Abstract
Fransicella tularensis, the causative agent of tularemia, is in the top category (Category A) of potential agents of bioterrorism. To develop a safer vaccine against aerosolized F. tularensis, we have employed an attenuated Listeria monocytogenes, which shares with F. tularensis an intracellular and extraphagosomal lifestyle, as a delivery vehicle for F. tularensis antigens. We constructed recombinant L. monocytogenes (rLm) vaccines stably expressing 7 F. tularensis proteins including IglC (rLm/iglC), and tested their immunogenicity and protective efficacy against lethal F. tularensis challenge in mice. Mice immunized intradermally with rLm/iglC developed significant cellular immune responses to F. tularensis IglC as evidenced by lymphocyte proliferation and CD4+ and CD8+ T-cell intracellular expression of interferon gamma. Moreover, mice immunized with rLm/iglC were protected against lethal challenge with F. tularensis LVS administered by the intranasal route, a route chosen to mimic airborne infection, and, most importantly, against aerosol challenge with the highly virulent Type A F. tularensis SchuS4 strain.
Keywords: Tularemia vaccine, Francisella tularensis, Listeria monocytogenes, and Biodefense
1. Introduction
Francisella tularensis is a gram-negative coccobacillus that causes tularemia, a zoonotic disease spread among small animals by blood sucking insects. There are four subspecies of F. tularensis: tularensis (Type A), holarctica (Type B), mediasiatica, and novicida. Of these, subsp. tularensis, found in North America, causes the most severe disease. Depending largely upon the mode of F. tularensis transmission, there are several forms of tularemia, including ulceronodular, typhoidal, and pneumonic, the most dangerous form as it carries a high fatality rate. Under natural circumstances, F. tularensis rarely infects humans. However, because it is one of the most pathogenic human pathogens known and can be spread by the airborne route to cause a highly fatal form of pneumonia, F. tularensis is classified as a Category A agent of bioterrorism, i.e. among the most likely pathogens to be employed in a bioterrorist attack. Indeed, F. tularensis has a long history of development as a bioweapon, having been stockpiled as a biowarfare agent by Japan in World War II [1] and by the U.S. and Soviet Union during the Cold War [2, 3].
Several vaccine strategies have been developed against virulent F. tularensis infection, including killed whole cell vaccines, subunit vaccines, live attenuated Type A strains and live attenuated non-Type A strains [4]. Killed whole cell vaccines have not afforded high-level protection against Type A F. tularensis in animal models [5, 6]. Subunit vaccines comprising an F. tularensis protein in an adjuvant formulation or F. tularensis lipopolysaccharide (LPS) purified from the Live Vaccine Strain (LVS) have not demonstrated high-level efficacy against non-Type A or virulent Type A F. tularensis in animal models [7–10]. Intraperitoneal immunization with an F. tularensis LVS outer membrane protein preparation protected 50% of mice challenged intranasally (i.n.) with Type A SchuS4 [11]. A spontaneous attenuated mutant of Type A F. tularensis SchuS4 strain was shown to be able to induce protective immunity [12]; however, attenuated Type A strains carry a potential risk of reversion to virulence. A purified auxotroph of F. tularensis SchuS4 was recently found to give poor protection against i.n. challenge with the homologous parental organism and no better than an analogous purine auxotroph of the Type B LVS strain [13].
LVS is a live attenuated strain of F. tularensis subsp. holarctica, a relatively mild subsp. of F. tularensis. It was approved as an investigational new drug by the U.S. FDA and has been studied extensively in humans. However, there are several major limitations for LVS as a vaccine against tularemia [4, 5]. First, it retains significant toxicity, even when administered by the intradermal (i.d.) route. Second, when administered by the relatively safe i.d. route, it provides incomplete protection against high dose aerosol challenge. Third, the underlying mechanism of attenuation is poorly characterized genetically making it difficult to assess the likelihood of reversion to virulence. Fourth, it displays a mixed colony morphology type (blue/grey colonies), and only one colony type induces protective immunity [14]. Recently, efforts have been made to further attenuate the LVS strain for vaccine purposes. However, several such mutants were unable to induce protective immunity against Type A strains [15–17]. Efforts have also been made to improve the vaccine’s efficacy by administering it by aerosol. While highly efficacious by the aerosol route, it was much more virulent, with most volunteers developing typhoidal tularemia [18].
Macrophages are the major host cells for F. tularensis [19]. Other cell types, e.g. hepatocytes, type II alveolar epithelial cells, and neutrophils can also serve as host cells for F. tularensis [20–22]. After entering human mononuclear phagocytes, both the highly virulent F. tularensis Type A and the F. tularensis LVS strain briefly inhabit a phagosome and then exit the phagosome and multiply free in the cytoplasm [23, 24]. Precise correlates of protective immunity against Type A F. tularensis challenge have not been defined. In the mouse, the LVS vaccine, which offers substantial protection against Type A F. tularensis, induces both humoral and cell-mediated immune responses, including CD4+ and CD8+ T-cell responses, to F. tularensis antigens [25].
In search for a safer vaccine against F. tularensis infection, we chose to use an attenuated heterologous intracellular bacterium, Listeria monocytogenes, as a live vaccine vector to express F. tularensis immunogenic proteins. L. monocytogenes is a facultative intracellular bacterium. It expresses cell-surface and secreted proteins that enable attachment to host cells, escape from the phagosome and movement in the cytosol of the invaded cells. Listeriolysin O (LLO) and actin-assembly-inducing protein (ActA), encoded by L. monocytogenes hly and actA genes, respectively, are both secreted proteins and virulence factors. LLO lyses the phagosomal membrane and mediates the invasion of the cytosol, triggering innate and adaptive immune responses. ActA propels bacteria through the cytoplasm and into neighboring cells. ActA-deficient L. monocytogenes strains are highly attenuated. However, vaccination with ActA-deficient L. monocytogenes induces innate immune responses and primes protective T-cell responses [26]. The parental L. monocytogenes strain selected in this work [Strain 10403S (serotype 1/2a)] was previously employed as a vaccine delivery vehicle for antigenic cancer proteins and an actA/pclB-deletion mutant of this strain has been demonstrated safe in humans [27, 28]. ActA-deficient L. monocytogenes is cleared within 7 days of administration [29] and pre-existing anti-listerial immunity does not affect therapeutic efficacy [30]. Using the highly attenuated recombinant ActA-deficient form of the L. monocytogenes strain (rLmΔactA), we constructed recombinant L. monocytogenes strains in which the F. tularensis genes were fused to the signal sequence and promoter of hly, such that the F. tularensis antigens expressed by the recombinant L. monocytogenes should be released into the cytosol of the infected host cells.
For F. tularensis antigens, we focused on seven major F. tularensis proteins: AcpA, Bfr, DnaK, GroEL, KatG, IglC, and Pld. AcpA (57 kDa) is a highly expressed respiratory-burst-inhibiting acid phophatase that exhibits some phospholipase C activity and shows no significant global amino acid sequence similarity to any other protein [31]. In F. tularensis subsp. novicida, AcpA is a virulence determinant [32]. Catalase-peroxidase (KatG) is an 80-kDa protein abundantly secreted into the culture filtrate of virulent F. tularensis and exhibits a functional signal peptide [33]. Bacterioferritin (Bfr), DnaK, and GroEL are also among the most abundant proteins in the culture filtrate of F. tularensis [33]. IglC is a 23-kDa protein encoded by the iglABCD operon in the Francisella Pathogenicity Island (FPI) [34], and shows no similarity to other known prokaryotic proteins. It is one of the most upregulated F. tularensis proteins during intracellular infection of macrophages, and is required for intracellular survival, replication and phagosome escape of F. tularensis [35–38]. Studies on iglC mutants in F. tularensis subsp. novicida, holarctica, and tularensis demonstrated that IglC is essential for virulence in mice [12, 39, 40]. Lastly, phospholipid D (Pld) belongs to the Pld superfamily that includes enzymes involved in signal transduction, lipid biosynthesis, and endonuclease activity in pathogenic viruses and bacteria, although the function of Pld in F. tularensis is not known.
L. monocytogenes shares with F. tularensis an intracellular and extraphagosomal (cytoplasmic) life style; hence F. tularensis antigens released by recombinant L. monocytogenes should be processed and presented in a way similar to antigens released by intracellular F. tularensis during infection. Our previous work has demonstrated that major secretory proteins of other intracellular pathogens, including Legionella pneumophila, Mycobacterium tuberculosis and Mycobacterium bovis, induce potent protective immunity against challenge with these organisms [41–43].
In this study, using recombinant L. monocytogenes as a delivery vector for F. tularensis proteins, we show that a) F. tularensis antigens expressed by the recombinant L. monocytogenes induce strong cell-mediated immune responses; b) animals immunized i.d. with recombinant L. monocytogenes expressing the F. tularensis protein IglC (rLm/iglC) are protected against lethal i.n. challenge with F. tularensis LVS, and c) most importantly, animals immunized i.d. with rLm/iglC are protected against lethal aerosol challenge with the highly virulent F. tularensis Type A SchuS4 strain.
2. Methods
2.1. Cell lines, bacteria, and mice
Human macrophage-like THP-1 cells (ATCC TIB-202) were cultured in RPMI 1640 containing penicillin (100 μg/ml) and streptomycin (100 U/ml) and supplemented with 10% FBS. F. tularensis LVS, SchuS4 and a virulent recent clinical isolate (RCI) of Type A strain (NY 96-3369) were obtained from the Centers for Disease Control and Prevention (Atlanta, Ga.). The bacteria were passaged once on monolayers of THP-1 cells, followed by amplification on chocolate II agar (BD BBL, Sparks, MD) for 3 days. The bacteria were then scraped from colonies on plates, suspended in sterile saline in the presence of 20% glycerol, and stored at −80°C. The F. tularensis RCI strain was used to isolate genomic DNA that served as a template for PCR amplification of Type A F. tularensis genes. The F. tularensis LVS strain served as a positive control for recombinant L. monocytogenes vaccines and was used to challenge mice by i.n. route. The F. tularensis SchuS4 strain was used to challenge mice by the aerosol route. Before each use in animals, one vial of LVS or SchuS4 was thawed immediately at 37°C, diluted in sterile saline and kept on ice until use.
Six to eight week old female BALB/c mice were purchased from Charles River Laboratory (Wilmington, MA), maintained in a specific-pathogen-free animal facility, and used according to protocols approved by the Animal Research Committees of UCLA and CSU.
2.2. Construction of recombinant L. monocytogenes vaccine candidates
The attenuated L. monocytogenes host strain, rLmΔactA, was generously provided by K. Bruhn and J. F. Miller at UCLA [27]. The coding nucleotide sequences for F. tularensis AcpA, Bfr, DnaK, GroEL, IglC, Pld and the mature peptide of KatG were PCR amplified from the genomic DNA of the RCI strain using primer pairs listed in Table 1 and cloned into the plasmid, pZErO (Invitrogen). The inserted nucleotides were confirmed by nucleotide sequencing, all of which were identical to those of the SchuS4 strain. The F. tularensis genes were subcloned into the vector pKB199, in which the F. tularensis gene was fused in frame with the promoter and signal sequence of L. monocytogenes hly. Each F. tularensis protein expression cassette was then excised from the cloning vector pKB199 by NotI and ligated to the NotI site of a phage-based Listeria site-specific integration vector pDP4189, which was subsequently transformed into SM10, the E. coli conjugation donor strain. Through conjugation, the plasmid was mobilized and transferred from its E. coli SM10 host into the recipient rLmΔactA strain. The conjugation mixture was selected on plates containing streptomycin (200 μg/ml) and chloramphenicol (7.5 μg/ml). The rLmΔactA strain is insensitive to streptomycin since it is derived from the L. monocytogenes strain 10403S, a spontaneous mutant resistant to streptomycin. E. coli SM10 is sensitive to streptomycin and therefore is not able to grow on the selective plate. The plasmid pDP4189 carries the chloramphenicol resistance gene and is unable to replicate in L. monocytogenes. Under the selection pressure from chloramphenicol, the integration vector containing the F. tularensis protein expression cassette driven by the hly promoter was integrated into the 3′ end of an arginine tRNA gene on the chromosome of the rLmΔactA strain. The resulting recombinant L. monocytogenes strains were verified by colony PCR using two pairs of primers specific for amplifying across the bacterial attachment site tRNAarg-attBB′ and across the hybrid attachment site tRNAarg-attBP′, respectively, as described previously [44], and one pair of primers specific for F. tularensis gene.
Table 1.
List of primers for amplifying nucleotide sequences encoding F. tularensis proteins
| Primer Pairs | Gene Amplified | Nucleotide sequence (5′ to 3′)* |
|---|---|---|
| 1F | acpA | CGGGATCCAAGCTCAATAAAATTACTTTAGGAATTTTAAGTCTA |
| 1R | acpA | CGGGATCCTTAGTTTAATTTATCCACTACTAATCCTGTCTTAGGGTC |
| 2F | Bfr | CGGGATCCAGAACTTCAATTAGAAAATAAACAAGAAATTATTGATCAA |
| 2R | Bfr | CGGGATCCTTATGCAGGTTTTCTTAACATTTTTTCTACTTCACCAATGTGCGT |
| 3F | dnaK | GCCCGGATCCCGGAAAAATAATAGGTATAG |
| 3R | dnaK | CCGCGTTAATTAAGCGGCCGCTTATTTTTTGTCGTCTTC |
| 4F | GroEL | CGGGATCCGGCTGCAAAACAAGTTTTATTTTCAGATGAAGCTC |
| 4R | GroEL | CGGGATCCCTATTACATCATGCCAGGCATACCGCCCATGCCACCGCC |
| 5F | katG | CATCGGATCCTGAAGATACCACAACGAAAAATGATAATCTTTCACCACAGAGCGTAGA |
| 5R | katG | CCTTAATTAAGCGGCCGCTTATTGTTGAACATCAAATCTGCCAAGCATCATAACTTTATGCCAAGC |
| 6F | iglC | CGGGATCCTAGTGAGATGATAACAAGACAACAGGTAACAAGTGGC |
| 6R | iglC | CGGGATCCTTACTATGCAGCTGCAATATATCCTATTTTAGCAACTCCTTTATCT |
| 7F | pld | CGGGATCCTCATGGAATTACTAAAACAATAGTACACAACTATCCTG |
| 7R | pld | CGGGATCCTTAGGTACAAGACGGAGTTGATATTATACCAACAG |
, Underlined sequences are restriction enzyme sites used for cloning F. tularensis nucleotide sequences into the vector pZErO.
2.3. Stability of recombinant L. monocytogenes strains
The stability of the recombinant L. monocytogenes integrants under nonselective growth conditions was tested by passaging 20 times each of the seven recombinant L. monocytogenes strains (25 colonies each) on Brain-Heart Infusion (BHI) plates in the absence of antibiotics. After every 5 passages, the 25 colonies were tested for growth on BHI plates containing 7.5 μg ml−1 of chloramphenicol and 50 μg ml−1 of streptomycin. At the end of stability test, one colony from each strain was tested for relevant F. tularensis protein expression in the culture filtrate.
2.4. Extracellular expression of F. tularensis proteins by recombinant L. monocytogenes
A single colony of each recombinant L. monocytogenes strain was inoculated into 3 ml BHI medium containing streptomycin and chloramphenicol and the bacteria were grown overnight at 37°C with shaking. The overnight culture was inoculated into 40 ml fresh MOPS-buffered BHI medium containing streptomycin and chloramphenicol at an initial optical density (OD) of 0.05 at 540 nm. The culture was grown until late logarithmic phase at 37°C with vigorous shaking before being harvested by centrifugation. The supernate was passed through a 0.2 μm filter membrane, and proteins in the culture filtrate were precipitated by trichloroacetic acid. The expression of F. tularensis proteins was analyzed by Western blotting using rabbit polyclonal antibody against the relevant protein.
2.5. Intracellular expression of F. tularensis proteins by recombinant L. monocytogenes
THP-1 cells were differentiated into a monolayer on a 24-well plate (2 × 105 cells/well) in the presence of 100 nM PMA (phorbol 12-myristate 13-acetate) and in the absence of antibiotics. The recombinant L. monocytogenes expressing IglC (rLm/iglC) or KatG (rLm/katG) culture was grown to late logarithmic phase (OD of 1.0 at 540 nm) in BHI broth and used to infect the THP-1 cell monolayer at a multiplicity of infection (MOI) of 50:1. After infection for 1 h at 37°C, the monolayer was washed twice with RPMI to remove extracellular bacteria and then treated with 1 ml medium containing gentamicin at a final concentration of 10 μg ml−1 to kill any remaining extracellular bacteria. At 24 h post-infection, cells were harvested, washed once with PBS, and boiled for 7 min in Laemmli buffer before analysis by SDS-polyacrylamide gel electrophoresis (SDS-PAGE) and Western blotting.
2.6. Recombinant protein expression, purification and antibody production
Recombinant AcpA, Bfr, DnaK, GroEL, KatG and Pld were expressed as fusion proteins tagged with 6 histidine residues in the N- or C-terminus of the protein. Purification of recombinant Bfr, GroEl and KatG has been described previously [33]. Recombinant AcpA was purified as described previously for KatG [33]. DnaK and PldD were purified as described for Bfr and GroEL [33]. The gene for IglC was PCR amplified from RCI genomic DNA, cloned into pZErO (Invitrogen) and sequence verified before it was subcloned into pTWIN1 vector (NEB) in such a way that it fused to the 3′ end of a chimeric gene sequence on the plasmid vector to generate pTWIN-iglC. The chimeric gene on pTWIN1 consists of the coding sequence for a chitin binding domain (CBD) and a DnaB intein. Therefore IglC was expressed as a CBD-DnaB intein-IglC fusion protein. The purification of IglC was carried out by chitin affinity chromatography, sequential elution with buffers of decreasing pH as recommended by the manufacturer, and by Q-Sepharose chromatography. The purity of the recombinant proteins was assessed by SDS-PAGE. IglC and KatG were tested for endotoxin level with an E-Toxate kit (Sigma) following the manufacturer’s instructions and had on average 0.3125 and 0.75 EU/μg, respectively. Purified recombinant proteins were used to immunize rabbits for antibody production (Covance, Denver, PA).
2.7. Western blot analysis
Protein expression by recombinant L. monocytogenes was analyzed by Western blotting using rabbit polyclonal antibodies specific to AcpA, Bfr, DnaK, GroEL, IglC, KatG, or Pld at a dilution of 1:5,000 and subsequently horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin G (Bio-Rad) at a dilution of 1:25,000. The blots were incubated with chemiluminescent substrate (Pierce) and the proteins were detected by exposing film to the blot.
2.8. Vaccination and challenge
Mice were vaccinated i.d. once, or twice at an interval of 4 or 5 weeks, at the base of the tail with each vaccine strain diluted in 50 μl sterile saline using 27G 1/2 cc Tuberculin syringes (Becton Dickson, NJ). Mice vaccinated with 50 μl of sterile saline served as negative control (Sham). Mice vaccinated with 1 to 5 × 104 CFU LVS served as positive control. Four weeks or later after the last vaccination, mice were challenged. We employed two mouse challenge models. Mouse challenge model I was used to screen vaccines in an ABSL2 Facility. Mice were challenged with a lethal dose of LVS by the i.n. route, a route chosen to mimic airborne infection. In initial studies, we used Isoflurane (Phoenix Pharmaceutical Inc. MO) to anesthetize mice. Subsequently we changed to Ketamine (80 mg/kg) and Xylazine (10 mg/kg) administered by intraperitoneal (i.p.) injection. The i.n. challenge was administered by pipetting F. tularensis LVS in a total volume of 20 μl sterile saline into the nostrils of mice. Mouse challenge model II was used for definitive tests of vaccines for efficacy in an ABSL3 Facility at Colorado State University. The aerosol challenge was conducted in a chamber of 5 cubic feet with the mice conscious and active, using a Glas-Col Inhalation Exposure System (Glas-Col, LLC, Terre Haute, IN). The estimated 1× and 10× LD100 dose for the SchuS4 strain was obtained by aerosolizing 5 ml of a suspension containing 3 or 30 million CFU/ml bacteria, respectively (15 or 150 million total bacteria, respectively) over a period of 15 minutes. Challenged mice were weighed and monitored daily for illness and death for 3 weeks. Mice that were moribund after challenge were euthanized and counted as a death. Mean time-of-survival (MTS) was calculated by dividing the sum of the surviving days of all mice by the total number of mice examined, with surviving animals given a time of 21 days, when the experiment was terminated.
To quantitate bacterial burden in host tissues, mice were euthanized at the indicated times post-infection. Liver, spleen and lung were removed aseptically and immediately homogenized in 2 ml sterile saline with a Pro200 Homogenizer (PRO Scientific Inc. Oxford, CT). Serial 10-fold dilutions of the homogenates were plated onto Chocolate agar plates containing sulfamethoxazole (40 μg/ml), trimethoprim (8 μg/ml) and erythromycin (50 μg/ml) [45], and incubated in a 5% CO2 incubator at 37°C for three days before colonies were enumerated.
2.9. Assay for lymphocyte proliferation and intracellular cytokine staining
Groups of BALB/c mice were sham-immunized or immunized with different vaccines twice at an interval of 3 to 5 weeks. At various times after the last vaccination, mice were anesthetized by i.p. injection of Ketamine and Xylazine and euthanized. Spleens were removed and splenocytes were prepared using PharmLyse (BD) according to the manufacturer’s instruction. A single suspension of splenocytes was seeded in U-bottom 96-well plates in duplicate at 2 × 106 cells per 0.1 ml per well in RPMI medium containing 10% FBS, polymyxin B (100 U/ml) in assays of lymphocyte proliferation (to inhibit any effect of endotoxin) or interleukin 2 (50 U/ml) in assays of intracellular cytokine staining, and cultured with or without purified recombinant proteins (10 μg/ml). Splenocytes from each animal cultured with concanavalin A (10 μg/ml) served as internal controls in the lymphocyte proliferation assay and splenocytes cultured with phorbol 12-myristate 13-acetate (PMA) and calcium ionophomore (A23187, Sigma) served as internal controls in the assay for intracellular cytokine staining. Lymphocyte proliferation was assayed as described previously with modifications [33]. Briefly, after 48 h of incubation, splenocytes were pulsed with 0.25 μCi of methyl-[3H]thymidine (Amersham Pharmacia Biotech) per well and harvested 2 h later with a cell harvester (Skatron). The amount of incorporated [3H]thymidine was determined by counting in a liquid scintillation counter. The stimulation index (SI) was defined as the ratio of the counts per minute obtained from cells incubated with the purified protein divided by the counts per minute obtained from cells incubated without protein. The mean SI for triplicate wells for each mouse was then computed and the mean SIs for three mice per group were averaged.
Intracellular cytokine staining was performed at day 6 after the last vaccination as described previously [33], using antibodies purchased from BD Biosciences Pharmingen. Briefly, after 24 h incubation, Golgi-Plug (BD Pharmingen) was added and incubated with cells for an additional 11 h at 37°C in a 5% CO2 incubator. Cells were pelleted at 250 × g for 5 min and resuspended in staining buffer (BD Pharmingen) containing Fc-Block (BD Pharmingen). After incubation for 15 min, cells were stained with fluorescein isothiocyanate (FITC)-labeled anti-CD4 or PE-Cy5-labeled anti-CD8 antibody at a 1:100 dilution for 30 min, washed twice in staining buffer, fixed with Cytofix solution for 20 min, and washed twice with Perm/Wash solution. Cells were then stained for intracellular interferon gamma (IFNγ) with PE-labeled rat anti-mouse IFNγ or a PE-labeled isotypic control immunoglobulin G at a dilution of 1:100. All the incubations were performed on ice in the dark. Stained cells were washed, resuspended in staining buffer, and analyzed on a FACSCalibur flow cytometer using CellQuest software.
2.10. Serum antibody detection by ELISA
In a separate experiment, mice were sham-immunized or immunized twice at weeks 0 and 4. Sera were collected at 4 weeks after the last vaccination and assayed for antibodies specific to F. tularensis proteins by ELISA. Briefly, 96-well EIA/RIA plates (Corning, NY) were coated or not coated with recombinant IglC or KatG (10μg/ml) in carbonate buffer overnight at 4°C. Excess antigen was removed by washing three times with PBS. Sera were diluted in PBS containing 1% bovine serum albumin. Sera at a starting dilution of 1:25 were titrated in duplicate wells through a two-fold dilution series down a row of twelve wells coated or not coated with proteins. The plates were incubated at ambient temperature for 3 h, and washed three times with TBS (0.05M Tris-HCl pH 7.4, 0.15M NaCl). The plates were subsequently incubated for 90 min at ambient temperature with alkaline phosphatase-conjugated goat anti-mouse IgG (Sigma, St. Louis, MO) at a dilution of 1:1000. The plates were washed three times after each incubation. One hundred μl of p-nitrophenylphosphate substrate in diethanolamine buffer (Phosphatase Substrate kit, BioRad, Hercules, CA) was added to each well. The yellow color that developed was read at 414 nm for absorbance using a multiscan microplate reader (TiterTek, Huntsville, AI). A dilution curve was plotted for the response to KatG protein. Sera from LVS-immunized animals at dilutions of 1:25 to 1:1,600 showed a linear increase in absorbance at 414 nm (A414 nm) when incubated with the KatG protein. Sera from rLm/katG immunized animals showed linear reading only with lower dilutions (1:25 to 1:200). Overall, the A414 nm ranged from 0.1 to 0.25 and from 0.1 to 1 in the absence and in the presence of KatG, respectively. In contrast, A414 nm was below 0.25 for all serum dilutions when incubated with IglC protein. For comparison, levels of serum antibody specific to KatG and IglC were determined by dividing the A414 nm in the presence of protein by the A414 nm in the absence of protein at dilutions of 1:50 and 1:25, respectively.
2.11. Statistical analyses
The student t-test was used to determine significance in comparisons of mean SIs of lymphocyte proliferative responses in the initial screening assay. Subsequently, one-way ANOVA with Bonferroni’s post test was performed using GraphPad Prism version 5.01 (San Diego, CA) to determine significance in comparisons of mean SIs for lymphocyte proliferative responses, the percentage of CD4+ or CD8+ T-cells staining for IFNγ, antibody responses, and organ CFU counts among mice in vaccinated and control groups. A logrank analysis was used to determine significance of survival curves among mice in immunized and in sham-immunized control groups.
3. Results
3.1. Construction of attenuated recombinant L. monocytogenes strains expressing F. tularensis antigens
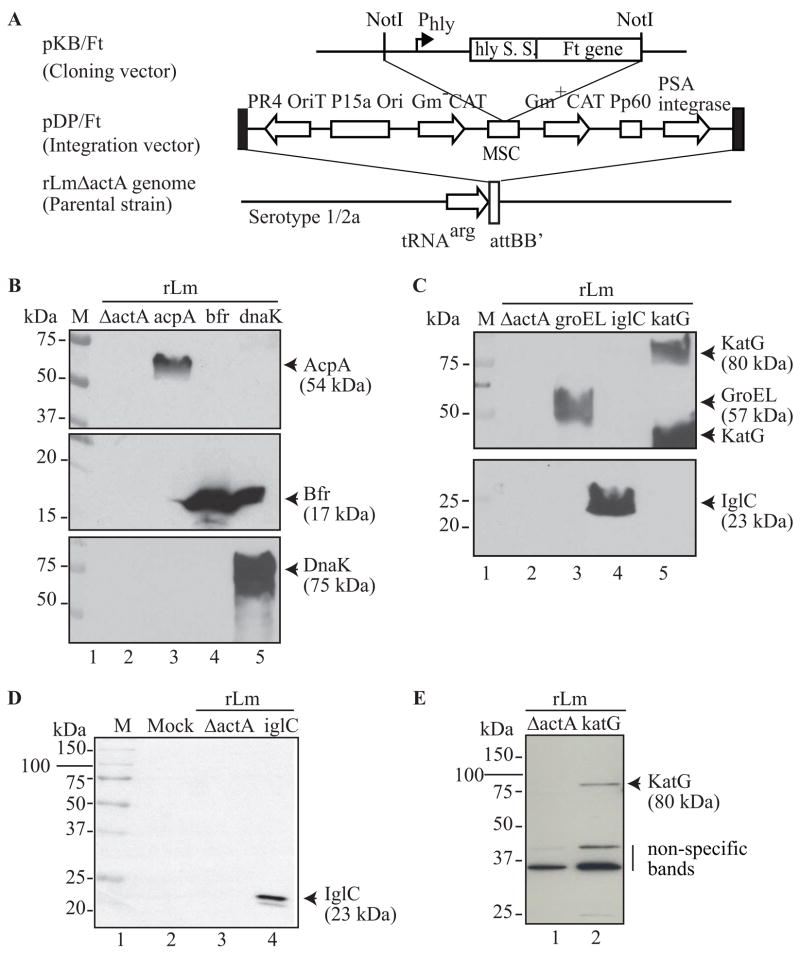
Using an ActA-deficient attenuated L. monocytogenes, rLmΔactA, as the parental strain, we constructed rLm/acpA, rLm/bfr, rLm/dnaK, rLm/groEL, rLm/iglC, rLm/katG, and rLm/pld expressing proteins of F. tularensis AcpA, Bfr, DnaK, GroEL, IglC, KatG, and Pld, respectively, fused to the signal peptide of LLO under the control of the L. monocytogenes hly promoter (Fig. 1A). Insertion of each F. tularensis protein expression cassette was confirmed by colony PCR as described in Materials and Methods, and they had no effect on the growth kinetics of recombinant L. monocytogenes strains when compared with the parental rLmΔactA strain (data not shown). To test the stability of the inserted F. tularensis protein expression cassette, we passaged each recombinant L. monocytogenes strain 20 times on non-selective BHI agar plates and found that all recombinant strains retained drug resistance and expressed the relevant F. tularensis protein in the culture filtrate at a level similar to the original stock, indicating that all strains had stably retained the integrated plasmid and a functionally active F. tularensis antigen expression cassette.
Figure 1.
Construction and expression of F. tularensis antigens by attenuated recombinant L. monocytogenes vaccines in broth culture and in human macrophages. A. Construction of attenuated recombinant L. monocytogenes expressing F. tularensis antigens. The F. tularensis nucleotide sequence encoding each antigen was PCR amplified from F. tularensis RCI genomic DNA and cloned into the vector pKB199 downstream of the promoter (Phly) and signal sequence (hly S.S.) of L. monocytogenes hly to generate pKB/Ft. The expression cassette of the fusion protein in pKB/Ft was excised by NotI and subcloned into the NotI site of the integration plasmid pDP4189 to generate pDP/Ft. The pDP/Ft plasmid was then integrated into the 3′ end of an arginine tRNA gene in the attenuated L. monocytogenes strain rLmΔactA through conjugation [60]. The resulting recombinant L. monocytogenes vaccines carried one single copy of the F. tularensis gene. A portion of the Figure was modified from Bruhn et al [60]. B and C. Protein expression in the culture supernatant of recombinant L. monocytogenes. Culture filtrates of each recombinant L. monocytogenes strain were concentrated and a volume of filtrate equivalent to 1 ml of the bacterial culture was analyzed by Western blotting using rabbit polyclonal antibody to AcpA (B, top panel), Bfr (B, middle panel), DnaK (B, bottom panel), GroEL and KatG (C, top panel), or IglC (C, bottom panel). D and E. Protein expression in human macrophages. THP-1 cells were mock infected or infected with the parental rLmΔactA strain, or the recombinant L. monocytogenes vaccines expressing F. tularensis IglC (rLm/iglC) or KatG (rLm/katG) at an MOI of 50. At 24 h post-infection, the infected cells were lysed and subjected to Western blotting using polyclonal antibody to IglC (D) or KatG (E). On the right border of each blot are listed the proteins of interest and their predicted mass. On the left border are listed the sizes of the molecular mass standards. M, Molecular mass standards.
3.2. Expression of F. tularensis antigens by attenuated recombinant L. monocytogenes strains
We analyzed the culture filtrates for release of F. tularensis proteins by the recombinant L. monocytogenes strains by Western blotting, using rabbit polyclonal antibody specific to the relevant F. tularensis protein. As shown in Figs. 1B and 1C, specific antibodies to each of the proteins reacted only with blots of culture filtrates of strains expressing the cognate protein and not with blots of the filtrates of other recombinant L. monocytogenes strains or the parental rLmΔactA strain. Antibodies to AcpA (Fig. 1B, top panel), Bfr (Fig. 1B, middle panel), DnaK (Fig. 1B, bottom panel), GroEL (Fig. 1C, top panel) and IglC (Fig. 1C, bottom panel) reacted to bands matching the size of the proteins in the F. tularensis proteome, as did antibody to Pld (not shown). Antibody to KatG specifically recognized an 80-kDa protein corresponding to the mass of the F. tularensis protein and a band of 40 kDa, presumably a breakdown product (Fig. 1C, top panel). These results confirmed that each of the recombinant L. monocytogenes strains released the relevant recombinant F. tularensis protein into the culture medium.
In immunoprotection studies to be described below, we identified two vaccines, rLm/iglC and rLm/katG, that protected mice from F. tularensis challenge. To evaluate the capacity of these two vaccines to express their recombinant F. tularensis protein intracellularly, we studied the expression of the proteins in human macrophages. We infected THP-1 cells with rLm/iglC or rLm/katG at an MOI of 50 and analyzed the relevant protein expression by Western blotting. Cells mock infected or infected with the parental rLmΔactA strain were used as negative controls. The antibody to IglC (Fig. 1D) detected a 23-kDa band specifically in rLm/iglC-infected THP-1 cells (lane 4) but not in mock-infected cells (lane 2) or cells infected with the parental rLmΔactA strain (lane 3). The antibody specific to KatG (Fig. 1E) detected three bands of approximately 80-, 45- and 35-kDa. The 80-kDa band was specifically detected in THP-1 cells infected with rLm/katG (lane 2) but not in cells infected with the parental rLmΔactA strain (lane 1). The 45- and 35-kDa bands were detected in THP-1 cells infected with both the parental and the rLm/katG strains, indicating the non-specificity of these two bands. It was noted that although the KatG protein was abundantly released by the rLm/katG strain into the culture supernatant (Fig. 1C, upper panel), its expression in the THP-1 macrophage cell line was relatively low (Fig. 1E). These results showed that the F. tularensis antigens were expressed by the recombinant L. monocytogenes strains in human macrophages.
3.3. Initial screen of attenuated recombinant L. monocytogenes strains expressing F. tularensis antigens
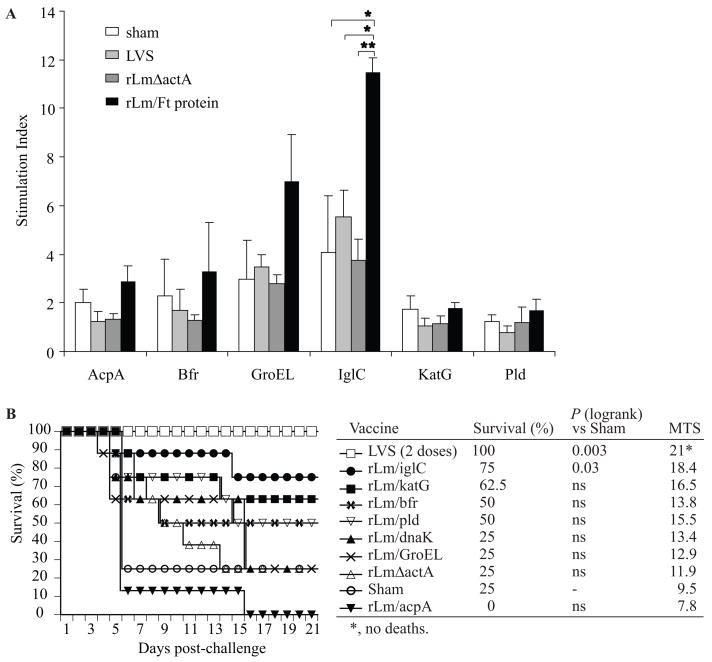
To examine if immunization with attenuated recombinant L. monocytogenes strains expressing F. tularensis proteins induces immune responses, we immunized BALB/c mice with six recombinant L. monocytogenes vaccines and analyzed lymphocyte proliferation in response to the relevant recombinant F. tularensis protein. BALB/c mice in groups of 3 were sham-immunized or immunized i.d. twice at weeks 0 and 5 with LVS (5 × 104 CFU/mouse) or each of the six recombinant L. monocytogenes strains (1 × 106 CFU/mouse) expressing different F. tularensis antigens. Four weeks after the second immunization (week 9), splenocytes were prepared and tested for lymphocyte proliferation after in vitro stimulation with the relevant protein. Mice immunized with rLm/iglC induced a significantly greater lymphocyte proliferative response to IglC than that induced in sham-, LVS-, and rLmΔactA-immunized mice (P = 0.03, 0.03, and 0.004, respectively). Mice immunized with the recombinant L. monocytogenes strains expressing AcpA, Bfr, GroEL, KatG, and Pld also induced greater lymphocyte proliferative responses to the relevant protein than the sham-immunized mice and mice immunized with the parental rLmΔactA strain or with F. tularensis LVS(Fig. 2A); however, such differences were not statistically significant..
Figure 2.
Immunogenicity and protective immunity induced by attenuated recombinant L. monocytogenes vaccines. A. Immunogenicity. Nine groups of 3 BALB/c mice were sham-vaccinated, or vaccinated twice at weeks 0 and 5 with 1 × 106 CFU of the parental recombinant L. monocytogenes vector (rLmΔactA) or the rLm vaccines expressing various F. tularensis antigens as indicated on the horizontal scale of the graph. Mice vaccinated twice with 5 × 104 CFU LVS served as positive controls. At week 9, mice were euthanized, a single cell suspension of splenocytes was prepared and incubated with the F. tularensis antigen (10 μg/ml) indicated on the horizontal scale of the graphs, and the culture then pulsed with 0.25 μCi of [3H]thymidine/ml for 2 h. The mean CPM varied from group to group, ranging from 90 to 380 in the absence of the F. tularensis protein and from 350 to 1500 in the presence of F. tularensis protein. The Stimulation Index (SI) was determined by dividing the mean CPM in the presence of the F. tularensis protein by the mean CPM in the absence of the F. tularensis protein. Values are the mean ± SE of the SI. The asterisks indicate that the difference in SI between the mice in a control group and the mice in the rLm/iglC-vaccinated group was significant. *, P < 0.05 and **, P < 0.01 by student t-test. B. Protective Immunity. Ten groups of 8 mice were immunized as described in A. At week 9, mice were anesthetized with Isoflurane, challenged i.n. with 1 × 106 CFU LVS (30 × LD50s), and monitored for illness and survival for three weeks. The differences in survival between the mice in the vaccinated groups and mice in the sham-vaccinated group were evaluated using a logrank analysis. ns, not significant (P > 0.05). Mean survival time (MST) was calculated by dividing the sum of the survival times of all mice in a group by the total number of mice challenged, with surviving animals given a survival time of 21 days, when the experiment was terminated.
To examine the capacity of recombinant L. monocytogenes vaccines to protect against challenge with F. tularensis, we established an LVS challenge model in an ABSL2 facility using BALB/c mice, a species that has been shown highly susceptible to F. tularensis infection [46]. We chose to use an i.n. challenge route to mimic airborne infection. To employ this model, we first established the LD50 for F. tularensis LVS by both the i.d. and i.n. routes, challenging groups of 8 BALB/c mice with F. tularensis LVS in doses ranging from 104 – 108 CFU/mouse i.d. or from 102 – 106 CFU i.n. The LD50 for the i.d. route was calculated to be 3 × 107 CFU. The LD50 for the i.n. route was calculated to be 3.2 × 104 CFU. We selected a challenge dose of 1 × 106 CFU/mouse i.n. for initial experiments testing the protective efficacy of vaccines. In these initial experiments, mice were anesthetized by inhalation with Isoflurane before i.n. challenge with LVS. However, we later found that when mice were challenged i.n. with LVS after inhaled Isoflurane, the survival of the mice varied considerably from one experiment to the other., Therefore, we changed the method of anesthesia to i.p. injection of Ketamine/Xylazine, a method of anesthesia that gave consistent survival and organ burden results. By this method of anesthesia, the LD50 of LVS i.n. was consistently calculated to be approximately 700 CFU.
In our initial screening of recombinant L. monocytogenes vaccines, ten groups of eight BALB/c mice were immunized i.d. twice, 5 weeks apart, with 1 × 106 CFU of each recombinant L. monocytogenes vaccines expressing F. tularensis antigens. Control animals were sham-immunized or immunized twice with the vector control (rLmΔactA) or with LVS (5 × 104 CFU); although LVS is typically administered just once, we determined that two immunizations sometimes provided greater protection with this vaccine than one immunization (data not shown) and resulted in a lower organ bacterial burden (See Fig. 4). Four weeks after the second immunization, mice were anesthetized with Isoflurane and challenged i.n. with 1 × 106 CFU LVS (~ 30 × LD50s) and observed for 3 weeks for illness and death (Fig. 2B). Among animals immunized with recombinant L. monocytogenes strains, the animals immunized with recombinant L. monocytogenes expressing IglC, KatG, Bfr, or Pld showed greater survival than the sham-immunized animals and animals immunized with the rLmΔactA vector control. Notably, animals immunized with rLm/iglC had a significant higher survival than sham-immunized animals, and animals in this group showed little or no signs of illness (ruffled fur, hunched back, or swollen eyes) after challenge. Animals immunized twice i.d. with LVS were 100% protected from i.n. challenge with the homologous LVS strain. Although the animals immunized with the vector control or recombinant L. monocytogenes expressing DnaK and GroEL did not show greater survival than the animals immunized with the vector control, the mean survival time was greater for these animals than for the sham-immunized controls, indicating some protection (Fig. 2B). Additional experiments demonstrated that, while immunization with F. tularensis protein in adjuvant or with recombinant L. monocytogenes expressing F. tularensis protein induced stronger immunoprotection than sham-immunization, significantly high-level protection was observed consistently only with selected recombinant L. monocytogenes vaccines, especially rLm/iglC (data not shown).
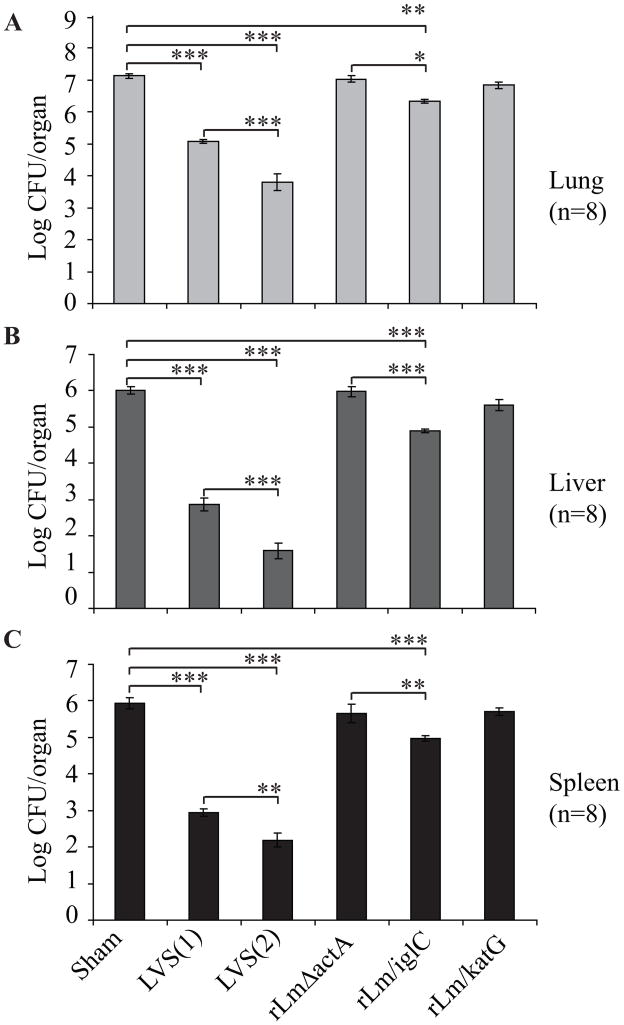
Figure 4.
Intradermal immunization with attenuated recombinant L. monocytogenes vaccines expressing IglC reduces the bacterial organ burden after i.n. challenge with LVS. Six groups of 8 BALB/c mice were sham-immunized, immunized once with LVS [LVS(1)], or twice with LVS [(LVS(2)], rLmΔactA, rLm/iglC or rLm/katG at an interval of 4 weeks. At week 8, mice were anesthetized with Ketamine/Xylazine and challenged i.n. with 4400 CFU LVS. At day 5 post-challenge, mice were euthanized, and the liver, spleen and lung were removed and assayed for CFU of F. tularensis as described in Figure 3B. Values represent the mean Log CFU per organ ± SE. The asterisks indicate that the differences in bacterial burden among the animals in the indicated paired groups are statistically significant. *, P < 0.05; **, P < 0.01; and ***, P < 0.001 by one-way ANOVA with Bonferroni’s post test.
In subsequent experiments, we focused on two recombinant L. monocytogenes vaccines that provided higher protection in the initial screening experiments: rLm/iglC and rLm/katG. In these experiments, we found that: (i) two immunizations with rLm/iglC, rLm/katG, or the combination of both strains provided better protection against LVS i.n. challenge than one immunization; (ii) Animals immunized once with rLm/iglC, rLm/KatG, or the combination of both strains 4 weeks before challenge were better protected than animals immunized once 8 weeks before challenge; (iii) Animals immunized with rLmΔactA vector control were partially protected against i.n. challenge with LVS; and (iv) immunization with recombinant L. monocytogenes vaccines at doses ranging from 105 to 107 CFU/mouse gave similar immunoprotection (data not shown). In these experiments, we utilized Isoflurane anesthesia during i.n. LVS challenge. Subsequently, we determined that, in mice challenged with LVS i.n. using Isoflurane anesthesia, there was variability in survival. Therefore in all subsequent experiments, we instead anesthetized animals by i.p. injection of Ketamine/Xylazine, which gave highly consistent results after LVS challenge.
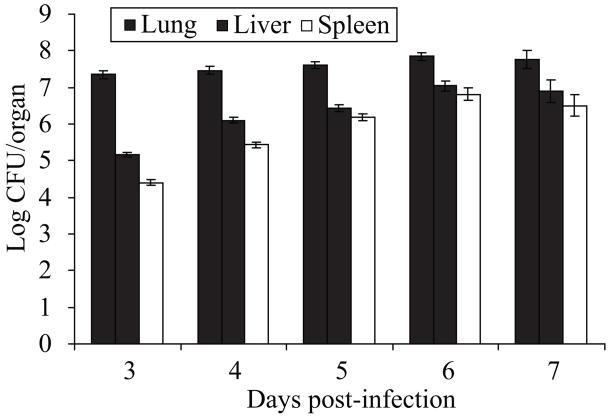
3.4. Intradermal immunization with recombinant L. monocytogenes vaccines reduces bacterial burden in host tissues after i.n. challenge with LVS
As a prelude to evaluating the impact of immunization with recombinant L. monocytogenes vaccines on the bacterial burden in host tissues after challenge, we assessed the bacterial burden in host tissues of non-immunized animals at various times after challenge with F. tularensis LVS. We anesthetized 40 BALB/c mice i.p. with Ketamine/Xylazine and infected them i.n. with 4.4 × 103 CFU LVS (≈6 × LD50s). We then monitored their body weight change daily, and at various times post-infection, we euthanized a subset of 8 mice, removed their liver, spleen and lung, and assayed CFU of LVS in these tissues. Mice began losing weight by 4 days post-infection and continued to lose weight until 7 days post-infection when the experiment was terminated (data not shown). Consistent with the body weight loss, the bacterial burden in lung, liver and spleen increased daily between 3 and 6 days post-infection and CFU levels among animals were very consistent at these time points, yielding small standard errors (Fig. 3). These results indicated that i.n. challenge with F. tularensis LVS after Ketamine/Xylazine anesthesia induces a uniformly large lung infection, which is spread systemically to the liver and spleen within 3 days after infection. We selected day 5 post-challenge to assess the impact of vaccines on the organ burden of F. tularensis LVS since animals still appeared relatively healthy at this time point and the organ bacterial burden was highly uniform in all three organs assayed.
Figure 3.
Bacterial burden in the host tissues of mice after intranasal challenge with F. tularensis LVS. Forty BALB/c mice were anesthetized with Ketamine/Xylazine and then infected i.n. with 4400 CFU of LVS. At the indicated times post-infection, 8 mice per group were euthanized and the liver, spleen and lung were removed and homogenized in 2 ml of sterile PBS for 15 seconds in a Pro200 homogenizer. CFU of F. tularensis in each organ was determined by plating serial dilutions of the homogenates on Chocolate agar containing sulfamethoxazole (40 mg/ml), trimethoprim (8 mg/ml) and erythromycin (50 mg/ml) and culturing for 3 days at 37°C. Values represent the mean Log CFU per organ ± SE.
To examine whether immunization with recombinant L. monocytogenes vaccines expressing F. tularensis IglC or KatG reduces the bacterial burden of challenge organisms in the host tissues, we immunized 6 groups of 8 mice once at week 0 with 1 × 104 CFU of LVS (Positive control, one dose), or twice at weeks 0 and 4 with sterile saline (Sham), 1×104 CFU LVS (Positive control, two doses), 1 × 106 CFU of rLmΔactA (Vector control), rLm/iglC, or rLm/katG. At week 8, the mice were anesthetized with Ketamine/Xylazine, challenged i.n. with 4.4 × 103 CFU LVS (≈6 × LD50s), euthanized at day 5 post-challenge, and assayed for bacterial burden in the lung, liver and spleen. As shown in Fig 4, animals immunized with rLm/iglC had a significantly lower mean bacterial burden in the lung (Fig. 4A), liver (Fig. 4B) and spleen (Fig. 4C) than sham-immunized animals (0.7, 1.1, and 1.0 log CFU lower, respectively, with P < 0.01, 0.001, and 0.001, respectively); animals immunized with rLm/iglC also had a significantly lower mean bacterial burden in the lung, liver, and spleen than animals immunized with the vector control (P < 0.05, 0.001, and 0.01, respectively). There was no significant difference in organ burden between animals in the sham-immunized group and in the rLm/katG-immunized group. The bacterial burden in the lung, spleen and liver of animals immunized with one or two doses of LVS were 2 – 5 logs lower than those in sham-immunized animals. Notably, animals immunized with two doses of LVS had a significantly lower organ bacterial burden in the lung, liver, and spleen than animals immunized with one dose of LVS (P < 0.001, 0.001, and 0.01, respectively).
3.5. Intradermal immunization with recombinant L. monocytogenes vaccines protects animals against i.n. challenge with F. tularensis LVS
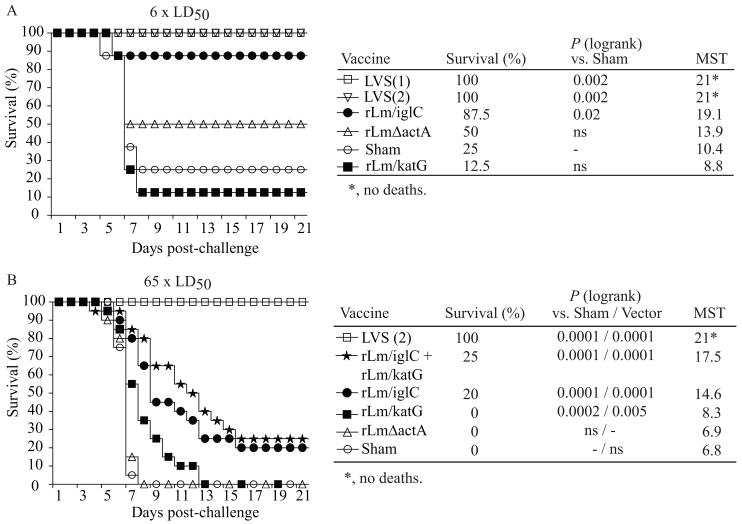
To investigate further the capacity of the recombinant L. monocytogenes vaccines expressing IglC or KatG to induce immunoprotection, we immunized 6 groups of 8 BALB/c mice with the same vaccines described in Fig. 4. At week 8, we anesthetized the mice with Ketamine/Xylazine, challenged them i.n. with 4.4 × 103 CFU LVS (≈6 × LD50s), and observed them for survival and illness for up to 3 weeks post-challenge. Consistent with lower bacterial burdens in their tissues, animals immunized with LVS and rLm/iglC had significantly greater survival rates than sham-immunized animals (P < 0.01 and 0.05, respectively) (Fig. 5A). Animals immunized with the vector control also had a higher survival rate than sham-immunized animals, consistent with the observation that the rLmΔactA vector itself provides some protection against LVS challenge (Figs. 5A and 9). However, immunization with rLm/katG did not protect animals that were anaesthetized with Ketamine/Xylazine against i.n. challenge with a lethal dose of LVS in this experiment (Fig. 5A).
Figure 5.
Intradermal immunization with attenuated recombinant L. monocytogenes vaccines expressing IglC protects mice against i.n. challenge with lethal dose of LVS. A. Intranasal challenge with 6 × LD50 of LVS. This challenge study was performed simultaneously with the one shown in Fig. 4. Six groups of 8 mice were sham-immunized or immunized with LVS or rLm vaccines at weeks 0 and 4. At week 8, mice were anesthetized with Ketamine/Xylazine, challenged i.n. with 4400 CFU of LVS, and monitored for survival for up to 3 weeks after challenge. B. Intranasal challenge with 65 × LD50 of LVS. Groups of mice were sham-immunized or immunized i.d. twice at weeks 0 and 4 with 5 × 104 CFU LVS or 1 × 106 CFU of rLmΔactA (vector), rLm/iglC, rLm/katG or rLm/iglC plus rLm/katG. At 4 – 6 weeks after the last immunization, mice were anesthetized with Ketamine/Xylazine, challenged i.n. with 4.5 × 104 CFU F. tularensis LVS (65 LD50s), and monitored for 3 weeks. Data shown in Fig. 5B are combined from three independent experiments totaling 20 mice per group. Survival curves among mice in the sham or vector-immunized group and mice in the LVS or rLm vaccine-immunized groups were compared by logrank analysis. ns, not significant (P > 0.05). Mean survival time (MST) was calculated by dividing the sum of the survival times of all mice in a group by the total number of mice challenged, with surviving animals given a survival time of 21 days, when the experiment was terminated.
Figure 9.
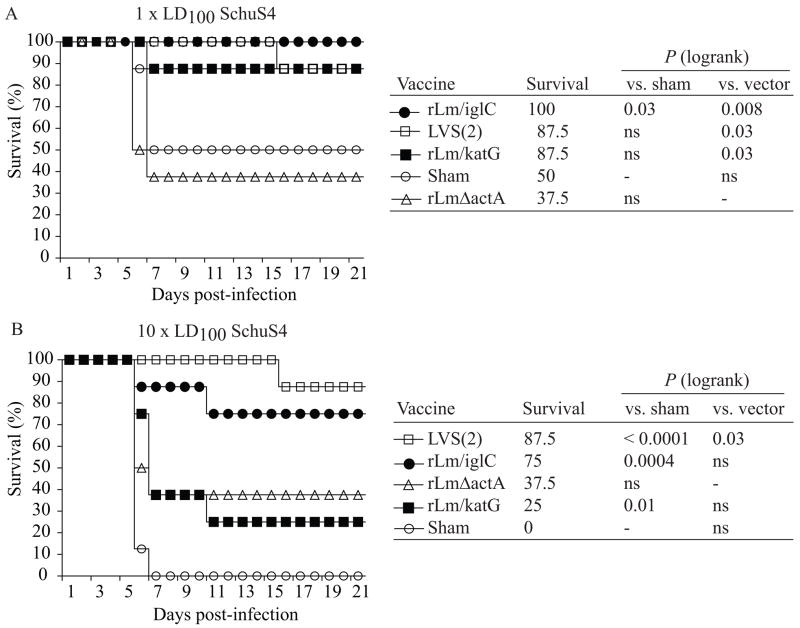
Intradermal immunization with recombinant L. monocytogenes vaccines protects mice against aerosol challenge with F. tularensis Type A SchuS4 strain. Ten groups of eight BALB/c mice were sham-immunized, or immunized i.d. twice at weeks 0 and 4 with 1×107 CFU rLmΔactA, rLm/iglC or rLm/katG. Mice immunized twice with 1 × 104 CFU LVS served as a positive control. Six weeks after the second immunization (week 10), mice were challenged by aerosol with F. tularensis SchuS4 with a dose estimated to be either 1 × LD100 (A) or 10 × LD100 (B). [(The effective dose actually delivered in (A) was less than 1 × LD100 as 50% of the animals survived, i.e. the dose was effectively 1 × LD50. The animals in (B) received 10 times the dose of the animals in (A), as detailed in Methods]. The difference in survival between the mice in a vaccinated group and mice in a sham- or vector-vaccinated group was evaluated using a logrank analysis. ns, not significant (P > 0.05).
To examine whether immunization with the recombinant L. monocytogenes vaccines expressing IglC or KatG could protect animals against higher dose LVS challenge, we immunized BALB/c mice i.d. twice at weeks 0 and 4 with rLm/iglC, rLm/katG, or the combination of both vaccines. Animals sham-immunized or immunized i.d. twice with the parental rLmΔactA strain served as negative controls. Animals immunized i.d. twice with 1 × 104 CFU LVS served as a positive control. At four to six weeks after the last immunization, mice were anesthetized i.p. with Ketamine/Xylazine and challenged i.n. with super lethal doses of LVS (4.5 × 104 CFU, equivalent to 65 × LD50s by Ketamine/Xylazine anesthesia). The results from 3 independent experiments including a total of 20 mice per group are summarized in Fig. 5B. We first compared the survival curves within each vaccine group, which showed no significant difference amongst the 3 independent experiments. We then combined the 3 experiments and compared the survival curves of animals immunized with various vaccines. Consistent with the results obtained from the i.n. challenge with 6 × LD50s of LVS (Fig. 5A), immunization with rLm/iglC provided significant protection to mice after i.n. challenge with 65 × LD50s of LVS; the mean survival time of animals immunized with rLm/iglC was 14.6 days vs. 6.8 days for sham-immunized animals and 6.9 days for animals immunized with the parental rLmΔactA strain (P< 0.0001). In this experiment, animals immunized with rLm/KatG survived significantly longer (P<0.0002) than the sham- and vector-immunized animals (8.3 days vs. 6.8 and 6.9 days, respectively). Animals immunized with rLm/iglC plus rLm/KatG had a higher survival rate and longer mean survival time than animals immunized with only rLm/iglC (17.5 vs. 14.6 days). Mice immunized twice i.d. with LVS were 100% protected against homologous i.n. challenge with a super lethal dose of LVS. These results confirmed our observations in the initial experiments when mice were anesthetized with Isoflurane, and demonstrated that a recombinant L. monocytogenes vaccine expressing a single F. tularensis protein, especially IglC, was able to provide protection against a super lethal challenge with F. tularensis LVS. In this experiment, where the LVS challenge dose was increased to 65 × LD50, the rLmΔActA vector itself was not able to induce protection.
3.6. Intradermal immunization with recombinant L. monocytogenes vaccines induces immune responses specific to F. tularensis antigens
3.6.1. T-cell mediated immune responses
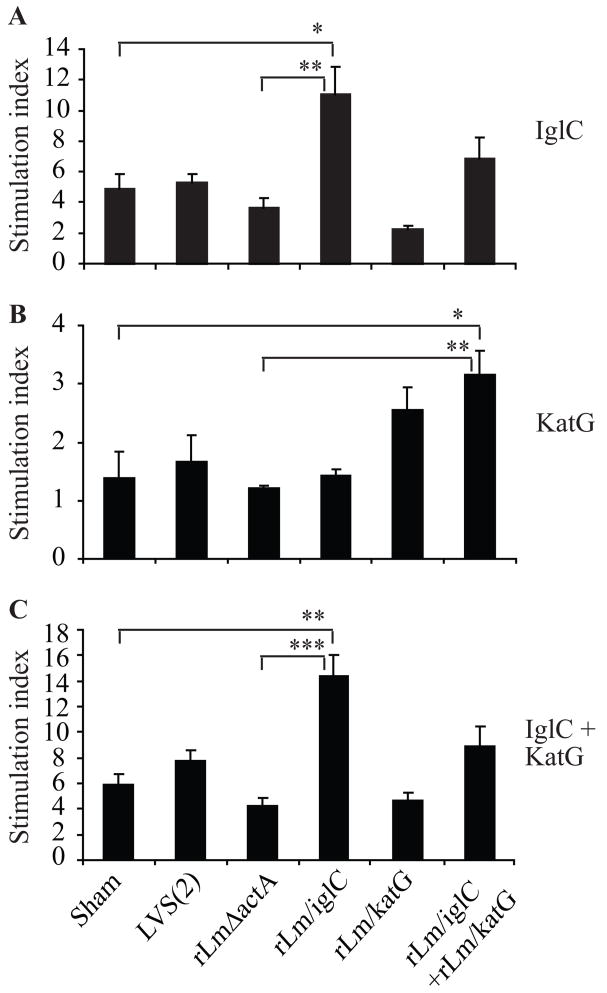
To examine further if immunization with attenuated recombinant L. monocytogenes expressing F. tularensis IglC or KatG induces T-cell mediated immune responses, we immunized BALB/c mice and analyzed IFN-γ secretion and lymphocyte proliferation in responses to F. tularensis recombinant proteins. BALB/c mice in groups of 3 were sham-immunized or immunized i.d. twice at weeks 0 and 3 with LVS at a dose of 1 × 104 CFU/mouse or rLm/iglC, rLm/katG or rLm/iglC plus rLm/katG at a dose of 1 × 106 CFU/mouse. Six days after the second immunization, when the MHC Class I restricted T-cell immune response induced by secondary infection with recombinant L. monocytogenes reaches a peak time [26], mice were euthanized, and a single cell suspension of splenocytes was prepared and tested for lymphocyte proliferation and IFNγ secretion upon in vitro stimulation with recombinant IglC, KatG, or IglC plus KatG proteins. Mice immunized with rLm/iglC had significantly increased lymphocyte proliferative responses to IglC (Fig. 6A) or IglC plus KatG (Fig. 6C) but not to KatG (Fig. 6B) compared with sham-immunized mice or mice immunized with the vector control. However, the lymphocyte proliferative response to KatG in mice immunized with rLm/katG was not significantly different from those in sham-immunized mice or mice immunized with the vector control (Fig. 6B). Mice immunized with rLm/iglC plus rLm/katG showed a significantly increased lymphocyte proliferative response to KatG (Fig. 6B); responses to IglC (Fig. 6A) or IglC plus KatG (Fig. 6C) were greater than those of sham-immunized mice or mice immunized with the rLmΔactA strain, but not significantly so. These results confirmed those shown in Fig. 2A that immunization with rLm/iglC induced significantly increased T-cell immune response specific to the F. tularensis IglC protein.
Figure 6.
Lymphocyte proliferation induced by intradermal immunization with attenuated L. monocytogenes vaccines expressing F. tularensis IglC or KatG. Groups of 3 BALB/c mice were sham-immunized, immunized i.d. twice with 1 × 104 CFU LVS, or 1×106 CFU recombinant L. monocytogenes vaccines expressing IglC (rLm/iglC), KatG (rLm/katG), or the combination of both at weeks 0 and 3. Six days after the second immunization, mice were euthanized and their splenocytes isolated and assayed for lymphocyte proliferation in response to recombinant IglC (A), KatG (B) or the IglC plus KatG (C) proteins. The mean CPM varied from group to group, ranging from 355 to 564 in the absence of the F. tularensis protein and from 493 to 4840 in the presence of the F. tularensis protein. The Stimulation Index (SI) was determined by dividing the mean CPM obtained in the presence of the F. tularensis protein by the mean CPM obtained in the absence of F. tularensis protein. Standard errors of the means of triplicate samples from three mice are shown. Asterisks indicate that the differences in SIs between the indicated groups are significant. *, P<0.05; **P<0.01; and ***P<0.001 by one-way ANOVA with Bonferroni’s post test.
3.6.2. IFNγ-secreting CD4+ and CD8+ T-cells
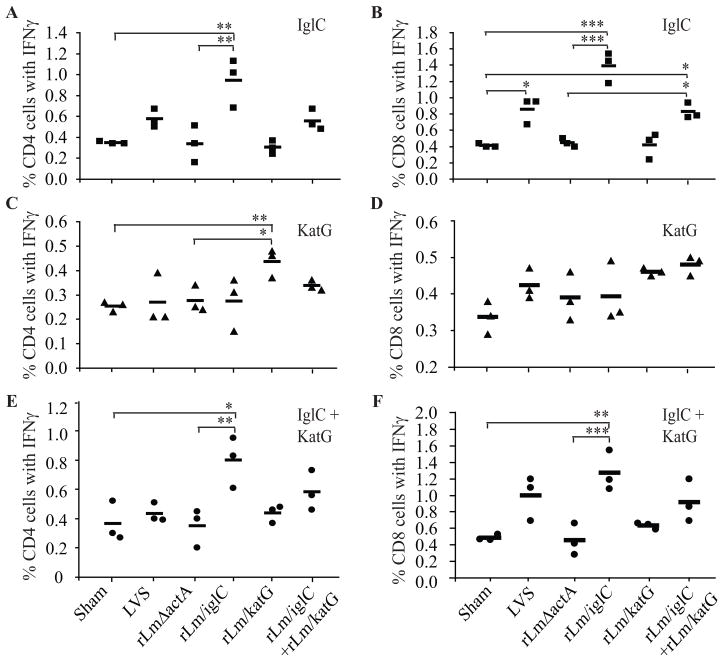
We also tested the capacity of rLm/iglC and rLm/katG to induce in mice CD4+ and CD8+ T-cells that secret IFNγ in response to the relevant F. tularensis protein. As shown in Figure 7, sham-immunized animals and animals immunized with the vector control had relatively low CD4+ and CD8+ T-cell responses to IglC, KatG, or IglC plus KatG. LVS-immunized animals showed significantly increased CD8+ T-cell responses to IglC, compared with sham-immunized mice (A and B). LVS immunized animals also showed greater CD4+ and CD8+ T-cell responses to KatG or KatG plus IglC than sham-immunized animals, but the differences were not statistically significant (C, D, E and F). In contrast, animals immunized with rLm/iglC showed significantly increased CD4+ and CD8+ T-cell responses to IglC (A and B) or the combination of IglC and KatG (E and F) but not to KatG alone (C and D) compared with sham-immunized mice or mice immunized with the vector control. Animals immunized with rLm/katG showed a significantly increased CD4+ response to KatG but not to IglC or IglC plus KatG compared with sham-immunized mice or mice immunized with the vector control (A, C and E). The CD8+ T-cell immune response in animals immunized with rLm/katG was not significantly increased compared with sham-immunized mice or mice immunized with the vector control (B, D and F). Animals immunized with the combination of rLm/iglC and rLm/katG showed a significantly increased CD8+ T-cell response to IglC; the CD8+ T cell response to KatG and IglC plus KatG was also increased compared with sham-immunized mice or mice immunized with the vector control (B, D, and F), but these differences were not statistically significant. rLm/iglC induced stronger CD4+ and CD8+ T-cell immune responses to IglC (~1–1.4% of CD4+ and CD8+ T-cells expressed IFNγ) than rLm/katG did to KatG (~0.4% of CD4 and CD8 cells expressed IFNγ). The above results were consistent with those from the lymphocyte proliferation assay and indicate that i.d. immunization with L. monocytogenes vaccines expressing IglC or KatG induces cell-mediated immune responses specific to the relevant F. tularensis proteins.
Figure 7.
Antigen-specific intracellular IFNγ secretion after intradermal immunization with recombinant L. monocytogenes vaccines expressing F. tularensis proteins. Groups of 3 BALB/c mice were sham-immunized or immunized i.d. twice at weeks 0 and 3 with 5 × 104 CFU LVS, with 1×106 CFU rLm/iglC, rLm/katG, or the same dose of both vaccines. Six days after the second immunization, mice were euthanized and their splenocytes were incubated with or without the relevant F. tularensis protein (10 μg/ml): IglC (A and B), KatG (C and D), or IglC plus KatG (E and F). The cells were stained with FITC-conjugated rat anti-mouse CD4 (A, C and E) or PE-Cy5-conjugated rat anti-mouse CD8 monoclonal antibody (B, D, and F). Cells were then washed and fixed per protocol and stained for intracellular IFNγ with PE-conjugated rat anti-mouse IFNγ antibody. Stained cells were analyzed on a FACSCalibur cytometer using CellQuest software. Each individual symbol represents result from an individual mouse. The bars represent the mean value for three animals. Asterisks indicate that the difference in the cell numbers between the mice in the indicated group and that of mice in the sham- or vector-immunized group was significant. *, P<0.05; **, P<0.01; ***, P<0.001 by one-way ANOVA with Bonferroni’s post test.
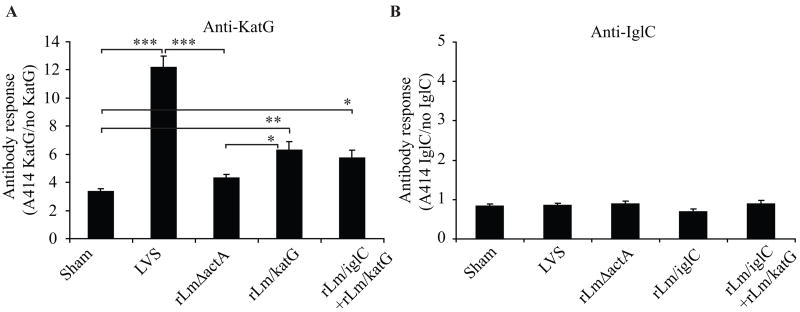
3.6.3. Humoral immunity
Groups of 5 BALB/c mice were sham-immunized or immunized i.d. at weeks 0 and 4 with LVS, the parental rLmΔactA, rLm/iglC, or rLm/katG. At 4 weeks after the last immunization (week 8), the sera were collected and tested for antibodies specific to F. tularensis proteins by ELISA. The antibody response to KatG was significantly increased in animals immunized with LVS and rLm/katG compared with sham-immunized mice (P < 0.001 and 0.01, respectively) or mice immunized with the parental rLmΔactA strain (P < 0.001 and 0.05, respectively). The antibody response to KatG was also significantly increased in animals immunized with rLm/iglC plus rLm/KatG compared with sham-immunized mice (P < 0.05) (Fig. 8A). In contrast, the antibody response to IglC was not detectable in any group of immunized mice (Fig. 8B). These results suggest that KatG, but not IglC, induces a humoral immune response when expressed by recombinant L. monocytogenes and delivered intradermally.
Figure 8.
Antibody response induced by intradermal immunization with recombinant L. monocytogenes. Groups of 5 mice were sham-immunized or immunized i.d. twice at weeks 0 and 4 with LVS, vector control (rLmΔactA), or recombinant L. monocytogenes vaccines expressing KatG (rLm/katG), IglC (rLm/iglC), or the combination of both vaccines. At week 8, mice were euthanized and sera were collected to measure the antibody (IgG) response by ELISA. For measuring antibody response to KatG (A), sera were diluted 1:50. For measuring antibody response to IglC (B), sera were diluted 1:25. The antibody responses are presented as the Absorbance at 414 nm (A414nm) in the presence of antigen divided by the A414nm in the absence of antigen for each individual mouse. Bars represent the mean of the antibody titer from the 5 mice per group. Asterisks indicate that the difference between the antibody response of mice in the indicated vaccinated group and mice in the sham-vaccinated group was significant. *, P<0.05; **, P<0.01; ***, P<0.001 by one-way ANOVA with Bonferroni’s post test.
3.7. Intradermal immunization with recombinant L. monocytogenes vaccines protects mice against aerosol challenge with Type A F. tularensis SchuS4
For more definitive testing of selected vaccines, we employed a mouse model in which animals were challenged by aerosol with the highly virulent F. tularensis Type A SchuS4 strain in an ABSL-3 facility. Groups of eight BALB/c mice were immunized i.d. twice at weeks 0 and 4 with sterile saline (Sham), LVS (1 × 104 CFU/mouse), the parental rLmΔactA strain, rLm/iglC or rLm/katG (1 × 107 CFU/mouse). Six weeks after the second immunization (week 10), mice were challenged with 1 × LD100 (Fig. 9A) or 10 × LD100 (Fig. 9B) of F. tularensis type A SchuS4 strain by the aerosol route, and observed for survival and weight change daily. Sham-immunized animals had 50% survival when exposed to 1 × LD100 and 0% survival when exposed to 10 × LD100 F. tularensis SchuS4. Animals immunized twice with LVS had a survival rate of 87.5% when exposed to either dose of F. tularensis SchuS4. Importantly, the animals immunized with rLm/iglC had 100% survival when exposed to 1 × LD100 and 75% survival when exposed to 10 × LD100 F. tularensis SchuS4, a greater survival rate than sham-immunized animals or animals immunized with the vector control and a survival rate comparable to that of animals immunized twice with LVS, which has typically been administered once in studies of protective efficacy, but which we observed was more efficacious when administered twice. Animals immunized with rLm/katG also showed greater survival than sham-immunized animals. Interestingly, animals immunized with the vector control (rLmΔactA) also had a greater survival rate than the sham-immunized animals, indicating that the vector control itself offers some protection against F. tularensis challenge. There was no significant weight loss in mice that survived challenge with F. tularensis SchuS4.
4. Discussion
Our study shows that i.d. vaccination with a live attenuated heterologous vector, recombinant L. monocytogenes, expressing a single F. tularensis protein, IglC, is able to induce protection against i.n. challenge with F. tularensis LVS and aerosol challenge with Type A F. tularensis in a highly susceptible host. To our knowledge, this is the first genetically defined vaccine and the first recombinant vaccine that is capable of inducing protection against aerosolized Type A F. tularensis and the first demonstration that a single F. tularensis protein, the unique antigen IglC, delivered by a heterologous vector is capable of inducing protective immunity against Type A F. tularensis.
The L. monocytogenes vector was chosen specifically because L. monocytogenes mimics the intracellular life style of F. tularensis. Most importantly, these two intracellular bacteria enter the cytoplasm of the host cell and release antigens at that site, one that favors presentation via Class I MHC molecules. In previous studies, we have employed a similar strategy in developing vaccines against tuberculosis, i.e. choosing as a vaccine vector an organism, BCG, that mimics the M. tuberculosis intracellular lifestyle, which, in contrast to F. tularensis, is intraphagosomal [42]. The strategy of choosing as a vaccine vector one that mimics the lifestyle of the target pathogen, thereby enabling the correct processing and presentation of recombinant immunoprotective antigens, may have general applicability to vaccines against intracellular pathogens. Hence, vectors that enter the cytoplasm, such as attenuated L. monocytogenes and replication-deficient adenovirus may be most efficacious for pathogens such as F. tularensis, Trypanosoma cruzi, and rickettsia, that escape the phagosome and multiply intracytoplasmically, whereas vectors that remain in and multiply within a phagosome, such as BCG and replication-deficient Legionella pneumophila, may be most efficacious for pathogens such as M. tuberculosis, Mycobacterium leprae, Leishmania sp., Chlamydia psittaci, Coxiella burnetii, and Yersinia pestis. While this paper does not focus on nor prove the general applicability of this strategy, it provides additional evidence in support of the general applicability of the strategy, which we now have used successfully to develop highly efficacious vaccines against four different intracellular pathogens – M. tuberculosis, M. leprae, M. bovis, and F. tularensis.
L. monocytogenes has been extensively studied as a vector to deliver foreign antigens against various pathogens. Recombinant L. monocytogenes expressing defined proteins or peptides from other intracellular pathogens such as HIV, SIV, Herpes Simplex Virus, lymphocytic choriomeningitis virus (LCMV), and M. tuberculosis provide protection against infection with the relevant pathogen [47–51]. L. monocytogenes vectors with deletions in actA and one additional gene have been well-tolerated in animal and in human studies [27]. Other types of attenuated L. monocytogenes vectors designed for safety in humans have also been utilized in vaccine studies [29, 48, 52]. Unexpectedly, the L. monocytogenes vector (rLmΔactA) itself provided a small degree of cross-protection against F. tularensis. Consistent with this, the F. tularensis LVS vaccine similarly provides some protection against a lethal Listeria challenge [53–55]. Cross-protection may reflect immunoprotective responses to shared antigens of the two intracellular bacterial pathogens. While not examined in this study, it is possible that a recombinant vaccine based upon an attenuated L. monocytogenes vector will protect against L. monocytogenes, a human pathogen, as well as against the target of the recombinant antigen. If so, this would be an additional benefit of using this vector.
IglC proved to be the most potent of the F. tularensis antigens evaluated. This 23-kDa protein is strongly induced by intracellular F. tularensis [35, 36] and likely a major factor contributing to its high pathogenecity and immunogenicity. IglC-deficient F. tularensis mutants are impaired in phagosomal escape and intramacrophage growth [37, 39, 56]. Interestingly, a F. tularensis mutant deficient in IglC was unable to protect against Type A F. tularensis challenge, despite its ability to persist and disseminate to the liver and spleen of the host [12], consistent with the importance of this molecule in immunoprotection against tularemia. Also of interest, recombinant L. monocytogenes expressing IglC induced strong CD4+ and CD8+ T-cell immune responses but poor antibody responses. This is consistent with a dominant role for cell-mediated immunity in host defense against Type A F. tularensis, with humoral immunity playing little or no role. The recombinant L. monocytogenes vaccine described herein is the first vaccine based upon this antigen, which importantly, has no homolog in the mammalian genome.
The mouse model provides a stringent test of tularemia vaccines, as mice are even more susceptible to F. tularensis than humans. Hence, all things being equal, success of a vaccine against F. tularensis in the mouse bodes well for success of the vaccine in humans. Further testing of a second-generation version of the rLm/iglC vaccine in non-human primates should provide additional safety and efficacy data upon which to base the appropriateness of the vaccine for human use.
For practical reasons, our study employed two mouse models. The first model was used to screen vaccines for safety and efficacy. This model, in which mice were challenged with lethal dose of F. tularensis LVS, has several major advantages. It requires only a BSL2 animal facility and thus is readily available to most researchers. In addition, work in a BSL2 facility is less biohazardous and less costly. The second mouse model was a definitive model for testing the efficacy of selected vaccines against aerosolized Type A F. tularensis. This required a BSL3 animal facility. By screening the vaccines in the first model and selecting only the most promising ones for testing in the second model, the amount of BSL3 biohazardous work and the cost of testing were minimized.
The efficacy of the rLm/iglC vaccine against SchuS4 compared favorably with that of the more toxic LVS vaccine (Fig. 9). LVS is designed for single administration in humans. However, in our study, one administration of LVS gave relatively poor protection against i.n. challenge with lethal doses of LVS – only 37% of animals survived in one study in which a single dose was tested (data not shown). In the same study, 75% of animals administered two doses of rLm/iglC survived. To achieve a high level of protection with LVS, two doses were required. Consistently, after lethal dose LVS challenge, animals immunized with two doses of LVS had bacterial burdens in the host tissues significantly lower than those in animals immunized with only one dose of LVS (Fig. 4). Hence, in our definitive study of the protective efficacy of recombinant L. monocytogenes vaccines against aerosolized Type A F. tularensis, we administered two doses of LVS as a positive control. Nevertheless, two immunizations with rLm/iglC gave protection comparable to two immunizations with LVS against challenge with aerosolized F. tularensis Type A.
Safety is of paramount importance in the development of vaccines against agents of bioterrorism, particularly because the threat from these agents is uncertain. In this regard, our approach, using live attenuated heterologous vectors to deliver key immunoprotective antigens, offers an attractive alternative to attenuated F. tularensis vaccines including LVS, which retains considerable toxicity. Attenuated F. tularensis vaccines investigated to date generally fall into one of two categories. One category consists of non-Type A F. tularensis vaccines more attenuated than LVS. Such vaccines, while less toxic than LVS, have not demonstrated high efficacy against Type A F. tularensis challenge [4, 15–17, 57], although a recent study showed that intranasal immunization with an attenuated LVS provides protection to F. tularensis SchuS4 challenge [58]. The second category consists of attenuated Type A F. tularensis. Generally, these vaccines have also not been efficacious against Type A challenge. Exceptionsare two Type A F. tularensis SchuS4 mutants with a deletion in either the FTT0918 [12] or the FTT1103 gene [59], which do protect against F. tularensis Type A challenge. However, attenuated Type A strains carry a potential risk of reversion to virulence. The deletion of additional genes will likely be required by regulatory authorities to ameliorate this concern; however, additional gene deletions may also diminish or even eliminate vaccine efficacy.
While the rLm/iglC vaccine described herein offers substantial protection against Type A F. tularensis challenge in a highly susceptible host, an even more potent vaccine may be needed to protect against aerosol challenge with high doses of Type A F. tularensis, such as might occur in a bioterrorist attack. With this in mind, we are pursuing several approaches to enhance the potency of the vaccines. One approach is to increase the intracellular expression of IglC by the rLm/iglC vaccine, e.g. by the use of promoters that are stronger inducers of the protein intracellularly in macrophages. Another approach is to employ a heterologous prime-boost vaccination strategy, utilizing a second unrelated highly attenuated recombinant vector expressing IglC in conjunction with the rLm/iglC vaccine described herein.
In summary, immunization with a recombinant L. monocytogenes vaccine expressing a single antigen unique to F. tularensis induces protection against aerosolized Type A F. tularensis; it is the first genetically defined vaccine and the first recombinant vaccine capable of so doing. A recombinant L. monocytogenes vaccine expressing IglC potentially offers a safer and genetically defined alternative to LVS for protection against a bioterrorist attack with F. tularensis. The strategy of using a vaccine vector that mimics the lifestyle of the target pathogen and enables correct processing and presentation of immunoprotective antigens may have general applicability to vaccines against intracellular pathogens.
Acknowledgments
This work was supported by grant DAMD17-03-1-0052 from the U.S. Army Medical Research and Materiel Command and by grants AI065359 and HL07700 from the National Institutes of Health.
We thank Barbara J. Dillon and Susan Som for technical assistance and Nicole Marlenee and Kristin Jones for assistance with the animal studies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Harris S. Japanese biological warfare research on humans: a case study of microbiology and ethics. Ann N Y Acad Sci. 1992;666:21–52. doi: 10.1111/j.1749-6632.1992.tb38021.x. [DOI] [PubMed] [Google Scholar]
- 2.Christopher GW, Cieslak TJ, Pavlin JA, Eitzen EM., Jr Biological warfare. A historical perspective. Jama. 1997;278:412–7. [PubMed] [Google Scholar]
- 3.Alibek K. Biohazard: the chilling true story of the largest covert biological weapons program in the world, told from the inside by the man who ran it. New York: Random House, Inc; 1999. p. 319. [Google Scholar]
- 4.Conlan WJ, Oyston PC. Vaccines against Francisella tularensis. Ann N Y Acad Sci. 2007;1105:325–50. doi: 10.1196/annals.1409.012. [DOI] [PubMed] [Google Scholar]
- 5.Griffin KF, Oyston PC, Titball RW. Francisella tularensis vaccines. FEMS Immunol Med Microbiol. 2007;49:315–23. doi: 10.1111/j.1574-695X.2007.00219.x. [DOI] [PubMed] [Google Scholar]
- 6.Baron SD, Singh R, Metzger DW. Inactivated Francisella tularensis live vaccine strain protects against respiratory tularemia by intranasal vaccination in an immunoglobulin A-dependent fashion. Infect Immun. 2007;75:2152–62. doi: 10.1128/IAI.01606-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conlan JW, Shen H, Webb A, Perry MB. Mice vaccinated with the O-antigen of Francisella tularensis LVS lipopolysaccharide conjugated to bovine serum albumin develop varying degrees of protective immunity against systemic or aerosol challenge with virulent type A and type B strains of the pathogen. Vaccine. 2002;20:3465–71. doi: 10.1016/s0264-410x(02)00345-6. [DOI] [PubMed] [Google Scholar]
- 8.Sjostedt A, Sandstrom G, Tarnvik A. Humoral and cell-mediated immunity in mice to a 17-kilodalton lipoprotein of Francisella tularensis expressed by Salmonella typhimurium. Infect Immun. 1992;60:2855–62. doi: 10.1128/iai.60.7.2855-2862.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fulop M, Mastroeni P, Green M, Titball RW. Role of antibody to lipopolysaccharide in protection against low- and high-virulence strains of Francisella tularensis. Vaccine. 2001;19:4465–72. doi: 10.1016/s0264-410x(01)00189-x. [DOI] [PubMed] [Google Scholar]
- 10.Golovliov I, Ericsson M, Akerblom L, Sandstrom G, Tarnvik A, Sjostedt A. Adjuvanticity of ISCOMs incorporating a T cell-reactive lipoprotein of the facultative intracellular pathogen Francisella tularensis. Vaccine. 1995;13:261–7. doi: 10.1016/0264-410x(95)93311-v. [DOI] [PubMed] [Google Scholar]
- 11.Huntley JF, Conley PG, Rasko DA, Hagman KE, Apicella MA, Norgard MV. Native outer membrane proteins protect mice against pulmonary challenge with virulent type A Francisella tularensis. Infect Immun. 2008;76:3664–71. doi: 10.1128/IAI.00374-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Twine S, Bystrom M, Chen W, Forsman M, Golovliov I, Johansson A, et al. A mutant of Francisella tularensis strain SCHU S4 lacking the ability to express a 58-kilodalton protein is attenuated for virulence and is an effective live vaccine. Infect Immun. 2005;73:8345–52. doi: 10.1128/IAI.73.12.8345-8352.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pechous RD, McCarthy TR, Mohapatra NP, Soni S, Penoske RM, Salzman NH, et al. A Francisella tularensis Schu S4 purine auxotroph is highly attenuated in mice but offers limited protection against homologous intranasal challenge. PLoS ONE. 2008;3:e2487. doi: 10.1371/journal.pone.0002487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eigelsbach H aCD. Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J Immunol. 1961;87:415–25. [PubMed] [Google Scholar]
- 15.Li J, Ryder C, Mandal M, Ahmed F, Azadi P, Snyder DS, et al. Attenuation and protective efficacy of an O-antigen-deficient mutant of Francisella tularensis LVS. Microbiology. 2007;153:3141–53. doi: 10.1099/mic.0.2007/006460-0. [DOI] [PubMed] [Google Scholar]
- 16.Sebastian S, Dillon ST, Lynch JG, Blalock LT, Balon E, Lee KT, et al. A defined O-antigen polysaccharide mutant of Francisella tularensis live vaccine strain has attenuated virulence while retaining its protective capacity. Infect Immun. 2007;75:2591–602. doi: 10.1128/IAI.01789-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raynaud C, Meibom KL, Lety MA, Dubail I, Candela T, Frapy E, et al. Role of the wbt locus of Francisella tularensis in lipopolysaccharide O-antigen biogenesis and pathogenicity. Infect Immun. 2007;75:536–41. doi: 10.1128/IAI.01429-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hornick RB, Eigelsbach HT. Aerogenic immunization of man with live Tularemia vaccine. Bacteriol Rev. 1966;30:532–8. doi: 10.1128/br.30.3.532-538.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.White JD, Rooney JR, Prickett PA, Derrenbacher EB, Beard CW, Griffith WR. Pathogenesis of Experimental Respiratory Tularemia in Monkeys. J Infect Dis. 1964;114:277–83. doi: 10.1093/infdis/114.3.277. [DOI] [PubMed] [Google Scholar]
- 20.Conlan JW, North RJ. Early pathogenesis of infection in the liver with the facultative intracellular bacteria Listeria monocytogenes, Francisella tularensis, and Salmonella typhimurium involves lysis of infected hepatocytes by leukocytes. Infect Immun. 1992;60:5164–71. doi: 10.1128/iai.60.12.5164-5171.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall JD, Craven RR, Fuller JR, Pickles RJ, Kawula TH. Francisella tularensis replicates within alveolar type II epithelial cells in vitro and in vivo following inhalation. Infect Immun. 2007;75:1034–9. doi: 10.1128/IAI.01254-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCaffrey RL, Allen LA. Francisella tularensis LVS evades killing by human neutrophils via inhibition of the respiratory burst and phagosome escape. J Leukoc Biol. 2006;80:1224–30. doi: 10.1189/jlb.0406287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Golovliov I, Baranov V, Krocova Z, Kovarova H, Sjostedt A. An attenuated strain of the facultative intracellular bacterium Francisella tularensis can escape the phagosome of monocytic cells. Infect Immun. 2003;71:5940–50. doi: 10.1128/IAI.71.10.5940-5950.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clemens DL, Horwitz MA. Uptake and intracellular fate of Francisella tularensis in human macrophages. Ann N Y Acad Sci. 2007;1105:160–86. doi: 10.1196/annals.1409.001. [DOI] [PubMed] [Google Scholar]
- 25.Elkins KL, Cowley SC, Bosio CM. Innate and adaptive immunity to Francisella. Ann N Y Acad Sci. 2007;1105:284–324. doi: 10.1196/annals.1409.014. [DOI] [PubMed] [Google Scholar]
- 26.Pamer EG. Immune responses to Listeria monocytogenes. Nat Rev Immunol. 2004;4:812–23. doi: 10.1038/nri1461. [DOI] [PubMed] [Google Scholar]
- 27.Bruhn KW, Craft N, Miller JF. Listeria as a vaccine vector. Microbes Infect. 2007;9:1226–35. doi: 10.1016/j.micinf.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 28.Angelakopoulos H, Loock K, Sisul DM, Jensen ER, Miller JF, Hohmann EL. Safety and shedding of an attenuated strain of Listeria monocytogenes with a deletion of actA/plcB in adult volunteers: a dose escalation study of oral inoculation. Infect Immun. 2002;70:3592–601. doi: 10.1128/IAI.70.7.3592-3601.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brockstedt DG, Giedlin MA, Leong ML, Bahjat KS, Gao Y, Luckett W, et al. Listeria-based cancer vaccines that segregate immunogenicity from toxicity. Proc Natl Acad Sci U S A. 2004;101:13832–7. doi: 10.1073/pnas.0406035101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Starks H, Bruhn KW, Shen H, Barry RA, Dubensky TW, Brockstedt D, et al. Listeria monocytogenes as a vaccine vector: virulence attenuation or existing antivector immunity does not diminish therapeutic efficacy. J Immunol. 2004;173:420–7. doi: 10.4049/jimmunol.173.1.420. [DOI] [PubMed] [Google Scholar]
- 31.Reilly TJ, Baron GS, Nano FE, Kuhlenschmidt MS. Characterization and sequencing of a respiratory burst-inhibiting acid phosphatase from Francisella tularensis. J Biol Chem. 1996;271:10973–83. doi: 10.1074/jbc.271.18.10973. [DOI] [PubMed] [Google Scholar]
- 32.Mohapatra NP, Balagopal A, Soni S, Schlesinger LS, Gunn JS. AcpA is a Francisella acid phosphatase that affects intramacrophage survival and virulence. Infect Immun. 2007;75:390–6. doi: 10.1128/IAI.01226-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee BY, Horwitz MA, Clemens DL. Identification, recombinant expression, immunolocalization in macrophages, and T-cell responsiveness of the major extracellular proteins of Francisella tularensis. Infect Immun. 2006;74:4002–13. doi: 10.1128/IAI.00257-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barker JR, Klose KE. Molecular and genetic basis of pathogenesis in Francisella tularensis. Ann N Y Acad Sci. 2007;1105:138–59. doi: 10.1196/annals.1409.010. [DOI] [PubMed] [Google Scholar]
- 35.Golovliov I, Ericsson M, Sandstrom G, Tarnvik A, Sjostedt A. Identification of proteins of Francisella tularensis induced during growth in macrophages and cloning of the gene encoding a prominently induced 23-kilodalton protein. Infect Immun. 1997;65:2183–9. doi: 10.1128/iai.65.6.2183-2189.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lai XH, Golovliov I, Sjostedt A. Expression of IglC is necessary for intracellular growth and induction of apoptosis in murine macrophages by Francisella tularensis. Microb Pathog. 2004;37:225–30. doi: 10.1016/j.micpath.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 37.Santic M, Molmeret M, Klose KE, Jones S, Kwaik YA. The Francisella tularensis pathogenicity island protein IglC and its regulator MglA are essential for modulating phagosome biogenesis and subsequent bacterial escape into the cytoplasm. Cell Microbiol. 2005;7:969–79. doi: 10.1111/j.1462-5822.2005.00526.x. [DOI] [PubMed] [Google Scholar]
- 38.Nano FE, Zhang N, Cowley SC, Klose KE, Cheung KK, Roberts MJ, et al. A Francisella tularensis pathogenicity island required for intramacrophage growth. J Bacteriol. 2004;186:6430–6. doi: 10.1128/JB.186.19.6430-6436.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Golovliov I, Sjostedt A, Mokrievich A, Pavlov V. A method for allelic replacement in Francisella tularensis. FEMS Microbiol Lett. 2003;222:273–80. doi: 10.1016/S0378-1097(03)00313-6. [DOI] [PubMed] [Google Scholar]
- 40.Pammit MA, Raulie EK, Lauriano CM, Klose KE, Arulanandam BP. Intranasal vaccination with a defined attenuated Francisella novicida strain induces gamma interferon-dependent antibody-mediated protection against tularemia. Infect Immun. 2006;74:2063–71. doi: 10.1128/IAI.74.4.2063-2071.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blander SJ, Horwitz MA. Vaccination with the major secretory protein of Legionella pneumophila induces cell-mediated and protective immunity in a guinea pig model of Legionnaires’ disease. J Exp Med. 1989;169:691–705. doi: 10.1084/jem.169.3.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Horwitz MA, Harth G, Dillon BJ, Maslesa-Galic S. Recombinant bacillus calmette-guerin (BCG) vaccines expressing the Mycobacterium tuberculosis 30-kDa major secretory protein induce greater protective immunity against tuberculosis than conventional BCG vaccines in a highly susceptible animal model. Proc Natl Acad Sci U S A. 2000;97:13853–8. doi: 10.1073/pnas.250480397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Horwitz MA, Harth G, Dillon BJ, Maslesa-Galic S. A novel live recombinant mycobacterial vaccine against bovine tuberculosis more potent than BCG. Vaccine. 2006;24:1593–600. doi: 10.1016/j.vaccine.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 44.Lauer P, Chow MY, Loessner MJ, Portnoy DA, Calendar R. Construction, characterization, and use of two Listeria monocytogenes site-specific phage integration vectors. J Bacteriol. 2002;184:4177–86. doi: 10.1128/JB.184.15.4177-4186.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kuolee R, Harris G, Conlan JW, Chen W. Oral immunization of mice with the live vaccine strain (LVS) of Francisella tularensis protects mice against respiratory challenge with virulent type A F. tularensis. Vaccine. 2007;25:3781–91. doi: 10.1016/j.vaccine.2007.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Conlan JW, Chen W, Shen H, Webb A, KuoLee R. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microb Pathog. 2003;34:239–48. doi: 10.1016/s0882-4010(03)00046-9. [DOI] [PubMed] [Google Scholar]
- 47.Rayevskaya M, Kushnir N, Frankel FR. Safety and immunogenicity in neonatal mice of a hyperattenuated Listeria vaccine directed against human immunodeficiency virus. J Virol. 2002;76:918–22. doi: 10.1128/JVI.76.2.918-922.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miki K, Nagata T, Tanaka T, Kim YH, Uchijima M, Ohara N, et al. Induction of protective cellular immunity against Mycobacterium tuberculosis by recombinant attenuated self-destructing Listeria monocytogenes strains harboring eukaryotic expression plasmids for antigen 85 complex and MPB/MPT51. Infect Immun. 2004;72:2014–21. doi: 10.1128/IAI.72.4.2014-2021.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shen H, Slifka MK, Matloubian M, Jensen ER, Ahmed R, Miller JF. Recombinant Listeria monocytogenes as a live vaccine vehicle for the induction of protective anti-viral cell-mediated immunity. Proc Natl Acad Sci U S A. 1995;92:3987–91. doi: 10.1073/pnas.92.9.3987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Orr MT, Orgun NN, Wilson CB, Way SS. Cutting Edge: Recombinant Listeria monocytogenes expressing a single immune-dominant peptide confers protective immunity to herpes simplex virus-1 infection. J Immunol. 2007;178:4731–5. doi: 10.4049/jimmunol.178.8.4731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boyer JD, Robinson TM, Maciag PC, Peng X, Johnson RS, Pavlakis G, et al. DNA prime Listeria boost induces a cellular immune response to SIV antigens in the rhesus macaque model that is capable of limited suppression of SIV239 viral replication. Virology. 2005;333:88–101. doi: 10.1016/j.virol.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 52.Brockstedt DG, Bahjat KS, Giedlin MA, Liu W, Leong M, Luckett W, et al. Killed but metabolically active microbes: a new vaccine paradigm for eliciting effector T-cell responses and protective immunity. Nat Med. 2005;11:853–60. doi: 10.1038/nm1276. [DOI] [PubMed] [Google Scholar]
- 53.Belyi YF, Petrosov VV, Tartakovskii IS, Suchkov YG. Live tularemia vaccine but not proteins purified from Francisella tularensis can confer protection against lethal Listeria infection in mice. Apmis. 1995;103:107–12. [PubMed] [Google Scholar]
- 54.Belyi YF, Tartakovskii IS, Mesheryakova IS, Petrosov VV, Prosorovskii SV. Live tularemia vaccine confers protection against lethal Legionella and Listeria infections in experimental animals. FEMS Immunol Med Microbiol. 1996;13:211–3. doi: 10.1111/j.1574-695X.1996.tb00239.x. [DOI] [PubMed] [Google Scholar]
- 55.Elkins KL, MacIntyre AT, Rhinehart-Jones TR. Nonspecific early protective immunity in Francisella and Listeria infections can be dependent on lymphocytes. Infect Immun. 1998;66:3467–9. doi: 10.1128/iai.66.7.3467-3469.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lindgren H, Golovliov I, Baranov V, Ernst RK, Telepnev M, Sjostedt A. Factors affecting the escape of Francisella tularensis from the phagolysosome. J Med Microbiol. 2004;53:953–8. doi: 10.1099/jmm.0.45685-0. [DOI] [PubMed] [Google Scholar]
- 57.Quarry JE, Isherwood KE, Michell SL, Diaper H, Titball RW, Oyston PC. A Francisella tularensis subspecies novicida purF mutant, but not a purA mutant, induces protective immunity to tularemia in mice. Vaccine. 2007;25:2011–8. doi: 10.1016/j.vaccine.2006.11.054. [DOI] [PubMed] [Google Scholar]
- 58.Bakshi CS, Malik M, Mahawar M, Kirimanjeswara GS, Hazlett KR, Palmer LE, et al. An improved vaccine for prevention of respiratory tularemia caused by Francisella tularensis SchuS4 strain. Vaccine. 2008;26:5276–88. doi: 10.1016/j.vaccine.2008.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Qin A, Scott DW, Thompson JA, Mann BJ. Identification of an essential Francisella tularensis subsp. tularensis virulence factor. Infect Immun. 2008 doi: 10.1128/IAI.01113-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bruhn KW, Craft N, Nguyen BD, Yip J, Miller JF. Characterization of anti-self CD8 T-cell responses stimulated by recombinant Listeria monocytogenes expressing the melanoma antigen TRP-2. Vaccine. 2005;23:4263–72. doi: 10.1016/j.vaccine.2005.02.018. [DOI] [PubMed] [Google Scholar]