Abstract
Objective
To estimate the joint effect of a multifaceted access intervention on primary care physician (PCP) productivity in a large, integrated prepaid group practice.
Data Sources
Administrative records of physician characteristics, compensation and full-time equivalent (FTE) data, linked to enrollee utilization and cost information.
Study Design
Dependent measures per quarter per FTE were office visits, work relative value units (WRVUs), WRVUs per visit, panel size, and total cost per member per quarter (PMPQ), for PCPs employed >0.25 FTE. General estimating equation regression models were included provider and enrollee characteristics.
Principal Findings
Panel size and RVUs per visit rose, while visits per FTE and PMPQ cost declined significantly between baseline and full implementation. Panel size rose and visits per FTE declined from baseline through rollout and full implementation. RVUs per visit and RVUs per FTE first declined, and then increased, for a significant net increase of RVUs per visit and an insignificant rise in RVUs per FTE between baseline and full implementation. PMPQ cost rose between baseline and rollout and then declined, for a significant overall decline between baseline and full implementation.
Conclusions
This organization-wide access intervention was associated with improvements in several dimensions in PCP productivity and gains in clinical efficiency.
Keywords: Access, productivity, cost, incentives, integrated group practice
This paper presents one part of the evaluation of Group Health Cooperative's (GHC) Access Initiative, an organizational innovation designed to improve access to improve quality (Ralston et al. in press). The Initiative's broad goal is to transform GHC from the standard health management organization (HMO) model, with managed care controls restricting enrollee access and choice, to a more patient-centered model, in which enrollees receive care when and how they want it from their choice of primary or specialty provider. We specifically examine the effect of this patient-centered intervention on primary care physician (PCP) productivity.
The Initiative comprises the following seven, system-wide reforms rolled out during 2002–2003:
Advanced access to primary care (appointments with a patient's PCP at the preferred time of the patient).
Direct access to most specialties without primary care gatekeeping.
Changes in physician compensation.
Primary care system redesign to control costs.
Patient-provider secure messaging through the MyGroupHealth enrollee website including physician financial incentives for secure messaging patients.
Internet access for enrollees to their electronic medical records (EMRs) through MyGroupHealth.
Health promotion information on the MyGroupHealth secure website.
GHC's Access Initiative is “ahead of the curve” in improving quality of care in concordance with national recommendations. In two prominent reports the Institute of Medicine (IOM) (2001) and RAND Community Quality Index Study (McGlynn et al. 2003) conclude that the U.S. health care delivery system is plagued by low-quality care and in need of fundamental change. The IOM argues that poorly designed delivery systems are a major cause of the problem, and that quality can be improved by changing systems to assure that health care is safe, effective, patient-centered, timely, efficient, and equitable. Complementing these objectives, the IOM also recommends changes in three areas: (1) new care processes guided by “simple rules” to serve patient needs (e.g., “patients should receive care whenever they need it and in many forms, not just face-to-face visits”); (2) better information technology to support care processes; and (3) alignment of provider payment with quality improvement (IOM 2001). Three of the IOM aims (patient-centeredness, timeliness, and efficiency) are central to the Access Initiative, and the Initiative includes all three IOM change areas (simple rules, information systems, and physician payment).
Our principal objective in this paper is to estimate and interpret effects of the Access Initiative on several dimensions of PCP productivity. While patient centered, the Initiative is also designed to enhance physician incentives and organizational structures and processes to support improved access and quality of care. Indeed, increased physician productivity is essential in realizing the Initiative's primary goal of improving access for patients, while maintaining financial viability.
A secondary objective of the paper is to assess the relationship between certain physician and enrollee characteristics and PCP productivity, while controlling for clinic attributes and time. This study is one of a small number addressing PCP productivity within an HMO (Lewandowski et al. 2006), and also one of the few using an extended time series (Hurdle and Pope 1989; Pope 1990), thereby allowing us to trace the evolution of primary care productivity.
Three of the Initiative's seven components directly address physician productivity:
Primary Care Redesign: Faced with declining enrollment, relative provider inefficiency when compared with similar group practices, and excessive overhead costs, GHC sought to reposition the group practice in October 2002 to be market competitive by restructuring primary care (Ralston et al. in press).
Changes in Physician Compensation: To support Advanced and Direct Access and Primary Care Redesign, the primary physician compensation method changed from 100 percent of guaranteed salary to a variable compensation system in April 2003. Primary physicians receive 80 percent guaranteed base salary plus additional variable compensation up to 120 percent of the guaranteed base, determined primarily by individual physician productivity (number and intensity of patient encounters).
Patient–Physician Secure Messaging through MyGroupHealth: In January 2002, GHC introduced web-based secure messaging between patients and providers. The website, MyGroupHealth, was introduced in 2000 and by April of 2002 allowed all enrollees to exchange electronic messages with their PCPs. Patient access to the EMR over MyGroupHealth is provided through a direct link to Group Health's clinical information system (CIS), EpicCare.™ Physician order entry and integrated systematic documentation in the CIS was rolled out at Group Health between October 2003 and December 2005.
New Contributions: This study makes several unique contributions to the evidence base on PCP productivity:
We control for enrollee case mix in productivity analyses, thus eliminating an important potential confounder in previous medical productivity studies.
This study examines case-mix-adjusted panel size, thus examining productivity beyond measures of service production per physician full-time equivalent (FTE).
Case-mix-adjusted, annual cost per member per quarter (PMPQ) in the provider's panel is also measured, allowing one to assess PCP clinical efficiency in caring for a defined population. To the extent that improved health of the physician's panel is related to lower annual care costs per enrollee, this PMPQ metric comes closer to capturing production of health—the ultimate “product” of physician services.
The time series of productivity experience (8 years) is the longest of extant studies of medical productivity.
We focus on the intervention's joint effect on productivity, rather than attempting to parse the impact of each of the seven Initiative components. The Access Initiative was conceived as an integrated package. Our evaluation design takes advantage of the phasing of key aspects of the Initiative to identify changes in productivity that are plausibly attributable to the Access Initiative, but we do not attempt to link discrete intervention components to changes in primary care productivity.
LITERATURE REVIEW
Several papers have addressed PCP productivity in the past two decades (Hurdle and Pope 1989; Gaynor and Pauly 1990; Pope 1990; Gaynor and Gertler 1995; Conrad et al. 2002; Goodman 2004; Lewandowski et al. 2006). The papers by Gaynor and Gertler (1995), Gaynor and Pauly (1990), and Conrad et al. (2002) stress the impact of production-based compensation on PCP productivity. All three estimate a significant positive effect of production-based compensation on output per physician. Using various measures of physician output (visits, relative value units [RVUs], inflation-adjusted charges per unit of physician time), those papers demonstrate that output is from 7 to 28 percent higher among physicians compensated on a 100 percent production basis, compared with those on production-neutral, salary-based compensation.
The latter three papers also found diseconomies of size (number of physicians) in medical practices. In a related review article, Pauly (1996) concludes that economies of scale do not explain the growth of multispecialty groups. Similarly, Conrad et al. (2002) and Kimball and Lorant (1977) found decreasing returns to scale in fee-for-service (FFS) medical practices. Physician characteristics appear to influence provider productivity. Other things being equal, female physicians appear to produce fewer visits and services per unit of time, and more experienced physicians are more productive (Gaynor and Pauly 1990; Conrad et al. 2002).
In nationwide physician surveys conducted by the Health Care Financing Administration and the National Opinion Research Center between 1975 and 1985, Pope (1990) and Hurdle and Pope (1989) find substantially declining physician visit productivity (i.e., patient visits per physician). Decreasing visit productivity is accompanied by increased service intensity and physician time per visit. More recent research (Weeks and Wallace 2003) confirms that continuing secular declines in patient visits per week between 1987 and 1998 of 9–28 percent, depending on physician specialty.
Previous econometric studies of physician productivity generally examined FFS medical practices (Kimball and Lorant 1977; Gaynor and Pauly 1990; Gaynor and Gertler 1995; Conrad et al. 2002). In contrast, Weiner's (2004) examination of physician staffing found that physician–population ratios in 10 large prepaid group practice HMOs were roughly 22–37 percent lower than the national average. Goodman (2004) remarks that Kaiser Permanente and GHC were in the lowest and next lowest quintiles of physicians per capita, respectively, in the 306 hospital referral regions listed in the Dartmouth Atlas. While not directly estimating physician productivity, the work by Weiner and Goodman does suggest potentially significant productivity differences between group HMO and FFS settings.
The most salient prior research for our paper is the longitudinal panel study of 105 PCPs employed at a large prepaid medical group in Minnesota during 1998–2002 (Lewandowski et al. 2006). Three major organizational changes were implemented in 2000: (1) PCP compensation method was altered from fixed salary to production based (with a guaranteed floor of 1999 compensation for the year 2000 only); (2) primary care scheduling was restructured to facilitate same-day appointments to one's regular physician; (3) size and scope of nurse triage systems and registered nurse staffing in most clinics were adjusted, aiming to improve appointment access. This “natural experiment” was associated with a rise of work relative value units (WRVUs) per FTE physician of 38 percent between 1998 and 2002 and declines of 13 and 20 percent, respectively, in PCP compensation per WRVU and clinic-operating costs per WRVU. The authors conclude, “It is possible to substantially and simultaneously improve costs of care, physician compensation, and patient access without harming patient satisfaction” (p. 573).
Finally, a recent study in the University of California Davis Health System (Liederman et al. 2005) compared productivity between physicians using a secure web messaging system and a control group. The authors observed a 10 percent increase in productivity among the physician web users relative to the controls. However, a systematic review by Chaudry et al. (2006) of the impact of health information technology (HIT) reported mixed effects of HIT on physician productivity and efficiency. Blumenthal and Glaser (2007) point out that health information and technology must be designed purposefully if HIT is to achieve specific cost and quality goals.
Implications of the Literature Review
This selective summary of prior physician productivity studies implies that examining PCP productivity within the prepaid group HMO setting is a novel enterprise. Moreover, secularly declining physician visit productivity and rising service intensity of visits reinforce the importance of identifying factors that affect physician productivity over time—including organizational interventions such as the GHC Access Initiative that incorporate changes in compensation incentives, practice redesign, alterations in patient appointment scheduling, and secure patient–physician web messaging. Productivity effects of implementing and maintaining advanced HIT are still unclear. Theory and evidence also suggests that PCP productivity studies must account for not only labor and capital inputs, but also provider characteristics and practice settings.
METHODS
Conceptual Model for Assessing Productivity
PCP productivity is multidimensional. The initial productivity margin for the PCP is case-mix-adjusted panel size—the number of enrollees for whom the PCP assumes clinical responsibility, controlling for underlying medical need and severity of illness. Second, PCP productivity is measured by patient visits per unit of own time (visits per FTE), controlling for other labor and capital inputs. Service intensity of visits (WRVUs per visit) captures a third margin of PCP productivity—the extent to which services and procedures are concentrated per visit, thus spreading fixed costs of provider and patient time. Multiplying service intensity by visits/FTE yields WRVUs per FTE: a broad measure of productivity reflecting the provider's case-mix-adjusted panel size, visit productivity, and service intensity of visits. Finally, recognizing that cost minimization is the “dual” (flip side) of productivity maximization in production theory (Silberberg 1990), we estimate the case-mix-adjusted per capita cost of caring (PMPQ) for the same study population of PCPs. Following production theory and our literature review, we posit that variations in labor and capital inputs and in provider characteristics and practice settings will affect these PCP productivity and cost measures.
To aid in interpretation of subsequent findings, we now state our expectations for the pattern of PCP productivity change in response to the intervention:
During the transition from baseline to rollout one might anticipate some decline in productivity, as PCPs adjust to new requirements for electronic documentation, heightened patient expectations for secure messaging, and lags in converting to the new enterprise-wide information system.
To the extent that direct enrollee access to specialists results in fewer visits to PCPs, the latter may produce fewer visits per FTE—possibly raising productivity through higher service intensity (RVUs per visit). Moreover, raising productivity through increased service intensity per visit may involve lower time and transaction costs to the PCP than increasing productivity through increased visit volumes.
PCPs also may respond to reduced primary care visits per enrollee by growing their panel size per FTE. The Access Initiative's compensation incentives for increased productivity have opposing effects: the heightened monetary payoff per unit of time itself will encourage more panel size per FTE and increased FTE (the positive “substitution effect”), while the ability to earn as much income as before, but in less time, could encourage a reduction in FTE (negative “income effect”).
Finally, duality in production theory between cost minimization and maximal efficiency (productivity) suggests that improved productivity—if realized by the intervention—should be accompanied by lower case mix-adjusted PMPQ cost.
RESEARCH SETTING
GHC
GHC is the nation's oldest and largest consumer-governed integrated health care organization and provides comprehensive health and preventive services for approximately 550,000 persons in Washington State and Northern Idaho. This study reports the experience of PCPs practicing within the integrated care delivery system that serves the Puget Sound region, within which GHC owns and operates 20 primary care clinics, four specialty centers, and one hospital. Each clinic contains a pharmacy (at which most enrollees receive their prescription medications), a laboratory, and imaging services. GHC contracts with the Group Health Permanente Medical Group (GHP), which provides care to enrollees within the integrated practice. GHC also contracts with thousands of providers and facilities that provide care to enrollees not enrolled in the integrated group practice.
Data Sources
All data used in this analysis are routinely collected and maintained by GHC or GHP. GHC has developed state-of-the-art health informatics systems that allow for detailed and extended longitudinal analyses of health care use among enrollees. These databases include complete eligibility, benefits, designated PCP, and home clinic, as well as diagnostic, procedural information, and ancillary services for all inpatient and outpatient encounters and prescription drug dispenses regardless of whether or not the patient is seen at a GHC-owned facility or by a GHP physician. Information about physician characteristics, including their age, gender, years in practice, and their FTE on a quarterly basis was obtained from GHP.
Data on cost of health care services provided to enrollees were obtained from an information system, which since January 1990 has captured and allocated health care costs for all services provided by GHP physicians at Group Health-owned and-operated facilities, as well as claims for covered services that enrollees receive from contracted providers or facilities. The cost-allocation system allows both the determination of costs of specific encounters and services and the aggregation of costs for individuals over time. Costs that are excluded from the allocation include those not directly related to the delivery of health services (e.g., costs of insurance administration, marketing costs) and patient out-of-pocket costs. GHC collects nominal cost data, and we adjust for inflation by stating dollar amounts in 2005 terms using the Seattle–Tacoma–Everett Medical Care Price Index maintained by the U.S. Bureau of Labor Statistics.
Data Set Creation
We collected data on all health care utilization and costs for GHC enrollees enrolled on a quarterly basis from January 1998 to December 2005, paneled to a GHP PCP with at least 0.25 FTE and at least 250 persons within their panel. An individual was considered to be enrolled during any quarter if they received care from Group Health under a medical contract for two or more months during that quarter. We created a physician-level data set that captured all WRVUs, FTE, ambulatory care office visits, secured messaging activity, and total costs of care for the PCP's adult and children panel members for each of the 32 quarters between 1998 and 2005.
Using enrollee-level information, we calculated mean age of panel members. We used the Resource Utilization Bands (RUB) of the Ambulatory Diagnosis Group software system to characterize the case mix of each provider's panel (Weiner et al. 1991). RUBs identify expected relative health care resource use on a six-point scale from 0 (low use) to 5 (high use). The case mix for each panel is identified through mean age, mean RUB, and percent female.
Regression Model Specification
We use regression analysis to estimate relative physician productivity using five specific measures as dependent variables: panel size, visits per FTE provider, WRVUs per visit, WRVUs per FTE, and cost of caring (PMPQ) for each provider's panel. The independent variables are identical in each equation. Physician-specific independent variables are gender, specialty, and years of practice in Group Health. Panel characteristics included in the model are mean age of panel members, percent female, and the mean RUB in the prior quarter. GHC does not retain clinic-specific or PCP-specific information on the physical capital (examining rooms, laboratory and imaging support, medical technology) or the labor inputs of nurses, medical assistants, and clerical staff supporting each PCP over time in the administrative databases used in this study. Therefore, fixed effects for clinic type and time and their interaction effects were included in our statistical models as surrogates for unmeasured labor and capital inputs.
We estimate productivity equations with repeated measures general estimating equations (GEE) using the GENMOD procedure within the SAS software system. Repeated measures GEE allows for missing data in a time series design; hence, physicians need not be represented during every quarter between January 1998 and December 2005. This approach supports complex variance structures caused by the intertemporal correlation of health care utilization and cost distributions that most closely fit the data. Robust standard errors are calculated using the “sandwich” estimator (Liang and Zeger 1986).
We divided the time series into three distinct periods. The baseline period from January 1998 through the second quarter (April–June) of 2002 is defined as pre-Initiative, before the rollout of the Initiative. The second, transition period, from mid-2002 through the third quarter of 2003, defines the months that GHC rolled out the Initiative. Time period 3 ending in the fourth quarter of 2005 marks the nine-quarter full implementation period.
To assess the Initiative's effect on physician productivity, we estimated regression-adjusted values for the five productivity measures for the three observed time periods defining GHC's intervention experience. We examined each productivity variable for pre-Initiative (baseline), rollout, and full implementation (post) periods and used the Contrast statement within GENMOD to test for differences in productivity across these periods. This allowed us to estimate the impact on productivity during each period and the net effect of full implementation relative to baseline and rollout.
RESULTS
Descriptive Statistics and Time Patterns
Table 1 provides information on PCPs whose productivity is examined. From January 1998 through December 2005, 352 PCPs maintained panels with at least 250 enrollees and practiced a minimum of 25 percent time during at least one quarter. The mean number of providers included in any quarter is 204 (SD 11.6, range 184–223). The majority of providers were men (57.4 percent) and had practiced within GHC for a mean of 13.8 years (median=14; SD=8.2).
Table 1.
Physician and Panel Characteristics: January 1998 to December 2005
| Physician characteristics (per quarter) | |
| N | 352 |
| Mean (SD) number of physicians with 0.25 FTE and minimum panel size of 250 per quarter | 204 (11.6) |
| Percent male | 57.4 |
| Mean (SD) years practicing in GHC (during each quarter) | 13.9 (8.2) |
| Mean FTE (SD) | 0.82 (.18) |
| Panel characteristics (per quarter) | |
| Mean per capita quarter total costs | 688.2 (244.5) |
| Mean work RVUs per physician FTE | 1,852.5 (1,005.9) |
| Mean work RVUs per visit | 1.9 (0.8) |
| Mean visits per physician FTE | 989.7 (343.5) |
| Panel size per FTE | 1,888.7 (580.6) |
FTE, full-time equivalent; GHC, Group Health Cooperative; RVU, relative value unit; SD, standard deviation.
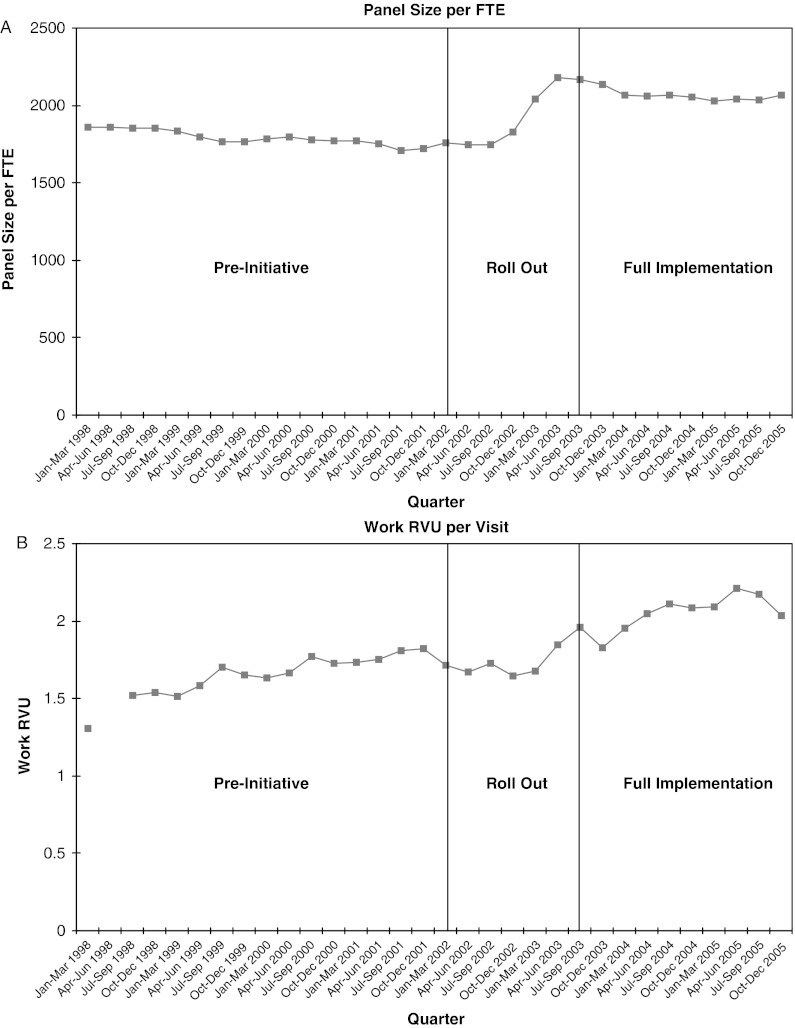
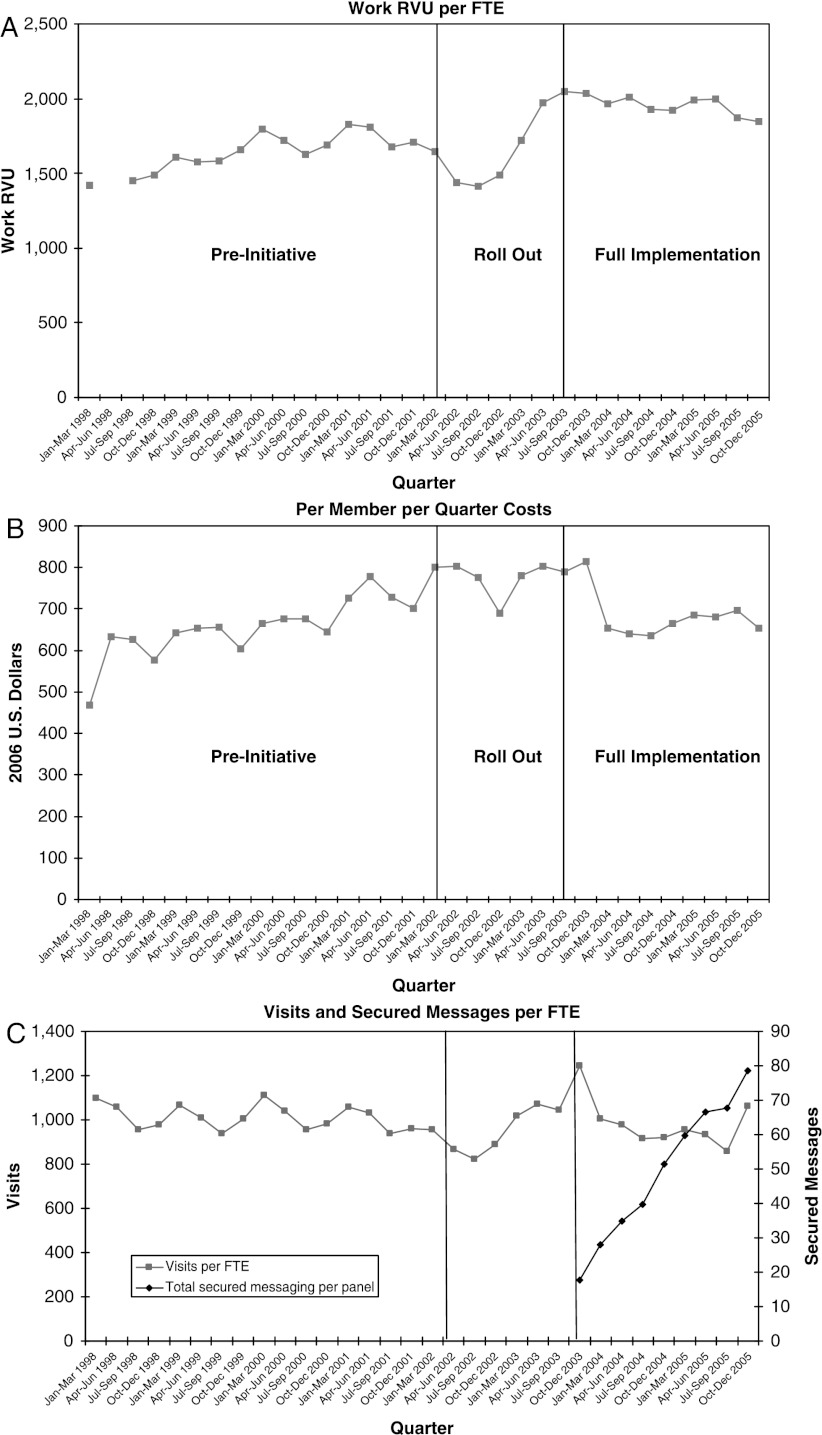
Quarterly plots of the selected dimensions of PCP productivity and clinical efficiency are displayed in Figures 1 and 2. Each figure is divided into pre-Initiative, rollout, and full implementation periods. Panel size per FTE is steady during baseline (pre-Initiative), rises toward the middle of the transition (rollout), and levels off during full implementation (post). Visit intensity rises in the latter quarters of rollout, continuing in the early and middle quarters of full implementation, before declining somewhat in the last two quarters of 2005. Figure 2C shows PCP ambulatory care office visits per FTE rising during rollout, followed by decline until an upward spike in the last quarter of full implementation, while secured messages per FTE rise steadily from their inception through the final quarter of 2005.
Figure 1.
(A) Panel Size per Full-Time Equivalent (FTE). (B) Work Relative Value Unit (RVU) per Visit.
Figure 2.
(A) Work Relative Value Unit (RVU) per Visit. (B) per Member per Quarter Costs. (C) Visits and Secured Messages per Full-Time Equivalent (FTE).
RVUs per FTE rise substantially from baseline through most of the transition, and then appear to level off during full implementation before declining somewhat in the last two quarters of 2005. PMPQ costs drift upward during the baseline period, remaining at historically high levels during rollout before declining in the second quarter of full implementation and remaining relatively flat thereafter.
Multivariate Analyses
To determine whether these changes in productivity and efficiency are plausibly attributable to the Access Initiative, we now proceed to multivariate analysis.
Table 2 summarizes the key GEE results, examining different views of PCP “productivity.” We report changes in each productivity dimension relative to Initiative (intervention) time, adjusting for model covariates: enrollee, provider, and practice characteristics. First, panel size per FTE rises significantly between baseline and rollout and between rollout and full implementation—for an increase of approximately 290 enrollees per FTE over the pre–post period. This net increase in panel size in the multivariate analysis matches the plots in Figure 1A. RVU per visit declines significantly between baseline and rollout, but rises significantly between rollout and full implementation, resulting in a significant net increase from baseline to rollout. This rise in visit intensity is mirrored in the descriptive plots of Figure 1B.
Table 2.
General Estimating Equation (GEE) Results
| Dependent Variables: Regression Coefficients (SE) |
|||||
|---|---|---|---|---|---|
| Independent Variables | Panel Size FTE | RVU Visit | Visit FTE | RVU FTE | PMPQ Cost |
| PCP years in group health | −2.53** | −0.0023 | 2.203 | −7.29*** | −1.337*** |
| (0.93) | (0.0014) | (1.23) | (1.71) | (0.413) | |
| PCP gender (female=1) | −146.11*** | −0.111** | −47.292 | −164.51** | 4.622 |
| (29.57) | (0.046) | (39.09) | (54.46) | (13.243) | |
| MD type (family practice=1) | 694.23*** | 0.112 | 153.09** | 395.14*** | 16.989 |
| (40.99) | (0.064) | (59.568) | (75.50) | (12.19) | |
| Panel case mix | |||||
| Panel % female | −690.63*** | −0.313** | 322.05** | −775.28*** | 31.059 |
| (87.97) | (0.14) | (147.88) | (220.58) | (38.366) | |
| Panel mean age | 35.63*** | 0.0088 | 1.918 | 13.37* | 8.649*** |
| (3.74) | (0.006) | (5.97) | (6.89) | (1.86) | |
| ACG case-mix score (mean RUB) | −249.58*** | −0.096 | 91.54** | 30.13 | 264.349*** |
| (33.5) | (0.052) | (41.17) | (61.79) | (18.289) | |
| Intervention time differences | |||||
| Post–rollout difference | 119.92*** | 0.33*** | −27.59*** | 237.25*** | −145.87*** |
| (33.79) | (0.02) | (13.14) | (25.16) | (6.47) | |
| Rollout–pre difference | 182.28*** | −0.09*** | −41.94*** | −166.93*** | 79.86*** |
| (36.12) | (0.02) | (13.51) | (28.87) | (5.58) | |
| Post–pre difference | 302.20*** | 0.24*** | −69.53*** | 70.32 | −66.01*** |
| (48.99) | (0.02) | (17.30) | (38.75) | (6.70) | |
| N (physician quarters) | 6,539 | 6,539 | 6,539 | 6,539 | 6,539 |
| Log likelihood | −50,337.32 | −8,052.68 | −47,118.35 | −54,330.78 | −40,551.33 |
Significant at p<.001.
Significant at p<.01.
Significant at p<.05.
FTE, full-time equivalent; RVU, relative value unit; PMPQ, per member per quarter; PCP, primary care physician; RUB, Resource Utilization Bands; ACG, Ambulatory Diagnosis Group; SE, standard error.
Adjusted for model covariates, visits per FTE decline significantly from baseline to rollout and from rollout to full implementation. In contrast to these multivariate results, the plot of visits per FTE (Figure 2C) shows little net change over the pre–post period. RVU per FTE dropped substantially between baseline and rollout, and then rebounded significantly between rollout and full implementation; however, the net increase between baseline and full implementation was not statistically significant. These RVU per FTE multivariate findings again contrast with the descriptive plots in Figure 2A, which suggest an increase from baseline to rollout—the higher level persisting during full implementation.
After rising between baseline and rollout, PMPQ cost drops sufficiently between rollout and full implementation to post a significant net decline between baseline and full implementation. These multivariate results are similar to the time pattern of the PMPQ plots in Figure 2B.
The relationship between physician years of experience in Group Health and productivity and PMPQ cost is negative for all five dependent measures—significantly so for panel size, RVU per FTE, and PMPQ cost. Coefficients for female physicians are significantly negative for all four productivity measures, but insignificantly positive for PMPQ cost. Family practice physicians have significantly larger panels, and more visits and RVUs per FTEs.
PCPs caring for a higher proportion of women have substantially smaller panels, lower RVUs per visit and per FTE, but significantly higher visits per FTE. PCPs with older panels have larger panels and higher levels of RVU per FTE and PMPQ cost, other things being equal. Controlling for model covariates and these other two panel characteristics, physicians caring for more resource-intensive patients have significantly smaller panels, more visits per FTE, and higher PMPQ costs.
CONCLUSIONS
The findings of this study suggest that implementation of a major, organization-wide access intervention in an integrated group practice was related to change in several dimensions of PCP productivity from baseline to full implementation: significant increases in average panel size per PCP (FTE) and resource intensity per visit, accompanied by reduced visits per FTE and decreased PMPQ cost. Net change in resource provision (RVU) per PCP was positive over the study period, but neither large nor statistically significant.
The decline in RVU per FTE and the rise in PMPQ cost between the baseline and rollout period are consistent with the results of qualitative interviews with physicians and discussions with management. The transition period involved substantial organizational change (seven intervention components) over 18 months. One would expect practitioners and managers to confront significant adjustment costs due to new electronic information systems, practice redesign, alterations in PCP compensation, changes in support staffing, time invested in additional clinical documentation, open access scheduling, and the introduction of patient self-referral to most specialties. In that sense, it may not be surprising that even the large burst in RVU productivity per FTE between the rollout and full implementation period was not sufficient to produce a net increase in RVU per FTE over the pre–post period. Interestingly, the significant post-rollout drop in PMPQ cost was enough to yield a net pre–post decline in cost.
In the absence of a comparable “control group” organization, it is impossible to infer direct causal effects of the Initiative on PCP productivity, but the significant increases in panel size, improvements in clinical efficiency (PMPQ cost), and increased resource intensity per visit are at least plausibly attributable to the intervention. The decline in visits per FTE PCP over the study period is a possible side effect of the “direct access” (enrollee self-referral to specialty care) aspect of the Initiative, which resulted in reduced primary care visits per enrollee. Such demand-side influences in the HMO may have indirectly affected PCP visit productivity. Although we did not aggregate secure messaging with “face-to-face” utilization counts, the substitution of secure messaging for ambulatory encounters during the latter periods may explain some of the decline in visits per FTE in the latter periods. Finally, the transitory increase in PMPQ cost between baseline and rollout did not continue; in fact, PMPQ costs declined significantly from pre to post—a pattern consistent with a net increase in clinical efficiency of PCPs, especially between the rollout and full implementation periods.
The broad purview of productivity dimensions examined in this study allows one to draw a rich portrait of physician response to the intervention. Even as the Access Initiative may have marginally reduced the demand for primary care visits, PCPs appear to have adjusted by increasing panel size and visit intensity, while simultaneously improving clinical efficiency. Because PMPQ costs were case-mix adjusted, and the observational time frame was relatively long, it seems unlikely that the diminution in per capita costs was achieved by compromising quality.
Combining the general pattern of results from this study with those of similar research based on a large prepaid multispecialty group practice in Minnesota (Lewandowski et al. 2006), it appears that a multifaceted intervention focused on changed PCP incentives, primary care redesign, systematic open-access changes in patient scheduling, and HIT has the potential to significantly enhance provider productivity and clinical efficiency. In future implementation, it would be particularly helpful to phase-in components of such initiatives and to follow performance in comparable, “control” organizations. In particular, given the rapid evolution of HIT and secure electronic mechanisms for provider–patient interaction, isolating the effects of those innovations on provider productivity would be especially informative. In general, such controlled, before–after and interrupted time series designs would allow one to better differentiate the impact of individual intervention components and to distinguish causal effects from secular change.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The project of which this paper is one component was supported by a grant from the Robert Wood Johnson Foundation Health Care Financing and Organization (HCFO) Initiative. Creative and highly competent computing and data management support was provided by David Carrell and Julia Hecht, and critical administrative support was delivered by Christine Mahoney and Hang Su of the Group Health Center for Health Studies.
Disclosures: The corresponding author and coauthors have no financial interests or conflicts of interest that might otherwise influence the results of this study and their interpretation.
Disclaimer: While acknowledging the grant support from the Robert Wood Johnson Foundation and the institutional support from colleagues at the University of Washington and Group Health Center for Health Studies, the authors are solely responsible for the study design, implementation, results, and judgments presented in this paper.
Supplementary material
The following supplementary material for this article is available online:
Appendix SA1. Author matrix.
This material is available as part of the online article from http://www.blackwell-synergy.com/doi/abs/10.1111/j.1475-6773.2008.00880.x (this link will take you to the article abstract).
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Blumenthal D, Glaser JP. Health Policy Report: Information Technology Comes to Medicine. New England Journal of Medicine. 2007;356(24):2527–34. doi: 10.1056/NEJMhpr066212. [DOI] [PubMed] [Google Scholar]
- Chaudry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care. Annals of Internal Medicine. 2006;144:742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- Conrad DA, Sales A, Liang SY, Chaudhuri A, Maynard C, Pieper L, Weinstein L, Gans D, Piland N. The Impact of Financial Incentives on Physician Productivity in Medical Groups. Health Services Research. 2002;37(4):885–906. doi: 10.1034/j.1600-0560.2002.57.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaynor M, Gertler PJ. Moral Hazard and Risk-Spreading in Partnerships. RAND Journal of Economics. 1995;26(4):591–613. [Google Scholar]
- Gaynor M, Pauly MV. Compensation and Productive Efficiency in Partnerships: Evidence from Medical Group Partnerships. Journal of Political Economy. 1990;98:544–73. [Google Scholar]
- Goodman DC. Perspective: Do We Need More Physicians? Health Affairs. 2004;23(Supplement 1):W4-67–W4-69. doi: 10.1377/hlthaff.w4.67. Web Exclusive. [DOI] [PubMed] [Google Scholar]
- Hurdle S, Pope GC. Physician Productivity: Trends and Determinants. Inquiry. 1989;26(1):100–15. [PubMed] [Google Scholar]
- Institute of Medicine. Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Kimball LJ, Lorant JH. Physician Productivity and Returns to Scale. Health Services Research. 1977;12(4):367–79. [PMC free article] [PubMed] [Google Scholar]
- Lewandowski S, O'Connor PJ, Solberg LI, Lais T, Hroscikoski, Sperl-Hillen JM. Increasing Primary Care Physician Productivity: A Case Study. American Journal of Managed Care. 2006;12(10):573–6. [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal Data Analysis Using Generalized Linear Models. Biometrika. 1986;73:13–22. [Google Scholar]
- Liederman EM, Lee JC, Baquero VH, Seites PG. The Impact of Patient–Physician Web Messaging on Provider Productivity. Journal of Healthcare Information Management. 2005;19(2):81–6. [PubMed] [Google Scholar]
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The Quality of Health Care Delivered to Adults in the United States. New England Journal of Medicine. 2003;348:2635–45. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- Pauly MV. Economics of Multispecialty Group Practice. Journal of Ambulatory Care Management. 1996;19(3):26–33. doi: 10.1097/00004479-199607000-00004. [DOI] [PubMed] [Google Scholar]
- Pope GC. Physician Inputs, Outputs, and Productivity, 1976–1986. Inquiry. 1990;27(2):151–60. [PubMed] [Google Scholar]
- Ralston JD, Grembowski DE, Fishman P, Martin DP, Conrad DA, Larson EB. Group Health Cooperative's Transformation to Patient-Centered Access. Managed Care Interface. 2008 doi: 10.1177/1077558709338486. forthcoming. [DOI] [PubMed] [Google Scholar]
- Silberberg E. The Structure of Economics: A Mathematical Analysis. New York: McGraw-Hill; 1990. [Google Scholar]
- Weeks WB, Wallace AE. Time and Money: A Retrospective Evaluation of Inputs, Outputs, Efficiency, and Incomes of Physicians. Archives of Internal Medicine. 2003;163:944–8. doi: 10.1001/archinte.163.8.944. [DOI] [PubMed] [Google Scholar]
- Weiner JP. Prepaid Group Practice Staffing and U.S. Physician Supply: Lessons for Workforce Policy. Health Affairs. 2004;23(Suppl 1):W4-43–W4-59. doi: 10.1377/hlthaff.w4.43. Web Exclusives. [DOI] [PubMed] [Google Scholar]
- Weiner JP, Starfield BH, Steinwachs DM, Mumford LM. Development and Application of a Population-Oriented Measure of Ambulatory Care Case-Mix. Medical Care. 1991;29(5):452–72. doi: 10.1097/00005650-199105000-00006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.