Abstract
We describe a case of a patient receiving warfarin who presented with a superior pubic ramus fracture after a trivial fall at home. She developed a massive retroperitoneal haematoma as a result of vascular injury and subsequently died. This case emphasises the importance of admitting and observing patients with pubic rami fractures who are receiving antithrombotic treatment, and haemorrhage should be considered if they become haemodynamically compromised.
No reports are available of a pubic ramus fracture after a simple fall causing massive uncontrolled haemorrhage. The association between unstable pelvic fracture and haemorrhage is clear, and the effectiveness of percutaneous angiographic embolisation has been shown.1 However, this is usually in unstable fractures after high‐energy trauma.
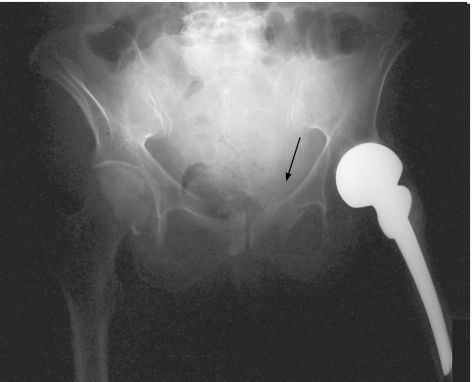
A 71‐year‐old woman was brought to the Accident and Emergency Department, Glasgow Royal Infirmary, Glasgow, UK, after a simple fall at home where she had tripped and landed on her left side. On arrival in the emergency department, she presented with hip pain on the left side. She had a history of deep‐venous thrombosis and pulmonary embolism for which she was given warfarin as an anticoagulant. She also had chronic obstructive airway disease, pulmonary hypertension and osteoporosis and had undergone left hip hemiarthroplasty after a fractured neck of the femur 2 years previously. On examination, her blood pressure was 140.95 mm Hg and her heart rate was 84 beats/min. The patient was tender in her left groin and had a decreased range of left hip movement but no neurovascular deficit to the leg. Her abdomen was soft and non‐tender, and she had no abdominal swelling. A radiograph of the pelvis showed a minimally displaced, stable fracture of the left superior pubic ramus (fig 1). A blood test showed a haemoglobin concentration of 13.2 g/dl, international normalised ratio of 2.2, and normal urea and creatinine levels. The patient was unable to move with a walking aid and was admitted for pain relief and rehabilitation.
Figure 1 Radiograph of the pelvis showing a fracture (arrow) of the left superior pubic ramus and a left hemiarthroplasty in situ.
Shortly after arrival in the ward, she developed suprapubic swelling. A provisional diagnosis of acute urinary retention was made; however, catheterisation produced a residual volume of only 150 ml of urine. Further examination showed that she had tachycardia and hypotension with increased abdominal swelling and had developed bruising in the periumbilical, groin and perineal regions. Her haemoglobin concentration was 6.3 g/dl. Blood transfusion was started and anticoagulation was reversed by using 3 units of fresh frozen plasma and 10 mg vitamin K. A contrast‐enhanced computed tomography showed a large retroperitoneal haematoma suggesting active bleeding in the pelvis. The haematoma was causing left‐sided ureteric obstruction. Emergency percutaneous transluminal angiography was carried out and this showed extravasation from a small pelvic artery. Initially this was believed to be an anterior branch of the internal iliac artery, which was then embolised with a stainless‐steel coil. Post‐embolisation angiogram showed that bleeding continued. This was identified as arising from the pubic branch of the left inferior epigastric artery. This vessel was selectively catheterised and embolised by using coils. This successfully stopped the pelvic bleeding. By this stage, she had been transfused with 10 units of packed red cells.
Angiography was carried out through the right femoral artery using a 12F gauge cannula. A “perclose” haemostat device was used before removing the sheath; nevertheless, the patient started to bleed profusely from the cannulation site in her right groin. Urgent exploration of the femoral artery under local anaesthesia showed a laceration in the superficial femoral artery, which was repaired using a 5‐0 non‐absorbable monofilament suture, and haemostasis was achieved.
The next day the patient developed respiratory failure, and a diagnosis of adult respiratory distress syndrome was made. She also developed acute renal failure, which was believed to be secondary to a combination of prolonged hypotension, large intravenous contrast exposure and unilateral ureteric obstruction. After anaesthetic assessment, it was thought that, in view of her history of pulmonary hypertension and compromised lung function, she was not an appropriate candidate for assisted ventilation. She was treated with oxygen therapy and intravenous fluids. She died from respiratory failure 48 h after admission.
Key points
Patients with pubic rami fractures who are receiving antithrombotic treatment should be admitted for observation.
Major pelvic bleeding should be considered if these patients become haemodynamically compromised.
Bleeding can be successfully controlled by angiography and embolisation, as with major pelvic fractures.
Discussion
Osteoporotic fractures of the pubic rami that occur after low‐energy injury are common in elderly people, with an incidence of 25.6 per 100 000 people per year in those aged >60 years.2 This type of injury is usually treated conservatively and with active mobilisation once the acute pain has settled.
In a thorough review of the literature, we could find no cases of life‐threatening haemorrhage after an isolated pubic ramus fracture due to a simple fall in an elderly person. There have been two case reports of isolated pubic rami fractures in young patients after high‐energy road traffic accidents that caused major pelvic bleeding.3,4
There has been one documented case of massive extraperitoneal haemorrhage after soft‐tissue trauma to the pelvis in an elderly patient who fell out of bed.5 The vessel responsible, as in the present case, was the pubic branch of the inferior epigastric artery, and it is believed that the vascular injury occurred as a result of the vessel being crushed against the pectineal ligament. The pubic artery descends close to the femoral ring behind the pubis and anastomoses with the pubic branch of the obturator artery. This is an anastomosis between the internal and the external iliac arteries and highlights why, in the present case, two different vessels required embolisation.
Antithrombotic agents account for many admissions to hospital owing to bleeding complications. In a recent study of 18 820 hospital admissions, it was found that warfarin accounted for 10.5% of admissions and the deaths of three patients.6 It is also accepted that the risk of bleeding complications during treatment with warfarin is related to the intensity of treatment with anticoagulants and deviation in the prothrombin time ratio.7 The retroperitoneal haemorrhage in our patient was probably compounded by her receiving anticoagulants.
References
- 1.Cook R E, Keating J F, Gillespie I. The role of angiography in the management of haemorrhage from major fractures of the pelvis. J Bone Joint Surg Br 200284178–182. [DOI] [PubMed] [Google Scholar]
- 2.Hill R M, Robinson C M, Keating J F. Fractures of the pubic rami. Epidemiology and five year survival. J Bone Joint Surg Br 2001831141–1144. [DOI] [PubMed] [Google Scholar]
- 3.Grainger M F, Porter K M. Life threatening haemorrhage from obturator vessel tear as a result of pubic ramus fracture. Injury 200334543–544. [DOI] [PubMed] [Google Scholar]
- 4.Perez H, Alcover H. Hypovolaemic shock due to a fracture of the superior pubic ramus in a young man. Injury 20043580–82. [DOI] [PubMed] [Google Scholar]
- 5.Wilson C J, Edwards R. Massive extraperitoneal haemorrhage after soft tissue trauma to the pubic branch of the inferior epigastric artery. J Trauma 200048779–780. [DOI] [PubMed] [Google Scholar]
- 6.Pirmohamed M, James S, Meakin A. Adverse drug reactions as a cause for admission to hospital: prospective analysis of 18 820 patients. BMJ 200432915–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fihn S D, Callahan C M, Martin D C. The risk for and severity of bleeding complications in elderly treated with warfarin. The National Consortium of Anticoagulation Clinics. Ann Intern Med 199624970–979. [DOI] [PubMed] [Google Scholar]