Abstract
Despite more than a century of existence as a clinical entity, the true origin of ulcerative colitis still remains elusive. Several factors probably contribute to the development of this condition. Recently discovered technologies have clarified the role of bacterial species, which may account for intestinal dysbiosis, as a factor triggering ulcerative colitis. Genetic susceptibility together with abnormal innate immunoreactivity probably comprise the essential prerequisites for the initiation and perpetuation of ulcerative colitis. Although the genetic background has been more clearly recognised in patients with Crohn's disease than in those with ulcerative colitis, some candidate loci associated with ulcerative colitis have also been intensively studied. Additionally, environmental factors may interfere with inherent predispositions to ulcerative colitis, and either suppress or reinforce them. Whatever the origin, the search for the aetiology of ulcerative colitis must have the same goal: the improvement of treatment and the quality of life in patients with ulcerative colitis.
Keywords: ulcerative colitis, inflammatory bowel disease, aetiology, pathogenesis
Ulcerative colitis, together with Crohn's disease, is part of the spectrum of inflammatory bowel diseases (IBDs). It is a chronic inflammatory condition with unknown aetiology and only a partially understood pathogenesis. Starting from the rectum, the disease may affect the mucosa of the large bowel to varying lengths. A typical clinical course of ulcerative colitis consists of rectal bleeding and diarrhoea; in severe cases, however, a systemic inflammatory reaction also becomes apparent. Moreover, at least 11% of patients with ulcerative colitis have extraintestinal manifestations that include joint involvement (enteropathic arthritis), hepatobiliary disease (primary sclerosing cholangitis), and several types of eye and skin lesions.1
Worldwide, the incidence of ulcerative colitis varies greatly from 0.5 to 24.5 per 100 000 inhabitants. Both the incidence and prevalence are related to the economic situation of a country, with the lowest rates in developing countries and the highest found in North America, as well as western and central Europe. At present, the incidence of ulcerative colitis seems to be increasing in central and eastern Europe, whereas it has been stable over the past 20 years in western Europe and the Scandinavian region.2
Aetiology
Although ulcerative colitis has been known as a clinical entity since 1859, the aetiological mystery has not yet been completely revealed.3 However, the incorporation of new molecular biology techniques has yielded considerable progress in the understanding of the aetiology of ulcerative colitis.4
What is the role of the intestine's bacterial contents in ulcerative colitis?
Some of the similarities between ulcerative colitis and infectious colitides have led many investigators to search for the unidentified microorganism triggering the chronic inflammation in the large bowel. However, until now, no single microbial agent has been associated, unequivocally, with the development of ulcerative colitis. Many arguments exist against an infectious aetiology of ulcerative colitis (box 1).5
Over the past few years, we have gained considerable evidence that it is an abnormal mucosal immune reactivity, against enteric bacteria, that is the key event leading to intestinal injury in patients with IBD. Molecular biology techniques have shown that the intestinal space of an adult may contain >500 different bacterial species; some of them exert a protective role, whereas others are aggressive. The number of bacterial strains along the small bowel progressively increases, with the predominance of Gram‐negative aerobes. The bacterial population in the large bowel reaches a density of around 1012 microbes per gram of luminal contents. More than 50% of the bacterial strains cannot be cultured under conditions currently available. In adults, the faecal bacterial composition is host specific and stable over time, with small fluctuations of the strains up to 20% (box 2).6
The gut bacteria have an essential role in the development of the gut immune system, as they stimulate the lymphocytes to clonal expansion and also prevent lymphocyte apoptosis.7 Selective bacterial stimulation may occur, with Gram‐positive bacteria preferentially stimulating interleukin (IL)12 production, whereas Gram‐negative organisms induce IL4 production. Gram‐negative bacteria and lipopolysacharide are responsible for inducing oral tolerance.8
Although standard cultivation techniques are capable of detecting up to 30% of total microflora, new techniques (including analysis of bacterial 16S ribosomal RNA, polymerase chain reaction, in situ hybridisation, flow cytometry and DNA microarray or chip analysis) have markedly increased the detection rate. The beneficial bacterial strains, such as bifidobacteria and lactobacilli, are generally absent from mucosa‐associated bacterial flora in patients with active ulcerative colitis.9 On the other hand, an increased mucosal concentration of Gram‐negative anaerobes, particularly Escherichia coli, Fusobacterium varium and bacteroides, along with a high frequency of Peptostreptococcus invasion, has been shown. Various authors have also shown severe bacterial invasions of the mucosa in most colonic specimens from patients with ulcerative colitis, contrary to that in healthy controls.10,11,12,13
Box 1: Arguments against the infectious aetiology of ulcerative colitis
Lack of transmission of ulcerative colitis between patients
High incidence of ulcerative colitis in countries with a low incidence of intestinal infections
Low levels of sanitation, and consumption of unprocessed food as protective factors
Early and frequent antibiotic treatment in childhood increases the risk for ulcerative colitis
Lack of sustained efficacy of antimicrobial agents in the treatment of ulcerative colitis
Inconsistent results of stool cultivation in patients with ulcerative colitis
The high bacterial mucosal invasion in patients with IBD corresponds well with titres of immunoglobulin G to bacterial antigens. Some of these can now be used for distinguishing between ulcerative colitis (eg, anti‐Peptostreptococcus anaerobius antibody) and Crohn's disease (eg, anti I2‐from Pseudomonas fluorescens antibody or antibody to an outer membrane porin of E coli—anti‐OmpC).13,14 Nevertheless, these differences in bacterial mucosal concentrations between ulcerative colitis and Crohn's disease were not found by several investigators.
The determination of our intestinal flora was previously proposed to be partially under genetic control. Changes in the faecal flora were also found among healthy relatives of patients with IBD.15 However, the question of whether the dysbiosis in patients with ulcerative colitis is the cause or the consequence of the disease still lacks a satisfactory answer.
The role of intestinal bacteria in the aetiopathogenesis of ulcerative colitis can be summarised as follows:
Microbial flora in patients with ulcerative colitis differs considerably from that in controls, in both composition and spatial distribution (mucosal invasion).6,7
Some commensal bacterial strains exert an essential role in mucosal homeostasis and the maturation of the intestinal immune system.16
Commensal bacterial strains are required to induce chronic inflammation in genetically susceptible mice or rats, and different bacterial species have a variable ability to induce chronic intestinal inflammation in these animals.17
Evidence from intervention studies with probiotics (E coli strain Nissle 1917, VSL #3), helminths (Trichuris suis) or antibiotics (rifaximin) in patients with ulcerative colitis supports therapeutic gains from manipulation of the bacterial flora.18
Box 2: Factors modifying the intestinal bacterial profile
Western type of diet
Use of antibiotics and chemotherapeutics
Modern infant nutrition
Public health measures
High hygienic standards and sanitation
Role of epithelial cells
Over the past two decades, many abnormalities have been described in the epithelial cells of patients with ulcerative colitis (box 3). This, conceptually, is based on the anatomical distribution of inflammation, which in the case of ulcerative colitis is associated predominantly with the rectum. Why such abnormalities are seen in patients with ulcerative colitis still remains elusive. The question is whether luminal factors, autoimmunity or a genetic basis is the major contributor to the aetiology of ulcerative colitis, or whether some combination of any or all of them accounts for the development of the disease.19,20
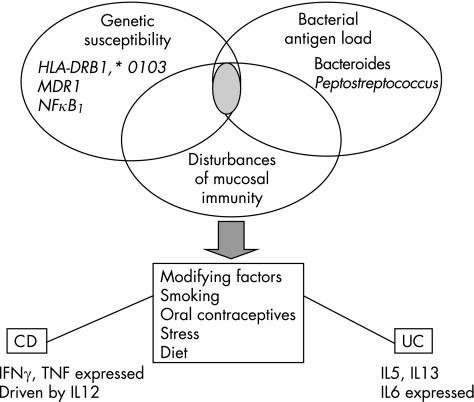
The newer approaches are focused on the interactions among epithelial cells and indigenous bacterial flora.21,22 The cells that comprise the intestinal epithelium have evolved sophisticated mechanisms for the identification of pathogens and counteractions against them, when necessary. These mechanisms include several recognition receptors with various locations on and in the cells, including toll‐like receptor (TLR) and nucleotide‐binding oligomerisation domain (NOD) receptor. Bacterial ligands binding to host cell receptors induce cellular signalling events, leading to the production of various molecules, including cytokines, eicosanoids and antimicrobial peptides. It has been hypothesised that disturbances in the recognition of molecular patterns on pathogens or commensal microflora might induce chronic and unrestricted inflammation. Members of the TLR family are variably expressed throughout the intestine and display compartmentalisation. TLRs were found to play a key part in the defence against infections by Gram‐positive bacteria and fungi. To date, 10 mammalian TLRs have been identified, responsible for recognising conserved bacterial structures. TLR4,9 encoded by gene polymorphisms is suggested to be responsible for the aetiology and pathogenesis of ulcerative colitis23 (fig 1).
Figure 1 Schematic view of the current concept of the aetiopathogenesis of ulcerative colitis and inflammatory bowel disease. Genetic susceptibility, bacterial antigens and disturbed mucosal immune response are the major factors of intestinal inflammation. Modifying factors may further serve as triggers or suppressors of the inflammation. HLA, human leucocyte antigen; IFN, interferon; IL, interleukin; MDR1, multridrug resistance gene 1; NF, nuclear factor; TNF, tumour necrosis factor; UC, ulcerative colitis.
Antimicrobial peptides are positively charged polypeptides, <100 amino acids in length, which are implicated in the microbial activity associated with phagocytes, inflammatory body fluids and epithelial secretions. Two of them, cathelicidins and defensins, exert antimicrobial effects and communicate with the host immune system, including neutrophil chemotaxis and recruitment of mastocytes. Defensins are heterogeneous peptides, which are produced by epithelial cells (α subfamily) or by Paneth cells (β subfamily).24 Substantial experimental evidence supports the important role of a deficiency of defensins in patients with Crohn's disease, and of disturbances in the secretion and harbouring of these peptides in the epithelial mucous layer in those with ulcerative colitis.25
Box 3: Abnormalities of epithelial cells in ulcerative colitis
Deficient β oxidation
Abnormal permeability of the cell membrane
Abnormal mucus composition
Abnormal cellular responses to stress
Inability to use butyrate—starving colonocytes
Polymorphisms in the toll‐like receptor gene
Deficiency of both defensins and cathelicidins
An understanding of the role of indigenous bacteria in promoting the development of healthy mucosal barrier function brings new light to the fundamental causes of ulcerative colitis. Manipulation of the intestinal microbial flora, by use of probiotics or antibiotics, may be to be a new and promising therapeutic modality in the near future.
Is ulcerative colitis an immunoregulatory disease?
Bacterial content of the gut permanently stimulates epithelial cells and the gut lymphoid tissue in both local and systemic immune responses. Close contacts between the intestinal epithelial cells and bacteria preserve homeostasis on the mucosa through the activation of an innate immunity. It is based on the rapid recognition of bacterial antigens, either by preformed membranous receptors (TLR) or by intracellular NOD family receptors. Pathogenic gut bacteria stimulate the production of pro‐inflammatory cytokines (eg, tumour necrosis factor α, interferon γ) by activating the transcription of relevant genes. In the case of invasion of non‐pathogenic microbes into the mucosa in healthy people, the regulatory cytokines (eg, transforming growth factor and IL10) are produced by immunocompetent cells. It must be emphasised that some bacterial strains (Lactobacillus, E coli strain Nissle 1917) down regulate the release of pro‐inflammatory cytokines and induce the apoptosis of activated lymphocytes.18
Epithelial cells have an important role not only in the development of innate immunity but also in the induction of memory pathways of acquired immunity. The main places where the acquired immune response takes place are at Peyer's patches and lymphatic follicles. The specialised dendritic cells transmit bacterial antigens to the lymphatic tissue to initiate the clonal expansion of T or B cells. The naive T cells then undergo differentiation into Th1, Th2 or T regulatory cells (Th3, Tr1 or CD25+ CD4+). These subpopulations of lymphocytes have markedly different effector capabilities. The major determining factor for T cells still remains to be completely elucidated.19 During the 1990s, some insights into the cell‐to‐cell mediators (cytokines) were obtained with the conception of the “Th1 and Th2 paradigm” in Crohn's disease (Th1) and ulcerative colitis (Th2). Nowadays, the reality seems to be much more complicated, and a strict differentiation between the two diseases, according to major cytokines, is far from perfect.20
The disturbances of intestinal mucosal immunity and defective interaction between commensal flora and immune compartments can lead to immunoregulatory disorders, including IBD. Owing to the high hygienic standards in developed countries, the contact between commensal bacterial flora and immunocompetent cells in the bowel is dramatically reduced in early childhood. Consequently, the loss of a tolerance to bacterial antigens may cause chronic intestinal inflammation later on. Such an explanation is called the “hygienic hypothesis”.21
Genetic background of ulcerative colitis
Increasing evidence suggests the importance of genetic susceptibility in the aetiology of IBD (box 4).
Both ulcerative colitis and Crohn's disease have a complex genetic basis, with multiple associated genes and great heterogeneity, but the genetic influence is much better recognised currently in Crohn's disease than in ulcerative colitis. Moreover, the disease phenotype is further modified considerably by gene interaction and by the influence of several external factors.
In the past decade, more than 10 genome‐wide screening and various linkage studies have delineated at least nine IBD susceptibility loci (IBD1–IBD9). Many independent studies have shown that the NOD2/CARD15 polymorphism is not linked to ulcerative colitis, whereas Crohn's disease susceptibility is increased in European and American Caucasian carriers of the NOD2/CARD15 polymorphism.26
Nevertheless, several other genes have been studied as candidate loci linked to ulcerative colitis. Experimental studies have shown that multidrug resistance gene 1 (MDR1)‐deficient mice develop colitis. Additional clinical studies showed that two polymorphs (C3435T and G2677T/C) of the MDR1 gene are associated with ulcerative colitis. The human MDR1 codes for a P‐glycoprotein that constitutes a barrier against xenobiotics. Polymorphism of this gene causes lower protein expression, and seems to be crucial in the defence against intestinal bacteria.27,28 However, other case–control studies did not confirm this finding. In the near future, outcomes of some ongoing studies on the IBD3 and IBD6 loci are expected. IBD3, located on chromosome 6p, contains the major histocompatibility complex genes. According to preliminary results, human leucocyte antigen alleles relevant to IBD seem to differ among ethnic groups (HLA‐DRB1*0103). The IBD6 locus encompasses the gene encoding integrin‐binding membrane protein, which is crucial for immune cellular adhesion and trafficking.29
Box 4: Arguments supporting a genetic basis in ulcerative colitis
Familial aggregation of ulcerative colitis (inflammatory bowel disease (IBD))
Association with rare hereditary syndromes (glycogenosis, Hermansky–Pudlak syndrome)
Similar patterns of ulcerative colitis (IBD) in family members
High incidence of ulcerative colitis (IBD) in some ethnic groups (eg, Ashkenazi Jews)
The close association between the polymorphism of members of the nuclear factor κB (NFκB) family and IBD has recently been described.30 This linkage study, focused on the polymorphism of the promoter region of the human NFκB1 gene on chromosome 4q (the most prominent member of NFκB family), which is involved in a variety of regulatory processes (including innate and adaptive immunity, cellular growth, apoptosis and cell differentiation), has also been carried out in patients with ulcerative colitis.31 The authors found an increased frequency of the −94ATTG deletion polymorphism of the NFκB1 promoter in Dutch Caucasian patients with ulcerative colitis as compared with controls. Furthermore, homozygotic patients with a −94ATTG deletion were younger at onset of ulcerative colitis than non‐homozygotic patients. The exact mechanism underlying the NFκB1‐related disease susceptibility to ulcerative colitis remains unknown. One explanation might be a poor innate immune response to bacterial antigens owing to the low level of transcriptional proteins, leading to an invasion of the bacterial strains into the mucosa and the induction of chronic inflammation. Also currently being studied intensively are the genes encoding TLR4 and TLR9 that modify responsiveness to intraluminal antigens in the gut.32 Despite all the new data mentioned above, genetic susceptibility to ulcerative colitis seems to be weaker than the genetic background of Crohn's disease. We presume, however, that the intensive genetic research on ulcerative colitis will eventually lead to an improved understanding of all aspects of the disease. Presently, clinical applications of the genetic aspects of ulcerative colitis, in contrast with, for example, bacterial flora manipulation, are not feasible.
Extrinsic factors for ulcerative colitis
Several environmental factors seem to serve as triggers of both initial presentation and subsequent relapses of ulcerative colitis.
Stress and psychological disorders
Psychoneuroimmunological studies have shown mechanisms by which behavioural factors and emotions can influence inflammation and the immune system at both the systemic and local tissue levels.33 Although ulcerative colitis was called a “psychosomatic disorder” at the beginning of the 1950s, the “renaissance” of this aspect had come up in the past. Patients with remission of IBD are shown to have a considerably increased risk of exacerbation if they exhibit high scores for depression.34 These findings are supported by experience from daily clinical practice, as well as by prospective studies suggesting that emotionally negative life events (eg, bereavement, depression or divorce) can provoke relapses of ulcerative colitis.35,36 In contrast with these findings, no study (so far) has brought forward any evidence that therapeutic manipulation reducing stress in patients with IBD notably influences the number, duration, frequency or severity of relapses of ulcerative colitis.37 Obviously, well‐designed, prospective clinical investigations, assessing the relationships between life events and ulcerative colitis patterns, are difficult to carry out.
Smoking and oral contraceptives
Ulcerative colitis predominantly affects non‐smokers and former smokers. Smoking improves the course of ulcerative colitis and decreases the need for oral steroids and the colectomy rate compared with that in non‐smokers. A meta‐analysis of several large series of patients with ulcerative colitis showed an odds ratio of 0.57 (95% confidence interval (CI) 0.38 to 0.85) for total colectomy in current smokers compared with that in non‐smokers.38 The putative mechanisms for the beneficial effect of smoking on ulcerative colitis include increased mucin synthesis, decreased production of pro‐inflammatory cytokines, reduction of smooth‐muscle tone in the gut and the modified intestinal permeability of macromolecules. The effects of nicotine and tobacco were studied experimentally as well as clinically in oral and local applications, with ambiguous results.39,40 Interestingly, the influence of cigarette smoking on both IBDs (beneficial in ulcerative colitis and harmful in Crohn's disease) has been clearly shown.
An effect of contraceptive use on ulcerative colitis is unclear. Only inconsistent data indicate that oral birth control may act as a trigger for relapses of ulcerative colitis. A meta‐analysis showed a notable, although a mild, relationship between the use of contraceptives and higher incidence of ulcerative colitis and Crohn's disease.41 At present, however, we do not have an unequivocal evidence to advise patients with ulcerative colitis against the use of oral contraceptives.
Dietary factors
A high intake of dairy products or a low intake of dietary fibre may be associated with the relapse of ulcerative colitis.42 The strongest evidence for a dietary factor is that sulphur and sulphate may be implicated in relapses of ulcerative colitis. This may be accomplished by their direct toxicity on colonocytes, and also indirectly by altering protein function and antigenicity. Another study further supports the idea that nutritional factors associated with a “modern life style” influenced the increasing frequency of IBD in the last centuries.43,44
Appendicectomy
It has been found that people who underwent appendicectomy before the age of 20 years were less likely to develop ulcerative colitis thereafter. An inverse relationship between appendicectomy and ulcerative colitis has been confirmed in a meta‐analysis of 13 case–control studies, where a pooled odds ratio of 0.31 (95% CI 0.25 to 0.38) suggested that appendicectomy at a young age provides an almost 70% reduction in the risk of developing ulcerative colitis.45 Again, the mechanisms of this prophylactic effect of appendicectomy are elusive. Some speculate that the removal of the appendix, with its abundant lymphoid aggregates, might alter the balance between the regulatory and effector T cells. This concept seems to be supported by experimental data suggesting a decreased rate of experimental colitis after resection of the caecum, and also by clinical observations showing that patients who are predisposed to ulcerative colitis might be less likely to develop appendicitis.46
Pathogenesis
The currently accepted model of the pathogenesis of ulcerative colitis is of an inappropriate immune response to host microorganisms in genetically susceptible people. The host's intestinal bacteria profoundly influence the local and systemic immune responses. The balance between homeostasis and chronic inflammation is determined by the host's genetically established immune response to luminal antigens.
A two‐component hypothesis for pathogenesis of ulcerative colitis
This hypothesis was proposed based on experimental studies showing that intestinal microorganisms in severe ulcerative colitis are pathogenic, as evidenced by allergic and immunological reactions, proved by agglutination and skin tests.47 Similar results were obtained in other intestinal diseases, which point to the existence of a non‐specific inflammation owing to intestinal microorganisms acquiring pathogenicity. Such a process may be superimposed on primary lesions of various origins, including that in the disease “inappropriately” termed ulcerative colitis.
Comprehensive clinical studies, with special attention to the periodic course of the disease, started in 1948. Till 1984, 959 cases of idiopathic proctocolitis (ulcerative colitis) were observed (compared with 303 cases of Crohn's disease).48,49,50 The population described was Czech and diagnoses were predominately made depending on clinical course, irrigography and rigid proctoscopy. Infection was excluded in every patient who had negative results for microbiological cultivation of stools. On the basis of the laboratory and clinical studies, the two‐component hypothesis was proposed in 1948,51 and developed further subsequently.52,53,54 According to the two‐component hypothesis, the primary component of the disease called ulcerative colitis presents as a haemorrhagic–catarrhal inflammation of unknown aetiology, possibly related to genetics and immunopathology, as evidenced by circulating anticolon antibodies and autoantibodies.55,56 It is a relatively mild disease, with periodic recurrences primarily affecting the rectum, with possible extension to the adjacent colon. The secondary component is superimposed on the primary lesion due to non‐specific infections by intestinal microorganisms. This is then responsible for the severe extensive ulcerative form, with local and systemic complications and sequelae. These suppress the typical periodicity and change the morphological picture of the primary process. This is the reason why advanced stages of colonic inflammations, of any nature, may have a similar ulcerative character, whereas typical histological changes are more distinct in the early stages.56
The potential weakness of this hypothesis might be the experience that patients with severe ulcerative colitis do not need antibiotics for treatment. By using this hypothesis, it is also difficult to explain the abrupt line of demarcation between normal and inflamed mucosa of the colon seen in patients with ulcerative colitis.
In view of this hypothesis, and to avoid incorrectness in and ambiguity of the term ulcerative colitis, the term idiopatic proctocolitis was proposed for the disease entity.51,53,56 This term covers both the mild haemorrhagic and the severe ulcerative form of the disease, and aptly states its main characteristics—namely, the constitutional character and predilection for association of the rectum.
“Hygiene” and “Old Friends” hypotheses
A high frequency of ulcerative colitis in the industrialised countries supports the idea that environmental factors have a dominant role in its aetiopathogenesis. The “hygiene” hypothesis states that in raising children, an extremely clean environment negatively affects the development of the immune system and, thus, predisposes them to immunologically driven diseases, such as allergy or ulcerative colitis. An important role is assigned to the helminths, because until modern times, most children were colonised by them early in life. Helminths regulate the host's immune system and prevent an excessive inflammatory reaction.57
The “Old Friends” hypothesis updates the previous hygiene theory. It is based on the assumption that changing patterns of infectious diseases might lead to an increased incidence of IBD and similar diseases. The multiple receptors of the innate immune system recognise old friends (lactobacilli, helminths, saprophytic mycobacteria and others) as harmless, as a consequence of their presence throughout mammalian evolutionary history. These antigens stimulate dendritic cells and cause their maturation. The immature dendritic cells may drive activation and exaggerated stimulation of T regulatory cells, which then induce an imbalance between Th1 and Th2 subpopulations of lymphocytes, as well as between T regulatory and T effector cells. Two methods of mucosal immunoregulation are possible. The first possibility represents the normal situation, which is characterised as a “bystander regulation”, thanks to continuous exposure to the old friends. The second possibility represents an abnormal immune response due to a lack of exposure to the old friends early in life. This immunoreaction finally acts against specific components of the gut, giving rise to chronic inflammation.58 The switch from the immunotolerance to a specific immunoreactivity, owing to inappropriate activation of innate and adaptive immunity, is a crucial moment predisposing a person to ulcerative colitis. This knowledge of the important roles of harmful (dysmicrobial) or beneficial (probiotic) intestinal contents opens new horizons for medical treatment in the future. The clinical trials, where people with active IBD were exposed to helminths (eg, T suis), can provide therapeutic gains.59,60,61
Conclusions
Despite unequivocal progress in the past 20 years in both aetiology and pathogenesis with the application of modern therapeutic approaches on ulcerative colitis, most of the fundamental questions remain unanswered. The list of fundamental unknowns includes the following.
Why does ulcerative colitis mucosal disease occur and why does the extent vary?
What are the causes of relapses of ulcerative colitis ?
Why does microscopic colitis not develop into ulcerative colitis?
At the moment, it seems unlikely that any single therapeutic approach will be universally successful in patients with ulcerative colitis in the future. The perspectives might lie in the application of individualised treatment, targeting the dominant stimulating antigen, correcting specific genetic defects, improving a destroyed mucosal barrier, eliminating luminal antigens due to manipulation with bacterial flora or delivering immunosuppressive molecules to block exaggerated mucosal immune reactivity. We hope that a wide application of probiotics, prebiotics, helminths or local antibiotics, as well as new molecules targeting pro‐inflammatory mediators and biologicals, or new promising methods (leucocytoapheresis or stem cell transplantation) could provide a greater chance for higher therapeutic successes for ulcerative colitis in the near future.
Abbreviations
IBD - inflammatory bowel disease
MDR1 - multidrug resistance gene 1
NOD - nucleotide‐binding oligomerisation domain
TLR - toll‐like receptor
Footnotes
Competing interests: None declared.
References
- 1.Cantor M, Bernstein Ch N. Clinical course and natural history of ulcerative colitis. In: Sartor RB, Sandborn WJ, eds. Kirsneŕs inflammatory bowel disease. Toronto: Elsevier, 2004280–288.
- 2.Lakatos L, Lakatos L P. Is the incidence and prevalence of inflammatory bowel diseases increasing in Eastern Europe? World J Gastroenterol 200682332–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilks S. The morbid appearance of the intestine of Miss Banks. Med Times Gazette 18592264 [Google Scholar]
- 4.Kirsner J B. Inflammatory bowel disease at The University of Chicago—early experience: a personal historical account. Inflamm Bowel Dis 200511407–416. [DOI] [PubMed] [Google Scholar]
- 5.Guarner F. Microecology as a target for therapeutic intervention in inflammatory bowel disease. Drugs 20036868–873. [PubMed] [Google Scholar]
- 6.Swidsinski A, Ladhoff A, Pernthaler A.et al Mucosal flora in inflammatory bowel disease. Gastroenterology 2003124(Suppl 1)S1370. [DOI] [PubMed] [Google Scholar]
- 7.Marteau P, Lepage P, Mangin I.et al Review article: gut flora and inflammatory bowel disease. Aliment Pharmacol Ther 200420(Suppl 4)S18–S23. [DOI] [PubMed] [Google Scholar]
- 8.Sartor R B. Microbial influences in inflammatory bowel disease: role in pathogenesis and clinical implication. In: Sartor RB, Sandborn WJ, eds. Kirsner's inflammatory bowel diseases. Toronto: Elsevier, 2004138–162.
- 9.Kleessen B, Kroesen A J, Buhr H J.et al Mucosal and invading bacteria in patients with inflammatory bowel disease compared with controls. Scand J Gastroenterol 2002371034–1041. [DOI] [PubMed] [Google Scholar]
- 10.Macfarlane S, Furrie E, Cummings J H.et al Chemotaxonomic analysis of bacterial populations colonizing the rectal mucosa in patients with ulcerative colitis. Clin Infect Dis 2004381690–1699. [DOI] [PubMed] [Google Scholar]
- 11.Tamboli C P, Neut C, Desreumax P.et al Dysbiosis in inflammatory bowel disease. Gut 2004531–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Furrie E, Macfarlane S, Cummings J H.et al Systemic antibodies towards mucosal bacteria in ulcerative colitis and Crohn's disease differentially activate the innate immune response. Gut 20045391–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okhusa T, Sato N, Ogiharo T.et al Fusobacterium varium localized in the colonic mucosa of patients with ulcerative colitis stimulates species‐specific antibody. J Gastro‐Hepatol 200217849–853. [DOI] [PubMed] [Google Scholar]
- 14.Mow W S, Vasiliauskas E A, Lin Y V.et al Association of antibody responses to microbial antigens and complications of small bowel Crohńs disease. Gastroenterology 2004126414–424. [DOI] [PubMed] [Google Scholar]
- 15.Van de Merwe J P, Schroder A M, Wensinck F.et al The obligate anaerobic fecal flora of patients with Crohn's disease and their first‐degree relatives. Scand J Gastroenterol 1988231125–1231. [DOI] [PubMed] [Google Scholar]
- 16.Sartor R B. Intestinal microflora in human and experimental inflammatory bowel disease. Curr Opin Gastroenterol 200117324–330. [DOI] [PubMed] [Google Scholar]
- 17.Guarner F. The intestinal flora in inflammatory bowel disease: normal or abnormal? Curr Opin Gastroenterol 200521414–418. [PubMed] [Google Scholar]
- 18.Borruel N, Carol M, Casellas F.et al Increased mucosal production TNF‐α in Crohn's disease can be downregulated ex vivo by probiotic bacteria. Gut 200251659–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mudter J, Neurath M. Mucosal T cells: mediators or guardians of inflammatory bowel disease? Curr Opin Gastroenterol 200319343–349. [DOI] [PubMed] [Google Scholar]
- 20.Rogler R. Update in inflammatory bowel disease pathogenesis. Curr Opin Gastroenterol 200420311–317. [DOI] [PubMed] [Google Scholar]
- 21.Rook G, Brunet L R. Microbes, immunoregulation and the gut. Gut 200554317–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gibson P R, Muir J G. Reinforcing the mucus: a new therapeutic approach for ulcerative colitis? Gut 200554900–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ismail A S, Hooper L V. Epithelial cells and their neighbors. IV. Bacterial contributions to intestinal epithelial barrier integrity. Am J Physiol Gastrointest Liver Physiol 2005289G779–G784. [DOI] [PubMed] [Google Scholar]
- 24.Mumy K L, McCormick B A. Events at the host‐microbial interference of the gastrointestinal tract II. Role of the intestinal epithelium in pathogen‐induced inflammation. Am J Physiol Gastrointest Liver Physiol 2005288G854–G859. [DOI] [PubMed] [Google Scholar]
- 25.Stange E F. Defensins in pathogenesis of IBD. Proceedings of the Annual IOIBD meeting. Bakabung, South Africa 2006
- 26.Silverberg M S, Satsangi J, Ahmad T.et al Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol 200519(Suppl A)5–36. [DOI] [PubMed] [Google Scholar]
- 27.Ho G T, Moodie F M, Satsangi J. Multidrug resistance 1 gene (P‐glycoprotein 170): an important determinant in gastrointestinal disease? Gut 200352759–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwab M, Schaffeler E, Marx C.et al Association between the C3435T MDR1 gene polymorphism and susceptibility for ulcerative colitis. Gastroenterology 200312426–33. [DOI] [PubMed] [Google Scholar]
- 29.Ahmad T, Armuzzi A, Neville M.et al The contribution of human leucocyte antigen complex genes to disease phenotype in ulcerative colitis. Tissues Antigens 200362527–535. [DOI] [PubMed] [Google Scholar]
- 30.Vermeire S, Rutgeerts P, Van Steen K.et al Genome wide scan in a Flemish inflammatory bowel disease population: support for the IBD4 locus, population heterogeneity, and epistatis. Gut 200453980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borm M E A, Van Bodegraven A A, Mulder C J J.et al A NFKB1 promoter polymorphism is involved in susceptibility to ulcerative colitis. Int J Immunogenet 200532401–405. [DOI] [PubMed] [Google Scholar]
- 32.Franchimont D, Vermeire S, El Housni H.et al Deficient host‐bacteria interactions in inflammatory bowel disease? The toll‐like receptors (TLR)‐4 Asp299gly polymorphism is associated with Crohn's disease and ulcerative colitis. Gut 200453987–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mayer E A. The neurobiology of stress and gastrointestinal disease. Gut 200047861–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mittermaier C, Dejaco C, Waldhoer T.et al Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18‐month follow‐up study. Psychosom Med 20046679–84. [DOI] [PubMed] [Google Scholar]
- 35.Bitton A, Sewitch M J, Peppercorn M A.et al Psychosocial determinants of relapse in ulcerative colitis: a longitudinal study. Am J Gastroentrol 2003982203–2208. [DOI] [PubMed] [Google Scholar]
- 36.Mawdsley J E, Rampton D S. Psychological stress in IBD. New insights into pathogenic and therapeutic manipulations. Gut 2005541481–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jantschek G, Zeitz M, Pritsch M.et al Effect of psychotherapy on the course of Crohn's disease. Results of the German prospective multicenter psychotherapy treatment study on Crohn's disease. German Study Group on Psychosocial Intervention in Crohn's Disease. Scand J Gastroenterol 1998331289–1296. [DOI] [PubMed] [Google Scholar]
- 38.Boyko E J, Perera D R, Koespell T D.et al Effects of cigarette smoking on the clinical course of ulcerative colitis. Scand J Gastroenterol 1988231147–1152. [DOI] [PubMed] [Google Scholar]
- 39.Ingram J R, Rhodes J, Ewans B K.et al Preliminary observations of oral nicotine therapy for inflammatory bowel disease. An open‐label phase I‐II study tolerance. Inflamm Bowel Dis 2005111092–1096. [DOI] [PubMed] [Google Scholar]
- 40.Sandborn W J, Tremaine W, Offord K P.et al Transdermal nicotine for mildly to moderately active ulcerative colitis: a randomized double‐blind, placebo controlled trial. Ann Intern Med 1997126364–371. [DOI] [PubMed] [Google Scholar]
- 41.Godet P G, May G R, Sutherland L R. Meta‐analysis of the role of oral contraceptives agents in inflammatory bowel disease. Gut 199537668–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fernandez‐Banares F, Hinojosa J, Sanchez‐Lombrana J L.et al Randomized clinical trial of Plantago ovata seeds (dietary fiber) as compared with mesalamine in maintaining remission in ulcerative colitis. Spanish Group for the Study of Crohn's Disease and Ulcerative Colitis (GETECCU). Am J Gastroenterol 199994427–433. [DOI] [PubMed] [Google Scholar]
- 43.Tilg H, Kaser A. Diet and relapsing ulcerative colitis: take off the meat? Gut 2004431399–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Russel M G, Engels L G, Muris J W.et al Modern life in the epidemiology of inflammatory bowel disease: a case control study with special emphasis on nutritional factors. Eur J Gastroenterol Hepatol 199810243–249. [DOI] [PubMed] [Google Scholar]
- 45.Koutroubakis I. E, Vlachonikolis IG. Appendectomy and the development of ulcerative colitis: results of a meta‐analysis of published case‐control studies, Am J Gastroenterol 200095171–176. [DOI] [PubMed] [Google Scholar]
- 46.Sandler R S, Loftus E V., Jr Epidemiology of inflammatory bowel diseases. In: Sartor RB, Sandborn WJ, eds. Kirsner's inflammatory bowel disease. Toronto: Saunders, 2004245–262.
- 47.Maratka Z, Wagner V. The treatment of non‐specific ulcerative colitis by autogenous vaccine. Correlated bacteriological and immunological studies. Gastroenterology 19481134–49. [PubMed] [Google Scholar]
- 48.Maratka Z, Spellberg M A. Observations on the clinical course of nonspecific ulcerative colitis. Gastroenterology 19491279–86. [PubMed] [Google Scholar]
- 49.Maratka Z, Nedbal J, Kocianova J.et al Incidence of colorectal cancer in proctocolitis: a retrospective study of 959 cases over 40 years. Gut 19852643–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Havelka J, Kocianova J, Maratka Z.et al Statistical analysis of 303 cases of regional enteritis [in Czech, with English summary]. Cs Gastroent Vyz 1993473–9. [Google Scholar]
- 51.Maratka Z.Colitis ulcerosa. Praha: Unie, 1948
- 52.Maratka Z. Pathogenesis and aetiology of inflammatory bowel disease. In: DeDombal FT, Myren J, Bouchier IAD, Watkinson G, eds. Inflammatory bowel disease. Oxford: Oxford University Press, 1986 (1st edn), 1993 (2nd edn)
- 53.Maratka Z. The role of intestinal bacteria in the pathogenesis of inflammatory bowel diseases. A two‐component hypothesis. Folia Gastroenterol Hepatol 200316–11. [Google Scholar]
- 54.Maratka Z, Wagner V. Recherches sur les autoanticorps anticolon au cours de la rectocolite hemorrhagique. Rev Franc Etud Clin Biol 19616182–185. [PubMed] [Google Scholar]
- 55.Maratka Z, Wagner V. On the role of the autoimmune mechanism in the genesis of ulcerative colitis. Acta Allerg 196318100–109. [Google Scholar]
- 56.Maratka Z. Differential diagnosis of inflammatory bowel diseases and the problem of so called indeterminate colitis [in Czech, with English summary]. Czech Slovak Gastroenterol Hepatol 2003578–17. [Google Scholar]
- 57.Weinstock J V, Summers R, Elliot D E. Helminths and harmony. Gut 2004537–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rook G A W, Brunet L R. Chronic inflammatory disorders, the gut and “Old Friends” hypothesis. In: Colombel JF, Scholmerich J, Vucelic B, eds. Inflammatory bowel disease: translation from basic research to clinical practice. Falk Symposium Vol 140. Berlin: Springer, 200543–58.
- 59.Summers R W, Elliott D E, Quadir K.et al Trichuris suis seems to be safe and possibly effective in the treatment of inflammatory bowel disease. Am J Gastroenterol 2003982034–2041. [DOI] [PubMed] [Google Scholar]
- 60.Ghosh S, van Heel D, Playford R J. Probiotics in inflammatory bowel disease: is it all gut flora modulation? Gut 200453620–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sheil B, McCarthy J, O'Mahony L.et al Is the mucosal route of administration essential for probiotic function? Subcutaneous administration is associated with attenuation of murine colitis and arthritis. Gut 200453694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]