Abstract
Objective
The emergence of a new generation of “point‐and‐shoot” digital cameras offers doctors a compact, portable and user‐friendly solution to the recording of highly detailed digital photographs and video images. This work highlights the use of such technology, and provides information for those who wish to record, store and display their own medical images.
Methods
Over a 3‐month period, a digital camera was carried by a doctor in a busy, adult emergency department and used to record a range of clinical images that were subsequently transferred to a computer database.
Results
In total, 493 digital images were recorded, of which 428 were photographs and 65 were video clips. These were successfully used for teaching purposes, publications and patient records.
Conclusions
This study highlights the importance of informed consent, the selection of a suitable package of digital technology and the role of basic photographic technique in developing a successful digital database in a busy clinical environment.
Keywords: digital photography, video, informed consent
Over the past 25 years, digital cameras have revolutionised the way photographs and video images are recorded. With recent improvements in small “point‐and‐shoot” digital cameras, detailed clinical images can now be recorded more quickly and more easily than ever before. This technology not only has the potential to improve documentation and diagnosis but can also “change the face of the classroom”1 by enhancing presentations and widening the dissemination of information across the world wide web. In addition, several medical specialities now use digital images in clinical trials to assess the response of patients to treatment. As practising doctors, we are privileged to witness an enormous range of clinical conditions and procedures during our working lives. Provided suitable consent is obtained, digital images of appropriate cases can be an invaluable resource to patients, relatives and health professionals alike. This paper intends to summarise 3 months of digital photography in an adult emergency department and from its findings provide information to those who wish to record, store and display their own medical images.
Methods
This study used a Sony Cybershot DSC P100 point‐and‐shoot digital camera in conjunction with a Sony Vaio VGN A115M laptop computer. Digital information was transferred from the camera via a Universal Serial Bus 2.0 port and processed through Sony Picture Package software. Adobe Photoshop 2.0 Elements and Adobe Premiere software were used to edit the images. These images were subsequently stored on a Thumbsplus database. The camera contained a 256‐MB memory card, which was capable of recording a range of 1–5 megapixel images or 6 min of continuous video footage. The camera was worn on a belt during each 12‐h shift for a 3‐month period and used to record digital photographs and video footage in an adult emergency department in Australia (fig 1). Selected images were presented to medical staff on Microsoft Office PowerPoint 2003 software at regular meetings. Any image that featured the appearance of a patient was only obtained with written consent.2 A consent form was designed for the project (Appendix 1).
Figure 1 The camera worn on a belt loop during a clinical shift.
The database created from this project was for strictly non‐commercial means and the images used solely for medical records and education.
This project was completed with ethical approval from the Human Research Ethics Committee—Eastern Section, Sydney, New South Wales, Australia.
Results
Over the course of 3 months, 428 digital photographs and 65 video clips were recorded, processed and stored on the database. Of these images, 207 contained all or part of the patient's appearance and were obtained with written consent. Table 1 presents a break‐down of these images. The remaining images included printed results and investigations of the patient, medical equipment and simulated procedures using volunteer health professionals as subjects.
Table 1 A summary of 207 clinical signs recorded during 3 months in an adult emergency department.
| Bone and soft tissue injuries | 94 (45%) |
| Including fractures, joint dislocations, tendon, ligament and muscle injuries | |
| Superficial masses and cutaneous lesions | 76 (37%) |
| Including both medical (ie, dermatological, rheumatological and endocrine) and surgical (ophthalmic, maxillofacial, ENT and general) abnormalities | |
| Examination of an abnormal system | 37 (18%) |
| Including respiratory, cardiovascular and neurological systems |
Electrocardiograms, radiographs, ultrasound scans, computed tomograms and magnetic resonance images were the most common examinations recorded. In addition, printed and handwritten information, such as phlebotomy and microbiology studies, with handwritten patient records and reports were also obtained.
Thirty two video clips and photographs of clinical procedures were recorded, and are summarised in box 1.
Discussion
At present, digital photography is widely used in clinical practice to improve documentation and direct treatment. This has applications for both acute (eg, the resolution of anaphylaxis and angioedema) and chronic (eg, treatment of burns, venous ulcers and localised cellulitis) conditions when written documentation may prove inadequate. Digital imaging also has a far wider application, informing and educating a large audience, and enhancing “the physician's ability to communicate with their peers, patients and public”.3 Until recently, conventional 35‐mm photography was used to satisfy all these requirements; however, this has often meant that doctors have had to rely heavily on the technical expertise of medical photographers and technicians to record and process the images they required.1 Such dependence has proved expensive and time consuming, and has led to a wealth of medical conditions and procedures going unrecorded in a busy clinical environment.4 Today, detailed video images and photographs can be recorded on small, lightweight cameras that can be viewed, edited and transmitted widely within minutes. This has, no doubt, encouraged the appearance of several sites on the world wide web, which display clinical images of interest to the doctor. Unfortunately, these resources have their limitations. Images can be slow and costly to download, their quality and subject matter may be limited, and issues of consent and confidentiality may remain in doubt. Although photographs are widely available on the world wide web, access to video footage is limited. Video footage of brief disorders such as transient ischaemic episodes, seizures or abnormal movements can provide an invaluable addition to a patient's medical record. Moving images can also detail rare (eg, Chvostek's sign in hypocalcaemia) or poorly understood (eg, raised jugular venous pressure) clinical signs, as well as a wide range of short procedures (eg, joint aspiration) and acute presentations (eg, calf squeeze test in a ruptured Achilles tendon), far better than a still photograph or the most eloquent textbook description. The authors of this project have found that when used with a suitable computer and compatible software, it is possible to create a comprehensive database of digital photographs and video images in a short period of time, which may well satisfy the educational and clinical needs of doctors, without having to rely on outside sources.
The experience gained from this project has led the authors to conclude that three important factors are necessary to create a successful medical images database: (1) a process for obtaining informed consent; (2) the use of appropriate technology; and (3) the successful application of basic photographic techniques. These factors are discussed in more detail.
Box 1: Examples of clinical procedures recorded as either digital photographs or video footage in the emergency department
Lumbar puncture
Basic and advanced airway management
Chest drain insertion
Manipulation of fractures and dislocations
Intra‐arterial cannulation
Joint aspiration
Central venous cannulation
Suprapubic and urethral urinary catheterisation
Application of casts
Use of a slit lamp for ophthalmic examination
Fibre‐optic endoscopy
Peripheral nerve block
Insertion of a nasogastric tube
Management of epistaxis
Peritoneal aspiration
Table 3 Important features of a digital camera in the clinical setting.
| Portable | A camera should be compact and light enough to be carried comfortably on a waistband or belt strap. A small stand, charger and an alternative memory source should also be available |
| User friendly | Recording, transferring and storing still photographs and video images should be a swift and straightforward process. Data processing should need only the most basic computing skills and all software should include a short training package for new users |
| Viewfinder and digital display | Both must be present. The digital display must be of sufficient size (minimum 3×3 cm) for the operator and participant to view photographs and video footage |
| Focus and exposure | These automatic features should be quick to adapt to a variety of lighting conditions and subjects. In addition, there should be the option to over‐ride both in certain circumstances (eg, controlling the overexposure possible when recording x rays) |
| Flash feature | All cameras should be fitted with a range of flash features, with an “anti‐red eye” function |
| Zoom | An optical zoom of ×2–3 magnitude is sufficient. This should not be confused with a digital zoom, which is part of the camera's own software and can cause the final image to become distorted |
| Macro function | This allows the camera to record images from a distance of only 10 cm from the subject, and is especially useful for images recorded through a slit lamp, microscope or fibre‐optic endoscope |
| Detail | To publish or present data, images will need to have a pixel density of ⩾200 pixels/inch. |
| Memory | A camera should be equipped with at least 256 MB of memory (either inbuilt or through a removable storage system) |
| Transfer, storage and presentation | A Universal Serial Bus (USB) connection offers the quickest and most economical way to transfer large amounts of data. Further software will be needed to edit (eg, Photoshop or Premiere), store (eg, Thumbsplus) and present (eg, PowerPoint) digital images and should be included in any database project budget |
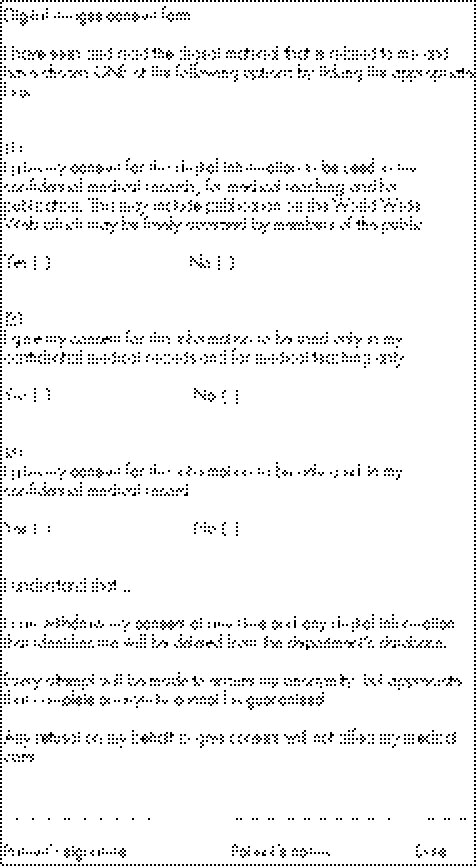
Consent
Many patients will have had considerable exposure to digital technology before their arrival at hospital. A large proportion will either have their own digital camera or will have at least featured in a digital image, whereas a few will be carrying a camera with them, usually incorporated into their mobile phone. During our research, the sight of a digital camera was often greeted with either invitations (“Go on, I've already taken a photo of it myself” or “You'll want a photo of this”) or considerable interest (“Can you show me some pictures?”). In the process of recording images, many patients suggested suitable poses or camera angles, whereas others insisted on checking each image on the digital display and altering their dress and make‐up accordingly. Several patients also showed a wider understanding of the medium by requesting copies of images to be sent to them by email. Despite large numbers of enthusiastic and informed volunteers, there will always be those who are either unwilling or unable to give suitable consent. This group may include a “potentially vulnerable population that may feel overtly or implicitly coerced” into providing consent and need very careful consideration.5 As health professionals we are obliged to ask ourselves the question, “Am I coercing this patient into providing consent?” When the answer is “yes”, it is often clear from the outset that these patients are unable to comprehend what is being asked of them. This may be due to features in a patient's presenting complaint, comorbidity or social situation, which should be identified in the early stages of a consultation. However, when the answer may seem to be “no” to the question of coercion, it is still conceivable that we might be overlooking several patients who believe that by refusing a request for consent, they may in turn receive inferior medical treatment. It is therefore vital that the patient is reassured, their symptoms controlled, and a clear plan of management described and implemented before any requests are made. To reduce the risk of coercion still further, an opportunity to withdraw consent at a later stage should be offered. The consent form devised for this project provided patients with a telephone contact, with email and postal address that allowed them an opportunity to change their consent status for up to 2 weeks after the image was recorded. Many patients will be aware of how easily digital images can be distributed across the world wide web, and may only consent to providing digital images if the results remain wholly within their confidential clinical records. By adapting a template now commonly used in a range of medical journals, we found it possible to provide a consent form that allowed patients to specify exactly how their image should be used.2 Like most medical publishers, this project sought consent from anyone whose body appeared directly in the image and emphasised the fact that anonymity and confidentiality could not be guaranteed when used outside of their medical records.
The choices made by our patients are summarised in table 2.
Table 2 Consent choices made by patients (n (%)) in this study.
| Consent for use in confidential medical records, medical teaching and publication | 190 (92%) |
| Consent for use in confidential medical records and medical teaching only | 15 (7%) |
| Consent for use in confidential medical records only | 2 (1%) |
| Refusal of consent | 7 |
Technology
Faced with an overwhelming amount of ever changing technology, the process of selecting and purchasing suitable equipment for a digital database can at first seem daunting. However, by identifying the features that are needed in clinical practice, it soon becomes possible to narrow the search for equipment and focus on a much smaller range of digital technology.
Box 2: Examples of conditions with clinical signs suitable for video recording
Ankylosing spondylitis
Bulbar and pseudo‐bulbar palsy
Cerebellar syndrome
Choreoathetosis
Cranial and peripheral nerve palsies
Ehlos Danlos syndrome
Motor neurone disease
Myasthenia gravis
Myotonic dystrophy
Ocular palsies
Parkinson's disease
Rheumatoid arthritis
Speech disorders
Systemic sclerosis
Thyroid disorders
For most of the images taken in the clinical arena, a modern point‐and‐shoot camera will be satisfactory. Although a digital single‐lens reflex camera can offer an enormous range of functions, point‐and‐shoot models are usually smaller, more affordable and easier to use. But despite these advantages, point‐and‐shoot cameras vary enormously and therefore before purchasing, it is worthwhile “test driving” several models first and to see if they satisfy the requirements listed in table 2.
Technique
Once informed consent has been obtained and suitable technology is in place, a photograph or video image can be recorded. Regardless of the technology used, it is worth bearing in mind that “good lighting, composition and photographic technique are as important as the camera”.1 Although modern editing software can contribute to the final image, much still depends on the experience and knowledge of the operator for success.
The first decision that must be made when recording images on a modern point‐and‐shoot digital camera is whether to record video footage or a still photograph. Most images, which rely on movement, such as the patient with myasthenia gravis tiring with repetitive exercises, should be recorded on video (box 2). Alternatively, stationary subjects, such as patients with skin lesions, are better suited to still photography. Despite obvious differences in subject matter, the process of recording suitable photographs or video images shares several common principles. Although a complete description of photographic techniques is beyond the scope of this article, it is possible to outline many points that should be considered when obtaining an image in the clinical environment. Above all, the photograph or video clip image should always be kept as simple as possible. The subject should be well lit and in focus, and the background should primarily act as a means of drawing attention towards the subject. This can be done in several ways. Contrasting colours, patterns and textures can all add emphasis to the subject of an image. In most clinical settings, a rich source of backgrounds is available, ranging from the patient's own clothes and belongings to fluorescent spinal boards and surgical towels found in an emergency department. Alternatively, straight lines can be used, such as walking sticks, frames or limbs, which provide “pointers” to the viewer, drawing the eye to the subject of the image.
When we glance at an image, most of us tend to be drawn towards its centre. By placing the subject of this image outside this area, the viewer is forced to spend more time studying the image. This can transform a “spot diagnosis”, which may hold the attention of the viewer for only a few seconds, into an image that forces the viewer to spend time finding the subject and absorbing the other details present in the image.
The use of balance is also important. By placing both hands of a patient with severe rheumatoid arthritis in a photograph, the severity of the condition is highlighted and forces the viewer to ask questions. How does the patient hold his walking frame? How does he roll up his sleeves? How does he put on his spectacles? Balance is also useful when comparing healthy and affected areas. These can be subtle, such as those seen in Horner's syndrome, or can provide a scale to much larger abnormalities such as joint arthrosis, dislocations or displaced fractures. The importance of balance is also important in a video recording. The positive Homan's Sign of a patient with a ruptured Achilles tendon is much clearer if a normal examination is also displayed. In conditions where it is impossible to compare affected and normal anatomy simultaneously, a fascinating story may emerge from a series of recordings made over the course of treatment. The successful treatment of a patient with asthma, or the use of a Hallpike manoeuvre for benign positional vertigo, can be recorded regularly over the course of treatment and may prove to be invaluable for all concerned. In other cases where it is not possible to record a comparison, it may be worthwhile placing a measuring device such as a ruler or tape measure alongside the affected area to highlight the extent of the abnormality. Alternatively, it is useful to have a collection of “normal” images. Normal radiographs, computed tomograms and ultrasound scans are invaluable when describing subtle changes to colleagues or to those who may be unfamiliar with the signs you wish to show.
Once the subject of the image has been decided, the photographer should record as many images as possible, varying the camera's position, exposure and focus, to obtain a range of different images. By varying the camera position, the operator will soon discover a host of interesting angles from which to view the subject, whereas altering the exposure (and use of the flash) will attempt to overcome the persistent problem of poor lighting in the clinical environment. Naturally, this will all take place in the usual clinical time restraints. However, with experience and experimentation, this process can soon be carried out quickly and efficiently.
Conclusion
Since the emergence of the first commercial electronic camera in 1981, digital photography has been embraced by medical professionals and the general public alike. “Point‐and‐shoot” cameras can now provide detailed photographs and video footage, which can be used by doctors to not only improve patient care but also change the way in which they communicate with the wider medical community. However, it is of crucial importance that this equipment is used appropriately and that voluntary, and informed consent is obtained from identifiable patients. Clearly, there is no place for a digital image if it risks compromising the privacy and autonomy of patients or their relationship with health professionals.
Main points
Digital images cannot only improve documentation and direct treatment but can also improve communication between health professionals and patients.
In the clinical environment, a digital camera needs to be portable, lightweight and user friendly.
Modern “point‐and‐shoot” digital cameras are suitable for recording detailed photographs and video images in clinical practice.
Appendix 1
Footnotes
Competing interests: None.
References
- 1.Chan L, Reilly K M. Integration of digital imaging into emergency medicine education. Acad Emerg Med 2002993–95. [DOI] [PubMed] [Google Scholar]
- 2.Hood C A, Hope T, Dove P. Videos, photographs and patient consent. BMJ 19983161009–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prasad S, Roy B. Digital photography in medicine. J Postgrad Med 200349332–336. [PubMed] [Google Scholar]
- 4.Johnson D, Johnson M. Digital video. Clin Orthop Relat Res 200442117–24. [DOI] [PubMed] [Google Scholar]
- 5.Marco C A, Larkin G L, Silbergleit R. Filming of patients in academic emergency departments. Acad Emerg Med 20029248–250. [DOI] [PubMed] [Google Scholar]
- 6.Andres B M, Khanna J, Wenz J F.et al A comparison of digital cameras – features essential for the orthopaedic surgeon. Clin Orthop Relat Res 200442110–16. [PubMed] [Google Scholar]