian and peritoneal cancer. Gynecol Oncol 88: 51–57 [DOI] [PubMed] [Google Scholar]
- Katsumata N, Watanabe T, Mukai H, Kasamatsu T, Tsunematsu R, Yamada T, Ohmi K (2001) A phase II trial of weekly paclitaxel/carboplatin (TJ) as salvage chemotherapy in patients with relapsed ovarian cancer. Proc Am Soc Clin Oncol 20, (abstr 865) [Google Scholar]
- Kikuchi A, Sakamoto H, Yamamoto T (2005) Weekly carboplatin and paclitaxel is safe, active, and well tolerated in recurrent ovarian cancer cases of Japanese women previously treated with cisplatin-containing multidrug chemotherapy. Int J Gynecol Cancer 15: 45–49 [DOI] [PubMed] [Google Scholar]
- Lau DH, Xue L, Young LJ, Burke PA, Cheung AT (1999) Paclitaxel (Taxol): an inhibitor of angiogenesis in a highly vascularized transgenic breast cancer. Cancer Biother Radiopharm 14: 31–36 [DOI] [PubMed] [Google Scholar]
- Mano A, Godinho I, Falcao AC (2005) CA 125 half-life breakpoint between a ‘good’ and ‘poor’ prognosis in patients with ovarian cancer. Int J Gynaecol Obstet 88: 333–335 [DOI] [PubMed] [Google Scholar]
- Markman M, Rothman R, Hakes T, Reichman B, Hoskins W, Rubin S, Jones W, Almadrones L, Lewis Jr JL (1991) Second-line platinum therapy in patients with ovarian cancer previously treated with cisplatin. J Clin Oncol 9: 389–393 [DOI] [PubMed] [Google Scholar]
- Mutch DG, Orlando M, Goss T, Teneriello MG, Gordon AN, McMeekin SD, Wang Y, Scribner Jr DR, Marciniack M, Naumann RW, Secord AA (2007) Randomized phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in patients with platinum-resistant ovarian cancer. J Clin Oncol 25: 2811–2818 [DOI] [PubMed] [Google Scholar]
- Neijt JP, ten Bokkel Huinink WW, van der Burg ME, van Oosterom AT, Willemse PH, Vermorken JB, van Lindert AC, Heintz AP, Aartsen E, van Lent M, Trimbos JB, De Meijer AJ (1991) Long-term survival in ovarian cancer. Mature data from The Netherlands Joint Study Group for Ovarian Cancer. Eur J Cancer 27: 1367–1372 [DOI] [PubMed] [Google Scholar]
- Piver MS, Baker TR, Piedmonte M, Sandecki AM (1991) Epidemiology and etiology of ovarian cancer. Semin Oncol 18: 177–185 [PubMed] [Google Scholar]
- Riedinger JM, Eche N, Basuyau JP, Dalifard I, Hacene K, Pichon MF (2008) Prognostic value of serum CA 125 bi-exponential decrease during first line paclitaxel/platinum chemotherapy: a French multicentric study. Gynecol Oncol 109: 194–198 [DOI] [PubMed] [Google Scholar]
- Rose PG, Smrekar M, Fusco N (2005) A phase II trial of weekly paclitaxel and every 3 weeks of carboplatin in potentially platinum-sensitive ovarian and peritoneal carcinoma. Gynecol Oncol 96: 296–300 [DOI] [PubMed] [Google Scholar]
- Rustin GJ (2003) Use of CA-125 to assess response to new agents in ovarian cancer trials. J Clin Oncol 21: 187s–193s [DOI] [PubMed] [Google Scholar]
- Schilder RJ, Sill MW, Chen X, Darcy KM, Decesare SL, Lewandowski G, Lee RB, Arciero CA, Wu H, Godwin AK (2005) Phase II study of gefitinib in patients with relapsed or persistent ovarian or primary peritoneal carcinoma and evaluation of epidermal growth factor receptor mutations and immunohistochemical expression: a Gynecologic Oncology Group Study. Clin Cancer Res 11: 5539–5548 [DOI] [PubMed] [Google Scholar]
- Simon R, Norton L (2006) The Norton-Simon hypothesis: designing more effective and less toxic chemotherapeutic regimens. Nat Clin Pract Oncol 3: 406–407 [DOI] [PubMed] [Google Scholar]
- Stronach EA, Rama N, Gabra H (2008) Identification of functional modulators of platinum resistance using isogenically matched ovarian cancer cell line models. Proc of the 99th Annual Meeting of the American Association for Cancer Research 699 [Google Scholar]
- Swisher EM, Mutch DG, Rader JS, Elbendary A, Herzog TJ (1997) Topotecan in platinum- and paclitaxel-resistant ovarian cancer. Gynecol Oncol 66: 480–486 [DOI] [PubMed] [Google Scholar]
- Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92: 205–216 [DOI] [PubMed] [Google Scholar]
- van der Burg ME, de Wit R, van Putten WL, Logmans A, Kruit WH, Stoter G, Verweij J (2002) Weekly cisplatin and daily oral etoposide is highly effective in platinum pretreated ovarian cancer. Br J Cancer 86: 19–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Burg ME, Hoff AM, van Lent M, Rodenburg CJ, van Putten WL, Stoter G (1991) Carboplatin and cyclophosphamide salvage therapy for ovarian cancer patients relapsing after cisplatin combination chemotherapy. Eur J Cancer 27: 248–250 [DOI] [PubMed] [Google Scholar]
- van der Burg ME, van der Gaast A, Vergote I, Burger CW, van Doorn HC, de Wit R, Stoter G, Verweij J (2005) What is the role of dose-dense therapy? Int J Gynecol Cancer 15(Suppl 3): 233–240 [DOI] [PubMed] [Google Scholar]
- Van der Burg ME, Vergote I, Burger CW, Van der Gaast A (2004) Phase II study of weekly paclitaxel carboplatin in the treatment of progressive ovarian cancer. J Clin Oncol 22: 5058 [Google Scholar]
- Watanabe Y, Nakai H, Ueda H, Hoshiai H (2005) Evaluation of weekly low-dose paclitaxel and carboplatin treatment for patients with platinum-sensitive relapsed ovarian cancer. Gynecol Oncol 96: 323–329 [DOI] [PubMed] [Google Scholar]