Abstract
Despite rapidly increasing incidence rates of breast cancer, recent immigrants such as Korean-American (KA) women report disproportionately lower utilization of screening tests compared with other ethnic groups. Early screening of breast cancer for this population may be greatly facilitated by indigenous lay health workers (LHWs). We conducted an intervention trial with a 6-month follow-up. Trained LHWs recruited 100 KA women 40 years of age or older who had not had a mammogram during the past 2 years. Ninety-three completed follow-up questionnaires. A 120-min, in-class education combined with LHW follow-up counseling and navigation assistance through the health care system was provided. Rates of breast cancer screening behaviors significantly increased at 6 months (P < 0.001); changes between pre- and post-intervention were 31.9% for mammography, 23% for clinical breast examination and 36.2% for breast self-examination. Modesty toward screening significantly decreased over time, but we did not find any significant differences in breast cancer knowledge and beliefs before and after the intervention. Results support the efficacy of this neighborhood-based, culturally sensitive intervention. Further research should seek to replicate these findings and to incorporate more self-care skills such as health literacy when designing an intervention program for linguistically and culturally isolated immigrant women.
Introduction
Breast cancer is the most common type of cancer and one of the leading causes of death among women aged 20 years and older in the United States [1]. While Asian-American women tend to have lower breast cancer incidence rates than non-Hispanic Whites [2], studies have reported a rapidly changing shift toward increased risk for breast cancer among Asian-American women [3–6]. For example, data analysis from the Los Angeles Cancer Surveillance Program (1993–97) showed an annual increase of 6.3% for Asian-American women over age 50 compared with 1.5% for non-Hispanic Whites [3]. Data from the 1988–99 California Cancer Registry also revealed that Asian women experienced the steepest increase in the incidence of breast cancer compared with other ethnic groups [7, 8]. Furthermore, some Asian groups with a larger percentage of immigrants appear to be more likely to receive a diagnosis at a later stage than non-Hispanic white women. For example, data from the Surveillance, Epidemiology and End Results Program [9] have shown that Korean-American (KA) women were 60% more likely than non-Hispanic white women to have tumors ≥1 cm at diagnosis.
Early detection of breast cancer through regular mammograms can reduce breast cancer mortality by up to 30% [10]. Although significant progress has been made nationally in breast cancer screening, considerable efforts still need to be made toward achieving uniformly high rates of screening across ethnic groups. According to data from the 2001 Behavioral Risk Factor Surveillance System, the mean percentage of US women aged 40 years and older who had a mammogram during the preceding 2 years was 74.4% [11]. In comparison, several studies [12–16] have reported disproportionately lower mammography screening among Asian women, with rates between 25 and 56%. Within the Asian subgroups, KA women were found to have consistently lower screening rates, ranging from 25% in convenience sample studies [16] to 34–47% in population-based studies [12, 13]. In addition, KA women were the least likely to report ever having had a mammogram than women in other Asian groups [17–19].
To promote screening for breast cancer in this population, we constructed and tested a lay health worker (LHW) intervention called ‘Better Breast Health for KA Women'. The use of indigenous LHWs has been associated with improved cancer screening behaviors in hard-to-reach ethnic minority communities as a culturally sensitive and linguistically appropriate strategy [20–25], though such an approach has rarely been applied to an Asian community [26–29]. To our knowledge, this is one of the first studies to have implemented and evaluated the effect of a LHW intervention to promote breast cancer screening among KA women who are predominantly first-generation immigrants [30]. This study tested the hypothesis that in comparison to baseline, after receiving a comprehensive intervention through in-class education, follow-up counseling and navigation assistance through the health care system from trained bilingual LHWs, KA women would show (i) increased rates of ever having had a mammogram, clinical breast examination (CBE) and breast self-examination (BSE); (ii) increased levels of perceived susceptibility to and benefits of breast cancer screening and breast cancer knowledge (BCK) and (iii) decreased levels of perceived and other culturally specific barriers (e.g. modesty, utilization of oriental medicine) to breast cancer screening.
Methods
Sample
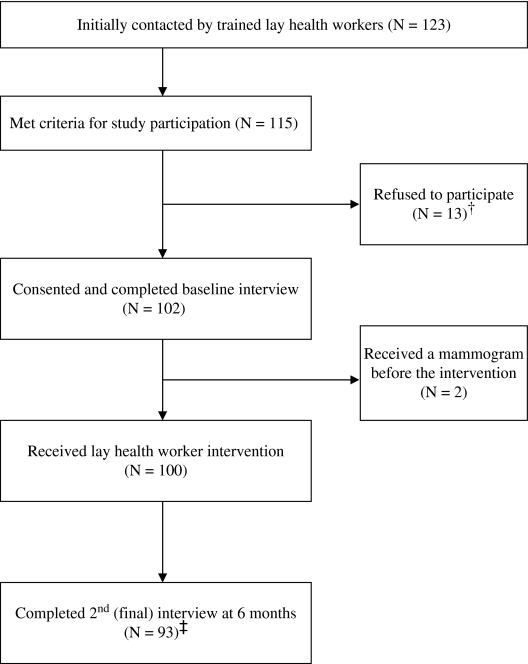
Participants were recruited by trained LHWs. Eligible KA women (i) were 40 years of age or older, (ii) had not had a mammogram during the past 2 years (being non-adherent) and (iii) had no history of breast cancer. Histories of mammogram receipt and breast cancer were determined by self-reports. LHWs initially made contact with 123 KA women and successfully recruited 115 eligible participants, with each enrolling 4–17 women. Of those who initially agreed to participate in our study, 13 dropped out before the education session began for a variety of reasons (e.g. change of mind, travel, moving and schedule conflict). In addition, two women received a mammogram before the intervention began. As a result, our intervention was delivered to a total of 100 participants (Fig. 1).
Fig. 1.
Participant tracking. †Reasons for refusal: change of mind (n = 8), moving (n = 1), travel (n = 1), already scheduled a mammogram (n = 1), schedule conflict (n = 1) and no reason (n = 1). ‡Reasons for dropping: lost contact (n = 4), schedule conflict (n = 2) and travel (n = 1).
Procedure
Study protocol was approved by the Institutional Review Board. The study consisted of three phases: construction of LHW intervention materials in both English and Korean, recruiting and training of LHWs and pilot testing of the intervention. In an attempt to integrate the information and advice derived from previous work regarding beliefs, attitudes and experiences regarding cancer screening among KA women and our community partners, it was important for us to address the following cultural and structural characteristics when developing our intervention: (i) KA women are not fluent in English, making screening appointments or receiving appropriate medical care difficult [31]; (ii) as is true for other groups of Asians with recent immigration history (e.g. Chinese and Vietnamese), many KA women have not been exposed to the notion of disease prevention and adopt a crisis-oriented system of care in which preventive medicine is often ignored [32, 33]; (iii) KA women are often forced to assume increased responsibility when the family immigrates to the United States since they now find the need to join the workforce, all the while carrying the traditional nurturing and supporting roles in the family. As a result, health is the lowest priority for many KA women [34] and (iv) some KA women demonstrate modesty and think the topic is embarrassing to discuss [35]. Together, these factors suggested that the content of educational messages be guided by the culture and belief of KA women and that adequately trained LHWs may be the most effective interventionists in the community, because they internalize health education messages, delivering this information directly to their community members in the language that they can easily understand [36]. We then reviewed the intervention materials at a series of weekly community–academic partner team meetings held at our community partner site (the Korean Resource Center) and finalized the materials by consensus among team members.
Upon completion of the intervention protocol, we recruited LHWs through ethnic newspaper advertisements, recommendations from ethnic church leaders and word of mouth. Since the key to our intervention was LHWs, identified individuals were interviewed by project staff about their characteristics (e.g. being dedicated, bilingual, flexible and time availability). Recruited LHWs (N = 20) participated in our 2-day training (16 hours) following our LHW manual specially designed to guide the in-class education using flip charts and individualized follow-up counseling in the topic focus of the intervention. The LHWs were all female, in their late 40s to early 60s, with at least a high school education. None of the LHWs had worked in the area of breast cancer. Of these, 18 completed the training (two quit before completion because of time conflict and a health problem). Two trainers independently rated LHW skills, using a LHW competency evaluation form developed for the study based on the core competency areas identified by the Department of Health Education of the State of California [37]. These areas included client intake (e.g. participant orientation to the study), group presentation (e.g. using examples), care coordination (e.g. providing referrals and information) and one-on-one health advising (e.g. identifying and prioritizing needs). Observational ratings by two independent trainers indicated that the LHWs' overall performance was satisfactory, with a total item mean of 2.86 (71.5% on a 100-point scale). Of the 18 LHWs who completed the training, seven dropped out before recruitment started for reasons including lack of time (n = 3), finding a new job (n = 3) and change of mind (n = 1). The remaining 11 LHWs enrolled 100 eligible KA women through their social networks, with each recruiting 4–17 women, and administered the baseline study questionnaires and delivered the intervention.
Intervention
Construction of the intervention was guided by the transtheoretical model (TTM) and the health belief model (HBM). The TTM [38] proposes that people move through a series of progressively more committed stages of adoption when modifying a health-related behavior (i.e. screening behavior). Following the lead of experts in the area of breast cancer screening, we defined stage of adoption as following: pre-contemplation (not thinking about getting a mammogram in the next 6 months), contemplation (thinking about getting a mammogram in the next 6 months), action (having had a mammogram within the last 12 months) and maintenance (being adherent with mammograms for the past 2 years) [39, 40]. Several researchers have noted that stage-matched tailored intervention can be more effective in encouraging mammography screening [41, 42].
The HBM [42] describes how behavioral change is determined by several interacting components. The fundamental premise is that individuals will screen for an ill-health condition (e.g. cancer) if they recognize a threat. In this study, HBM variables were not used as predictors. Rather, the model provided the basic concepts for an effective intervention program to bring about the desired behavioral changes such as breast cancer screening. These include (i) an increase in perceived susceptibility, (ii) an increase in perceived benefits, (iii) a decrease in perceived barriers and (iv) a cue to action, such as a reminder for screening appointments.
The 2-hour education sessions were held at a variety of community sites, including a community center, ethnic churches, ethnic grocery stores and the participants’ homes. Using flip charts with specific talking points, LHWs delivered the same core curriculum every time to KA women (see Table I), aiming to (i) enhance knowledge of breast cancer and screening methods, (ii) introduce specific steps to obtain a mammography and (iii) promote self-care behaviors for breast health such as BSE.
Table I.
In-class education protocol
| Contents | Time (min) | Education methods |
| Greetings | 10 | — |
| Activity 1. Is it common?—Overview of breast cancer and relevant statistics | 10 | Quiz, lecture |
| Activity 2. Breast structure | 10 | Brainstorming, breast models |
| Activity 3. Risk factors and symptoms of breast cancer | 15 | Brainstorming, tutorial |
| Activity 4. Let's talk about it—Mammography | 15 | Tutorial |
| Break | 10 | — |
| Activity 5. Breast self-exam | 10 | Role-playing, breast models |
| Activity 6. Case presentation—Screening for life | 10 | Real-world references |
| Activity 7. Barriers to breast cancer screening | 10 | Pictorial game |
| Activity 8. Better breast health—Prevention of breast cancer | 15 | Brainstorming, tutorial |
| Closing | 5 | — |
| Total | 120 |
Individually tailored follow-up counseling via telephone or home visits for 6 months was an integral part of the intervention program. In particular, the follow-up approach was determined by the participant's readiness to move to the next stage of adoption. Due to eligibility criteria, no KA women were in action or maintenance stages at baseline. For KA women at the lowest stage of motivation (pre-contemplation), LHW counseling was focused on increasing awareness of breast screening benefits and exploring barriers that prevent them from getting screening. For KA women with moderate motivation (contemplation), discussions were focused on individual barriers and facilitators to screening and setting tangible goals to reduce barriers. During the calls or home visits, LHWs assessed participants’ concerns/problems related to obtaining a mammogram, following a counseling protocol that outlined key points to be addressed. Identified problems were revisited at the next contact. In addition, constant navigation assistance was offered during the intervention period to address specific logistic barriers to breast cancer screening experienced by KA women in the sample (e.g. referrals to a health provider or other services such as the Maryland Breast and Cervical Cancer Program). As partial compensation for their time commitment, LHWs received a monthly stipend of $15 per hour per KA participant to cover incidental expenses.
Measurements
All study variables were measured twice at baseline and at 6 months by self-reports. Instruments used in this study were exclusively in Korean since all participants were born in Korea and preferred using their native language.
Breast cancer knowledge
BCK was measured using 10 items from the BCK test [43] (validated by several researchers in African-American and Jordanian women [44, 45]) in order to reflect updated screening guidelines. Knowledge scores were calculated by counting the number of correct responses to statements, such as ‘Most breast cancer is associated with hereditary factors'. Scores ranged from 0 to 10. In this study, the alpha coefficient of the Korean translation was 0.70.
Perceived susceptibility, benefits and barriers
The Champion HBM scales [46, 47] were used. A three-item Likert scale instrument assessed perceived susceptibility to breast cancer, asking beliefs of personal threat or harm related to breast cancer (e.g. ‘It is likely that I will get breast cancer.’). A five-item Likert scale instrument measured perceived benefits of mammography asking positive outcomes of mammography. Sample items include ‘Having a mammogram will help me find breast lumps early’. Perceived barriers to mammography were assessed by an 11-item Likert scale instrument that examined perceived emotional, physical or structural concerns related to mammography. Sample items include ‘Mammography is embarrassing, takes too much time, is costly, and painful’. The modified scale included five additional barriers specific to immigrant women such as a lack of English proficiency [48, 49], transportation [50, 51], health insurance [50, 52, 53] or physician recommendation [50, 53]. Higher scores indicated higher levels of perceived susceptibility, benefits and barriers. Reliability and validity of the scales have been reported with Cronbach's alphas ranging from 0.75 to 0.88 and test–retest reliability from 0.61 to 0.71 [46, 47, 54]. Construct validity was established using exploratory and confirmatory factor analyses and logistic regression for theoretical relationships [46, 47, 54]. In this sample of KA women, Cronbach's alphas measured 0.85, 0.90 and 0.71 at baseline for perceived susceptibility, benefits and barriers scales, respectively.
Modesty and utilization of oriental medicine
Modesty and utilization of oriental medicine are culture-specific barriers that women immigrating to the United States from eastern countries may have to receiving mammography and have been negatively associated with screening behaviors [14, 26, 35, 53]. We used Tang, Solomon and McCracken's instrument [53] to assess modesty and utilization of oriental medicines. The modesty section consists of a six-item Likert scale regarding perceived cultural barriers to getting screened (e.g. ‘I feel uncomfortable talking about my body with a doctor.’). The utilization of oriental medicine portion consists of a three-item Likert scale. A sample item is ‘I sometimes use oriental medicine as a treatment for health problems’. Higher scores indicate higher levels of modesty and reliance/preference for oriental medicine. Reliabilities for the scales were 0.72 and 0.68 in the sample, respectively.
Receipt of a mammogram, CBE and BSE
Participants self-reported the receipt of mammograms and CBE and their rate of regular BSE. If they ever had a mammogram and/or CBE, participants were asked when and where the last tests took place. While self-report of screening has been found reliable [55], overestimation of utilization has been reported among low-income minority women [56, 57]. We strongly encouraged candid and accurate responses to survey questions. In addition, we emphasized that participants’ identities would be protected by using a sealed envelope for follow-up questionnaires and, therefore, LHWs would not have access to them.
Analysis
Analysis was performed on 93 KA women who completed both the baseline and 6-month follow-up interviews (Fig. 1). Participants who completed and did not complete the study shared no significant sociodemographic differences (e.g. age, education, income and health insurance). Descriptive statistics helped to summarize sample characteristics and study variables. The primary outcome variables were self-reported receipt of a mammogram, CBE and BSE. Regular BSE was defined as BSE performed monthly or bimonthly. Secondary outcome variables were breast cancer screening knowledge, attitudes and beliefs. We compared each participant's matched responses with the baseline and 6-month follow-up questions to determine if their primary and secondary outcome variables had changed. McNemar chi-square tests were used to detect changes in receipt of a mammogram, CBE and BSE. Paired t-tests were used to determine changes before and after the LHW intervention in screening knowledge, beliefs and attitudes. A P value of <0.05 was considered significant.
Results
Sample characteristics
Table II presents sample characteristics at baseline. Study participants were mostly middle aged, with a mean age of 55.3 (±10.8) years (range = 40–80 years). About equal numbers of KA women in their 40s (n = 32), 50s (n = 28) and 60s or more (n = 33) participated in the study. Most women were married (69.9%), unemployed (64.5%), uninsured (55.9%), and had high school education or less (63.4%); 90.3% reported limited or absent English skills, though residing in the United States for an average of 17.4 (±8.4) years. Nearly two-thirds (65.5%) reported their income levels as being less than comfortable or difficult to manage.
Table II.
Baseline characteristics of the sample
| Variable | Category | n (%) |
| Age | 40–49 | 32 (34.4) |
| 50–59 | 28 (30.1) | |
| ≥60 | 33 (35.5) | |
| Marital status | Married | 65 (69.9) |
| Single/widowed | 28 (30.1) | |
| Employment status | Unemployed | 60 (64.5) |
| Full-time/part-time | 33 (35.5) | |
| Health insurance | None | 52 (55.9) |
| Private/others | 23 (24.7) | |
| Medicare/medicaid | 18 (19.4) | |
| Educational level | High school or less | 59 (63.4) |
| Some college or more | 34 (36.6) | |
| Income | Difficult to manage | 25 (26.9) |
| It is OK | 36 (38.7) | |
| Comfortable | 32 (34.5) | |
| English proficiency | Poor | 12 (12.9) |
| Limited | 72 (77.5) | |
| Fluent | 9 (9.6) | |
| Perceived health status | Fair | 5 (5.4) |
| Good | 69 (74.2) | |
| Very good | 15 (16.1) | |
| Excellent | 4 (4.3) | |
| Family history of breast cancer | Yes | 5 (5.5) |
| No | 88 (94.5) | |
| Menopausal status | Yes | 60 (64.6) |
| No | 33 (35.4) | |
| Taking hormones | Hormone replacement therapy | 5 (5.4) |
| Hormones for birth control | 3 (3.3) | |
| No | 85 (91.3) |
Most women (94.6%) perceived their health as being good or better. While no women in the study had been diagnosed with breast cancer, 5.5% had a family history of breast cancer with either their mother or sister. Nearly two-thirds of study participants (64.6%) were menopausal, with an average age of menopause onset being 49.0 (±5.4) years. Only 5.4% reported taking hormone replacement therapy at the time of the study.
Changes in primary outcomes
At baseline, the majority had heard of breast cancer (80.2%) or mammograms (71.4%), yet only 51.6% had ever had a mammogram. Similarly, less than half had ever had a CBE (46.2%) or had performed regular BSE monthly or bimonthly (19.8%) at baseline. At 6-month follow-up, participants showed increases in receipt of a mammogram by 31.9%, CBE by 23% and regular BSE by 36.2% compared with baseline (Table III). All these changes in screening behaviors were statistically significant (P < 0.001).
Table III.
Changes in screening behaviors before and after the intervention
| Variable | Baseline, n (%) | 6 months, n (%) | χ2 (P) |
| Heard of breast cancer | 73 (80.2) | 88 (94.6) | 0.36 (0.001) |
| Heard of mammography | 65 (71.4) | 85 (93.4) | 0.07 (0.000) |
| Heard of CBE | 53 (58.2) | 63 (69.2) | 3.94 (0.121) |
| Heard of BSE | 75 (82.4) | 87 (95.6) | 19.6 (0.000) |
| Ever had a mammogram (N = 93) | 48 (51.6) | 78 (83.5) | 28.0 (0.000) |
| Ever had a CBE | 42 (46.2) | 63 (69.2) | 34.7 (0.000) |
| Performed regular BSE | 18 (19.8) | 51 (56.0) | 37.6 (0.000) |
N = 91 due to missing data except for receipt of a mammogram.
We further examined time from the start of the intervention to mammogram receipt for women who reported obtaining a mammogram (n = 61) during the study period. These women received a mammogram at an average of 9.61 (±7.44) weeks from the start of the intervention. Following the stage definitions used in previous studies [39, 40], more than two-thirds of KA women in the study (67.7%) were in contemplation stage of mammography adoption and the rest (32.3%) in pre-contemplation stage at baseline. At 6-month follow-up, 61 women (65.6%) were in action stage, while 14 (15.1%) were in contemplation and 18 (19.4%) in pre-contemplation stages, respectively. Those women in contemplation stage at baseline were more likely than the women in pre-contemplation stage to report receipt of a mammogram (i.e. movement forward to action stage) at 6-month follow-up (χ2 = 7.03, P = 0.011).
Changes in secondary outcomes
We examined the effects of the LHW intervention on several secondary outcomes (Table IV). There was no statistically significant difference in mean BCK score before and after the intervention [6.3 (±1.4) versus 6.6 (±1.6), P = 0.104]. When individual items were examined, a few items related to specific breast cancer screening guidelines were found to be particularly difficult, with fewer than half of the sample responding correctly both at baseline and 6 months. These items included ‘Women without a family history of breast cancer should begin breast screening at the age of 30’ or ‘Women with a family history of breast cancer should undergo mammography screening at least every 5–10 years'.
Table IV.
Changes in BCK and beliefs before and after the intervention
| Variable | Baseline, mean (±SD) | 6 months, mean (±SD) | t (P) |
| Knowledge | 6.3 (±1.4) | 6.6 (±1.6) | −1.6 (0.104) |
| Perceived benefits | 19.4 (±3.0) | 19.7 (±2.5) | −0.6 (0.510) |
| Perceived susceptibility | 6.0 (±2.3) | 5.8 (±2.1) | 0.7 (0.459) |
| Perceived barriers | 40.4 (±7.1) | 38.9 (±8.9) | 1.5 (0.128) |
| Modesty | 16.1 (±3.2) | 14.8 (±3.5) | 3.9 (0.000) |
| Utilization of oriental medicine | 7.6 (±1.9) | 7.4 (±1.2) | 1.6 (0.114) |
SD, standard deviation.
The mean total scores on the Champion HBM scales slightly increased over time for perceived benefits and decreased for perceived susceptibility and barriers. None of the differences was statistically significant. When changes in modesty and utilization of oriental medicine were examined as culture-specific barriers to obtaining a mammogram, a significant reduction was observed in modesty (t = 3.9, P < 0.001) but not in utilization of oriental medicine.
Process evaluation
Our process evaluation focused on monitoring the delivery, acceptability and satisfaction of the LHW intervention. Every enrolled woman received LHW education about breast cancer screening. While there was variation in the length of the education sessions (ranging from 100 to 150 min, mean = 122.5 ± 24 min) due to group sizes (varying from 1 to 13, but mostly 4), the same core curriculum was delivered every time to KA women using flip chart guides with specific LHW talking points.
Women received follow-up LHW counseling and/or assistance regarding health care system navigation as a means of addressing individual barriers to obtaining a mammogram. Study participants received three to nine follow-up counseling sessions from their LHW via home visits or telephone calls during the intervention period (mean = 5.7 ± 1.0 sessions). Navigation assistance provided included information about mammogram facilities near participants’ homes (54%), updated information about low-income state cancer screening programs (36%), appointments for a mammogram (34%) and transportation and translation services (20%).
Upon completion of the intervention, acceptability of and satisfaction with the LHW program were assessed by survey items. Acceptability of the intervention was high, with an average of 4.25 (±1.0) on a five-point scale. Likewise, participants’ overall satisfaction with the program was high, with an average rating of 8.9 (±1.5) on a 10-point scale.
Discussion
The results demonstrate that the LHW model is both feasible and effective in reaching traditionally under-screened KA women and providing an intervention that increases their adherence to breast cancer screening guidelines. After the multifaceted intervention, the proportions of KA women increased significantly for every targeted screening procedure compared with baseline. LHWs may be the most effective strategy a person with limited access to health care services has to obtain health education and navigate the health care provider systems. The findings are mostly consistent with previous LHW interventions which showed improvements in cancer screening behaviors in hard-to-reach ethnic minority communities [20, 21, 24, 26]. LHW interventions were rarely combined with theory-driven behavioral tailoring, however. Rather, LHWs were used primarily as a culturally sensitive intervention approach. Stage-matched tailoring is increasingly used to more effectively guide behavioral interventions [39]. Our study, which was guided by the TTM in tailoring LHW counseling, yielded an increase of 31.9% in receipt of a mammogram as compared with 6–26% in the previous studies [47, 58–62]. On the whole, study results seem to suggest the need for interventions that combine theory-based behavioral tailoring with the use of LHWs in order to maximize intervention effectiveness.
The navigation assistance provided by trained LHWs proved to be a key factor in obtaining the resources for and promoting the utilization of preventive health care services. KA women struggle with not only language barriers but also a health system that is very different from their native country's [34, 63]. Our LHWs helped KA women through finding low-cost screening programs, locating mammogram facilities, making medical appointments, providing transportation and assisting the KA woman during procedures. One pitfall of such an interpersonally oriented method of intervention is that only a limited number of women can be reached directly. Since such an approach is often focused more on accommodating women's needs rather than developing their skills (e.g. providing translation rather than helping them learn basic English and essential medical terminology), the assumption that women would acquire skills to help them to move to the action stage and decrease their need for additional assistance does not appear to hold true. Recently, limited health literacy, closely associated with limited English language proficiency, is emerging as a far-reaching, major barrier to effective cancer screening, independent of race or socioeconomic status [64–66]. Health literacy is defined as ‘the degree to which individuals have the capacity to obtain, process and understand basic health information and services to make appropriate health decisions [67]'. KA women represent one of the most vulnerable recent immigrant groups because of their monolingual status and cultural isolation. Incorporating essential English and health literacy skills into an intervention program for linguistically isolated immigrant women such as KA may be worth of further investigation.
We have little explanations as to why we did not find any statistically significant differences in breast cancer knowledge and beliefs before and after the intervention, except for modesty. The result may indicate an insensitivity of the knowledge and beliefs instruments we used in capturing changes that were induced by the LHW intervention in this sample. These methodological issues require further investigation. The result might also have been due to the fact that the women received general information about breast cancer, risk factors and recommended screening guidelines. Another possibility is that movement forward to a better or higher stage of behavioral adoption (i.e. breast cancer screening) might not necessarily result from change in beliefs in the desired direction in this sample of KA women. For example, a recently published study [39] of women aged 50 years or older (N = 1245; 53% African-American, 44% White) revealed that no change in beliefs also predicted forward stage movement. Specifically, no change (compared with a decrease) was predictive of forward change movement. Likewise, stability (no change) in self-efficacy (compared with a decrease) was a significant predictor of forward movement in stage of mammography adoption. Changes in perceptions of susceptibility and knowledge were not significantly associated with forward stage movement in the study. While our study is not equipped to conduct similar logistic models due to a small sample size, the results warrant further investigation to identify the beliefs whose changes (or no changes) predict stage progression in the target population.
There were several potential limitations to the study. First, there was no comparison group in the study. When we first designed the study, our community partners felt strongly about providing the intervention to every participant. Due to the nature of pilot testing of this study (i.e. short time period with limited resources), we decided to conduct one-group pre- and post-test study instead of other alternatives (e.g. wait-list design or attention control design). Second, the results cannot be generalized to other ethnic groups. However, the strong impact on breast cancer screening behaviors that we observed plus increased breast cancer screening rates demonstrated in other studies [20, 21, 24–26] lend support to the theoretical foundations of the intervention, suggesting that this intervention approach using LHWs may have wide applicability in hard-to-reach minority women with limited resources. Third, screening behaviors were all self-reported. While these reports may have inflated the true screening rates, we attempted to minimize this potential bias by assuring confidentiality by using a sealed envelope for follow-up questionnaires and emphasizing the importance of accurate reporting in order to make the study meaningful for other KA women who might benefit from a similar program. Researchers have found good correlations between breast cancer screening rates derived from patient surveys and those derived from chart audits [55]. Finally, the study does not allow us to determine which intervention component contributed more or less to improving screening rates. However, the findings suggest that when these components are offered together as one cohesive intervention protocol, it can lead to significant improvements in breast cancer screening rates among KA women.
In conclusion, our neighborhood-based intervention that combined in-class education with follow-up counseling and navigation assistance by trained LHWs was successful in addressing the particular issues typical among recent Korean immigrants, such as language and cultural differences, and social isolation—barriers to obtaining adequate health knowledge and utilizing recommended cancer screening tests. Our findings indicate that tailoring the health education message with cultural sensitivity maximized by LHWs should be encouraged and adopted by other investigators who are developing effective cancer control interventions among underserved ethnic minority communities.
Funding
National Institutes of Health (CA110939 and P30 NR008995).
Conflict of interest statement
None declared.
Acknowledgments
The authors are grateful to all KA women and LHWs who participated in this study and research staff, Moonju Ko and Myunghee Kim. The authors also would like to add tribute to the efforts of Dr Victoria Mock, a mentor and a coinvestigator of this study, who was respected and admired by her students and colleagues.
References
- 1.American Cancer Society. Cancer Facts and Figures 2008. Atlanta, GA: American Cancer Society; 2008. [Google Scholar]
- 2.Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence—SEER 17 Regs Public-Use, Nov 2005 Sub (2000–2003) Available at: http://seer.cancer.gov/faststats/sites.php?site=Breast+Cancer&stat=Incidence#age. Accessed: 7 June 2007. [Google Scholar]
- 3.Deapen D, Liu L, Perkins C, et al. Rapidly rising breast cancer incidence rates among Asian American women. Int J Cancer. 2002;99:747–50. doi: 10.1002/ijc.10415. [DOI] [PubMed] [Google Scholar]
- 4.Ministry of Health and Welfare. Annual Report of the Central Cancer Registry in Korea 2001. Available at: http://www.mohw.go.kr/services/service.jsp?itn=tbdata&sa=11&sno=3409&bunrcode=320&page=2&face=1203&btype=1. Accessed: 21 November 2007. [Google Scholar]
- 5.McCracken M, Olsen M, Chen MS, Jr, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin. 2007;57:190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 6.Maskarinec G. Breast cancer-interaction between ethnicity and environment. In Vivo. 2000;14:115–23. [PubMed] [Google Scholar]
- 7.Innos K, Horn-Ross PL. Recent trends and racial/ethnic differences in the incidence and treatment of ductal carcinoma in situ of the breast in California women. Cancer. 2003;97:1099–106. doi: 10.1002/cncr.11104. [DOI] [PubMed] [Google Scholar]
- 8.Hedeen AN, White E, Taylor V. Ethnicity and birthplace in relation to tumor size and stage in Asian American women with breast cancer. Am J Prev Med. 1999;89:1248–52. doi: 10.2105/ajph.89.8.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller BA, Hankey BF, Thomas TL. Impact of sociodemographic factors, hormone receptor status, and tumor grade on ethnic differences in tumor stage and size for breast cancer in US women. Am J Epidemiol. 2002;255:534–45. doi: 10.1093/aje/155.6.534. [DOI] [PubMed] [Google Scholar]
- 10.US Preventive Services Task Force. Guide to Clinical Preventive Services. 2nd edn. Baltimore, MD: Williams & Wilkins; 1996. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Surveillance summaries. Morb Mortal Wkly Rep. 2003 52(No. SS-8) [Google Scholar]
- 12.Wismer BA, Moskowitz JM, Chen AM, et al. Mammography and clinical breast examination among Korean American women in two California counties. Prev Med. 1998;27:144–51. doi: 10.1006/pmed.1997.0259. [DOI] [PubMed] [Google Scholar]
- 13.Juon HS, Choi YJ, Kim MT. Cancer screening health behaviors among Korean American women. Cancer Detect Prev. 2000;24:589–601. [PubMed] [Google Scholar]
- 14.Tu SP, Yasui Y, Kuniyuki A, et al. Breast cancer screening among Cambodian American women. Cancer Detect Prev. 2000;24:549–63. [PubMed] [Google Scholar]
- 15.McPhee SJ, Stewart S, Brock KC, et al. Factors associated with breast and cervical cancer screening practices among Vietnamese American women. Cancer Detect Prev. 1997;21:510–21. [PubMed] [Google Scholar]
- 16.Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. Am J Prev Med. 2000;18:62–8. doi: 10.1016/s0749-3797(99)00110-5. [DOI] [PubMed] [Google Scholar]
- 17.Tu SP, Yasui Y, Kuniyuki AA, et al. Mammography screening among Chinese-American women. Cancer. 2003;97:1293–302. doi: 10.1002/cncr.11169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast cancer and cervical carcinoma screening rates and healthy people 2000 objectives. Cancer. 2000;89:696–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 19.Gomez S, Tan S, Keegan TH, et al. Disparities in mammographic screening for Asian women in California: a cross-sectional analysis to identify meaningful groups for targeted intervention. BMC Cancer. 2007;7:201. doi: 10.1186/1471-2407-7-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Earp JA, Eng E, O'Malley MS, et al. Increasing use of mammography among older, rural African American women: results from a community trial. Am J Public health. 2002;92:646–54. doi: 10.2105/ajph.92.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eng E, Smith J. Natural helping functions of lay health advisors in breast cancer education. Breast Cancer Res Treat. 1995;35:23–9. doi: 10.1007/BF00694741. [DOI] [PubMed] [Google Scholar]
- 22.Brownstein JN. The challenge of evaluating CHA services. In: Rosenthal EL, Wiggins N, Brownstein JN, et al., editors. Report of the National Community Health Advisor Study. Baltimore, MD: University of Arizona Press; 1998. pp. 50–74. [Google Scholar]
- 23.Yabroff KR, Mangan P, Mandelblatt J. Effectiveness of interventions to increase Papanicolaou smear use. J Am Board Fam Med. 2003;16:188–203. doi: 10.3122/jabfm.16.3.188. [DOI] [PubMed] [Google Scholar]
- 24.Navarro AM, Senn KL, McNicholas LJ, et al. Por La Vida model intervention enhances use of cancer screening tests among Latinas. Am J Prev Med. 1998;15:32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- 25.Margolis KL, Lurie N, McGovern PG, et al. Increasing breast and cervical cancer screening in low-income women. J Gen Intern Med. 1998;13:515–21. doi: 10.1046/j.1525-1497.1998.00161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bird JA, McPhee SJ, Ha NT, et al. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev Med. 1998;27:821–9. doi: 10.1006/pmed.1998.0365. [DOI] [PubMed] [Google Scholar]
- 27.Lam TK, McPhee SJ, Mock J, et al. Encouraging Vietnamese-American women to obtain Pap tests through lay health worker outreach and media education. J Gen Intern Med. 2003;18:516–24. doi: 10.1046/j.1525-1497.2003.21043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moskowitz JM, Kazinets G, Wong JM, et al. “Health is strength”: a community health education program to improve breast and cervical cancer screening among Korean American women in Alameda County, California. Cancer Detect Prev. 2007;31:173–83. doi: 10.1016/j.cdp.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Mock J, McPhee SJ, Nguyen T, et al. Effective lay health worker outreach and media-based education for promoting cervical cancer screening among Vietnamese American women. Am J Public Health. 2007;97:1693–700. doi: 10.2105/AJPH.2006.086470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paisano EL. We the Americans: Asians. Washington, DC: US Department of Commerce, Bureau of the Census; 1993. [Google Scholar]
- 31.Shin H, Bruno R. Language Use and English-Speaking Ability. 2000 Available at: http://www.census.gov/prod/2003pubs/c2kbr-29.pdf. Accessed: 21 November 2007. [Google Scholar]
- 32.Vu HH. Cultural barriers between obstetrician-gynecologists and Vietnamese/Chinese immigrant women. Tex Med. 1996;19:47–52. [PubMed] [Google Scholar]
- 33.Kim MJ, Cho H, Cheon-Klessig YS, et al. Primary health care for Korean immigrants: sustaining a culturally sensitive model. Public Health Nurs. 2002;19:191–200. doi: 10.1046/j.0737-1209.2002.19307.x. [DOI] [PubMed] [Google Scholar]
- 34.Han HR, Kang J, Kim KB, et al. Barriers to and strategies for recruiting Korean Americans for community-partnered health promotion research. J Immigr Minor Health. 2007;9:137–46. doi: 10.1007/s10903-006-9022-x. [DOI] [PubMed] [Google Scholar]
- 35.Sadler GR, Ryujin LT, Ko CM, et al. Korean women: breast cancer knowledge, attitudes and behaviors. BMC Public Health. 2001;1:7. doi: 10.1186/1471-2458-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brownstein JN, Bone LR, Dennison CR, et al. Community health workers as interventionists in research and practice for the prevention of heart disease and stroke. Am J Prev Med. 2005;29(Suppl. 1):128–33. doi: 10.1016/j.amepre.2005.07.024. [DOI] [PubMed] [Google Scholar]
- 37.San Francisco Department of Health Education. Sample Competency Checklist. Available at: www.communityhealthworks.org/chtdc_SOP.doc. Accessed: 6 March 2006. [Google Scholar]
- 38.Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research, and Practice. 2nd edn. San Francisco, CA: Jossey-Bass Publishers; 1997. pp. 60–84. [Google Scholar]
- 39.Menon U, Champion V, Monahan PO, et al. Health belief model variables as predictors of progression in stage of mammography adoption. Am J Health Promot. 2007;21:255–61. doi: 10.4278/0890-1171-21.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rakowki W, Ehrich B, Goldstein MG, et al. Increasing mammography among women aged 40–74 by use of a stage-matched, tailored intervention. Prev Med. 1998;27:748–56. doi: 10.1006/pmed.1998.0354. [DOI] [PubMed] [Google Scholar]
- 41.Stoddard AM, Rimer BK, Lane D, et al. Underusers of mammogram screening: stage of adoption in five U.S. subpopulations. Prev Med. 1998;27:478–87. doi: 10.1006/pmed.1998.0310. [DOI] [PubMed] [Google Scholar]
- 42.Strecher VJ, Rosenstock IM. The health belief model. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research, and Practice. 2nd edn. San Francisco, CA: Jossey-Bass Publishers; 1997. pp. 41–59. [Google Scholar]
- 43.McCance KL, Mooney KH, Smith KR, et al. Validity and reliability of a breast cancer knowledge test. Am J Prev Med. 1990;6:93–8. [PubMed] [Google Scholar]
- 44.Mandanat H, Merrill RM. Breast cancer risk-factor and screening awareness among women nurses and teachers in Amman, Jordan. Cancer Nurs. 2002;24:276–82. doi: 10.1097/00002820-200208000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Hall CP, Wimberley PD, Hall JD, et al. Teaching breast cancer screening to African American women in the Arkansas Mississippi river delta. Oncol Nurs Forum. 2005;32:857–63. doi: 10.1188/05.onf.857-863. [DOI] [PubMed] [Google Scholar]
- 46.Champion VL. Revised susceptibility, benefits, and barriers scale for mammography screening. Res Nurs Health. 1999;22:341–8. doi: 10.1002/(sici)1098-240x(199908)22:4<341::aid-nur8>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 47.Champion V, Maraj M, Hui S, et al. Comparison of tailored interventions to increase mammography screening in nonadherent older women. Prev Med. 2003;36:150–8. doi: 10.1016/s0091-7435(02)00038-5. [DOI] [PubMed] [Google Scholar]
- 48.Han Y, Williams RD, Harrison RA. Breast cancer screening knowledge, attitudes, and practices among Korean American women. Oncol Nurs Forum. 2000;27:1585–90. [PubMed] [Google Scholar]
- 49.Yu MY, Hong OS, Seetoo AD. Uncovering factors contributing to under-utilization of breast cancer screening by Chinese and Korean women living in the United States. Ethn Dis. 2003;13:213–9. [PubMed] [Google Scholar]
- 50.Maxwell AE, Bastani R, Warda US. Breast cancer screening and related attitudes among Filipino-American women. Cancer Epidemiol Biomarkers Prev. 1997;6:719–26. [PubMed] [Google Scholar]
- 51.Maxwell AE, Bastani R, Warda US. Mammography utilization and related attitudes among Korean American women. Women Health. 1998;27:89–107. doi: 10.1300/J013v27n03_07. [DOI] [PubMed] [Google Scholar]
- 52.Hiatt RA, Pasick RJ, Stewart S, et al. Community-based cancer screening for underserved women: design and baseline findings from the Breast and Cervical Cancer Intervention Study. Prev Med. 2001;33:190–203. doi: 10.1006/pmed.2001.0871. [DOI] [PubMed] [Google Scholar]
- 53.Tang TS, Solomon LJ, McCracken LM. Cultural barriers to mammography, clinical breast exam, and breast self-exam among Chinese-American women 60 and older. Prev Med. 2000;31:575–83. doi: 10.1006/pmed.2000.0753. [DOI] [PubMed] [Google Scholar]
- 54.Rawl SM, Champion VL. Measuring breast and colorectal cancer screening beliefs and behaviors. In: Frank-Stromborg M, Olsen SJ, editors. Instruments for Clinical Health Care Research. 3rd edn. Sudbury, MA: Jones & Bartlett; 2004. pp. 428–54. [Google Scholar]
- 55.Caplan LS, McQueen DV, Qualters JR, et al. Validity of women's self-reports of cancer screening test utilization in a managed care population. Cancer Epidemiol Biomarkers Prev. 2003;12:1182–7. (Pt 1) [PubMed] [Google Scholar]
- 56.McGovern PG, Lurie N, Margolis KL, et al. Accuracy of self-report of mammography and Pap smear in a low-income urban population. Am J Prev Med. 1998;14:201–8. doi: 10.1016/s0749-3797(97)00076-7. [DOI] [PubMed] [Google Scholar]
- 57.Champion VL, Menon U, McQuillen DH, et al. Validity of self-reported mammography in low-income African American women. Am J Prev Med. 1998;14:111–7. doi: 10.1016/s0749-3797(97)00021-4. [DOI] [PubMed] [Google Scholar]
- 58.Kreuter MW, Sugg-Skinner C, Holt CL, et al. Cultural tailoring for mammography and fruit and vegetable intake among low-income African-American women in urban public health centers. Prev Med. 2005;41:53–62. doi: 10.1016/j.ypmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 59.Rimer BK, Conaway M, Lyna P, et al. The impact of tailored interventions on a community health center population. Patient Educ Couns. 1999;37:125–40. doi: 10.1016/s0738-3991(98)00122-0. [DOI] [PubMed] [Google Scholar]
- 60.Champion VL, Springston JK, Zollinger TW, et al. Comparison of three interventions to increase mammography screening in low income African American women. Cancer Detect Prev. 2006;30:535–44. doi: 10.1016/j.cdp.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 61.Jibaja-Weiss ML, Volk RJ, Kingery P, et al. Tailored messages for breast and cervical cancer screening of low-income and minority women using medical records data. Patient Educ Couns. 2003;50:123–32. doi: 10.1016/s0738-3991(02)00119-2. [DOI] [PubMed] [Google Scholar]
- 62.Ahmad F, Cameron JI, Stewart DE. A tailored intervention to promote breast cancer screening among South Asian immigrant women. Soc Sci Med. 2005;60:575–86. doi: 10.1016/j.socscimed.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 63.Kandula NR, Kersey M, Lurie N. Assuring the health of immigrants: what the leading health indicators tell us. Annu Rev Public Health. 2004;25:357–76. doi: 10.1146/annurev.publhealth.25.101802.123107. [DOI] [PubMed] [Google Scholar]
- 64.Lindau ST, Tomori C, McCarville MA, et al. Improving rates of cervical cancer screening and Pap smear follow-up for low-income women with limited health literacy. Cancer Invest. 2001;19:316–23. doi: 10.1081/cnv-100102558. [DOI] [PubMed] [Google Scholar]
- 65.Garbers S, Chiasson MA. Inadequate functional health literacy in Spanish as a barrier to cervical cancer screening among immigrant Latinas in New York City. Prev Chronic Dis. 2004;1:A07. [PMC free article] [PubMed] [Google Scholar]
- 66.Lindau ST, Tomori C, Lyons T, et al. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol. 2002;186:938–43. doi: 10.1067/mob.2002.122091. [DOI] [PubMed] [Google Scholar]
- 67.US Department of Health and Human Services. Health Literacy Definition. Washington, DC: US Department of Health and Human Services; 2000. [Google Scholar]