Abstract
Tako‐tsubo cardiomyopathy is a cardiac syndrome precipitated by profound emotional stress and anxiety, particularly in middle‐aged women. It presents as a mimic of acute myocardial infarction, but coronary angiography shows normal coronary arteries and a characteristic left ventriculogram resembling an “octopus pot”. The condition seems to have a favourable prognosis. Initially described in Japan, and with many names in the literature, it is being increasingly recognised in the West owing to early coronary angiography and primary coronary intervention, accounting for up to 1 in 30 primary cases of angioplasty in some institutions. A typical case is described, and the clinical features, pathophysiology and management reviewed.
Acute psychological and emotional stress can precipitate acute myocardial infarction (AMI), but also a variant mimicking AMI, with reversible left ventricular (LV) dysfunction and normal coronary arteries at angiography. So called “tako‐tsubo cardiomyopathy”, also known as “apical ballooning syndrome”, “ampulla cardiomyopathy”, “stress cardiomyopathy” or “broken‐heart syndrome” was initially reported in Japan,1 but is now increasingly recognised in the West,2,3 owing to the increasing availability of primary coronary angioplasty. “Tako‐tsubo”—literally “octopus pot”— is a Japanese fishing octopus trap, and describes the characteristic shape of the left ventricle seen in this syndrome. With increasing availability of primary coronary angioplasty, tako‐tsubo cardiomyopathy is an important differential of AMI. Clinicians need to understand and recognise this syndrome.
Case report
A 71‐year‐old woman was admitted for the management of a relatively uncommon form of primary headache—short‐lasting unilateral neuralgiform headache attacks with conjuctival injection and tearing (SUNCT).4 As part of her treatment, a continuous lidocaine infusion was started at 15 mg/h, which provided considerable relief of symptoms.5 An initial electrocardiogram (ECG) and echocardiogram were normal. Cardiovascular risk factors included a positive family history and cholesterol of 5.2 mmol/l.
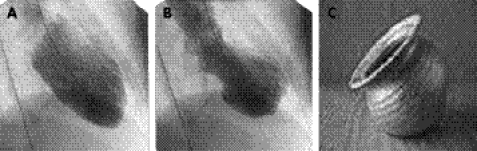
After 7 days, in preparation for discharge, the lidocaine infusion was stopped. After this, the pain returned and the patient became extremely anxious and frightened,6 and developed severe central crushing chest pain without haemodynamic compromise. An ECG showed an acute anterolateral ST segment elevation myocardial infarction, and the patient was transferred for primary angioplasty. At angiography, the epicardial coronary arteries were normal, but both the circumflex and left anterior descending arteries had sluggish flow. A left ventriculogram showed characteristic mid to apical hypokinesis of all walls (apical ballooning), with marked hyperkinesis of the basal left ventricular segments (fig 1). The left ventricular end‐diastolic pressure was raised at 25 mm Hg (normal range 5–12 mm Hg). The diagnosis of tako‐tsubo cardiomyopathy was suspected. She was treated medically as for an acute coronary syndrome with aspirin, low‐molecular‐weight heparin, angiotensin‐converting enzyme (ACE) inhibitor, analgesia and supportive therapy. An echocardiogram on day 1 showed impaired left ventricular function, with an ejection fraction of 25%. The peak troponin T concentration was 0.49 µg/l (normal reference <0.01 µg/l) and creatinine kinase was 125 IU/l (normal reference 25–170 IU/l). Over the next 4 days, there was no further chest pain, and the ECG normalised. She was discharged on day 5, and a repeat echocardiogram on day 10 was entirely normal.
Figure 1 (A) The left ventricular angiogram showing left ventricle in diastole. (B) In systole the base of the heart is hyperkinetic, and the apex is hypokinetic, mimicking an octopus pot. (C) “Tako‐tsubo” is Japanese for “octopus pot”, a round‐bottomed, narrow‐necked pot used to catch octopus.
Discussion
This case describes a classic case of tako‐tsubo cardiomyopathy. The patient was a postmenopausal woman presenting with an AMI precipitated by a period of profound stress and anxiety. The coronary arteries were normal at angiography, but the left ventricle showed a characteristic pattern of severe apical dysfunction, which recovered completely within 10 days.
Tako‐tsubo cardiomyopathy accounts for 1% of admissions for suspected AMI in Japan,7 but is now increasingly recognised in the West owing to primary coronary intervention, accounting for up to 1 in 30 cases of primary angioplasty.2,3 Patients, commonly postmenopausal women, present with chest pain or dyspnoea after profound psychological stress. Initial ECG changes range from ST segment elevation, T wave inversions, new‐onset bundle branch block or new, sometimes transient, Q waves. Angiography shows normal epicardial coronary arteries, but often slow flow. Any release of cardiac enzymes is smaller than the initial extent to which left ventricular wall motion abnormalities would predict. A striking hallmark of this syndrome is the characteristic left ventricular dysfunction, characterised by apical hypokinesia with basal hyperkinesis, giving the left ventricle its characteristic “tako‐tsubo” shape. Provided the patient survives the initial period, there is rapid and complete resolution of left ventricular dysfunction within days to weeks.8
The mechanisms underlying tako‐tsubo cardiomyopathy are unclear, but catecholamine excess has been implicated. Unlike classic AMI, the distribution of primary cardiac insult does not correspond to the perfusion territory of a single coronary artery, and there is myocardial stunning rather than infarction. Patients usually have supraphysiological levels of plasma catecholamines and stress‐related neuropeptides. Multivessel epicardial coronary artery spasm has been reported, but microvascular spasm has also been suggested. Alternatively, catecholamines could directly affect myocytes via cyclic‐AMP‐mediated calcium overload or free‐radical generation. Such proposed explanations do not fully explain the characteristic myocardial distribution. It is of interest that the apical myocardium has a higher adrenoceptor density than elsewhere.9
Features of tako‐tsubo cardiomyopathy
Acute psychological stress before the onset of chest pain or dyspnoea.
Ischaemic changes on the electrocardiogram (usually ST segment elevation or T‐wave inversion).
Normal epicardial coronary arteries, but there may be slow flow.
Apical ballooning with basal hyperkinesis on the left ventriculogram.
Cardiac enzyme release less than the extent to which left ventricular dysfunction would predict.
Rapid resolution of left ventricular dysfunction (days to weeks).
When suspected, patients are probably best managed initially, as for AMI, by urgent coronary angiography with a view to primary coronary intervention. After excluding significant coronary artery disease, an appropriate approach is to use aspirin, low‐molecular‐weight heparins, ACE inhibitors, possibly β‐blockers and diuretics if necessary. Patients should be monitored for the development of arrhythmias, heart failure and mechanical complications. Acute haemodynamic support, either with an intra‐aortic balloon pump or inotropes, may be necessary in the short term. Apical thrombus can form, and short‐term anticoagulation may be needed.5 One report suggests that this syndrome may recur in up to 10% of patients, making it difficult to know how long to continue treatment.10
One intriguing aspect of the presented case is the occurrence after the withdrawal of intravenous lidocaine. We speculate that lidocaine may have “anaesthetised” the cardiac mechanoreceptors and chemoreceptors (endoanaesthesia), causing a rebound tachyphylaxis phenomenon preferentially in the afferent sympathetic pathway, potentiating the emotional stress‐induced sympathetic stimulation. An extensive case series indicates that the pain of SUNCT can be extremely severe,11 such that the pain and distress of the SUNCT recurrence after cessation of lidocaine may be sufficient to trigger substantial catecholamine release.
This case emphasises the importance of psychological stress as a trigger for myocardial dysfunction. Although catecholamine‐induced myocardial stunning may be the underlying mechanism, a more complete understanding of its pathogenesis requires future research. Given the transient nature of the dysfunction, and increasing availability of early coronary angiography and primary coronary intervention, this syndrome will become increasingly recognised. Although treatment options are currently empirical, patients mainly seem to have a favourable prognosis.
Learning points
Tako‐tsubo cardiomyopathy is a cardiac syndrome, precipitated by profound emotional stress and anxiety, initially mimicking, and hence an important differential of, acute myocardial infarction.
The diagnosis should be suspected at coronary angiography, which shows normal epicardial coronary arteries, with a characteristic left ventriculogram resembling an “octopus pot”.
Tako‐tsubo cardiomyopathy is becoming increasingly recognised in the West owing to increasing availability of primary coronary intervention and early coronary angiography.
Clinicians need to understand and recognise this syndrome, as patients seem to have a favourable prognosis.
Abbreviations
ACE - angiotensin‐converting enzyme
AMI - acute myocardial infarction
ECG - electrocardiogram
SUNCT - short‐lasting unilateral neuralgiform headache attacks with conjuctival injection and tearing
Footnotes
Competing interests: None.
References
- 1.Dote K, Sato H, Tateishi H.et al Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol 199121203–214. [PubMed] [Google Scholar]
- 2.Seth P S, Aurigemma G P, Krasnow J M.et al A syndrome of transient left ventricular apical wall motion abnormality in the absence of coronary disease: a perspective from the United States. Cardiology 200310061–66. [DOI] [PubMed] [Google Scholar]
- 3.Desmet W J, Adriaenssens B F, Dens J A. Apical ballooning of the left ventricle: first series in white patients. Heart 2003891027–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.A Headache Classification Committee of The International Headache Society The international classfication of headache disorders (second edition). Cephalgia 200424(Suppl 1)1–160. [Google Scholar]
- 5.Matharu M S, Cohen A S, Goadsby P J. SUNCT syndrome responsive to intravenous lidocaine. Cephalgia 200424985–992. [DOI] [PubMed] [Google Scholar]
- 6.Gil‐Gouveia R, Goadsby P J. Neuropsychiatric side effects of lidocaine examples from the treatment of headache and a review. Cephalgia. 2006;26. In press [DOI] [PubMed]
- 7.Tsuchihashi K, Ueshima K, Uchida T.et al Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina pectoris‐myocardial infarction investigations in Japan. J Am Coll Cardiol 20013811–18. [DOI] [PubMed] [Google Scholar]
- 8.Bybee K A, Kara T, Prasad A.et al Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST‐segment elevation myocardial infarction. Ann Intern Med 2004141858–865. [DOI] [PubMed] [Google Scholar]
- 9.Wittstein I S, Thiemann D R, Lima J A.et al Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005352539–548. [DOI] [PubMed] [Google Scholar]
- 10.Sharkey S W, Lesser J R, Andrey G.et al Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation 2005111472–479. [DOI] [PubMed] [Google Scholar]
- 11.Cohen A S, Matharu M S, Goadsby P J. Revisiting the International Headache Society Criteria for SUNCT: a case series of 52 patients. Cephalgia 2005251194 [Google Scholar]