Abstract
Background
Globally many doctors, particularly in low-income countries, have no formal training in using new information to improve their practice. As a first step clinicians must have access to information and so we explored reported access in graduating medical students in Nairobi.
Objectives
To evaluate final year medical students’ access to new medical information.
Methods
A cross-sectional survey of fifth (final) year medical students at the University of Nairobi using anonymous, self-administered questionnaires.
Findings
Questionnaires were distributed to 291 (85%) of a possible 343 students and returned by 152 (44%). Within the previous 12 months half reported accessing some form of new medical information most commonly from books and the internet. However, only a small number reported regular access and specific, new journal articles were rarely accessed. Absence of internet facilities, slow internet speeds and cost were common barriers to access while current training seems rarely to encourage students to seek new information.
Conclusion
Almost half the students had not accessed any new medical information in their final year in medical school suggesting they are ill prepared for a career that may increasingly demand life-long, self-learning.
INTRODUCTION
Evidence based medicine (EBM) is life-long, self directed learning in which patient care defines the need for clinically important information on diagnosis, prognosis, cost-effectiveness and other related issues. Evidence-based practice is the integration of the best research and other scientific evidence with clinical expertise and patient values and is widely believed to help optimise care. [1-14, 19] These approaches in theory, therefore, help bridge the “know-do” gap translating research into useful interventions, actions and policies. [20, 21] To promote the use of evidence and enhance skills in life-long learning many medical schools are attempting to move away from teaching based on traditional rote learning and the expert opinion of experienced clinicians and include learning based on accessing and interpreting research evidence [4]. Thus most medical programmes in the United States attempt to teach EBM, although this is not always successful [5]. Here in Kenya and indeed in sub-Saharan Africa, such efforts at the undergraduate level are much more modest [17],[6] despite the fact that introducing skills in evidence acquisition and use have been shown to increase current and future use of evidence, and boost students’ confidence in clinical decision making. [7, 8, 18]
Set in Kenya’s largest medical school we sought to characterise the exposure students have to research evidence as the first part of this process and, by implication, explore how successful efforts at research dissemination are in reaching one, potentially important audience.
METHODOLOGY
The University Of Nairobi, School Of Medicine, established in 1967, had a total student population of about 1,750 in 2007. The College of Health Sciences library is located within a few hundred metres of the hospital and classrooms where 3rd, 4th and 5th year students are taught. This library can seat 250 and serves a total college population of about 3,750 people. Internet access was made available in 2000 and, at the time of study, there were 40 networked computers and 77 free, fixed access ports for those with portable computers. The library offers full text electronic access to many journal sites through HINARI and specific university access codes. In addition a Local Area Network has been set up in rooms in the adjacent student halls of residence although less than a third of the students reside in these halls.
We aimed to evaluate exposure to ‘research’ evidence by exploring self-reported access to, sources and value of research information amongst final year medical students in Nairobi. Employing a specifically developed, self administered questionnaire data were collected from October to November 2007, at the end of students’ five year training. Questionnaires were distributed at two, separate seminars intended for the entire year group that were held 4 weeks apart. Those who indicated they had completed a questionnaire in the first round were not given a questionnaire in the second round. Questionnaires were anonymous with the only personal data collected being sex and whether university costs were state subsidised or borne entirely by the student. Questionnaires were collected at the end of the seminars or the following day.
The questionnaire was designed to allow quantitative analysis of whether medical students were able to access research findings and to explore the value they place on research. Question topics or themes were based on an understanding of the context (5 of the authors are medical students) and were piloted with 4th year students. The questionnaire was structured with predominantly pre-coded, closed questions and made use of a five-point Likert scale in some cases to ascertain strength of agreement with specific statements. The latter responses were subsequently collapsed to three-point scales (agree / neutral / disagree) during analysis.
For the purposes of this study the following definition was provided as part of the questionnaire: NEW medical information is defined as information not found in standard medical textbooks but representing a recent addition to medical knowledge. We defined a priori primary sources (original research papers or systematic reviews in journals) or secondary sources (books with new findings, narrative literature overviews, research briefs/ highlights, conferences/ seminars/ workshops or journal clubs). Data were double entered using Epi Info version 3.3.2 and validated before analysis with Stata version 9.2.
RESULTS
During the two distribution rounds self-administered questionnaires were issued to 291 students out of a potential class of 343. A total of 152 questionnaires were returned giving an overall response rate of 44% (152/343). As there were no differences between the respondents’ demographic characteristics (table 1) from the two distribution episodes and as neither of these two baseline characteristics appeared to influence any of the responses (analyses not shown) all data were pooled for this descriptive analysis.
Table 1. Demographic characteristics of respondents.
| Whole 5th year class ( Total = 343) | Responding students (n = 152) | |
|---|---|---|
| Government sponsored students | 132 (38%) | 62 (43%) |
| Self-sponsored students | 211 (62%) | 83 (57%) |
| Male students | 164 (48%) | 74 (50%) |
| Female students | 179 (52%) | 74 (50%) |
Access and sources
Out of 152 respondents, 77 (51%) had accessed primary (58/152, 38%) and / or secondary (68/152, 45%) sources of new research information (RI) with 75 (49%) reporting that they had not accessed any of these sources of new information. Ninety five (63%) students reported that they had read at least one complete article, not necessarily new, in any journal in the previous 12 months with the East African Medical Journal (59 / 152, 39%), available in paper copy in the library, the most often accessed. Other journals students had reportedly read articles from included the New England Journal of Medicine and the British Medical Journal, both cited by 27/152 (18%) of students.
From the subset of students attempting to find new information frequently (at least weekly) books and the internet were the most commonly reported sources of research information (table 2). Students reported very limited access to journal clubs and conferences or research seminars and only occasional access to journals (table 2). The university library was the most popular point of access for research information whereas public libraries were accessed by only 6/152 students (4%). The internet was accessed from both the university library and, less often, private sources.
Table 2. Frequency reported by final year medical students of accessing different sources of new medical information in the 12 months prior to the survey.
| Frequency (n = 152) | Specific Journals | Journal Clubs | Internet sites (other than specific journals) | Books | Conferences / Seminars / Workshops |
|---|---|---|---|---|---|
| Weekly | 13 (9%) | 3 (2%) | 58 (38%) | 40 (26%) | 2 (2%) |
| Monthly | 30 (20%) | 6 (4%) | 16 (11%) | 7 (5%) | 18 (12%) |
| Annually | 22 (14%) | 3 (2%) | 5 (3%) | 4 (3%) | 44 (29%) |
| Never | 87 (57%) | 143 (92%) | 73 (48%) | 101 (66%) | 88 (57%) |
Interest in accessing research information
The majority of the respondents, 106/152 (70%), expressed an interest in accessing research information, while 21 (14%) were indifferent, 7 (5%) were not interested and 18/152 (11%) gave no response. In about half of those seeking new information it was to improve general knowledge with 32/77 (41%) in this group accessing research information to help with an assignment. Only 12/77 (15%) in this group had accessed new research information in response to a perceived requirement of the curriculum.
Hindrances to accessing research information
The questionnaire listed lack of time, slow internet speed, cost, unavailability and ‘other reasons’ as possible hindrances. Out of 132 students providing responses, 112 (85%) indicated that one or more of these made accessing research information problematic (figure 1). Research papers, literature reviews and journal clubs were generally reported to be unavailable. Lack of time and slow internet speeds were identified as the main hindrance to accessing journals and lack of time and cost as hindrances to accessing seminars and conferences.
Figure 1. Proportion of medical students reporting that access to a source of new medical information was hard or very hard on a five-point scale ranging from very easy to very hard.
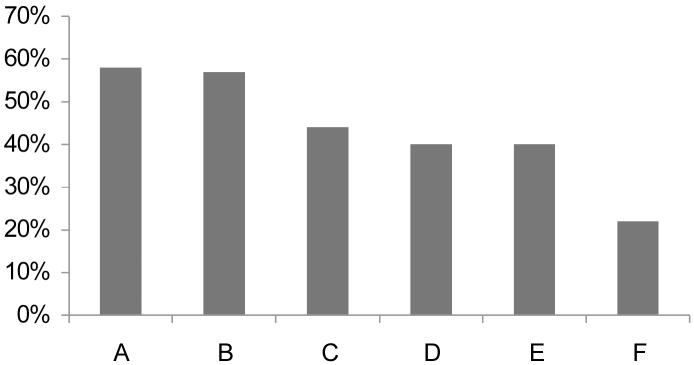
A = access to research papers, B = access to journal clubs, C = access to conferences / seminars, D = access to literature summaries, E = access to whole journals, F = access to appropriate books
One hundred and thirty six students responded to questions concerning the value of research information. Most (124/136, 91%) considered it to be of value to medical students and two thirds felt it already influences teaching and practice of medicine in Kenya. Interestingly despite the relatively low frequency in accessing research information and despite there being no specific teaching on interpretation of biomedical literature students reported themselves in 58/136 (43%) of cases to be good at interpreting research findings with only 16/136 (12%) reporting themselves to be poor. When asked to rate the credibility of research information sources on a scale of 5 (very high) to 1 (very low) average scores varied from (and in order): conferences / seminars (average score = 4.0), books (3.9), journals (3.8), research overviews (3.7), journal clubs (3.3) and information provided by pharmaceutical company representatives (2.7).
Discussion
Competent clinicians are required to keep abreast with new findings in the medical world in order to offer the best treatment to their patients. It has also been argued that researchers share some of the responsibility for bridging the ‘know-do’ gap. For these reasons we sought to evaluate the access to, sources of and views on the value of new research information from the point of view of final year medical students at the University Of Nairobi, Kenya, a country host to a relatively large research community for a low-income setting, To our knowledge this is the first local study to address these issues.
The study was conducted at around the time of final exams and the response rate was approximately 50%, similar to that in many studies using a similar methodology. Although conducting this survey at another time may have improved response rates opportunities to approach nearly 350 final year students are rare and only minimal resources were available for this study. We cannot, therefore, exclude the possibility of bias within our respondent population. However, it was similar in composition to the entire class with respect to two basic characteristics, sex and proportion self-funding their studies, providing some reassurance that views are representative of all students graduating in 2007.
The main findings are that most respondents (63%) had read something (old or new) from at least one journal in the past year but only 51% reported looking at new medical information within this period even when a wide variety of possible sources, of which books and the internet were the most frequent, were considered. In many settings hard-copy books would perhaps not be regarded as good sources of new information (making our estimate over optimistic) however others have also found that books are commonly cited as sources of ‘new’ information in health. [8] The internet was identified as the second most accessed source a finding that contrasts with a study done in Canada [15] where the internet was most used.
The majority of students (84%) reported that one or more simple practical issues hindered access to research information which may explain the difference observed between those interested in new information and those actually accessing it. Among the hindrances faced by students, cost, followed by lack of time and lack of opportunity were commonly reported, consistent with findings from Nigeria[16] However, although most students do not have a personal computer and the available, free internet access is slow (observation of the authors) it is our experience that many students are neither aware that they pay a fee ($50 per year) for internet access nor that their library has free full text access to many online journals. This may reflect a lack of emphasis on new information within the curriculum and indicates that improving awareness around and demand for new information will also be required if students in Nairobi are to become better prepared for life-long learning. It is also clear that Kenyan medical students are largely unaware of the research work done in their own and other developing countries.
Acknowledgements
This work was undertaken and is reported with the permission of the College of Health Sciences whose help we would like to recognise. We would also like to thank the final year students who took part in this study and the KEMRI / Wellcome Trust Programme who played host to the medical students during their elective period when this project was conducted.
Financial Support
Mike English is supported by a Wellcome Trust Senior Fellowship (#076827). There was no specific financial support for this work although the KEMRI / Wellcome Trust Programme provided general support for student electives.
Footnotes
Conflict of Interest
GI & AW are employed by the University of Nairobi and ME is an honorary lecturer. However, any opinions expressed are those of the authors and not the University. No funding agency had any influence on the decision to publish nor the content of the report.
REFERENCES
- 1.Shaughnessy Allen F, Slawson David C. Are we providing doctors with the training and tools for lifelong learning? BMJ. 1999;319:1280. doi: 10.1136/bmj.319.7220.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sackett David L, Rosenberg William M C. The need for Evidence-based Medicine. J R Soc Med. 1995;88:620–624. doi: 10.1177/014107689508801105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rafuse Jill. Evidence-based medicine means MDs must develop new skills, attitudes. Can Med Assoc J. 1994;150(9):1479–81. [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas Patricia A., Cofrancesco Joseph. Introduction of Evidence-based Medicine into an Ambulatory Clinical clerkship. J Gen Intern Med. 2001;16:244–249. doi: 10.1046/j.1525-1497.2001.016004244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Del Mar Chris, Glasziou P, Mayer D. Teaching evidence based medicine: Should be integrated into current clinical scenarios? BMJ. 2004;329:989–90. doi: 10.1136/bmj.329.7473.989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okoromah C, Adenuga A, Lesi F. Evidence-based medicine curriculum: impact on medical students. Medical Education. 2006;40:459–489. doi: 10.1111/j.1365-2929.2006.02454.x. [DOI] [PubMed] [Google Scholar]
- 7.Leung GM, Johnston JM, Tin KY, Wong IO, Ho LM, Lam WW, Lam TH. Randomized controlled trial of clinical decision support tools to improve learning of evidence based medicine in medical students. BMJ. 2003;327:1090. doi: 10.1136/bmj.327.7423.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dorsch J, Aiyer M, Meyer LE. Impact of an evidence-based medicine curriculum on medical students’ attitudes and skills. J Med Libr Assoc. 2004;92(4) [PMC free article] [PubMed] [Google Scholar]
- 9.Stewart R, Wiggins M. Exploring the Evidence-Practice Gap: A Workshop Report on Mixed and Participatory Training for HIV Prevention in Southern Africa. Education for Health. 2005;18(2):224–235. doi: 10.1080/13576280500148536. [DOI] [PubMed] [Google Scholar]; Schilling K, Wiecha J, Polineni D, Khalil S. An Interactive Web-based Curriculum on Evidence-based Medicine: Design and Effectiveness. Fam Med. 2006;38(2):126–32. [PubMed] [Google Scholar]
- 10.Srinivasan M, Weiner M, Breitfeld PP, Brahmi F, Dickerson K, Weiner G. Early introduction of an EBM course to preclinical medical students. J Gen Intern Med. 2002;17:58–65. doi: 10.1046/j.1525-1497.2002.10121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thom D, Haugen J, Sommers PS, Lovett P. Description and evaluation of an EBM curriculum using a block rotation. BMC Medical Education. 2004;4:19. doi: 10.1186/1472-6920-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wanvarie S, Sathapatayavongs B, Sirinavin S, Ingsathit A, Ungkanont A, Sirinan C. Evidence-based Medicine in Clinical Curriculum. ANN ACAD MED Singapore. 2006;35:615–8. [PubMed] [Google Scholar]
- 13.Chinnock P, Nandi Siegfried N, Clarke M. PLoS Medicine. 2005;2(5):e107. doi: 10.1371/journal.pmed.0020107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bridges Patricia H, Bierema Laura L, Valentine Thomas. The propensity to adopt evidence-based practice among physical therapists. BMC Health Services Research. 2007;7:103. doi: 10.1186/1472-6963-7-103. doi:10.1186/1472-6963-7-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schultz K, Kirby J, et al. Medical Students’ and Residents’ preferred site characteristics and preceptor behaviours for learning in the ambulatory setting: a cross-sectional survey. BMC MEDICAL EDUCATION. 2004;4:12. doi: 10.1186/1472-6920-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bello IS, Arogundade FA, Sanusi AA, Ezeoma IT, Abioye-Kuteyi EA, Akintola A. Knowledge and Utilization of Information Technology Among Health Care Professionals and Students in Ile-Ife, Nigeria: A Case Study of a University Teaching Hospital. J Med Internet Res. 2004;17(6(4)):e45. doi: 10.2196/jmir.6.4.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santesso N, Tugwell P. Knowledge translation in developing countries. Journal Of Continuing Education In The Health Professions. 2006;26:87–96. doi: 10.1002/chp.55. [DOI] [PubMed] [Google Scholar]
- 18.Genuis SK, Genuis JK. Exploring the continuum the translation of knowledge into clinical practice. Journal Of Evaluation In Clinical Practice. 2006;12:49–82. doi: 10.1111/j.1365-2753.2005.00608.x. [DOI] [PubMed] [Google Scholar]
- 19.Hanney S, Mugford M, et al. Assessing the benefits of health research lessons from research into antenatal corticosteroids. SOCIAL SCIENCE & MEDICINE. 2005;60:937–947. doi: 10.1016/j.socscimed.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 20.Garner P, Meremikwu M, Volmink J, Hu Q, Smith H. Putting evidence into practice: how middle & low income countries get it together. BMJ. 2004;329:1036–1039. doi: 10.1136/bmj.329.7473.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pang T, Pablos-Menendez A, IJsselmuiden C. From Bangkok to Mexico; towards a framework of turning knowledge into action to improve health systems. Bulletin WHO. 2004;82(10):70–72. [PMC free article] [PubMed] [Google Scholar]
- 22.Hurwitz B. How does evidence based guidance influence determinations of medical negligence? BMJ. 2004;329:1024–1028. doi: 10.1136/bmj.329.7473.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]


