Abstract
Objective
To investigate the efficacy of cholecalciferol (vitamin D3) in raising serum 25-hydroxyvitamin D (25[OH)]D) levels and reducing parathyroid hormone (PTH) levels in patients with chronic kidney disease (CKD).
Methods
In this double-blind, randomized controlled pilot study, participants with CKD stage 3 and 4 (estimated glomerular filtration rate, 15–59 mL/min/1.73 m2), vitamin D insufficiency (serum 25[OH]D <30 ng/mL), and serum intact PTH levels >70 pg/mL were randomly assigned to receive either 50 000 IU of cholecalciferol or placebo once weekly for 12 weeks. Primary outcomes (25[OH]D and PTH levels) were measured at baseline, week 6, and week 12. Secondary outcomes (1,25-dihydroxvitamin D and bone turnover markers) were measured at baseline and week 12. Because of skewed data distribution, statistical analyses were performed on a logarithmic scale. The difference between the group means was exponentiated to provide the geometric mean ratio. A linear mixed model using an unstructured variance-covariance matrix was used to examine change in the primary and secondary outcomes over time.
Results
Geometric mean serum 25(OH)D concentrations of the study groups were similar at baseline (P = .77). At week 6, a significant difference between the treatment and placebo groups was detected (P = .001); this difference was maintained at week 12 (P = .002). Among cholecalciferol-treated participants, serum 25(OH)D concentration increased on average from 17.3 ng/mL (95% confidence interval [CI], 11.8–25.2) at baseline to 49.4 ng/mL (95% CI, 33.9–72.0) at week 12. As-treated analysis indicated a trend toward lower PTH levels among cholecalciferol-treated participants (P = .07).
Conclusion
Weekly cholecalciferol supplementation appears to be an effective treatment to correct vitamin D status in patients with CKD.
INTRODUCTION
Vitamin D is an important nutrient for calcium homeostasis and optimal bone health (1,2). The main circulating form of vitamin D is 25-hydroxyvitamin D (25[OH]D) (calcidiol), which requires activation by renal 1 α-hydroxylase to form the metabolically active form of vitamin D, 1,25-dihydroxvitamin D (1,25[OH]2D) (calcitriol) (3). Parathyroid hormone (PTH) increases activity of the renal 1 α-hydroxylase in response to low calcium levels (4). Because chronic kidney disease (CKD) results in decreased kidney mass, there is a compensatory elevation in PTH to maintain adequate blood levels of 1,25(OH)2D for optimal intestinal absorption of calcium (5). Chronic elevation of PTH, termed secondary hyperparathyroidism, in combination with altered phosphorus metabolism (6), can lead to renal osteodystrophy (7) and increased mortality due to cardiovascular disease (8).
Low serum 25(OH)D levels can further exacerbate hyperparathyroidism in patients with CKD (9). There is an inverse relationship between PTH and 25(OH)D levels in healthy individuals (10,11) and in patients with CKD (12). A recent cross-sectional study of patients from geographically diverse regions of the United States has shown that up to 86% of predialysis patients with CKD are vitamin-D insufficient (12). The National Kidney Foundation guidelines state that optimal 25(OH)D levels should be greater than 30 ng/mL (13). The National Kidney Foundation recommends correction of vitamin D insufficiency with oral ergocalciferol; however, these recommendations are based on limited prospective clinical trials (13). Treatment of secondary hyperparathyroidism involves addressing vitamin D status followed by various therapies to reduce PTH levels including calcitriol, vitamin D analogues, calcimimetics such as cinacalcet hydrochloride, or parathyroid-ectomy (13). Furthermore, there are no data regarding patients with CKD from studies evaluating the correction of vitamin D insufficiency with cholecalciferol (vitamin D3), which appears to more effectively raise 25(OH)D levels than ergocalciferol (vitamin D2) (14,15).
We conducted a double-blind, placebo-controlled, 12-week pilot study to evaluate the effectiveness of weekly supplementation with cholecalciferol in reducing PTH levels and correcting vitamin D insufficiency in patients with stage 3 and 4 CKD. Primary endpoints assessed were 25(OH)D and PTH levels. We were interested in determining 25(OH)D and PTH levels over the 12-week period and in analyzing whether changes in these outcomes were dependent on the intervention therapy. For the secondary endpoints, we examined the change from baseline in levels of 1,25(OH)2D and bone turnover markers—bone-specific alkaline phosphatase, C-telopeptide, and tartarate-resistant acid phosphatase isoform 5b (TRAP5b).
PATIENTS AND METHODS
The study was approved by the Emory University Institutional Review Board and was conducted at the Emory Clinic.
Study Participants
Patients with CKD whose conditions were clinically stable were prescreened for eligibility on the basis of the following inclusion criteria: age, 18 to 85 years; CKD, stage 3 or 4 (estimated glomerular filtration rate, 15 to 59 mL/min/1.73 m2 body surface area measured twice 90 days apart); serum 25(OH)D concentrations, 30 ng/mL or less; and serum PTH levels, greater than 70 pg/mL documented within the last 6 months. Estimated glomerular filtration rate was calculated by using the original Modification of Diet in Renal Disease Study equation (online at http://www.nkdep.nih.gov) (16). Participants were excluded on the basis of the following criteria: history of liver failure (serum aspartate aminotransferase or alanine aminotransferase level greater than 3-fold the upper limit of the reference range); requirement of dialysis at any stage of the study; history of intestinal malabsorption or chronic diarrhea; serum calcium level (corrected for serum albumin) greater than 10.5 mg/dL; calcium ×phosphorus product greater than 70; treatment with more than 1000 IU of vitamin D per day; or current treatment with a vitamin D analogue or calcimimetic, an antiepileptic medication, or other medications that could affect vitamin D metabolism (eg, phenobarbital, phenytoin, rifampicin) (17).
Eligible participants who had given their informed consent were assigned in a double-blind manner into the cholecalciferol and placebo groups using permuted blocked randomization of size 2 (18). Blocked randomization guaranteed that after every second randomly assigned participant, the number of participants in each group were equal. Participants were randomly assigned according to their levels of 25(OH)D and PTH determined within the last 3 months of screening. On the basis of 25(OH)D and PTH baseline measurements that were assessed at the beginning of the study, some participants were determined ineligible shortly after randomization, and thus it was decided to exclude these individuals from further participation. Postrandomization dropouts were equal in both groups. Because no further information was available from these dropouts, we completed an as-treated analysis.
Participants had blood drawn to establish baseline levels of serum creatinine, 25(OH)D, 1,25(OH)2D, PTH, calcium, phosphate, and bone turnover markers (bone-specific alkaline phosphatase, TRAP5b, and C-telopeptide). Participants in the cholecalciferol treatment group ingested 50 000 IU of cholecalciferol once weekly for 12 weeks (Tischon, Salisbury, Maryland). Participants in the placebo group ingested a pill identical in appearance to cholecalciferol once weekly for 12 weeks (Tischon, Salisbury, Maryland). At baseline, week 6, and week 12, measurements of the primary endpoints (25[OH]D and PTH) were performed. Measurements of the secondary endpoints (1,25[OH]2D, bone-specific alkaline phosphatase, C-telopeptide, and TRAP5b) were performed at baseline and week 12.
Analytic Methods
Measurements of serum calcium, phosphate, albumin, alanine aminotransferase, aspartate aminotransferase, and creatinine were performed using standard methods of the Emory University Hospital Chemistry Laboratory. Commercially available enzyme-linked immunosorbent kits were used to measure concentrations of serum 25(OH)D and 1,25(OH)2D (IDS Ltd, Fountain Hills, Arizona), PTH (Diagnostic Systems Laboratories, Webster, Texas), bonespecific alkaline phosphatase (IDS Ltd, Fountain Hills, Arizona), C-telopeptide (Quidel, San Diego, California), and TRAP5b (Quidel, San Diego, California).
Statistical Methods
Because of the skewed distributions of 25(OH)D and PTH data, statistical analyses by treatment group were performed on a logarithmic scale so that the data distribution would be roughly Gaussian. Because the data were log-transformed, each mean was expo-nentiated to express the result in the original unit of measurement. The exponentiated arithmetic mean of the log-transformed data is the geometric mean of the original data. Exponentiating the difference between group arithmetic means of the log-transformed values provided the geometric mean ratio. A geometric mean ratio of 1 suggests no treatment effect.
Measurements of the primary endpoints were performed on the same participant at 3 time points. The linear mixed model (19) was used in the analysis because it allowed us to address patterns of correlation and variation that are typically present in data obtained from repeated measurements. The model-based means are unbiased with unbalanced and missing data, as long as the missing data are uninformative (missing at random). Valid standard errors were calculated, and efficient statistical tests were performed. An unstructured variance-covariance form among the repeated measurements was assumed for each outcome. Any difference in response profiles among treatments was reflected in the group-by-time interaction term, indicating that group differences varied with time. Measurements of the secondary study endpoints were performed at baseline and at week 12. To compare the 2 treatment groups, we used analysis of covariance, treating the baseline measurement as a covariate in the model (20).
The study was designed to have 80% power to detect a difference of 10 ng/mL in 25(OH)D between the cholecalciferol and placebo groups at the end of 12 weeks, with a standard deviation of 10 ng/mL (21) at a significance level of 0.05 using a 2-sample t test. We estimated that 17 participants would be needed for each group. No adjustment was made for participant withdrawal or dropout. All statistical calculations were performed using SAS version 9.1. Confidence intervals were determined using a confidence level of 95%; statistical tests were 2-sided and performed at a 5% level of significance. Biostatistical support was provided by the Emory University Biostatistics Consulting Center.
RESULTS
Baseline Participant Characteristics
Forty-five participants were eligible on prescreening on the basis of estimated glomerular filtration rates and serum PTH and 25(OH)D levels. Thirty-four subjects agreed to participate and gave initial consent for the study. Participants were randomly assigned equally to the placebo group (n = 17) and the cholecalciferol treatment group (n = 17). Two participants in the cholecalciferol group and 1 in the placebo group were excluded after the baseline 25(OH)D level was determined to be greater than 30 ng/ mL. Three participants in the placebo group and 2 participants in the cholecalciferol group were excluded after baseline PTH was determined to be less than 70 pg/mL. During the study, 2 participants in the cholecalciferol group and 2 participants in the placebo group withdrew consent. One participant in the cholecalciferol group and 1 participant in the placebo group were lost to follow-up. Thus, a total of 10 participants in each of the placebo and cholecalciferol groups completed the 12-week study and were eligible for the as-treated analysis.
Participants in the placebo and cholecalciferol treatment groups were similar with respect to sex, age, ethnicity, serum albumin levels, and hemoglobin levels (Table 1). Nine out of 10 participants in the cholecalciferol group and 8 out of 10 in placebo group consumed daily over-the-counter vitamin D supplements, but none consumed more than 800 IU of vitamin D as determined by history.
Table 1.
Baseline Characteristics of Patients With Chronic Kidney Disease Treated With Placebo or Cholecalciferol (Vitamin D3)a
| Placebo | Cholecalciferol | |
|---|---|---|
| Characteristics | (n = 10) | (n = 10) |
| Ethnicity, No. | ||
| African American | 7 | 6 |
| Nonhispanic white | 3 | 4 |
| Female, No. | 6 | 6 |
| Age, y | 59.5 (10.4) | 62.2 (11) |
| GFR, mL/min/1.73 m2 body surface area | 29.8 (13.6) | 33.3 (26.8) |
| Stage 4 kidney disease (GFR,15– 30 mL/min/1.73 m2 body surface area), No. |
5 | 3 |
| Stage 3 kidney disease (GFR, 31– 59 mL/min/1.73 m2 body surface area), No. |
5 | 7 |
| Serum albumin, g/dL | 3.7 (0.3) | 3.5 (0.3) |
| Hemoglobin, g/dL | 11.9 (0.9) | 12.0 (1.6) |
| Serum phosphorus, mg/dL | 3.9 (0.6) | 4.1 (0.6) |
| Calcium ×phosphorus product | 36.3 (7.6) | 39.3 (7.5) |
| Serum AST, U/L | 22.3 (5.4) | 24.2 (9.2) |
| Serum ALT, U/L | 18.2 (4.7) | 21.8 (8.8) |
| Participants taking daily multivitamin supplements, No. |
8 | 9 |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; GFR, glomerular filtration rate.
Data are presented as mean (SD) unless otherwise indicated.
Serial Calcium, Vitamin D, and PTH Levels
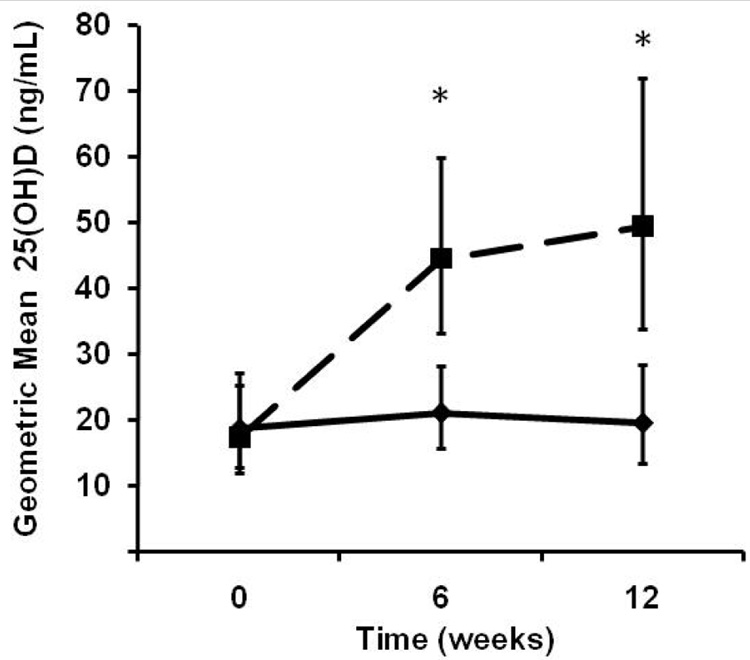
The change in both primary and secondary outcomes from baseline to week 12 is summarized in Table 2. Although the 25(OH)D geometric means of the cholecalciferol and placebo groups were not significantly different at baseline (P = .77), the gap between the treatment groups began to emerge at week 6 (P = .001) and was maintained at week 12 (P = .002). The treatment group-by-time interaction was significant (P<.001). Fig. 1 shows the 25(OH)D response profiles of the 2 treatment groups during the 12-week study period.
Table 2.
Serum Measures of Vitamin D Status and Bone Metabolism in Patients With Chronic Kidney Disease Treated With Placebo or Cholecalciferol (Vitamin D3)a,b
| Placebo |
Cholecalciferol |
|||||
|---|---|---|---|---|---|---|
| Analyte | Week 0 | Week 6 | Week 12 | Week 0 | Week 6 | Week 12 |
| Total | 9.0 | 9.5 | 9.1 | 9.7 | ||
| calcium, | (8.8–9.3) | … | (9.3–9.6) | (8.9–9.4) | … | (9.5–9.8) |
| mg/dL | n = 9 | n = 10 | n = 9 | n = 10 | ||
| 25(OH)D, | 18.6 | 21 | 19.5 | 17.3 | 44.5 | 49.4 |
| ng/mL | (12.8–27.1) | (15.7–28.2) | (13.4–28.4) | (11.8–25.2) | (33.1–59.8) | (33.9–72.0) |
| n = 10 | n = 9 | n = 10 | n = 10 | n = 7 | n = 10 | |
| PTH, pg/mL | 290.5 | 335.1 | 269.7 | 288.9 | 254.7 | 200.5 |
| (179.7–469.8) | (214.2–524.1) | (153.3–474.5) | (178.7–467.2) | (161.4–401.9) | (114.0–352.8) | |
| n = 10 | n = 9 | n = 10 | n = 10 | n = 7 | n = 10 | |
| 1,25(OH)2D, | 29.7 | 30.8 | 29.1 | 40.2 | ||
| pg/mL | (17.3–51.0) | … | (24.8–38.1) | (16.9–50.0) | … | (32.8–49.2) |
| n = 9 | n = 9 | n = 10 | n = 10 | |||
| BAP, IU/L | 18.4 | 22.0 | 20.3 | 20.4 | ||
| (10.2–33.3) | … | (19.3–25.0) | (13.4–30.5) | … | (18.0–23.1) | |
| n = 8 | n = 8 | n = 9 | n = 9 | |||
| CTX, pg/mL | 0.36 | 0.24 | 0.34 | 0.29 | ||
| (0.18–0.74) | … | (0.14–0.40) | (0.15–0.76) | … | (0.18–0.49) | |
| n = 8 | n = 8 | n = 9 | n = 9 | |||
| TRAP5b, | 2.9 | 3.5 | 3.8 | 3.2 | ||
| pg/mL | (1.8–4.8) | … | (2.9–4.1) | (2.5–5.6) | … | (2.7–3.8) |
| n = 9 | n = 9 | n = 10 | n = 10 | |||
Abbreviations: BAP, bone-specific alkaline phosphatase; CTX, serum C-telopeptide; 1,25(OH)2D, 1,25-dihydroxyvitamin D; 25(OH)D, 25-hydroxyvitamin D; PTH, parathyroid hormone; TRAP5b, tartarate-resistant acid phosphatase isoform 5b.
Because the data were log-transformed, the mean was exponentiated to express the results in the original unit of measurement; the result is the geometric mean. To compare the geometric means of the treatment and placebo groups, the geometric mean ratio is used. A ratio equal to 1 suggests no treatment effect.
Data are presented as sample geometric mean (95% confidence interval for the true geometric mean).
Fig. 1.
Geometric mean for serum 25-hydroxyvitamin D (25[OH]D) concentrations in patients with stage 3 and 4 chronic kidney disease treated with placebo or cholecalciferol, 50 000 IU once weekly, for 12 weeks. Serum 25(OH)D levels were measured as a marker of vitamin D status in participants treated with placebo (diamonds) or cholecalciferol (squares) at baseline, 6 weeks, and 12 weeks of the study. The response profiles of cholecalciferol-treated and placebo-treated patients are significantly different starting at 6 weeks and at 12 weeks (P<.001) as indicated by the asterisks. Error bars indicate 95% confidence intervals.
Baseline serum 1,25(OH)2D levels were similar in both groups, with a geometric mean ratio of 1.04 (P = .95); at the end of 12 weeks, the geometric mean ratio increased to 1.38, which was not significant (P = .07). No significant change in calcium level was observed at baseline (P = .67) or at the end of 12 weeks (P = .12). No participant developed hypercalcemia (corrected serum calcium level greater than 10.5 mg/dL) during the study.
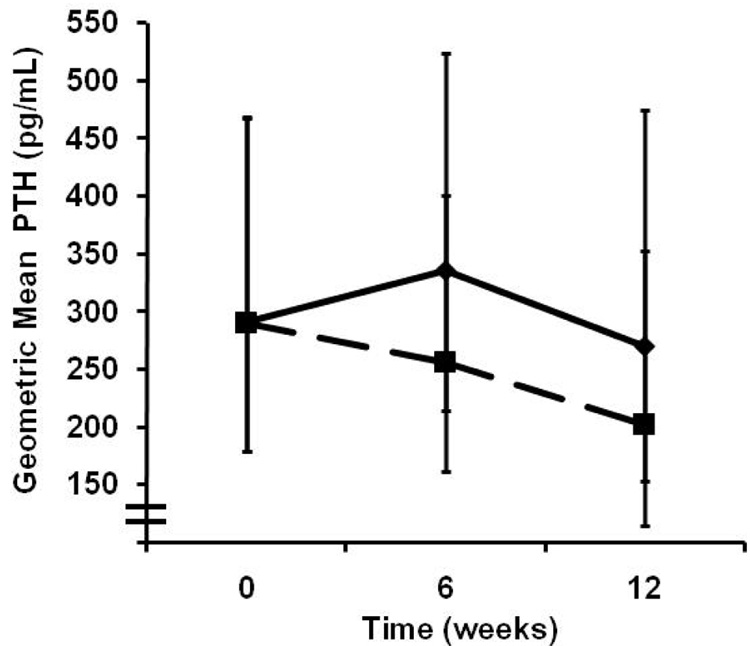
In explaining the variability in log serum PTH concentration, the interaction of time of visit and treatment was insignificant (P = .14). This suggests that the PTH geometric mean ratio between the intervention and placebo groups was not significantly different from 1 at all 3 time points. Fig. 2 shows that although the PTH geometric mean of the cholecalciferol group was lower at weeks 6 and 12, the PTH variability was too high to ascribe significance.
Fig. 2.
Geometric mean for serum parathyroid hormone (PTH) concentrations in patients with stage 3 and 4 chronic kidney disease treated with placebo or cholecalciferol, 50 000 IU once weekly, for 12 weeks. Serum PTH levels were measured in participants treated with placebo (diamonds) or cholecalciferol (squares) at baseline, 6 weeks, and 12 weeks of the study. The PTH levels of the 2 study groups are not significantly different at each of the 3 time points (P = .14). Error bars indicate 95% confidence intervals.
Markers of Bone Turnover—Bone-Specific Alkaline Phosphatase, C-telopeptide, TRAP5b
As the overlapping 95% confidence intervals in Table 2 suggest, taking into account the baseline values, no statistically significant difference between the 2 study groups was observed in levels of bone turnover markers at the end of 12 weeks: serum bone-specific alkaline phosphatase (bone formation marker), P = .39; serum C-telopeptide (bone resorption marker), P = .55; and TRAP5b (osteoclast function marker), P = .46.
DISCUSSION
Findings from our as-treated analysis demonstrate that weekly supplementation with 50 000 IU of cholecalciferol for 12 weeks is an effective way of correcting vitamin D status in patients with CKD stage 3 and 4. Nine of the 10 subjects randomly assigned to receive cholecalciferol treatment became vitamin D sufficient (serum values 30 ng/mL or greater) within 6 weeks of supplementation. At 12 weeks of therapy, participants supplemented with cholecalciferol demonstrated an average increase of 185% in serum 25(OH)D concentrations compared with an average increase of 5% in the placebo group. At 12 weeks, PTH levels also decreased by 31% in the cholecalciferol-treated group compared with only a 7% decrease in the placebo group, but this did not achieve statistical significance because of the high PTH variability. None of the subjects developed hypercalcemia or other adverse events.
Several protocols exist to correct vitamin D insufficiency in healthy adults including a single high dose of ergocalciferol orally (22), a daily dosage of ergocalciferol or cholecalciferol for several months (23,24), or weekly high doses of ergocalciferol (50 000 IU once or twice weekly) (25,26). Elevated PTH due to vitamin D deficiency will return to normal levels in most healthy individuals without CKD after correction of vitamin D status (26,27).
In patients with CKD, several small studies have evaluated ergocalciferol to correct vitamin D insufficiency. Many of these studies have been retrospective analyses, which demonstrate variable results in the effectiveness of ergocalciferol in reducing PTH values in patients with CKD. A study to evaluate the effectiveness of the Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines found that only about 60% of participants with stage 3 and 4 CKD who were given ergocalciferol therapy (up to 50 000 IU weekly) reached 25(OH)D levels greater than 30 ng/mL (28). The ergocalciferol therapy resulted in a 13% decrease and 2% increase in PTH level in participants with stage 3 and 4 CKD, respectively (28). Pesenson et al retrospectively evaluated 45 patients with CKD who were mildly vitamin-D insufficient (mean serum 25(OH)D concentration of 26.1 ng/mL) and who were treated with ergocalciferol in wide range of dosages over a 6-month period (29). The investigators found that serum 25(OH)D levels increased only slightly (mean of 8.1 ng/mL) and, as expected, that there was no change in PTH values from baseline assessment. In a similar retrospective study, Shah et al reported that treatment with various regimens of ergo-calciferol did not decrease PTH values significantly (30). In a larger study of 85 patients with stage 3 to 5 CKD, Thorp et al reported that PTH levels decreased significantly (about 16%) after 12 weeks of ergocalciferol therapy ranging from a mean daily dosage of 800 IU to 7100 IU (31). In another study, patients with CKD receiving peritoneal dialysis who were given 50 000 IU ergocalciferol per week for 4 weeks had only a 7% decrease in PTH levels (32). Thus, ergocalciferol therapy in CKD is generally modestly effective in correcting vitamin D nutriture and/or the current dosing recommendations are inadequate to reach target levels established by the National Kidney Foundation.
In healthy individuals, several investigators have demonstrated that ergocalciferol is less effective in raising 25(OH)D levels than cholecalciferol (14,15). Trang and colleagues gave healthy participants 4000 IU of ergocalciferol or cholecalciferol for 14 days and found that the rise in serum 25(OH)D levels in the cholecalciferol treatment group was nearly twice the rise observed in the ergocalciferol treatment group (15). Armas et al demonstrated that a single cholecalciferol dose of 50 000 IU was much more effective in raising 25(OH)D levels than ergocalciferol (14). These findings are of interest because the National Kidney Foundation currently recommends ergocalciferol for correction of vitamin D insufficiency in patients with CKD, and ergocalciferol is the only vitamin D available by prescription in high-dose strength (13). The precise explanation for why cholecalciferol is more effective than ergocalciferol in raising 25(OH)D levels is not known, but has been proposed by some to be due in part to ergocalciferol’s weaker affinity to vitamin D–binding protein (33).
Optimal vitamin D status is important to decrease PTH secretion in patients with CKD. Circulating 25(OH)D provides the substrate for the renal 1α-hydroxylase to form 1,25(OH)2D, which binds to the vitamin D receptor in the parathyroid cell to decrease secretion of PTH (34). The parathyroid gland itself also contains 1α-hydoxylase so that the metabolically active form of vitamin D can be produced locally in a paracrine/auto-crine fashion to inhibit PTH (35,36). Several other tissues such as colon, breast, placenta, and prostate also contain the 1α-hydroxylase, which further supports the role for paracrine/autocrine regulation by 1,25(OH)2D (37–40). Findings from preclinical studies suggest that locally produced 1,25(OH)2D acts as an antiproliferative hormone to prevent the growth of various malignancies (41).
Secondary hyperparathyroidism results from stimulation of the parathyroid gland in response to decreased circulating calcium and 25(OH)D (5). Chronic stimulation of the parathyroid gland causes hyperplasia of the parathyroid tissue to compensate for declining renal 1α-hydroxylase and decreased production of 1,25(OH)2D (42). In patients with CKD, phosphate levels are commonly elevated, which inhibit the renal 1α-hydroxylase and decrease serum calcium levels to further exacerbate hyperparathyroidism (43). Uremia also decreases the production of megalin, an important carrier protein that transports 25(OH)D into the proximal tubules before hydroxylation by the renal 1α-hydroxylase (44). Decreased 25(OH)D substrate into the renal epithelial before conversion to the metabolically active 1,25(OH)2D worsens hyperparathyroidism.
Vitamin D status is often addressed late in the treatment course of patients with CKD. In a cross-sectional study by LaClair et al, most patients in CKD stage 3 and 4 exhibited vitamin D insufficiency (12). It is not known whether earlier intervention with attention to optimizing vitamin D status would decrease the incidence of hyperparathyroidism in CKD in the later stages. Improving vitamin D status by restoring 25(OH)D levels to normal is not usually associated with increases in 1,25(OH)2D because the production of 1,25(OH)2D is tightly regulated by PTH and calcium levels in healthy individuals (45). We show that raising serum 25(OH)D levels more than 2-fold with cholecalciferol therapy is associated with increases in 1,25(OH)2D with a trend towards significance (P = .07 after 12 weeks of therapy). This finding indicates that circulating concentrations of 25(OH)D are important for production of 1,25(OH)2D in patients with CKD who have limited renal 1α-hydroxylase activity (46).
Hyperparathyroidism has serious consequences in patients with CKD. Increased cardiovascular mortality has been attributed to hyperparathyroidism (47,48). Chronic hyperparathyroidism can lead to renal osteodys-trophy, which increases the risk for osteoporotic fractures (49). Less-calcemic vitamin D analogues and calcimimetics have been developed to decrease PTH secretion (50); however, data addressing whether treatment with vitamin D analogues improves survival in patients with CKD in large randomized controlled studies are still lacking.
One of the study limitations is that we did not evaluate cholecalciferol vs ergocalciferol in a head-to-head manner; therefore, we cannot conclude that cholecalciferol is superior to ergocalciferol in treating vitamin D insufficiency in patients with CKD. Our study findings do demonstrate that serum 25(OH)D increases significantly (by greater than 2-fold) in patients after 12 weeks of receiving 50 000 IU of cholecalciferol weekly and that this treatment is safe. This response is much higher than reported treatment responses to high-dose ergocalciferol (31,32). We did not evaluate the impact of correcting vitamin D status on bone health and cardiovascular outcomes. We evaluated only surrogate makers of bone including bone formation and bone resorption markers. Larger and more long-term studies are needed to determine whether correction of vitamin D status would improve bone and cardiovascular health.
CONCLUSION
Treatment of vitamin D insufficiency with cholecalciferol, 50 000 IU once a week for 12 weeks, in patients with CKD results in optimal vitamin D status in most individuals. This regimen is safe, inexpensive, and associated with a trend toward a decrease in PTH levels. Correction of vitamin D status in all patients with CKD should be undertaken in the earlier stages of renal failure to prevent secondary hyperparathyroidism. Larger studies to address the long-term impact of optimizing vitamin D status on bone health, cardiovascular outcomes, and mortality with cholecalciferol therapy in patients with stage 3 and 4 CKD are recommended.
ACKNOWLEDGMENT
The investigators acknowledge the assistance of physicians Dr. Patrick Bowen, Dr. Sabreena Basu, Dr. Sumathi Srivatsa, and Dr. Priya Dayamani in the referral of participants for the study.
This work is part of a master’s thesis submitted to the Graduate Program in Nutrition and Health Sciences, Emory University, Atlanta, Georgia.
This work is supported by the UV Foundation, Atlanta VA Medical Center, Atlanta Research and Education Foundation, and NIH K23AR054334.
Abbreviations
- CKD
chronic kidney disease
- 1,25(OH)2D
1,25-dihydroxvitamin D
- 25(OH)D
25-hydroxyvitamin D
- PTH
parathyroid hormone
- TRAP5b
tartarate-resistant acid phosphatase isoform 5b
Footnotes
DISCLOSURE
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80 Suppl 6:1678–1688. doi: 10.1093/ajcn/80.6.1678S. [DOI] [PubMed] [Google Scholar]
- 2.Heaney RP. The Vitamin D requirement in health and disease. J Steroid Biochem Mol Biol. 2005;97:13–19. doi: 10.1016/j.jsbmb.2005.06.020. [DOI] [PubMed] [Google Scholar]
- 3.DeLuca HF. Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr. 2004;80 Suppl 6:1689–1696. doi: 10.1093/ajcn/80.6.1689S. [DOI] [PubMed] [Google Scholar]
- 4.Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 2001;22:477–501. doi: 10.1210/edrv.22.4.0437. [DOI] [PubMed] [Google Scholar]
- 5.Slatopolsky E, Brown A, Dusso A. Pathogenesis of secondary hyperparathyroidism. Kidney Int Suppl. 1999;73:14–19. doi: 10.1046/j.1523-1755.1999.07304.x. [DOI] [PubMed] [Google Scholar]
- 6.Ganesh CK, Stack AG, Levin NW, Hulbert-Shearon T, Port FK. Association of elevated serum PO(4), Ca x PO(4) product, parathyroid hormone with cardiac risk in chronic hemodialysis patients. J Am Soc Nephrol. 2001;12:2131–2138. doi: 10.1681/ASN.V12102131. [DOI] [PubMed] [Google Scholar]
- 7.Malluche H, Faugere MC. Renal bone disease 1990: an unmet challenge for the nephrologist. Kidney Int. 1990;38:193–211. doi: 10.1038/ki.1990.187. [DOI] [PubMed] [Google Scholar]
- 8.Teng M, Wolf M, Lowrie E, Ofsthun N, Lazarus JM, Thadhani R. Survival of patients undergoing hemodialysis with paricalcitol or calcitriol therapy. N Engl J Med. 2003;349:446–456. doi: 10.1056/NEJMoa022536. [DOI] [PubMed] [Google Scholar]
- 9.Cannata-Andía JB, Gómez Alonso C. Vitamin D deficiency: a neglected aspect of disturbed calcium metabolism in renal failure. Nephrol Dial Transplant. 2002;17:1875–1878. doi: 10.1093/ndt/17.11.1875. [DOI] [PubMed] [Google Scholar]
- 10.Chapuy MC, Preziosi P, Maamer M, et al. Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int. 1997;7:439–443. doi: 10.1007/s001980050030. [DOI] [PubMed] [Google Scholar]
- 11.Tangpricha V, Pearce EN, Chen TC, Holick MF. Vitamin D insufficiency among free-living healthy young adults. Am J Med. 2002;112:659–662. doi: 10.1016/s0002-9343(02)01091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.LaClair RE, Hellman RN, Karp SL, et al. Prevalence of calcidiol deficiency in CKD: a cross-sectional study across latitudes in the United States. Am J Kidney Dis. 2005;45:1026–1033. doi: 10.1053/j.ajkd.2005.02.029. [DOI] [PubMed] [Google Scholar]
- 13.National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42 Suppl 3:1–201. [PubMed] [Google Scholar]
- 14.Armas LA, Hollis BW, Heaney RP. Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab. 2004;89:5387–5391. doi: 10.1210/jc.2004-0360. [DOI] [PubMed] [Google Scholar]
- 15.Trang HM, Cole DE, Rubin LA, Pierratos A, Siu S, Vieth R. Evidence that vitamin D3 increases serum 25-hydroxyvitamin D more efficiently than does vitamin D2. Am J Clin Nutr. 1998;68:854–858. doi: 10.1093/ajcn/68.4.854. [DOI] [PubMed] [Google Scholar]
- 16.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 17.Pascussi JM, Robert A, Nguyen M, et al. Possible involvement of pregnane X receptor-enhanced CYP24 expression in drug-induced osteomalacia. J Clin Invest. 2005;115:177–186. doi: 10.1172/JCI21867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedman L, Furberg CD, DeMets DL. Fundamentals of Clinical Trials. 3rd ed. New York, NY: Springer Science+Business Media; 1998. p. 361. [Google Scholar]
- 19.Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York, NY: Springer-Verlag; 2000. p. 608. [Google Scholar]
- 20.Matthews JNS. Introduction to Randomized Controlled Clinical Trials. New York, NY: Chapman & Hall; 2006. p. 304. [Google Scholar]
- 21.Tangpricha V, Koutkia P, Rieke SM, Chen TC, Perez AA, Holick MF. Fortification of orange juice with vitamin D: a novel approach for enhancing vitamin D nutritional health. Am J Clin Nutr. 2003;77:1478–1483. doi: 10.1093/ajcn/77.6.1478. [DOI] [PubMed] [Google Scholar]
- 22.Shah BR, Finberg L. Single-day therapy for nutritional vitamin D-deficiency rickets: a preferred method. J Pediatr. 1994;125:487–490. doi: 10.1016/s0022-3476(05)83303-7. [DOI] [PubMed] [Google Scholar]
- 23.Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003;77:204–210. doi: 10.1093/ajcn/77.1.204. [erratum in Am J Clin Nutr. 2003;78:1047] [DOI] [PubMed] [Google Scholar]
- 24.Vieth R, Chan PC, MacFarlane GD. Efficacy and safety of vitamin D3 intake exceeding the lowest observed adverse effect level. Am J Clin Nutr. 2001;73:288–294. doi: 10.1093/ajcn/73.2.288. [DOI] [PubMed] [Google Scholar]
- 25.Adams JS, Kantorovich V, Wu C, Javanbakht M, Hollis BW. Resolution of vitamin D insufficiency in osteopenic patients results in rapid recovery of bone mineral density. J Clin Endocrinol Metab. 1999;84:2729–2730. doi: 10.1210/jcem.84.8.5899. [DOI] [PubMed] [Google Scholar]
- 26.Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351:805–806. doi: 10.1016/s0140-6736(05)78933-9. [DOI] [PubMed] [Google Scholar]
- 27.Kantorovich V, Gacad MA, Seeger LL, Adams JS. Bone mineral density increases with vitamin D repletion in patients with coexistent vitamin D insufficiency and primary hyperparathyroidism. J Clin Endocrinol Metab. 2000;85:3541–3543. doi: 10.1210/jcem.85.10.6909. [DOI] [PubMed] [Google Scholar]
- 28.Zisman A, Hristova M, Ho LT, Sprague SM. Impact of ergocalciferol treatment of vitamin D deficiency on serum parathyroid hormone concentrations in chronic kidney disease. Am J Nephrol. 2007;27:36–43. doi: 10.1159/000098561. [DOI] [PubMed] [Google Scholar]
- 29.Pesenson A, Maski M. Prevalence of 25-OH Vitamin D (25-OH) Deficiency in Patients (Pts) with Chronic Kidney Disease (CKD) and Effects of Correction Following KDOQI Guidelines [abstract] J Am Soc Nephrol. 2006 Suppl 1 [Google Scholar]
- 30.Shah TP, Fumo P. Effect of 25-OH Vitamin D Supplementation on Secondary Hyperparathyroidism in Patients with Early Chronic Kidney Disease. J Am Soc Nephrol. 2006 Suppl 1 [Google Scholar]
- 31.DeVille J, Thorp ML, Tobin L, Gray E, Johnson ES, Smith DH. Effect of ergocalciferol supplementation on serum parathyroid hormone and serum 25-hydroxyvitamin D in chronic kidney disease. Nephrology (Carlton) (11) 2006;2006:555–559. doi: 10.1111/j.1440-1797.2006.00698.x. [DOI] [PubMed] [Google Scholar]
- 32.Shah N, Bernardini J, Piraino B. Prevalence and correction of 25(OH) vitamin D deficiency in peritoneal dialysis patients. Perit Dial Int. 2005;25:343–347. [PubMed] [Google Scholar]
- 33.Houghton LA, Vieth R. The case against ergocalciferol (vitamin D2) as a vitamin supplement. Am J Clin Nutr. 2006;84:694–697. doi: 10.1093/ajcn/84.4.694. [DOI] [PubMed] [Google Scholar]
- 34.Slatopolsky E, Weerts C, Thielan J, Horst R, Harter H, Martin KJ. Marked suppression of secondary hyperparathyroidism by intravenous administration of 1,25-dihydroxy-cholecalciferol in uremic patients. J Clin Invest. 1984;74:2136–2143. doi: 10.1172/JCI111639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ritter CS, Armbrecht HJ, Slatopolsky E, Brown AJ. 25-Hydroxyvitamin D(3) suppresses PTH synthesis and secretion by bovine parathyroid cells. Kidney Int. 2006;70:654–659. doi: 10.1038/sj.ki.5000394. [erratum in Kidney Int. 2006;70:1190] [DOI] [PubMed] [Google Scholar]
- 36.Segersten U, Correa P, Hewison M, et al. 25-hydroxyvitamin D(3)-1alpha-hydroxylase expression in normal and pathological parathyroid glands. J Clin Endocrinol Metab. 2002;87:2967–2972. doi: 10.1210/jcem.87.6.8604. [DOI] [PubMed] [Google Scholar]
- 37.Schwartz GG, Whitlatch LW, Chen TC, Lokeshwar BL, Holick MF. Human prostate cells synthesize 1,25-dihydroxyvitamin D3 from 25-hydroxyvitamin D3. Cancer Epidemiol Biomarkers Prev. 1998;7:391–395. [PubMed] [Google Scholar]
- 38.Tangpricha V, Flanagan JN, Whitlatch LW, et al. 25-hydroxyvitamin D-1alpha-hydroxylase in normal and malignant colon tissue. Lancet. 2001;357:1673–1674. doi: 10.1016/S0140-6736(00)04831-5. [DOI] [PubMed] [Google Scholar]
- 39.Nanes MS. Vitamin D metabolism in pregnant and pseudopregnant rats: identification of 25-hydroxycholecalciferol- 1-hydroxylase in decidual tissue. Calcif Tissue Int. 1988;42:369–374. doi: 10.1007/BF02556355. [DOI] [PubMed] [Google Scholar]
- 40.Bell NH. Renal and nonrenal 25-hydroxyvitamin D-1alphahydroxylases and their clinical significance. J Bone Miner Res. 1998;13:350–353. doi: 10.1359/jbmr.1998.13.3.350. [DOI] [PubMed] [Google Scholar]
- 41.Garland CF, Garland FC, Gorham ED, et al. The role of vitamin D in cancer prevention. Am J Public Health. 2006;96:252–261. doi: 10.2105/AJPH.2004.045260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Drüeke TB. Cell biology of parathyroid gland hyper-plasia in chronic renal failure. J Am Soc Nephrol. 2000;11:1141–1152. doi: 10.1681/ASN.V1161141. [DOI] [PubMed] [Google Scholar]
- 43.Portale AA, Halloran BP, Morris RC., Jr Physiologic regulation of the serum concentration of 1,25-dihydroxyvitamin D by phosphorus in normal men. J Clin Invest. 1989;83:1494–1499. doi: 10.1172/JCI114043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nykjaer A, Dragun D, Walther D, et al. An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3. Cell. 1999;96:507–515. doi: 10.1016/s0092-8674(00)80655-8. [DOI] [PubMed] [Google Scholar]
- 45.Chesney RW, Rosen JF, Hamstra AJ, Smith C, Mahaffey K, DeLuca HF. Absence of seasonal variation in serum concentrations of 1,25-dihydroxyvitamin D despite a rise in 25-hydroxyvitamin D in summer. J Clin Endocrinol Metab. 1981;53:139–142. doi: 10.1210/jcem-53-1-139. [DOI] [PubMed] [Google Scholar]
- 46.Halloran BP, Schaefer P, Lifschitz M, Levens M, Goldsmith RS. Plasma vitamin D metabolite concentrations in chronic renal failure: effect of oral administration of 25-hydroxyvitamin D3. J Clin Endocrinol Metab. 1984;59:1063–1069. doi: 10.1210/jcem-59-6-1063. [DOI] [PubMed] [Google Scholar]
- 47.Raggi P, Boulay A, Chasan-Taber S, et al. Cardiac calcification in adult hemodialysis patients: A link between endstage renal disease and cardiovascular disease? J Am Coll Cardiol. 2002;39:695–701. doi: 10.1016/s0735-1097(01)01781-8. [DOI] [PubMed] [Google Scholar]
- 48.Goodman WG, Goldin J, Kuizon BD, et al. Coronaryartery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000;342:1478–1483. doi: 10.1056/NEJM200005183422003. [DOI] [PubMed] [Google Scholar]
- 49.Atsumi K, Kushida K, Yamazaki K, Shimizu S, Ohmura A, Inoue T. Risk factors for vertebral fractures in renal osteodystrophy. Am J Kidney Dis. 1999;33:287–293. doi: 10.1016/s0272-6386(99)70302-1. [DOI] [PubMed] [Google Scholar]
- 50.Lindberg JS, Moe SM, Goodman WG, et al. The calcimimetic AMG 073 reduces parathyroid hormone and calcium x phosphorus in secondary hyperparathyroidism. Kidney Int. 2003;63:248–254. doi: 10.1046/j.1523-1755.2003.00720.x. [DOI] [PubMed] [Google Scholar]