Abstract
Background
Modern professional tennis involves powerful movements repeatedly subjecting the musculoskeletal system to heavy mechanical load. Thus tennis players are exposed to high risk of overuse injuries including stress fractures.
Objective
To determine the incidence and distribution of stress fractures in elite tennis players.
Study design
Retrospective cohort study.
Methods
The cohort study population consisted of 139 elite players (mean (SD) age, 20.0 (5.0) years; 48 female, 91 male). Stress fractures were identified and confirmed radiologically from medical records during a two year period. Injuries were analysed according to age, sex, site, severity, delay in diagnosis, and time needed to return to sports.
Results
15 players sustained 18 stress fractures, corresponding to an overall case incidence of 12.9% (95% confidence interval (CI), 8.1 to 20.0). The tarsal navicular was most affected (n = 5; 27%), followed by the pars interarticularis (n = 3; 16%), the metatarsals (n = 3; 16%), the tibia (n = 2; 11%) and the lunate (n = 2; 11%). Magnetic resonance imaging showed a greater incidence of “high grade” lesions (94.4%). Stress fracture incidence was significantly higher in juniors (20.3% (95% CI, 11.4 to 33.2)) than in professional players (7.5% (2.8 to 15.6)) (p = 0.045).
Conclusions
There was a high absolute risk (12.9%) of stress fractures in elite tennis players over a two year period. Junior players were at highest risk. The lesions are a major cause of disruption both of training and of competition. Risk factors should therefore be identified and prevention emphasised.
Keywords: stress fracture, tennis, overuse, lunate bone, MRI
Stress fractures are considered common overuse injuries among athletes and represent a major disruption to training and competition.1,2 They result from excessive, repetitive, submaximal loads on bones that cause an imbalance between bone resorption and formation. Several investigators have mentioned that stress fractures in tennis players are rarely observed,3,4,5 but there is limited scientific information about such injuries in this particular sport. Most available data regarding stress fractures in tennis players are to be found in case reports and case series of athletes participating in different sports.1,6,7 Case series allow assessment of their relative frequency in comparison with other injuries and with other sports, but has no value in estimating the incidence of stress fracture in a population.1,6 A single case report, although often used to present details about an unusual stress fracture, does not provide any additional information.
Modern competitive tennis encompasses a variety of powerful actions that place the player at risk of injury by subjecting the skeleton to repeated high mechanical loads.8 The incidence of stress fractures in elite tennis players seems to be increasing, probably because of increased diagnostic suspicion, increased intensity and volume of training, and new stroke techniques. To the best of our knowledge this is the first study investigating stress fractures in a tennis player cohort.
Our aim was to determine the incidence and distribution of stress fractures in elite tennis players.
Methods
Study design
Incidence is the more widely used measure in stress fracture reports.6 It quantifies the number of new injuries that develop in a population of individuals at risk during a specific time interval.9 A retrospective cohort study design was instituted to determine stress fracture incidence and distribution in elite tennis players.
Subjects
Players designated by the Argentine Tennis Association for medical care at the High Performance National Training Centre during a two year period (2003/2004) were selected as the study population. The standard programme comprised two full medical examinations each year. All subjects were top ranked national players, male and female, professionals and juniors. Subjects were included in the study if they met the following criteria: age between 13 and 35 years; girls had to be post‐menarcheal; and no disease or drug treatment likely to influence bone density.
The cohort included 145 tennis players (95 male, 50 female). Sixteen were excluded from the analysis, representing an overall attrition rate of 10.9%. Of these exclusions, four retired from regular tennis training, two moved to another country, two girls had primary amenorrhoea, one player had type I diabetes which is potentially linked to osteopenia, and seven did not attend scheduled medical follow up visits. The final study population included 139 elite tennis players (mean (SD) age, 20.0 (5.0) years; 91 male, 48 female). Eighty players (57.5%) were “professionals” (over 18 years of age) and 59 (42.4%) were “juniors” (under 18).
Procedures
This study was undertaken after approval from the institutional research and ethics committee.
After the 24 month period, we reviewed documented medical records, looking for all confirmed clinical cases of stress fracture, regardless of anatomical location. Diagnostic criteria for stress fracture were as follows:
no history of related trauma;
pain associated with exercise and relieved by rest;
localised bony tenderness, pain on bone loading or on pain‐eliciting manoeuvres;
radiographic and magnetic resonance imaging confirmation of diagnosis;
minimum follow up six months after returning to sports.
For practical reasons, the term “stress fracture” in this study is used to refer to the full spectrum of bone stress injuries.
Time to diagnosis was defined as the period between symptom onset and stress fracture imaging diagnosis.
All players with suspected diagnosis of stress fracture were evaluated with conventional radiographs and magnetic resonance imaging (MRI). Additionally, players presenting with clinical symptoms consistent with spondylolysis were evaluated by single photon emission computed tomography (SPECT). Radiographs were considered positive if they showed fracture lines, periosteal reaction, medullar sclerosis, or callus formation.10,11,12 MRI is considered the gold standard for stress fracture diagnosis.10,13,14,15,16 It has a sensitivity comparable to radionuclide techniques for bone abnormality detection, with the additional advantage of depicting soft tissue processes, as well as providing greater specificity. All MRI studies were done using high field strength equipment (Echo‐Speed 1.5 T, General Electric, Milwaukee, USA). A combination of T1 weighted sequences, which optimise anatomical detail, and a sequence depicting bone oedema is required for assessment of stress injuries. T2 weighted and T2 fat‐sat sequences were also obtained routinely. All MRI studies were evaluated by a radiologist specialising in the musculoskeletal system. Stress fractures were classified according to the guidelines of Arendt et al (table 1), which have shown a significant correlation between the MRI appearance and injury morbidity.13,14 These same investigators have also advocated a simplified classification into “low grade stress fracture” and “high grade stress fracture”.14 Finally, “low risk stress fracture” and “high risk stress fracture” were determined according to anatomical site, time to healing, and propensity to union.2,17 “Low risk stress fractures” have a favourable prognosis when treated with activity restriction and include all upper extremity lesions, ribs, pars interarticularis, sacrum, pubic rami, femoral shaft, tibial shaft, fibula, calcaneus, and metatarsal shaft.17 In contrast, “high risk stress fractures” are prone to delayed union or non‐union, especially if diagnosis is delayed, and include the femoral neck, patella, anterior tibial cortex, medial malleolus, talus, tarsal navicular, fifth metatarsal, second metatarsal base, and great toe sesamoids.2,17
Table 1 Radiological grading of stress fractures (Arendt et al13).
| Radiology | Bone scan | MRI | ||
|---|---|---|---|---|
| Normal | Normal | Normal | Normal | |
| Grade 1 | Normal | Poorly defined area of increased activity | Positive STIR image | |
| Grade 2 | Normal | More intense but still poorly defined | Positive STIR plus positive T2 | |
| Grade 3 | Discrete line (?), discrete periosteal reaction (?) | Sharply demarked area of increased activity focal or fusiform | Positive T1 and T2 but without definite cortical break | |
| Grade 4 | Fracture or periosteal reaction | More intense transcortical localised uptake | Positive T1 and T2 fracture line |
MRI, magnetic resonance imaging; STIR, short T1 inversion recovery.
Time to return to sport was obtained from medical records and checked for all patients. Both “full return” and “return with activity restriction” were charted. “Full return” was defined as the ability of the player to practise and compete without restrictions and without relapse.13 “Return with activity restriction” was defined as a return to tennis but with participation on a limited basis (practice time).13
Results
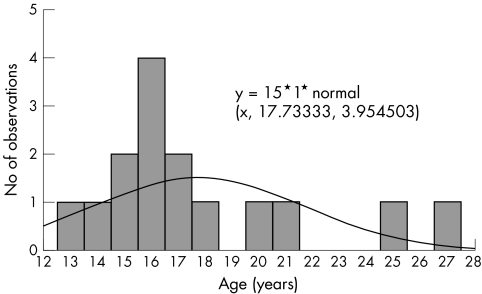
Four women and 11 men (mean (SD) age, 17.8 (4.0) years) of the total of 139 study participants sustained stress fractures; three women suffered bilateral injuries. Consequently, 15 participants sustained 18 stress fractures, generating an overall case incidence of 12.9% (95% confidence interval (CI), 8.1 to 20.0) in elite tennis players. The incidence of more than one injury was 2.9%. No significant difference between the male rate (12.1% (95% CI, 6.5 to 21.0)) and the female rate (14.6% (6.1 to 27.8)) was observed (p = 0.451, Fisher's exact test). The age of injured players averaged 17.3 (4.0) years; the age distribution is presented in fig 1. Stress fracture incidence was significantly higher in “junior” players (20.3% (95% CI, 11.4 to 33.2)) than in “professionals” (7.5% (2.8 to 15.6) (p = 0.0455, Fisher's exact test).
Figure 1 Age distribution of stress fractures in a cohort group of elite tennis players.
The tarsal navicular site was the most common for stress fractures (n = 5; 27.7%), followed by the pars interarticularis (n = 3; 16.6%), the metatarsal bones (n = 3; 16.6%), the tibia (n = 2; 11.1%), the lunate (n = 2; 11.1%), the pubic rami (n = 1; 5.5%), the metacarpals (n = 1; 5.5%), and the ulna (n = 1; 5.5%). Lower limb stress fractures (n = 10; 55.5%) were more common than upper extremity lesions (n = 4; 22.2%) and core injuries (n = 4; 22.2%).
None of the players sustaining stress fracture during the study period had a prior history of such lesions. One junior male player sustained two injuries (cases 11 and 13) at separate sites and on different occasions (non‐dominant ulna and lumbar spondylolysis).
Time to diagnosis averaged 7.0 (4.9) weeks and was longer for spondylolysis and navicular cases. The clinical results are summarised in table 2.
Table 2 Descriptive results of stress fractures in elite tennis players.
| Case | Sex, | Anatomical site | MRI | Time to diagnosis | Return to sport |
|---|---|---|---|---|---|
| age (y) | grade | ||||
| 1 | F, 27 | Tarsal navicular R | 4 | 4 w | AR, 32 w |
| Tarsal navicular L | 4 | 4 w | |||
| 2 | M, 25 | Tarsal navicular R | 4 | 6 w | Full, 20 w |
| 3 | F, 14 | Tarsal navicular R | 3 | 18 w | Full, 15 w |
| Tarsal navicular L | 3 | 18 w | |||
| 4 | M, 18 | 4th metatarsal R | 3 | 3 w | Full, 9 w |
| 5 | M, 17 | 2nd metatarsal R | 4 | 2 w | Full, 7 w |
| 6 | F, 15 | 1st metatarsal L | 4 | 4 w | Full, 9 w |
| 7 | F, 20 | Tibia R | 3 | 5 w | Full, 12 w |
| Tibia L | 3 | 5 w | |||
| 8 | M, 17 | 2nd metacarpal D | 3 | 3 w | Full, 10 w |
| 9 | M, 16 | Lunate D | 3 | 3 w | Full, 10 w |
| 10 | M, 15 | Lunate D | 3 | 4 w | Full, 9 w |
| 11 | M, 16 | Ulna L | 1 | 8 w | Full, 2 w |
| 12 | M, 16 | Pars interarticularis L5 R+L | 4 | 6 w | Full, 20 w |
| 13 | M, 17 | Pars interarticularis L5 L | 4 | 14 w | Full, 24 w |
| 14 | M, 13 | Pars interarticularis L5 R+L | 4 | 8 w | Full, 23 w |
| 15 | M, 21 | Pubic ramus L | 3 | 10 w | Full, 10 w |
AR, return with activity restriction; D, dominant; F, female; L, left side; M, male; MRI, magnetic resonance imaging; R, right side; w, weeks; y, years.
Radiographs were initially negative in 14 cases (77.7%). All three players with lumbar spondylolysis (table 2, cases 12, 13, and 14) had fracture lines on oblique views, and a fourth metatarsal stress fracture (table 2, case 4) showed cortical disruption.
Of the 18 stress fractures diagnosed by MRI, one was grade 1 (5.5%), none were grade 2, nine were grade 3 (50%), and eight were grade 4 (44.4%). Following the simplified classification, one was considered a “low grade stress fracture” (5.5%) and 17 were considered “high grade stress fractures” (94.4% (95% CI, 73.0 to 99.9)). A prognostic classification based on bone involvement showed that five injuries were “high risk stress fractures” (27.7%) and 13 were “low risk stress fracture” (72.2%). All high risk stress fractures were tarsal navicular injuries. Lunate stress fractures were considered to be low risk stress fractures.
No bone biopsies were done. All patients were treated conservatively, with management depending on location. Supervised physical therapy was completed at the same medical centre.
Time required to return to sports averaged 15.1 (8.4) weeks. Fourteen patients (93.3%) returned to pre‐injury tennis performance levels; one female player (6.7%) who had bilateral tarsal navicular grade 4 stress fractures returned to professional competition but with persistent discomfort after matches and was forced to reduce training volume. A significant correlation was observed between grade of injury determined by MRI and time needed to return to tennis (r = 0.66; p = 0.002, Pearson test).
Discussion
The results of this study showed that an elite tennis player had 12.9% absolute risk of developing a stress fracture during a two year period. Although various clinical series have described the relative frequency of stress fractures in tennis players, few studies have reported true incidence figures. Goldberg and Pecora4 reviewed the medical records of stress fractures in collegiate athletes over a three year period and estimated the rate for tennis players to be 8%. Johnson et al5 conducted a two year prospective study in different collegiate athletes and found no cases among tennis players. Other case series have reported relative stress fracture incidences, comparing several sports and the distribution of stress fractures in tennis players.18,19 The higher incidence observed in the present series probably reflects the elite athletic level of this population, who are usually exposed to heavy training loads.
There is consensus that particular sports are associated with specific stress fracture sites.2,6 Brukner et al18 have studied 180 cases of stress fractures in several sports retrospectively; the pars interarticularis and the fibula were the most affected bones in tennis players. Iwamoto and Takeda19 reviewed 196 cases of stress fracture in athletes, and reported only five cases (2.6%) affecting tennis players (tibia and ribs).
Female tennis players had a higher incidence of stress fractures than male participants. Although studies in military populations have reported that female recruits are at higher risk of stress fractures than male recruits,20 sex differences in stress fractures among athletes have not been so evident.5,6,21 In the present study, the medical records of the female tennis players did not show any pathological conditions usually associated with stress fractures such as amenorrhoea, osteoporosis, or eating disorders.
One of the main findings of this study was that junior elite players had a higher incidence of stress fractures than professional adults. It is unclear whether age as an independent factor influences stress fracture risk.6 Results in the military are conflicting, and there are no studies in athletes investigating the incidence of stress fractures in individuals of different ages engaged in identical training programmes. Milgrom et al22 reported that with each year of increase in age from 17 to 26 years, stress fracture risk for any site decreased by 28%. Young competitive tennis players usually engage in intense, professional participation and perform long daily training sessions from an early age. Often, adult training volume and progression formulas are mistakenly applied to adolescent tennis players.23 There is evidence that many competitive tennis players are overtrained and exposed to excessive physical activity which may increase the risk of injury and decrease performance.23 Pain is the key symptom in overuse injuries such as stress fractures. However, it is typically a late indicator, and inappropriate loads may already have been applied for several weeks. To minimise the risk of overuse injury in young competitive tennis players, a detailed training programme based on improved scheduling, progression, and cross training principles should be instituted.24 As a simple rule, all adolescents involved in competitive tennis should rest at least one day a week and undertake one week of light training per month.25
Clinically, it seems that recurrence of stress fractures at new sites is common,1 possibly indicating the persistence of risk factors in susceptible individuals.6 Interestingly, we observed a no history of stress fractures in the 15 players who sustained lesions.
An early accurate diagnosis of stress fractures is essential for avoiding both complications and prolonged delay of return to competition. Imaging is an essential step when considering stress fractures as differential diagnosis for sports related injuries. Although conventional radiographs continue to be used as the primary method for diagnosis,26 limitations in early stress fracture detection have been increasingly recognized: two third are negative and only half of these will ever develop radiographic evidence of a stress fracture.27 Before the development of MRI, bone scintigraph represented the primary diagnostic method for clinically suspected stress fractures.10,11,13,15,28 It has high sensitivity and allows estimation of healing potential.15 However, MRI is currently considered the gold standard for diagnostic evaluation of stress fractures. It is highly sensitive and allows the detection of abnormalities early after symptom onset. MRI is capable of depicting the full range of stress injury involving bone10,27,29 and is very specific in determining the age of the stress phenomenon.15 The grading system proposed by Arendt et al14 is useful in determining stress fracture severity and estimating morbidity. Radionuclide techniques still play a role in the assessment of patients complaining of overuse related pain, especially for injuries to the spine and ribs.30
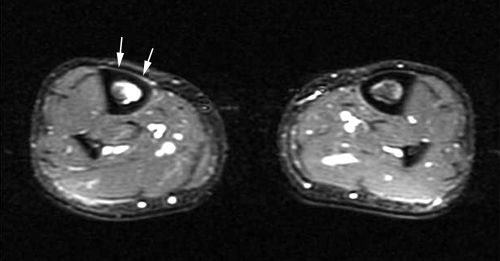
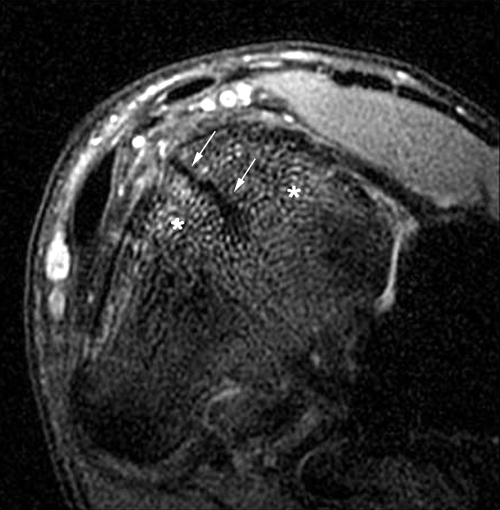
As for all weight bearing sports, in tennis most stress fractures occurred in the lower extremities2 (fig 2). In the present study, the tarsal navicular and the metatarsals were the bones most affected. These sites also correspond to typical power sport stress injury locations.6 Stress fractures to the navicular bone warrant special consideration because of diagnostic and treatment challenges. These injuries are difficult to visualise radiographically. In this series, all five cases had negative initial x rays. CT is more sensitive than MRI for fracture line detection, but MRI detects a higher proportion of medullary extensions.31 Thus the diagnosis of navicular stress injuries may benefit from both imaging modes. Treatment is complicated by the relative avascularity of the central third of the bone. Risks of navicular stress fracture include complete fracture or displacement, delayed union, and non‐union.13 Indeed, one player in this study (table 2, case 1) reached her highest professional ranking after recovering from a bilateral grade 4 navicular stress fracture (fig 3) but, at final follow up, was still suffering pain which partially restricted her activity. It is interesting that the majority of foot stress fractures were high grade at the time of the initial visit. This may be explained by the fact that athletes tolerate more foot pain before seeking consultation.13
Figure 2 Case 7: bilateral tibial stress fracture. Axial short T1 inversion recovery (STIR) image (TR2000/TE40/TI150) shows bone marrow oedema and hyperintense line adjacent to the anteromedial border of the right tibia, representing periosteal oedema (white arrows).
Figure 3 Case 1: grade 4 tarsal navicular stress fracture. Coronal DP fat suppressed image (TR1900/TE47) shows bone marrow oedema as diffuse signal enhancement. The linear hypointense image represents the fracture line (white arrows) involving the dorsal cortical oriented in the sagittal plane through the upper two third of the navicular bone.
Central injuries were dominated by lumbar pars interarticularis stress fractures. Spondylolysis is the most common identifiable cause of back pain in active adolescents.32 The isthmic variety occurs more commonly in athletes and the most common vertebral body affected is L5.33 Although a hereditary predisposition may play a role in the development of spondylolysis, physical forces are the major contributing factor. Repetitive hyperextensions for serving, or extensions and rotations for two handed backhands, place the spine at risk in tennis. As in the present cases, diagnostic delay is not uncommon. When the pain is severe or present for long enough to cause an adolescent tennis player to seek medical attention, a specific diagnostic work up should be aggressively pursued, including radiographs, MRI, CT, and SPECT.32 Although only 30–50% of cases of spondylolysis show bone healing, the majority of athletes become asymptomatic and develop no long term sequelae.17
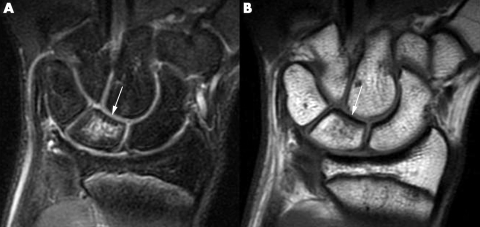
In tennis, upper limb stress fractures have been considered uncommon33,34 but injuries of the humerus,35 the distal radius,36 the distal ulna,37,38 the hamate hook39 and the second metacarpal3,40 have been reported. However, upper extremity stress fractures in elite players should not be underestimated, and accounted for 22% of all injuries in this series. The present study included two adolescent players sustaining lunate stress fractures of the dominant wrist (table 2, cases 9 and 10). The primary complaint was dorsal wrist pain during overuse of forehand strokes. Radiographs were non‐specific and MRI showed lunate bone marrow oedema in short T1 inversion recovery (STIR) and T1 weighted sequences without a fracture line (fig 4). Schmitt et al41 have reported Kienbock's disease as the most common cause of abnormal signal intensity in the lunate on MRI, followed by ulnolunate impaction syndromes and intraosseous ganglion. Lunate stress fracture should be differentiated from osteonecrosis and should be considered in the differential diagnosis in athletes complaining of dorsal wrist pain. During rehabilitation, patients were encouraged to modify their original “Western forehand grip”, which has been thought to increase hand and the wrist loading forces during tennis strokes.42 To the best of our knowledge, this is the first report of lunate stress fracture in the orthopaedic literature. Both junior players returned to pre‐injury tennis levels.
Figure 4 Case 9: grade 3 lunate stress fracture of dominant wrist. (A) Coronal DP fat suppressed image (TR1900/TE47) showing diffuse bone marrow oedema. (B) Coronal T1 image (TR519/TE14) showing hypointense signal of lunate bone marrow (white arrows), without a cortical fracture line.
What is already known on this topic
Modern competitive tennis involves powerful movements and hard training subjecting the musculoskeletal system to heavy mechanical loads
Elite tennis players are exposed to high risk of overuse injuries including stress fractures but scientific data on stress fractures in this specific population are limited
What this study adds
Tennis players have a high absolute risk of sustaining stress fractures
Male junior players seem to be the most susceptible injury risk group
The tarsal navicular, the spine, and the metatarsals are the most affected bones. This study also reports on two cases of lunate stress fractures which have not been previously published in the sports medicine literature
Ulnar wrist side overuse syndromes are common in professional tennis players. Extensor carpi ulnaris tendinopathies and complex fibrocartilage lesions are the most frequent source of ulnar sided pain, but stress fractures of the ulna have been also reported in the non‐dominant forearm of players using double handed backhands.37,38 MRI appears to be essential for accurate diagnosis; lesions are usually of low severity and resolve after a short rest period. Ulnar stress fractures have to be included as a potential cause of ulnar sided wrist pain in competitive tennis players.
Conclusions
This study is one of the few to have investigated the incidence of stress fractures in a tennis player cohort. The results show that elite tennis players have a high absolute risk of stress fractures on biannual examination. The lower extremity was more affected, but upper limb stress fractures were not uncommon. Overall, the most common bone injury sites were the navicular, the metatarsals, and the pars interarticularis. This series also included two cases of lunate stress fractures that have not been reported previously in the sports medicine literature. Junior male players involved in intense tennis training are at particular risk of sustaining stress fractures. Because competitive tennis is a sport where stress fractures are common, attention should be paid to prevention strategies such as risk factors identification and appropriate training prescription.
Footnotes
Competing interests: none declared
References
- 1.Bennel K L, Malcolm S A, Thomas S A.et al The incidence and distribution of stress fractures in competitive track and field athletes. Am J Sports Med 199624211–217. [DOI] [PubMed] [Google Scholar]
- 2.Boden B P, Osbahr D C. High‐risk stress fractures. J Am Acad Orthop Surg 20008344–353. [DOI] [PubMed] [Google Scholar]
- 3.Muramatsu K, Kuriyama R. Stress fracture at the base of second metacarpal in a soft tennis player. Clin J Sports Med 200515279–280. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg B, Pecora C. Stress fractures: a risk of increased training in freshman. Physician Sportsmed 19942268–78. [DOI] [PubMed] [Google Scholar]
- 5.Johnson A W, Weiss C B, Wheeler D L. Stress fractures of the femoral shaft in athletes –more common than expected. A new clinical test. Am J Sports Med 199422248–256. [DOI] [PubMed] [Google Scholar]
- 6.Bennel K L, Brukner P D. Epidemiology and site specificity of stress fractures. Clin Sports Med 1997162. [DOI] [PubMed] [Google Scholar]
- 7.Jones B H, Thacker S B, Gilchrist J.et al Prevention of lower extremity stress fractures in athletes and soldiers: a systematic review. Epidemiol Rev 200224228–247. [DOI] [PubMed] [Google Scholar]
- 8.Kibler W B. The 400‐watt tennis player: power development for tennis. In: Sports medicine applied to tennis, vol 2. Buenos Aires: Argentine Tennis Association, 2005129–134.
- 9.Hennekens C H, Buring J E.Epidemiology in medicine. Boston: Little, Brown and Co, 198754–98.
- 10.Anderson M W, Greenspan A. Stress fractures. Radiology 19961991–12. [DOI] [PubMed] [Google Scholar]
- 11.Maitra R S, Johnson D L. Stress fractures: clinical history and physical examination. Clin Sports Med 199716259–274. [DOI] [PubMed] [Google Scholar]
- 12.Savoca C J. Stress fractures. A classification of the earliest radiographic signs. Radiology 1971100519–524. [DOI] [PubMed] [Google Scholar]
- 13.Arendt E A, Agel J, Heikes C.et al Stress injuries to bone in collegiate athletes: a retrospective review of experience at a single institution. Am J Sports Med 200331959–969. [DOI] [PubMed] [Google Scholar]
- 14.Arendt E A, Griffiths H J. The use of MR imaging in the assessment and clinical management of stress reaction of bone in high‐performance athletes. Clin Sports Med 199716291–306. [DOI] [PubMed] [Google Scholar]
- 15.Deutsch A L, Coel M N, Mink J H. Imaging of stress injuries to bone: radiography, scintigraphy and MR imaging. Clin Sports Med 199716275–290. [DOI] [PubMed] [Google Scholar]
- 16.Steinbronn D J, Bennet G L, Kay D B. The use of magnetic resonance imaging in the diagnosis of stress fractures of the foot and ankle: four case reports. Foot Ankle Int 19941580–83. [DOI] [PubMed] [Google Scholar]
- 17.Boden B P, Osbahr D C, Jimenez C. Low‐risk stress fractures. Am J Sports Med 200129100–111. [DOI] [PubMed] [Google Scholar]
- 18.Brukner P D, Bradshaw C, Khan K M.et al Stress fractures: a review of 180 cases. Clin J Sports Med 1996685–89. [PubMed] [Google Scholar]
- 19.Iwamoto J, Takeda T. Stress fractures in athletes: a review of 196 cases. J Orthop Sci 20038273–278. [DOI] [PubMed] [Google Scholar]
- 20.Jones B H, Bovee M W, Harris J M.et al Intrinsic risk factors for exercise‐related injuries among male and female army trainees. Am J Sports Med 199321705–710. [DOI] [PubMed] [Google Scholar]
- 21.Bennel K L, Malcolm S A, Thomas S A.et al The incidence and distribution of stress fractures in competitive track and field athletes. A twelve‐month prospective study. Am J Sports Med 199624211–217. [DOI] [PubMed] [Google Scholar]
- 22.Milgrom C, Finestone A, Shlamkovitch N.et al Youth is a risk factor for stress fractures: a study of 783 infantry recruits. J Bone Joint Surg Br 19947620–22. [PubMed] [Google Scholar]
- 23.Maquirriain J. Medical approach to sports injuries in young tennis players. In: Crespo M, Pluim B, Reid M, editors. Tennis medicine for tennis coaches. International Tennis Federation 2000
- 24.Mountjoy M, Micheli L.et al IOC Medical Commission. IOC consensus statement on training the elite child athlete. www.olympics.org (searched 19 Nov 2005)
- 25.Hawley C J, Schoene R B. Overtraining syndrome. Physician Sportsmed 20033125–31. [DOI] [PubMed] [Google Scholar]
- 26.American College of Radiology ACR appropriateness criteria: stress/insufficiency fracture (excluding vertebral). Reston, VA: ACR, 1999
- 27.Froelich J W. Imaging of fractures: stress and occult. J Rheumatol 1991184–6. [PubMed] [Google Scholar]
- 28.Ammann W, Matheson G O. Radionuclide bone imaging in the detection of stress fractures. Clin J Sports Med 19911115–122. [Google Scholar]
- 29.Mink J H, Deutsch A L. Occult cartilage and bone injuries of the knee: detection, classification and assessment with MRI. Radiology 1989170823–829. [DOI] [PubMed] [Google Scholar]
- 30.Connolly L P, Connolly S A. Rib stress fractures. Clin Nucl Med 200429614–616. [DOI] [PubMed] [Google Scholar]
- 31.Burne S G, Mahoney C M, Forster B B.et al Tarsal navicular stress injuries: long term outcome and clinicoradiological correlation using both computed tomography and magnetic resonance imaging. Am J Sports Med 2005331875–1881. [DOI] [PubMed] [Google Scholar]
- 32.Moeller J L, Rifat S F. Spondylolysis in active adolescents: expediting return to play. Physician Sportsmed 20012912. [DOI] [PubMed] [Google Scholar]
- 33.Brukner P. Stress fractures of the upper limb. Sports Med 199826415–424. [DOI] [PubMed] [Google Scholar]
- 34.Sinha A K, Kaeding C C, Wadley G M. Upper extremity stress fractures in athletes: clinical features of 44 cases. Clin J Sports Med 19999199–202. [DOI] [PubMed] [Google Scholar]
- 35.Rettig A C, Beltz A F. Stress fracture in the humerus in an adolescent tennis tournament player. Am J Sports Med 19851355–58. [DOI] [PubMed] [Google Scholar]
- 36.Loosli A R, Leslie M. Stress fractures of the distal radius: a case report. Am J Sports Med 199119523–524. [DOI] [PubMed] [Google Scholar]
- 37.Rettig A C. Stress fracture of the ulna in an adolescent tournament tennis player. Am J Sports Med 198311103–106. [DOI] [PubMed] [Google Scholar]
- 38.Fragniere B, Landry M, Siegrist O. Stress fracture of the ulna in a professional tennis player using a double‐handed backhand stroke. Knee Surg Sports Traumatol Arthrosc 20019239–241. [DOI] [PubMed] [Google Scholar]
- 39.Guha A R, Marynissen H. Stress fracture of the hook of the hamate. Br J Sports Med 200236224–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bespalchuk A, Okada K, Nishida J.et al Stress fracture of the second metacarpal bone. Skeletal Radiol 200433537–540. [DOI] [PubMed] [Google Scholar]
- 41.Schmitt R, Christopoulos G, Kalb K.et al [Differential diagnosis of the signal‐compromised lunate in MRI. ] Rofo2005177358–366. [DOI] [PubMed] [Google Scholar]
- 42.Knudson D V. Factors affecting force loading on the hand in the tennis forehand. J Sports Med Phys Fitness 199131527–531. [PubMed] [Google Scholar]