Abstract
Background
CT Colonography (CTC) is a non-invasive option for colorectal cancer (CRC) screening. The accuracy of CTC as a screening tool among asymptomatic adults has not been well defined.
Methods
The National CT Colonography Trial recruited 2600 asymptomatic participants, age ≥ 50 years, at 15 study centers. CTC images were acquired using standard bowel preparation, stool/fluid tagging, mechanical insufflation, ≥16 row CT scanners. Trained CTC radiologists reported all lesions ≥ 5 mm in diameter. Colonoscopy was performed according to established clinical protocols at each center and served as the reference standard. Detection by CTC of patients with large (≥10 mm), histologically-confirmed adenomas and adenocarcinomas which were detected by colonoscopy was the primary endpoint; detection of smaller (6–9 mm) colorectal lesions was also evaluated.
Results
Complete data were available for 2531 (97%) participants. For large adenomas and cancers the per patient estimates for sensitivity, specificity, positive and negative predictive values and area under the receiver operating characteristic curve were 0.90 ±0.03, 0.86 ± 0.02, 0.23 ± 0.02, 0.99 ±<0.01 and 0.89 ± 0.02, respectively. The sensitivity of 90% indicates that CTC failed to detect a lesion ≥10mm in 10% of patients. Per-polyp sensitivity for large adenomas or cancers was 0.84 ± 0.04. Per-patient sensitivity estimates in detecting patients with adenomas ≥ 6 mm, was 0.78.
Conclusions
In this study of asymptomatic adults, CTC screening identified 90% of patients with adenomas and cancers ≥ 10 mm in diameter. These findings augment published data regarding the role of CTC in average-risk CRC screening.
Introduction
Colorectal cancer (CRC) is the third most common cancer and second leading cause of cancer death in the United States with an estimated 153,760 new CRC cases and 52,180 CRC deaths in 2007.(1) There is an enormous opportunity to save lives with broadly applied, widely accepted early detection programs as the natural history of CRC permits the recognition and curative treatment of both precursor adenomas and localized cancers. Data from multiple sources support reduced CRC mortality through regular screening.(1–3) Despite its effectiveness, CRC screening remains underutilized for many reasons, including limitations in the performance, comfort, availability and expense of currently endorsed test options.
Computerized tomographic colonography (CTC) employs advanced visualization technology that permits a minimally invasive, structural evaluation of the entire colorectum. CTC has several potential advantages over other CRC screening tests, including rapid imaging of the entire colorectum, relatively non-invasive technique without the need for sedation and low risk for procedure-related complications.(4, 5)
CTC performance characteristics for screen-detecting asymptomatic colorectal lesions remain controversial, perhaps in part due to the heterogeneous subject populations, imaging protocols and reader qualifications included in prior studies. To further evaluate CTC as a primary CRC screening tool, the American College of Radiology Imaging Network (ACRIN) National CT Colonography Trial was designed to assess the accuracy of CTC for detecting participants with large (≥ 10 mm in diameter) histologically-confirmed, colorectal neoplasms (adenomas and cancers), using optical colonoscopy (the current clinical standard for CRC screening) as the reference standard.
Methods
A total of 15 clinical sites participated in this HIPAA-compliant study, and approval was obtained from the Institutional Review Board at each site prior to activation. Subjects were recruited from among all asymptomatic patients 50 years or older, prescheduled for routine colonoscopy at the participating sites between February 2005 and December 2006. Exclusion criteria were melena and/or hematochezia on more than one occasion in the previous six months, lower abdominal pain, inflammatory bowel disease and/or familial polyposis syndrome, serious medical conditions associated with excessive colonoscopy risk, colonoscopy within the previous five years, anemia (hemoglobin less than 10 gm/dl), or positive fecal occult blood test (FOBT). Each enrolled study participant provided written informed consent.
Radiologist Training
Each participating radiologist was required to submit confirmation of having (a) interpreted at least 500 CTC examinations or (b) having participated in a specialized 1.5 day CTC training session. In addition, all participating radiologists were required to complete a pre-study qualifying examination with ≥ 90% detection of ≥ 10 mm polyps in a reference image set. Of 20 radiologists who met the initial entry criteria, 15 with the highest qualifying examination scores were subsequently invited to participate. Details regarding the credentialing process have been reported in abstract form.(6)
CT Colonography
The preparation included stool tagging, laxative purgation and fluid tagging (Appendix 1). Colonic insufflation was obtained with an automated CO2 insufflator (PROTOC02L, E-Z-EM, Inc., Lake Success, NY). Room air with manual insufflation was utilized if adequate colon distention could not be obtained using the mechanical insufflator. One milligram of subcutaneous glucagon was administered 7–15 minutes prior to the examination unless contraindicated or refused by the study participant.
Supine and prone data acquisitions were obtained. All examinations were performed using at least a 16 slice CT scanner. Images were acquired using 0.5–1.0 mm collimation, pitch of 0.98–1.5, matrix 512 × 512, field-of-view to fit, 50 effective mAs, 120 kVp, and standard reconstruction algorithm. Images for prone and supine acquisitions were reconstructed to slice thicknesses of 1–1.25 mm with a 0.8 mm reconstruction interval.(7)
The studies were randomly assigned to be read independently using either a primary 2D search method (conventional 2D image display with 3D endoluminal problem solving), or a primary 3D search method (including the capability of displaying multiplanar 2D). Lesion location, size, and observer confidence were noted for each abnormality, with CTC size determination based on 2D images using the greatest diameter. Observer confidence that each finding was a polyp was rated on a scale of 0 (not a lesion) to 5 (high confidence). Interpretations were performed without prior knowledge of the colonoscopy results. Radiologists were instructed to only record findings ≥ 5 mm.
Colonoscopy
Following the CTC examination, index colonoscopy was performed according to standard clinical protocol at each participating site. Same day CTC and colonoscopy examinations were performed for 2512/2531 (99%) of participants. Identified lesions were photographed during the withdrawal phase. Withdrawal time was not included as these data were not routinely available from colonoscopy reports. All index colonoscopy examinations were performed or directly supervised by an experienced endoscopist (staff gastroenterologist or surgeon) without prior knowledge of the CTC results. Participants with CTC-detected lesions ≥ 10 mm that were not identified during the index colonoscopy were advised to undergo repeat colonoscopy within 90 days; endoscopists were provided with the CTC results prior to repeat colonoscopy.
Histology Review and Lesion Matching
Tissue samples from all lesions ≥ 5 mm were centrally reviewed by an experienced gastrointestinal pathologist (LJB) and these data were used for all histology-related analyses. Adenomas were defined as having cytologic dysplasia involving the epithelium at the luminal surface of polyp, and extending to any crypt depth or meeting the criteria of aberrant proliferation defined as "sessile serrated adenoma" by Torlakovic et al.(8, 9) Hyperplastic polyps were defined as having a serrated architecture, no superficial epithelial hyperchromasia and lacking the full thickness mucosal proliferative changes defined as sessile serrated adenoma.
In accordance with prior studies,(10, 11) lesion size was determined from the pathology report, unless the lesion was resected piecemeal, fulgurated or not removed; for these lesions, colonoscopy-derived size estimates were employed. Lesion matching between CTC and colonoscopy examinations was performed by two experienced central radiologists (CDJ, JPH), who were not involved with initial lesion detection, based on an established algorithm that incorporated lesion location (within one colonic segment) and size (+/−50%).(10, 12, 13) Lesion match status was also evaluated electronically using the same algorithm. Discrepancies in lesion matching status were adjudicated by consensus opinion of the central radiologists. If consensus opinion could not be reached, the case was reviewed by an experienced gastroenterologist (PJL) for final determination of match status.
Statistical Analysis
Colonoscopy (and repeat colonoscopy, when performed) and pathology results were the reference standard for determining lesion size, location, and histology. A positive CTC result was defined as any findings ≥ 5 mm identified on CTC exam. For a participant with positive CTC result, if there were one or more appropriately-sized (i.e. ≥ 10 mm, ≥ 6 mm, etc.) lesions also identified on the reference standard, the CTC result was considered as true positive (TP) at that size level. Participants with a positive CTC result, if there was no appropriately-sized lesions found on the reference standard, the CTC result was considered false positive at that size level. The utility of CTC as screening tool was assessed by per-patient accuracy. To reflect community practice, we present results averaged across radiologists. (10, 13, 14) (15) Therefore per-patient sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were first estimated for each radiologist and then averaged across radiologists.(16) Sensitivity was computed as the percent of patients with lesions greater or equal to the pre-specified threshold seen on colonoscopy that were detected by CTC for each radiologist. 1-sensitivity is equal to the false negative rate for CTC and estimates the percentage of patients with lesions detected by optical colonoscopy that were missed by CTC for each radiologist. Specificity was computed as the percent of participants with no lesions larger than pre-specified threshold seen on colonoscopy that were also considered negative by CTC for each radiologist. 1-specificity is equal to the false positive rate for CTC and estimates the percentage of negative participants by optical colonoscopy that were considered positive by CTC for each radiologist. PPV was computed as the percent of participants with CTC findings that were seen on colonoscopy, while NPV was computed as the percent of participants with no CTC findings larger than pre-specified threshold that were considered negative. Exact 95% confidence intervals (CIs) were computed for each radiologist, and large sample 95% CIs were constructed for overall estimates using standard errors (SEs) that allowed for variation across radiologists. The sample size was computed to provide a sufficient number of patients with at least one histologically confirmed adenoma or cancer ≥ 10 mm found on colonoscopy to ensure that, for anticipated values of sensitivity, the SE of the average sensitivity across radiologists was less than 0.05 when that SE allowed for anticipated variation in sensitivity across radiologists. Receiver operating characteristic (ROC) curves were estimated based on data pooled across radiologists, due to the small number of positive cases reviewed by each participating radiologist. Similar analyses were also performed for per-polyp sensitivities, and for detection of participants with any abnormal lesions ≥ 10 mm, i.e., not limited to neoplasm. Per-polyp sensitivity was computed as the percent of lesions greater or equal to the pre-specified threshold that were detected by colonoscopy and matched to the CTC findings using the previously described algorithm.
Estimates of sensitivity, specificity, NPV, and PPV were obtained for participants at increased risk for colorectal cancer due to familial or personal history, and for participants at average risk. In addition, sensitivities were calculated for 2D and 3D search methods, for different types of bowel preparation, and different overall quality of preparation. Because of the small number of positive cases each radiologist reviewed in the above subset analyses, only pooled estimates for sensitivity were calculated, and uncertainty in estimates was quantified using exact 95% CIs.
Results
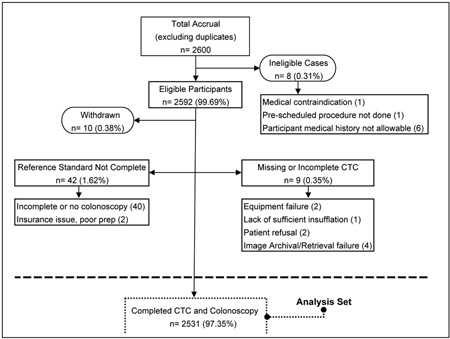
The total number of participants enrolled was 2600 (2617 registrations, 17 duplicates). Complete CTC and colonoscopy results were available for 2531 (97%) participants, which constituted the study set (Appendix 2). Demographic data are provided in Table 1. The majority of subjects (89%) had no known CRC risk factors other than age. Two hundred thirty-five (9%) subjects had a first degree relative with a history of colorectal polyps or cancer, 34 (1%) had a personal history of polyps or cancer, and 13 (1%) had both. All others were considered to be of average risk for CRC screening. Baseline demographics were similar between the final analytic cohort and all eligible participants.
Table 1.
Demographic characteristics of participants, overall and by size of reported colorectal neoplasia
| No Cancer / Adenomas ≥ 5 mm N = 2249 | Cancer / Adenomas ≥ 5 mm and < 10 mm N = 173 | Cancer / Adenomas ≥ 10 mm N = 109 | NCTCT Overall N = 2531 | |
|---|---|---|---|---|
| Age at Enrollment - yr | ||||
| Mean | 58.0 | 59.6 | 60.8 | 58.3 |
| Interquartile range | 52 – 62 | 53 – 65 | 54 – 66 | 52 – 62 |
| Gender – no. (%) | ||||
| Male | 1036 (46.1) | 108 (62.4) | 61 (56.0) | 1205 (47.6) |
| Female | 1213 (53.9) | 65 (37.6) | 48 (44.0) | 1326 (52.4) |
| Race – no. (%)** | ||||
| American Indian or Alaskan Native | 18 (0.8) | 2 (1.2) | 3 (2.8) | 23 (0.9) |
| Asian | 55 (2.5) | 4 (2.3) | - - | 59 (2.3) |
| Black or African American | 295 (13.1) | 24 (13.9) | 14 (12.8) | 333 (13.2) |
| Native Hawaiian or other Pacific Islander | 7 (0.3) | - - | - - | 7 (0.3) |
| White | 1856 (82.5) | 142 (82.1) | 93 (85.3) | 2091 (82.6) |
| Unknown/Missing | 42 (1.9) | 2 1.2) | 2 (1.8) | 46 (1.8) |
| Ethnicity – no. (%) | ||||
| Not Hispanic or Latino | 2156 (95.9) | 170 (98.3) | 104 (95.4) | 2430 (96.0) |
| Hispanic or Latino | 89 (4.0) | 3 (1.7) | 5 (4.6) | 97 (3.8) |
| Unknown | 4 (0.2) | - - | - - | 4 (0.2) |
| Medical History – no. (%) | ||||
| Family history of colon cancer | 213 (9.5) | 12 (6.9) | 10 (9.2) | 235 (9.3) |
| Personal history of polyps or cancer | 30 (1.3) | 1 (0.6) | 3 (2.8) | 34 (1.3) |
| Both family and personal history | 13 (0.6) | - - | - - | 13 (0.5) |
Multiple races may be endorsed by a single participant, such that the total over all options may sum to greater than 100%.
Per-patient Assessment
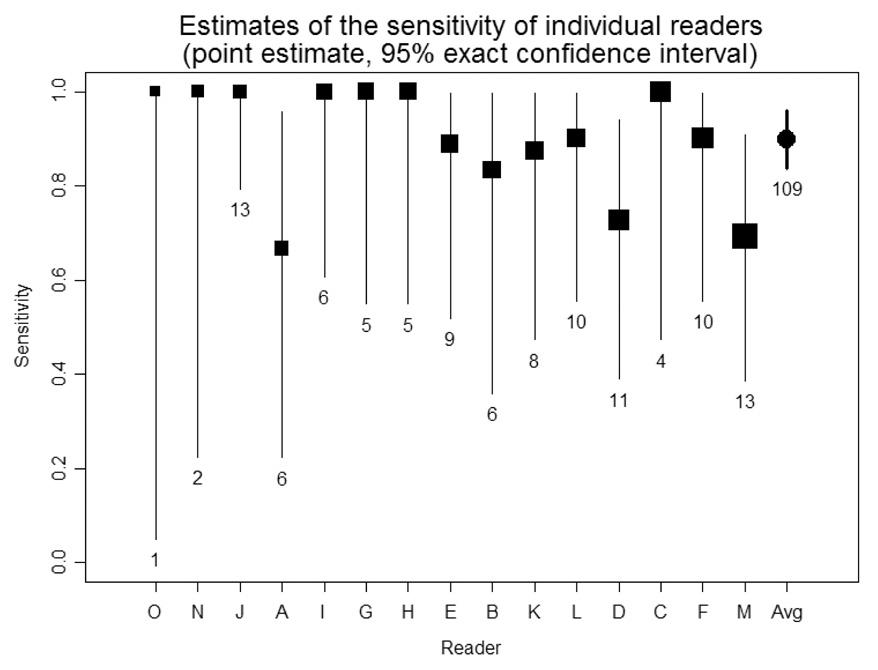
The overall diagnostic performance of CTC for screen-detecting patients with at least one lesion (adenoma or cancer) ≥ 5 mm is shown in Table 2. Sensitivity, specificity, PPV, NPV and area under the ROC curve (AUC) for large lesions ≥ 10 mm were 0.90 (SE = 0.031), 0.86 (0.022), 0.23 (0.020), 0.99 (0.002) and 0.89 (0.020), respectively. Our estimate of sensitivity of 90% for detection patients with large lesions was based on the following computation: of the 1 to 13 patients seen by each radiologist with one or more large lesions detected by optical colonoscopy, CTC detected patients with large lesions 90% on average; this indicates that for 10% of patients with one or more large lesions detected by colonoscopy, CTC did not detect a large lesion. Sensitivity for the detection of adenoma or cancers ≥ 5 mm, ≥ 6 mm, ≥ 7 mm, ≥ 8 mm and ≥ 9 mm was 0.65, 0.78, 0.84, 0.87, and 0.90, respectively, with specificity ranging from 0.86–.0.89. Sensitivity, specificity, PPV, and NPV were similar for participants at increased risk and those at average risk for colorectal cancer. Figure 1 plots the estimates of the sensitivity for individual readers. Sensitivity varied from 67% – 100% with 7 of 15 (47%) radiologists discovering all of the patients with large lesions. For the detection of patients with lesions ≥ 10 mm regardless of histology, the estimate (S.E.) of sensitivity, specificity, PPV, NPV and AUC were 0.87 ± 0.035, 0.86 ± 0.022, 0.28 ± 0.026, 0.99 ± 0.002 and 0.88 ± 0.019.
Table 2.
Per-patient accuracy in detecting patients with adenomas or cancers at CTC
| Size of adenomas or cancers detected on optical colonoscopy | ||||||
|---|---|---|---|---|---|---|
| ≥ 5 mm | ≥ 6 mm | ≥ 7 mm | ≥ 8 mm | ≥ 9 mm | ≥ 10 mm | |
| Est. | Est. | Est. | Est. | Est. | Est. | |
| (N) | (N) | (N) | (N) | (N) | (N) | |
| (LCB, UCB) | (LCB, UCB) | (LCB, UCB) | (LCB, UCB) | (LCB, UCB) | (LCB, UCB) | |
| Sens | 0.65 | 0.78 | 0.84 | 0.87 | 0.90 | 0.90 |
| (282) | (210) | (174) | (154) | (120) | (109) | |
| (0.579 , 0.727) | (0.711 , 0.849) | (0.776 , 0.912) | (0.803 , 0.929) | (0.832 , 0.960) | (0.838 , 0.960) | |
| Spec | 0.89 | 0.88 | 0.87 | 0.87 | 0.86 | 0.86 |
| (2249) | (2321) | (2357) | (2377) | (2411) | (2422) | |
| (0.851 , 0.923) | (0.840 , 0.920) | (0.831 , 0.914) | (0.825 , 0.909) | (0.817 , 0.902) | (0.813 , 0.900) | |
| PPV | 0.45 | 0.40 | 0.35 | 0.31 | 0.25 | 0.23 |
| (423) | (423) | (423) | (423) | (423) | (423) | |
| (0.389 , 0.513) | (0.335 , 0.463) | (0.299 , 0.397) | (0.256 , 0.355) | (0.209 , 0.292) | (0.194 , 0.273) | |
| NPV | 0.95 | 0.98 | 0.99 | 0.99 | 0.99 | 0.99 |
| (2108) | (2108) | (2108) | (2108) | (2108) | (2108) | |
| (0.941 , 0.965) | (0.971 , 0.984) | (0.980 , 0.992) | (0.984 , 0.994) | (0.990 , 0.998) | (0.991 , 0.998) | |
| Area under ROC | 0.80 | 0.84 | 0.87 | 0.88 | 0.89 | 0.89 |
| (2531) | (2531) | (2531) | (2531) | (2531) | (2531) | |
| (0.763 , 0.828) | (0.810 , 0.878) | (0.833 , 0.902) | (0.842 , 0.913) | (0.853 , 0.930) | (0.854 , 0.933) | |
LCB (UCB): Lower (Upper) 95% Confidence Bound Sens=sensitivity, Spec=specificity, PPV=positive predictive value, NPV=negative predictive value, Area under ROC=area under receiver operating characteristic curve.
Sensitivity indicates the percent of patients who had a lesions (of the specified size) detected by optical colonoscopy, which were detected by CTC averaged across radiologists. Specificity indicates the percent of participants who had no lesions detected on optical colonoscopy, who had no lesions detected on CTC average across radiologists. Positive predictive value indicates the percent of participants with CTC findings (of the specified size) which were detected by optical colonoscopy average across radiologists. Negative predictive value indicates the percent of participants who had no lesions with specified size detected by CTC, who had no lesions detected on optical colonoscopy average across radiologists. Receiver operating characteristic curve plots the sensitivity against the false positive rate, and the area under ROC represents the accuracy of the CTC.
Figure 1. Estimates of the sensitivity of individual readers for detecting patients with adenomas or cancers 10mm or larger based on identifying CTC findings 5 mm or larger.
Readers are ordered by total number of cases read (squares are proportional to the square root of same). The count of positive cases (at least one anenoma or cancer ≥ 10 mm) is printed below each confidence interval.
The distribution, histology, and sizes of the lesions found at colonoscopy are listed in Table 3. There were 128 large lesions in 109 (4.3%) patients. Seven adenocarcinomas in seven patients were all ≥ 10 mm. Non-adenomatous lesions ≥ 5 mm included 136 (25%) hyperplastic polyps, 7 (1%) lipomas and 30 (5%) with other histologies.
Table 3.
Distribution of colonoscopy detected lesions according to location, histology, and size.
| Lesions detected on optical colonoscopy** | ||||
|---|---|---|---|---|
| 5–9 mm | ≥ 10 mm | Total | ||
| Segment | Histology* | |||
| Rectum | ||||
| Adenomas or Carcinoma | 25 | 25 | 50 | |
| Non-Adenomas | 33 | 7 | 40 | |
| Sigmoid | ||||
| Adenomas or Carcinoma | 62 | 32 | 94 | |
| Non-Adenomas | 49 | 4 | 53 | |
| Descending | ||||
| Adenomas or Carcinoma | 32 | 8 | 40 | |
| Non-Adenomas | 16 | 2 | 18 | |
| Transverse | ||||
| Adenomas or Carcinoma | 52 | 17 | 69 | |
| Non-Adenomas | 22 | 4 | 26 | |
| Ascending | ||||
| Adenomas or Carcinoma | 47 | 27 | 74 | |
| Non-Adenomas | 16 | 7 | 23 | |
| Cecum | ||||
| Adenomas or Carcinoma | 28 | 19 | 47 | |
| Non-Adenomas | 10 | 3 | 13 | |
| Total | ||||
| Adenomas or Carcinoma | 246 | 128 | 374 | |
| Non-Adenomas | 146 | 27 | 173 | |
A total of 7 lesions ≥ 5 mm were malignant (2 were 10 mm, 1 was 15 mm, 2 were 25 mm, 1 was 55 mm and 1 was 100 mm): 3 in the rectum and 1 in each of the sigmoid, descending, transverse, and cecum. All were ≥ 10 mm. One malignant lesion measuring 10 mm was not seen at CTC. Thirteen (9 were 10 mm, 1 was 11 mm, 2 were 16 mm and 1 was 25 mm) adenomas ≥ 10 mm were not seen at CTC.
A total of 1629 of the 2531 had no polyps of any size; 2141 had no polyps ≥ 5 mm. 512 of the 2531 had at least one polyp and the largest polyp was < 5 mm. Data in the table represents the 258 participants with polyps 5–9 mm and the 132 with polyps ≥ 10 mm. Mean size of polyps (at least 5 mm by study design was 8.9 mm (SD =7.2)). Size measurements from colonoscopy were used for 333 (61%) of 547 polyps, because the polyps were removed by pieces.
Per-polyp Assessment
The sensitivity of CTC for the detection of lesions with varying size is shown in Table 4 for the study overall. The overall sensitivity estimate for the detection for large lesions was 0.84 (SE = 0.043).
Table 4.
CTC detection rates for adenomas and cancers – per polyp analysis
| Size* of adenomas or cancers | ||||||
|---|---|---|---|---|---|---|
| ≥ 5 mm | ≥ 6 mm | ≥ 7 mm | ≥ 8 mm | ≥ 9 mm | ≥ 10 mm | |
| Est. | Est. | Est. | Est. | Est. | Est. | |
| (N) | (N) | (N) | (N) | (N) | (N) | |
| (SE) | (SE) | (SE) | (SE) | (SE) | (SE) | |
| Detection Rates | 0.59 | 0.70 | 0.75 | 0.80 | 0.82 | 0.84 |
| (374) | (270) | (220) | (187) | (143) | (128) | |
| (0.045) | (0.046) | (0.042) | (0.041) | (0.042) | (0.043) | |
Detection rates indicates the percent of lesions (of the specified size) detected by optical colonoscopy, which were matched through lesion matching algorithm by CTC average across radiologists. Lesion sizes were determined by the reference standard (either pathology measure or colonoscopy estimate).
Missed Lesion Assessment
The median size of the neoplasms (≥ 5 mm by study design) that were detected and those that were missed at CTC was 10 mm and 6 mm, respectively. There was not an association between missed detections and polyp location or morphology. A single 10 mm cancer in the low rectum was missed at CTC. This lesion was not visible in retrospect.
A total of 30 lesions ≥ 10 mm were detected in 27 participants by CTC, but were not detected at the initial colonoscopy. Fifteen of these 27 participants with 18 reported lesions returned for repeat colonoscopy per the protocol instructions. Five out of 18 lesions were confirmed on repeat colonoscopy (these were considered true positive CTC findings). These five lesions were 9 (inflammatory polyp), 10 (tubular adenoma), 11 (tubular adenoma), 14 (inflammatory polyp), and 35 mm in diameter (tubulovillous adenoma with dysplasia), polypoid and were located in five different segments. In the remaining patients confirmatory colonoscopy was not obtained. Three participants had findings that did not warrant recall (1 surgical hemicolectomy, 1 benign stricture, and 1 the CTC finding was discounted by a colonoscopist), three participants refused to return and in six patients the referring physician determined that recall was not warranted.
Colon preparation included Polyethylene Glycol solution in 1020 (40%), Phosphosoda in 1403 (55%), Magnesium Citrate in 102 (4%) and other in 6 (0.2%). Barium sulfate for fecal tagging and iodinated contrast material for fluid tagging were taken as directed by 2482 (98%) and 2390 (94%) of the participants, respectively. Glucagon was administered in 2328 (92%) participants. Glucagon was not given for: brittle diabetes (78), borderline glucose level (1), pheochromocytoma (2), patient request (69), drug unavailable (47), and physician not available during administration (6).
Imaging
CTC examinations were performed on 16, 40 and 64 slice scanners in 1140 (45%), 83 (3%) and 1308 (52%) cases, respectively. 1280 interpretations were performed using primary 2D interpretation with 3D problem solving, and 1251 using primary 3D endoluminal fly through with 2D problem solving, respectively. CTC software for radiologist interpretation included Vital Images, General Electric, Siemens, Viatronix and TeraRecon.
The pooled sensitivity for detecting participants with large lesions using primary 2D conventional and primary 3D endoluminal fly-through viewing software were similar: 0.87 (95% CI: 0.75 – 0.95) and 0.88 (95% CI: 0.76 – 0.95), respectively. The difference between the two types of viewing software was not significant. Mean time for the primary 2D versus primary 3D interpretation was 19.4 minutes vs. 25.3 minutes. There was no correlation between the number of cases interpreted and reader performance (Figure 1).
Adverse Events
Adverse events (considered grade 3 or higher) were reported in three participants (severe nausea and vomiting for <24 hours after CTC; hematochezia following snare polypectomy requiring 2 day hospitalization, hospitalization for E Coli bacteremia 24 hours after both procedures)..
Extracolonic Findings
Extracolonic findings were observed in 66% of the participants; however, only 16% were deemed either to require additional evaluation or to be highly significant requiring urgent care. These findings were located in the chest (27%), gastrointestinal tract (18%), genitourinary tract (45%), vascular system (6%), and musculoskeletal system (3%).
Discussion
In our study CTC identified 90% of patients with large (≥10 mm), asymptomatic colorectal lesions (adenomas and cancers) that were detected by optical colonoscopy with an area under the ROC curve of 0.89. Secondary analyses demonstrated lower sensitivity for smaller (6–9 mm) colorectal lesions.
Our estimates of the sensitivity of CTC for detecting lesions found on colonoscopy are higher than estimates in some other studies.(10, 13, 14) The study by Pickhardt et al. reported results similar to ours.(12) Although the higher accuracy in Pickhardt’s study compared with other studies has been attributed by some to use of a primary 3D endoluminal reading technique, our study showed similar performance of both image display methods and software brands, with the primary 3D technique requiring nearly six additional minutes for interpretation compared with the primary 2D technique.
The main objective of this prospective trial was to evaluate the screening performance characteristics of CTC using optimized, yet reproducible, image acquisition and interpretation methods in a diverse, multi-center setting, and to compare these observations to screening colonoscopy, as the existing reference standard. To maximize the likelihood that the colonoscopy data were reflective of usual clinical practice, we intentionally avoided incorporating advanced endoscopist training (beyond usual credentialing requirements) and non-standard examination techniques (such as segmental unblinding) into our study design. Since adenoma miss rates of 2% and 13% for ≥ 10 mm and ≥ 5 mm polyps, respectively, have been reported from tandem colonoscopy studies,(17) the CTC performance characteristics reported from our trial may actually be underestimated. The specificity estimate for large lesions observed in our study was lower than other recent multi-institutional studies.(12–14) This may be due to the training sessions that emphasized polyp detection (maximizing sensitivity), and a potential weakness of the training process. This trial required all readers to be trained on at least 50 CTC cases prior to demonstrating the minimal level of competence. Most of the radiologists in our trial were required to obtain additional education beyond the initial 50 cases in order to recognize lesions that are difficult to detect.
Similar to other recent prospective CTC screening studies,(10, 12–14) we focused on lesions ≥ 5 mm in the present trial since the prevalence of advanced histologic features in diminutive (i.e., < 5 mm) polyps is reportedly below 2%.(18) Specificity estimates can be improved if the minimum size threshold for radiologic finding is increased. Based on the reference standard, the overall prevalence of large adenomas and cancers in this population was 4.3%. If all patients with a 5 mm or larger radiologic finding detected at CTC were to be referred for colonoscopy, the colonoscopy referral rate, based on our results, would be 16.7%. If a 6 mm threshold were used for CTC, the colonoscopy referral rate would decrease to 12.2%. By increasing the size threshold for radiologic finding to 6 mm, specificity increases to 91%, with little decrease in sensitivity (to 88%) for large adenomas.
Extracolonic abnormalities identified from this study are similar to those previously reported.(19–24) Further definition of inter-disciplinary management algorithms for these findings is needed to optimize the public health benefit from CTC screening.
Despite consensus opinion that CRC screening is effective,(2, 3) adherence with current guidelines remains low among screen-eligible adults.(25) CRC screening guidelines support multiple test options so that patients and providers can work together to determine their preferred examination modality. The less invasive nature of CTC and its low risk for procedure-related complications compared with colonoscopy may be attractive to patients and may improve CRC screening adherence rates by addressing currently unmet needs of some patients and/or providers.
In summary, this large, multi-center study of asymptomatic adults demonstrated that CTC screening identified 90% of patients with adenomas and cancers ≥10 mm in diameter. These findings support and extend previously published data regarding the role of CTC in average-risk CRC screening.
Acknowledgments
We are indebted to the many people at the headquarters of the American College of Radiology Imaging Network and at the recruiting sites for their important contributions to the study; to the radiologists, gastroenterologists, and research associates at the clinical sites; to Bruce Hillman, Mitchell Schnall, Steven King, Charles Apgar, Donna Hartfeil, Nancy Fredericks, Jamie Downs, Tina Taylor, Maria Oh, Rex Welsh, Tim Welsh, Fraser Wilton, Anthony Levering, James Gimpel, Cheryl Crozier, Mary Kelly Truran, Chris Steward, Josephine Schloesser, Sharlene Snowdon, Dave Vanness, Ronald Summers, Richard Farrell, David Rubin, Joel G. Fletcher, Debora Shreve, and the following members of the American College of Radiology Biostatistics Center: Constantine Gatsonis, Ilana Gareen, and Meridith Blevins.
Financial Disclosure
Doctors Johnson and Hara report patents and royalties from GE Healthcare. Doctor Dachman reports consulting fees/advisory board from ICAD and E-Z-EM, lecture fees from Philips, Inc., grant support from Philips, Inc, ICAD and American Cancer Society. Doctor Fidler reports grant support from E-Z-EM. Doctor Limburg reports consulting fees or paid advisory boards from Clinica del Sol, lecture fees from the American School of Oncology, and grant support from Olympus and Fujinon, Inc. Doctor Heiken reports consulting fees or paid advisory boards from Mallinckrodt, Inc., grant support from Bracco Diagnostics, GE Healthcare, patents and royalties from Mallinckrodt. Doctor Toledano reports grant support from Brown University. Doctor Yee reports lecture fees and grant support from GE Healthcare.
Grant support for this study provided by the National Cancer Institute (NCI) in cooperation with the American College of Radiology Imaging Network (ACRIN).
Appendix 1. CT Colonography Technique
Stool Tagging (24 hours prior to laxatives)
16 grams Barium sulfate (Tagitol V, Lake Success, NY) in three divided doses 4–6 hours apart
Bowel cleansing (ordered at the preference of the referring physician) Administered day prior to examination
Polyethylene glycol electrolyte lavage (generally 4 liters)
Or
Magnesium Citrate (generally 300 ml)
Or
Phosphosoda (45–90 ml)
Plus (added to any of the three regimens above)
Bisacodyl tablets (generally 10 mg)
Fluid Tagging (taken orally the evening prior to the examination)
60 ml water-soluble iodinated oral contrast material (diatrizoate meglumine and diatrizoate sodium, Gastroview, Mallinckrodt Imaging, ST. Louis, MO)
Glucagon (administered 7–15 minutes prior to CT acquisition unless contraindicated or refused by patient)
1 milligram subcutaneously.
Appendix 2. Patient accrual flowchart
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics 2008. CA Cancer J Clin. 2007;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Guide to Clinical Preventive Services, 2006. Recommendations of the U.S. Preventive Services Task Force. 2006 www.ahrq.gov/clinic/pocketgd/index.
- 3.Winawer S, Fletcher R, Rex D, et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale--update based on new evidence. Gastroenterol. 2003;124(2):544–560. doi: 10.1053/gast.2003.50044. [DOI] [PubMed] [Google Scholar]
- 4.Burling D, Halligan S, Slater A, Noakes MJ, Taylor SA. Potentially serious adverse events at CT colonography in symptomatic patients: national survey of the United Kingdom. Radiology. 2006;239(2):464–471. doi: 10.1148/radiol.2392051101. [DOI] [PubMed] [Google Scholar]
- 5.Pickhardt PJ. Incidence of colonic perforation at CT colonography: review of existing data and implications for screening of asymptomatic adults (review) Radiology. 2006;239(2):313–316. doi: 10.1148/radiol.2392052002. [DOI] [PubMed] [Google Scholar]
- 6.Fletcher JG, Johnson CD, Toledano A, et al. ACRIN 6664: Lessons for CT colonography (CTC) training and certification (abstract); Radiological Society of North America Scientific Assembly and Annual Meeting Program; 2005; Chicago, IL. 2005. [Google Scholar]
- 7. www.acrin.org/pdf_file2.html?file=protocol_docs/A6664partial_summary.pdf.
- 8.Li SC, Burgart L. Histopathology of serrated adenoma, its variants, and differentiation from conventional adenomatous and hyperplastic polyps. Arch Pathol Lab Med. 2007;131:440–445. doi: 10.5858/2007-131-440-HOSAIV. [DOI] [PubMed] [Google Scholar]
- 9.Torlakovic EE, Gomez JD, Driman DK, et al. Sessile serrated adenoma (SSA) vs. traditional serrated adenoma (TSA) Am J Surg Pathol. 2008;32:21–29. doi: 10.1097/PAS.0b013e318157f002. [DOI] [PubMed] [Google Scholar]
- 10.Johnson CD, Harmsen WS, Wilson LA, et al. Prospective blinded evaluation of computed tomographic colonography for screen detection of colorectal polyps. Gastroenterology. 2003;125(2):311–319. doi: 10.1016/s0016-5085(03)00894-1. [DOI] [PubMed] [Google Scholar]
- 11.Johnson CD, MacCarty RL, Welch TJ, et al. Comparison of the relative sensitivity of CT colonography and double-contrast barium enema for screen detection of colorectal polyps. Clin Gastroenterology and Hepatology. 2004;2:314–321. doi: 10.1016/s1542-3565(04)00061-8. [DOI] [PubMed] [Google Scholar]
- 12.Pickhardt PJ, Choi JR, Hwang I, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003;349(23):2191–2200. doi: 10.1056/NEJMoa031618. [DOI] [PubMed] [Google Scholar]
- 13.Rockey DC, Paulson E, Niedzwiecki D, et al. Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet. 2005;365(9456):305–311. doi: 10.1016/S0140-6736(05)17784-8. [DOI] [PubMed] [Google Scholar]
- 14.Cotton DB, Durkalski VL, Pineau BC, et al. Computed tomographic colonography (virtual colonoscopy): a multicenter comparison with standard colonoscopy for detection of colorectal neoplasia. JAMA. 2004;291(14):1713–1719. doi: 10.1001/jama.291.14.1713. [DOI] [PubMed] [Google Scholar]
- 15.Obuchowski NA, Zepp RC. Simple steps for improving multiple-reader studies in radiology. AJR Am J Roentgenol. 1996;166(3):517–521. doi: 10.2214/ajr.166.3.8623619. [DOI] [PubMed] [Google Scholar]
- 16.Ahn C. Statistical methods for the estimation of sensitivity and specificity of site-specific diagnostic tests. J Periodont Res. 1997;32(4):351–354. doi: 10.1111/j.1600-0765.1997.tb00544.x. [DOI] [PubMed] [Google Scholar]
- 17.van Rijn JC, Reitsma JB, Stocker J, Bossuyt PM, van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol. 2006;101(2):343–350. doi: 10.1111/j.1572-0241.2006.00390.x. [DOI] [PubMed] [Google Scholar]
- 18.Butterly LF, Chase MP, Pohl H, Fiarman GS. Prevalence of clinically important histology in small adenomas. Clin Gastroenterol Hepatol. 2006;4(3):343–348. doi: 10.1016/j.cgh.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 19.Gluecker T, Johnson CD, Wilson LA, et al. Extracolonic findings at CT colonography: evaluation of prevalence and cost in a screening population. Gastroenterology. 2003;124:911–916. doi: 10.1053/gast.2003.50158. [DOI] [PubMed] [Google Scholar]
- 20.Hara A, Johnson CD, MacCarty RL, Welch TJ. Incidental extracolonic findings at CT colonography. Radiology. 2000;215:353–357. doi: 10.1148/radiology.215.2.r00ap33353. [DOI] [PubMed] [Google Scholar]
- 21.Hellstrom M, Svensson MH, Lasson A. Extracolonic and incidental findings on CT colonography (virtual colonoscopy) AJR Am J Roentgenol. 2004;182:631–638. doi: 10.2214/ajr.182.3.1820631. [DOI] [PubMed] [Google Scholar]
- 22.Rajapaksa RC, Macari M, Bini EJ. Prevalence and impact of extracolonic findings in patients undergoing CT colonography. J Clin Gastroenterol. 2004;38:767–771. doi: 10.1097/01.mcg.0000139035.38568.18. [DOI] [PubMed] [Google Scholar]
- 23.Xiong T, Richardson M, Woodroffe R, Halligan S, Morton D, Lilford RJ. Incidental lesions found on CT colonography: their nature and frequency. Br J Radiol. 2005;78:22–29. doi: 10.1259/bjr/67998962. [DOI] [PubMed] [Google Scholar]
- 24.Yee J, Kumar NN, Godara S, et al. Extracolonic abnormalities discovered incidentally at CT colonography in a male population. Radiology. 2005;236:519–526. doi: 10.1148/radiol.2362040166. [DOI] [PubMed] [Google Scholar]
- 25.Smith RA, Cokkinides V, Eyre HJ. Cancer screening in the United States, 2007: a review of current guidelines, practices and prospects. CA Cancer J Clin. 2007;57:90–104. doi: 10.3322/canjclin.57.2.90. [DOI] [PubMed] [Google Scholar]