Abstract
The authors examined the longitudinal association between persisting posttraumatic stress disorder (PTSD) symptoms and multiple domains of life functioning in a community sample of 1,377 American Legionnaire Vietnam veterans first assessed in 1984 and followed-up 14 years later. Almost 30 years after their return from Vietnam, 10% of veterans continued to experience severe PTSD symptoms. At all levels of combat exposure, persisting severe PTSD symptoms were associated with worse family relationships, more smoking, less life satisfaction and happiness, more mental health service use, and more nonspecific health complaints at the 14-year follow-up. Further investigation is needed to determine whether the PTSD-functioning relationship is causal and if successful treatment of PTSD is associated with improvement in functioning.
During the period 1964−1975, approximately 8 million people served in the United States Armed Forces. Estimates of the numbers who served in the Vietnam theater (i.e., in the Republic of Vietnam, its surrounding waters or airspace) range from 3 (32%) to 4.4. (48%) million (Cohany, 1992; Fischer, Boyler, Bucuvalas, & Schulman, 1980). About 56,000 soldiers died as direct casualties of the Vietnam conflict; at least 300,000 were physically wounded. Nearly two decades ago the National Vietnam Veterans Readjustment Study (NVVRS; Kulka et al., 1990) reported a lifetime posttraumatic stress disorder (PTSD) prevalence of 30.9% among male veterans who served in the Vietnam theater during 1964−1975. Posttraumatic stress disorder had become a chronic condition for about half of these veterans: The prevalence of current PTSD was 15.2% when they were assessed in the mid-to-late 1980s. The NVVRS and subsequent studies of Vietnam veterans have documented the adverse effects of persistent PTSD on multiple domains of life functioning. Specifically, PTSD has been strongly associated with increased utilization of medical treatment services (Schnurr, Friedman, Sengupta, Jankowski, & Holmes, 2000), marital and parenting difficulties (Caselli & Motta, 1995; Jordan et al., 1992; Ruscio, Weathers, King, & King, 2002; Samper, Taft, King, & King, 2004; Taft et al., 2005), smoking and substance use disorders (Beckham, 1999; Eisen et al., 2004; Koenen et al., 2006), and mortality from multiple causes (Boscarino, 2004, 2006). Chronic PTSD in Vietnam veterans has also been associated with decreased well-being, compromised health and quality of life, and poor psychosocial adjustment (Ferrada-Noli, Asberg, Ormstad, Lundin, & Sundbom, 1998; McFarlane, Atchison, Rafalowicz, & Papay, 1994; Taft, Stern, King, & King, 1999). However, the majority of the above-cited studies are cross-sectional; the effect of persisting PTSD on functioning in Vietnam veterans has rarely been examined longitudinally in a community sample. Moreover, most studies have focused on the association between PTSD and one specific domain of functioning, such as relationship quality or smoking, rather than comprehensively examining the PTSD-functioning association across multiple domains.
To address this absence of time course data on PTSD symptoms and Vietnam veteran well-being, we conducted a 14-year follow-up study of a random sample of American Legionnaires who had served in Southeast Asia (SEA) during the Vietnam War and whom we surveyed in 1984 and again in 1998. The results of our 1984 survey documented a cross-sectional association between higher combat exposure and worse functioning in this sample (Snow, Stellman, Stellman, & Sommer, 1988; Stellman, Stellman, & Sommer, 1988a-1988d). We also documented a dose-response relation between combat exposure and current severe PTSD symptoms in the 1984 survey (Snow et al., 1988). Using the follow-up data in 1998, we have reported on the risk factors for the course of severe PTSD symptoms in a subsample (Koenen, Stellman, Stellman, & Sommer, 2003).
In this study, we first examine whether the association between higher combat exposure and worse functioning documented in 1984 is still evident in 1998. We then test whether persisting PTSD symptoms are associated with deficits in four important areas of current functioning: family relationships, negative health behaviors, personal well-being, and nonspecific health problems, after stratifying by combat exposure.
METHOD
Participants
The cohort was originally surveyed in 1984 for a study of the health and well-being of American Legion members (Snow et al., 1988; Stellman et al., 1988a-1988d). It was composed by randomly sampling all male members of the American Legion who, in October, 1983, belonged to any American Legion post in Colorado, Indiana, Maryland, Minnesota, Ohio, or Pennsylvania, and had served in the U.S. Armed Forces during the official Vietnam War period: January, 1961 through May, 1975. The American Legion is the largest veterans’ organization in the country with 2.8 million members. Of that number, between 850,000 and 900,000 served during the Vietnam era. Approximately 40% of those actually served in SEA during the Vietnam War.
The cohort sample selection procedures are described elsewhere (Snow et al., 1988; Stellman et al., 1988a-1988d). In 1998, a second questionnaire, nearly identical to the 1984 version, was mailed to cohort members (Time 2). Extensive efforts were made to update the 1984 mailing list and especially to locate those who had dropped their Legion membership in the interim or who may have died. These efforts included use of private tracing firms, online Yellow Pages, commercial name and address listings, accession of military record data from the National Personnel Records Center (U.S. National Archives and Records Administration, St. Louis, MO), and networking within The American Legion. Through these efforts 8,088 eligible veterans were located and sent questionnaires. Nonrespondents were followed-up with several repeat mailings and additional inquiries. As a result, 4,490 men completed and returned their questionnaires, for a response rate of 55.5% to the Time 2 mailing. The breakdown by service area of those responding in both waves (n = 3,281) was 51% who did not serve in SEA and 54% who were Vietnam veterans. Follow-up efforts and questionnaire responses regarding military assignments resulted in some corrections to the military service status reported in 1984.
The present analysis is of the 1,377 Vietnam theater veterans who responded at both Time 1 and Time 2 and whose questionnaires we could evaluate for combat and PTSD. Vietnam veterans who did not respond at Time 2 were not different from those who did respond on any demographic variables, but nonresponse in 1998 was associated with lower combat exposure (M = 13.02, SD = 7.48) and higher PTSD symptoms in 1984 (M = 43.72, SD = 13.62) than those who responded at both times, combat M = 19.18, SD = 7.89; t (2574.37) = −24.07, p < .001; PTSD M = 37.37, SD = 14.54; t(2906.60) = −13.69, p < .001.
Measures
The study protocol, survey instruments, and explanatory cover letters for 1984 and 1998 were approved by the Institutional Review Board of the Columbia College of Physicians and Surgeons, New York. The survey development was described in more detail in previous reports (Koenen et al., 2003; Snow et al., 1988; J.M. Stellman et al., 1988a, 1988b; S.D. Stellman et al., 1988a, 1988b). Questionnaires in both times included items on demographic information and a detailed military service history (S.D. Stellman et al., 1988a).
Vietnam combat exposure was assessed with an eight-question Likert-type scale with five possible responses that has previously been validated in studies of Vietnam veterans (Figley, 1978; Frye & Stockton, 1982; Koenen, Stellman, Sommer, Dohrenwend, & Stellman, 2007; S.D. Stellman et al., 1988a). The questions, covering the extent of enemy fire and life-threatening situational exposures, were summed with a total score ranging from 8 to 40. The test–retest reliability was .88 over 14 years. For these analyses, we use responses provided by the veterans in 1984 (Time 1) because they are closer in time to the events. For comparability with our previous report, the scores were categorized as low (n = 520; 8−15), medium (n = 566; 16−25), or high (n = 291; 26−40).
Posttraumatic stress disorder severity was evaluated in reference to combat exposure in the Vietnam theater at both times using the 17-item 5-point Likert-type PTSD Symptom Frequency Scale developed for the 1984 survey following the diagnostic criteria for PTSD as defined by the Diagnostic and Statistical Manual for Mental Disorders, Third Edition (DSM-III; American Psychiatric Association [APA], 1980). Veterans were asked how frequently they experienced each symptom in the past month, with response options ranging from never to very often. Construct validity was demonstrated by the scale's dose-response relationship to combat exposure (Koenen et al., 2003; Snow et al., 1988). Because the PTSD symptoms from DSM-III were identical to those in The Diagnostic and Statistical Manual for Mental Disorders, Third Edition, Revised (DSM-III-R; APA, 1987), in previous work we made a presumptive PTSD diagnosis (Koenen et al., 2003) according to DSM-III-R criteria to make results comparable to other studies of Vietnam veterans (Kulka et al., 1990). That is, veterans who reported often or very often to experiencing one symptom in the intrusive reexperiencing cluster, three symptoms in the avoidance/numbing cluster, and two symptoms in the arousal cluster were classified as having presumptive PTSD. However, in this report, we describe veterans who meet the DSM-III-R symptom criteria for PTSD as having severe PTSD symptoms rather than a presumptive PTSD diagnosis. We made this change in terminology because our PTSD measure has not been validated against a structured interview for PTSD.
The following scales were adapted from the Psychiatric Epidemiology Research Instrument (Dohrenwend, Shrout, Egri, & Mendelsohn, 1980). Family functioning was examined through three separate scales. Marital satisfaction was defined as the sum of six items from a 5-point Likert-type scale that asked how often in the past 6 months the veteran had different experiences. Sexual satisfaction was determined by the sum of three items from a 5-point Likert-type scale that asked how often in the past 6 months the veteran has experienced sexual problems (e.g., difficulty reaching climax). Parenting difficulties were defined by the sum of six items from a 4-point Likert-type scale that asked how often in the past 6 months the veteran was satisfied with different aspects of parenting (e.g., getting along with your children).
Alcohol use and current smoking were determined by a series of questions taken from the American Cancer Society's Cancer Prevention Study II (S. D. Stellman & Garfinkel, 1986). Alcohol use was defined as number of drinks per week among drinkers.
Life satisfaction was measured by response to “In general, how satisfying is your life,” rated on a 4-point Likert-type scale ranging from not at all satisfying to very satisfying. Happiness was assessed by the response to “Taking all things together, how happy are you these days?” rated on a 4-point Likert-type scale ranging from not at all happy to very happy. Mental health service use was determined by veterans’ response to the question of whether they had “. . . ever seen anyone for an emotional, nervous, or mental problem?”
Veterans were asked to rate the extent to which each of 28 physical health conditions was “currently a problem” by circling a number: 1 (not a problem), 2 (a minor problem), 3 (a problem), or 4 (really a major problem). Factor analysis produced five well-separated factors that each appeared to represent a distinct health outcome dimension: faintness (Faint), fatigue or physical depression (Fatigue), aches and pains (Aches), colds (Colds), and skin effects (Skin). We have described the creation of the scales in more detail previously (Stellman et al., 1988b).
Data Analysis
First, we examined the association between combat exposure and severe PTSD symptoms at Time 1 and Time 2 using logistic regression among SEA theater veterans. The strength and significance of the association were assessed by the odds ratio (OR) with 95% confidence intervals (CIs).
Next, we conducted a set of analyses to examine whether combat exposure level had a dose-response relation with functioning at Time 2. We conducted one-way ANOVAs with three levels (combat exposure: low, medium, high) for continuous outcomes. For significant ANOVAs we conducted post hoc tests (Fisher's least significant difference [LSD] method) to determine which combat groups were significantly different in functioning outcomes at Time 2. Consistent with our previous work, we measured the association between combat exposure level and categorical outcomes using logistic regression, estimating the strength and significance by the OR with 95% CIs.
Finally, we conducted a set of analyses to examine whether persistence of severe PTSD symptoms was related to worse functioning over a 14-year period, regardless of combat exposure level. For continuous outcomes, we conducted a 3 (combat exposure level: low, medium, high) × 2 (time: 1984, 1998) × 2 (severe PTSD symptoms: no, yes) analysis of covariance (ANCOVA) controlling for severe PTSD symptoms at Time 1 to examine whether PTSD symptoms at Time 2 were associated with persisting negative effects. Time was a within-subjects variable; combat exposure level and severe PTSD symptoms were between-subjects variables. Simple effects analyses using ANOVA were conducted to examine group differences in 1998 measures when the Wilks's lambda was significant for an interaction term. These were followed by paired sample t tests to assess change over time within level of combat exposure or PTSD. We measured the association between severe PTSD symptoms and categorical outcomes using logistic regression, controlling for combat exposure level and severe PTSD symptoms at Time 1, estimating the strength and significance by the OR with 95% CIs.
All analyses were repeated using nonparametric tests, which produced similar patterns of results and so are not presented.
RESULTS
At Time 1, 11.8% of the Vietnam veterans had severe PTSD symptoms. This decreased to a prevalence of 10.5% at Time 2. Participants with severe PTSD symptoms at Time 1 were over 14 times more likely to have severe symptoms at Time 2 (OR = 14.32, 95% CI = 9.30−21.67). At both time periods, combat exposure showed a dose-response relation with severe PTSD symptoms as shown in Figure 1. (Time 1 low combat OR = 1.0 [Ref]; medium combat OR = 3.40, 95% CI = 2.26−5.13; high combat OR = 8.58, 95% CI = 5.01−13.13; Time 2 low combat OR = 1.0 [Ref]; medium combat OR = 3.02, 95% CI = 1.97−4.63; high combat OR = 6.12, 95% CI = 4.25−10.29). The association between combat exposure and PTSD was unchanged when the number of years since the veterans had served in SEA was entered into the regression model.
Figure 1.
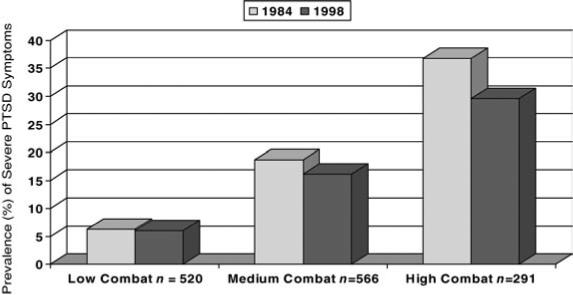
Prevalence of severe posttraumatic stress disorder (PTSD) symptoms measures in 1984 and 1998 for Vietnam veterans (n = 1377) stratified by level of combat exposure. Veterans were classified as having severe PTSD symptoms if they met the symptom criteria For PTSD according to DSM-III-R diagnostic criteria.
Combat Exposure and Functioning
We found a significant dose-response relation between level of combat exposure assessed in 1984 and all 1998 functioning measures except alcohol use, which showed a strong trend, F (2, 1271) = 2.97, p = .052. Specifically, level of combat exposure predicted less marital satisfaction among partnered veterans, F (2, 1192) = 5.69, p < .01, less sexual satisfaction, F (2, 1318) = 9.05, p < .001, more parenting difficulties among veterans with children, F (2, 1099) = 3.15, p < .05, less life satisfaction, F (2, 1339) = 14.32, p < .001, and less happiness, F (2, 1341) = 15.73, p < .001. Combat exposure was also associated with more nonspecific health problems including feeling faint, F (2, 1279) = 4.58, p = .01, fatigue, F (2, 1171) = 26.26, p < .001, aches, F (2, 1201) = 14.66, p < .001, colds F (2, 1277) = 5.28, p < .01, and skin problems F (2, 1279) = 21.09, p < .001. Post hoc tests revealed that veterans in the high combat groups had significantly (p < .05) worse functioning on all measures than veterans in the low combat group except for alcohol use, which showed a strong trend (p = .06). Medium combat veterans had significantly worse functioning than low combat veterans on all measures of functioning except parenting satisfaction (p = .11) and feeling faint (p = .06). High combat veterans had significantly worse outcomes than medium combat veterans on life satisfaction, happiness, and the nonspecific health complaints of fatigue, aches, and skin problems. For categorical outcomes, combat exposure level was significantly related to ever having been divorced, χ2 (2, N = 1377) = 14.41, p < .001 (low combat OR = 1.0 [Ref] vs. medium combat OR = 1.35, 95% CI = 1.04−1.76; vs. high combat OR = 1.81, 95% CI = 1.33−2.48; high vs. medium combat OR = 1.34, 95% CI = 1.00−1.81). Combat exposure level also significantly predicted being a current smoker, χ2 (2, N = 1377) = 29.06, p < .001 (low combat OR = 1.0 [Ref] vs. medium combat OR = 1.68, 95% CI = 1.29−2.19; vs. high combat OR = 2.24, 95% CI = 1.64−3.05; high vs. medium combat OR = 1.33, 95% CI = 1.00−1.78) and was related to use of mental health services, χ2 (2, N = 1377) = 31.00, p < .001 (low combat OR = 1.0 [Ref] vs. medium combat OR = 1.62, 95% CI = 1.18−2.23; vs. high combat OR = 2.68, 95% CI = 1.88−3.81; high vs. medium combat OR = 1.65, 95% CI = 1.20−2.28).
PTSD and Functioning
Table 1 presents the results of the PTSD and functioning analyses stratified by combat exposure level. The column labeled Time effect presents the F-statistic (Wilks's lambda) for the test of whether scores on continuous outcomes changed significantly over time. For continuous outcomes, the column labeled PTSD Time 2 effect presents the F-statistic (Wilks's lambda) for the Time 2 PTSD × Time interaction. For categorical outcomes, the same column presents the results of the Wald test for the severe PTSD symptoms at Time 2 in the logistic regression model. All models adjusted for Time 1 PTSD.
Table 1.
Measures of Family Relationships, Health Behaviors, Personal Well-Being, and Nonspecific Health Problems Among Vietnam Veterans By Posttraumatic Stress Disorder (PTSD) Status in 1998, in Relation to Vietnam Combat Experience
| Combat level and PTSD severity |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low |
Medium |
High |
||||||||||||
| −(n = 500) |
+(n = 20) |
−(n = 505) |
+(n = 61) |
−(n = 227) |
+(n = 64) |
|||||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | Time effect | PTSD Time 2 Effect | |
| Functioning outcome | ||||||||||||||
| Family functioning | ||||||||||||||
| Marital satisfaction (among partnered) | ||||||||||||||
| 1984 | 0.12 | 0.90 | −0.63 | 0.90 | −0.14 | 1.01 | −0.76 | 1.00 | −0.16 | 1.17 | −0.85 | 1.24 | F(1, 1123) = 2.28 | F(1,1123) = 27.29*** |
| 1998 | 0.07 | 0.94 | −1.46 | 1.67 | −0.11 | 0.96 | −1.14 | 1.29 | −0.03 | 1.01 | −0.70 | 1.13 | ||
| Sexual satisfaction | ||||||||||||||
| 1984 | 0.06 | 0.96 | −0.84 | 1.08 | −0.11 | 0.97 | −0.83 | 1.31 | −0.28 | 1.24 | −0.70 | 1.15 | F(1, 1290) < 1 | F(1,1290) = 5.45* |
| 1998 | 0.02 | 1.01 | −0.84 | 1.21 | −0.14 | 0.98 | −0.79 | 1.13 | 0.16 | 1.07 | −0.90 | 1.09 | ||
| Separated or divorced (among ever married) | ||||||||||||||
| % ever 1998 | 28.3 | 52.6 | 35.8 | 48.3 | 39.9 | 59.0 | − | χ2 (1, N = 1239) 6.65** | ||||||
| Parenting difficulties (among parents) | ||||||||||||||
| 1984 | −0.07 | 0.99 | 0.69 | 1.21 | 0.05 | 0.94 | 0.57 | 1.16 | −0.06 | 1.07 | 0.60 | 1.38 | F(1,1008) = 1.94 | F(1,1008) = 4.95* |
| 1998 | −0.02 | 0.93 | 1.01 | 1.43 | 0.06 | 0.92 | 0.68 | 1.17 | 0.08 | 1.12 | 0.73 | 1.23 | ||
| Negative health behaviors | ||||||||||||||
| Drinks per week (among drinkers) | ||||||||||||||
| 1984 | 13.03 | 16.40 | 25.65 | 31.88 | 14.49 | 21.46 | 22.70 | 37.19 | 16.02 | 27.07 | 25.27 | 33.14 | F(1,1366) = 49.39*** | F(1,1366) < 1 |
| 1998 | 9.16 | 14.26 | 14.65 | 18.16 | 11.30 | 22.24 | 19.03 | 33.04 | 10.67 | 17.93 | 17.43 | 33.89 | ||
| Current smokers, % | ||||||||||||||
| 1984 | 39.4 | 50.0 | 42.3 | 55.7 | 57.3 | 53.2 | - | χ2 (1, N = 1351) 5.60* | ||||||
| 1998 | 24.5 | 35.0 | 33.7 | 53.3 | 40.4 | 50.8 | ||||||||
| Personal well-being | ||||||||||||||
| Life satisfaction | ||||||||||||||
| 1984 | 0.10 | 0.94 | −0.69 | 0.94 | −0.11 | 0.98 | −0.94 | 1.01 | −0.22 | 1.07 | −0.92 | 1.30 | F(1,1237) < 1 | F(1,1237) = 36.29*** |
| 1998 | 0.04 | 0.91 | −1.35 | 1.20 | −0.08 | 0.96 | −1.41 | 1.12 | −0.19 | 1.06 | −1.25 | 1.14 | ||
| Happiness | ||||||||||||||
| 1984 | 0.12 | 0.92 | −0.85 | 1.25 | −0.11 | 0.97 | −0.85 | 0.98 | −0.21 | 1.02 | −0.99 | 1.27 | F(1,1236) < 1 | F(1,1236) = 25.87*** |
| 1998 | 0.05 | 0.91 | −0.97 | 1.10 | −0.09 | 0.97 | −1.39 | 1.03 | −0.18 | 1.03 | −1.20 | 1.26 | ||
| Used mental health services, % ever 1998 | 15.9 | 31.6 | 20.9 | 53.7 | 26.8 | 60.3 | χ2(1) = 25.51*** | |||||||
| Non-specific physical health Problems | ||||||||||||||
| Faint | ||||||||||||||
| 1984 | 0.03 | 1.11 | 0.43 | 1.52 | 0.07 | 1.00 | 0.55 | 1.66 | 0.09 | 1.00 | 0.72 | 1.75 | F(l,1170) = 1.09 | F(l,1170) = 7.87** |
| 1998 | 0.01 | 0.97 | 1.22 | 1.75 | 0.11 | 1.07 | 0.88 | 1.70 | 0.14 | 1.07 | 0.88 | 1.45 | ||
| Fatigue | ||||||||||||||
| 1984 | −0.09 | 0.90 | 1.01 | 1.13 | 0.18 | 1.07 | 1.11 | 1.36 | 0.53 | 1.20 | 1.74 | 1.89 | F(1,1052) < 1 | F(l,1052) = 27.85*** |
| 1998 | −0.06 | 0.87 | 1.69 | 1.62 | 0.15 | 1.03 | 1.53 | 1.46 | 0.30 | 1.09 | 1.95 | 1.51 | ||
| Aches | ||||||||||||||
| 1984 | −0.09 | 0.97 | 0.85 | 1.29 | 0.13 | 1.03 | 0.67 | 1.36 | 0.26 | 1.14 | 0.64 | 1.28 | F(1,1184) < 1 | F(l,1184) = 6.15* |
| 1998 | −0.06 | 0.93 | 0.86 | 1.23 | 0.07 | 0.98 | 0.86 | 1.23 | 0.29 | 1.13 | 0.82 | 1.34 | ||
| Colds | ||||||||||||||
| 1984 | −0.04 | 0.92 | 0.96 | 1.47 | 0.08 | 1.01 | 0.91 | 1.81 | 0.25 | 1.25 | 0.45 | 1.43 | F(1,1172) < 1 | F(l,1172) = 12.23*** |
| 1998 | −0.03 | 0.88 | 1.42 | 1.97 | 0.12 | 1.05 | 1.05 | 1.64 | 0.07 | 0.98 | 0.87 | 1.66 | ||
| Skin | ||||||||||||||
| 1984 | 0.00 | 0.91 | 0.33 | 1.33 | 0.25 | 1.19 | 0.71 | 1.41 | 0.42 | 1.31 | 0.89 | 1.79 | F(l,1145) = 1.74 | F(l,1145) = 15.51*** |
| 1998 | −0.07 | 0.90 | 0.50 | 1.32 | 0.19 | 1.09 | 1.06 | 1.54 | 0.27 | 1.22 | 1.21 | 1.57 | ||
Note. + = Classified as having severe PTSD symptoms, −= not classified as having severe PTSD symptoms. All values represent z-score M (SD.) unless otherwise indicated. Ns vary due to missing data.
p < .05.
p < .01.
p < .001.
The PTSD × Time interaction effects in the ANCOVAs were significant for marital satisfaction, sexual satisfaction, parenting difficulties, life satisfaction, happiness, and a range of nonspecific health complaints including feeling faint, fatigue, aches, colds, and skin problems. Simple effects comparisons indicated that veterans who had severe PTSD symptoms in 1998 exhibited significantly worse functioning (p < .001) than those who did not meet criteria for severe PTSD symptoms across all outcome measures. The association between severe PTSD symptoms at Time 2 and worse functioning remained significant (p < .001) when analyses were stratified by level of combat exposure. Veterans with severe PTSD symptoms in 1998 also showed significant declines in marital satisfaction (p < .001), life satisfaction (p < .001), and happiness (p < .01) between Time 1 and Time 2. Veterans without severe PTSD symptoms at Time 2 showed no significant worsening on any measure.
For categorical outcomes, after controlling for combat exposure and severe PTSD symptoms at Time 1, severe PTSD symptoms at Time 2 were significantly related to ever having been divorced (OR = 1.69, 95% CI = 1.13−2.56). Posttraumatic stress disorder at Time 2 was also significantly associated with being a current smoker (OR = 1.59, 95% CI = 1.08−2.36) and was related to use of mental health services (OR = 2.87, 95% CI = 1.91,4.32). The Time effect was only significant for alcohol use, which declined significantly between assessments. The PTSD Time 2 × Time interaction was not significant for alcohol use. The Combat Exposure Level × Time and Combat Exposure Level × Time × PTSD interactions were not significant at p < .05 for any measure.
DISCUSSION
Our findings demonstrate that exposure to combat during the Vietnam War continues to place veterans at risk for a wide variety of adverse psychological and social outcomes. Cross-sectional studies of this cohort and others have shown that PTSD symptoms increase in a dose-response relationship with combat exposure (Dohrenwend et al., 2006; Kulka et al., 1990; Snow et al., 1988). Indeed, our longitudinal data demonstrate that the strength of the association between combat exposure and PTSD symptoms has not diminished with time since military service. Almost 30 years after their return from Vietnam, 10% of veterans in our sample continued to experience significant PTSD symptoms. Moreover, persisting PTSD was associated with worse family functioning, more smoking and drinking, less life satisfaction and happiness, more mental health service use, and more nonspecific health complaints.
The association of PTSD with current smoking and nonspecific health complaints deserves further attention. A smaller proportion of veterans with persisting PTSD quit smoking between 1984 and 1998. Over 50% of veterans with PTSD in the medium and high combat groups were current smokers in 1998 compared to 30%−40% of those exposed to similar levels of combat, but who did meet criteria for severe PTSD symptoms. The significant association between combat-related PTSD and current smoking is consistent with other studies of veterans (Beckham, 1999; Eisen et al., 2004; Koenen et al., 2006; Schnurr & Spiro, 1999). Moreover, smoking has been posited as a mediator of the consistent association between PTSD and worse health and may be one reason veterans with PTSD had more nonspecific health complaints. Growing evidence suggests veterans with PTSD are at higher risk for future tobacco-related diseases including coronary heart disease and lung and other cancers (Boscarino, 2004, 2006; Kubzansky, Koenen, Spiro, Vokonas, & Sparrow, 2007). However, PTSD appears to have direct negative effects on self-reported health and coronary heart disease that are independent of the PTSD-smoking association (Kubzansky et al., 2007; Schnurr, Ford, et al., 2000; Schnurr & Spiro, 1999). In fact, path analytic studies suggest the direct effect of PTSD on health accounts for more of the variance than the indirect of PTSD through smoking (Schnurr & Spiro, 1999). Further longitudinal research aimed at clarifying the relationships among PTSD, smoking, and health problems in veterans is needed.
This study has several strengths including the large sample size and longitudinal follow-up. The primary limitation of our study is related to the nature of our sample. We randomly sampled from membership in a veteran's service organization (VSO). Thus, findings from our study cannot be generalized to the entire population of male Vietnam veterans. Many veterans suffering from PTSD might have been less likely to be members of this VSO and to have participated at Time 1 because one characteristic of PTSD is distancing from social relationships. Our conclusions are based on American Legionnaires who participated in the study two times 14 years apart and thus can be considered to represent a best-case scenario of men who had actively joined a VSO and twice filled out a mailed questionnaire. This best case would have resulted in a systematic underestimate of the prevalence of PTSD in The American Legion. Moreover, even within The American Legion, PTSD in 1984 was, in fact, associated with failure to have been located and to respond in 1998. As a result, we might have lost some of the most chronically ill veterans at follow-up. Indeed, 9.5% of Time 1 subjects who also responded at Time 2 met criteria for severe PTSD symptoms. The prevalence of such symptoms among those who did not respond at Time 2 was 11.1%. Thus, the persisting negative effects of PTSD are likely to be underestimated in this study.
The second major limitation of our study is the use of the self-report survey methodology. Our assessment of combat exposure and the functioning outcomes in this study were all based on veterans’ self-report, raising concerns about reporting biases. Moreover, our categorization of combat exposure as low, medium, and high was done to maintain consistency with previous work in this cohort. The actual cut-offs for each category were somewhat arbitrary as they were based on the distribution of the combat exposure measure in the original cohort. Time 1 of this study took place at least 13 years after the veterans returned from Vietnam so that immediate sequelae cannot be taken into account. The PTSD assessment was made according to a questionnaire and not validated by clinical interviews. The PTSD symptoms were assessed at two discrete points in time so that some individuals in the “no PTSD” group might have had PTSD at another time in their lives that was missed. This would result in misclassification of these individuals, dilution of differences between the PTSD, and no PTSD groups, and hence underestimation of effects.
Our findings provide further evidence that a substantial minority of Vietnam veterans continue to suffer from chronic combat-related PTSD that is associated with profound and wide-ranging negative effects on multiple areas of functioning and well-being (Zatzick et al., 1997). These findings have implications for both PTSD researchers and for clinicians caring for veterans. Further research examining the life-course sequelae of PTSD in different populations is needed. Such research will need to move beyond documenting associations, as was done in the current study, and aim to identify causal relationships between PTSD and outcomes. Longitudinal designs whereby PTSD and multiple domains of functioning are assessed at three or more time points would allow for a more thorough examination of the effect of PTSD on functioning over time and the ways in which specific domains of functioning affect the course of PTSD. Treatment studies may be particularly suited for this purpose (Schnurr, Hayes, Lunney, McFall, & Uddo, 2006).
The vast majority of men who served in the Vietnam theater are now in the 47−66 year age group, and represent almost 13% of their generation (Cohany, 1992). This group's demands on the health care system will likely increase as they age. Many veterans with PTSD, like civilians, may go to primary care physicians with non-specific health complaints rather than seeking mental health services (Neria et al., 2006). Veterans may not be aware that their current difficulties, with quitting smoking for example, may be related to persisting combat-related PTSD. Close collaboration between primary care physicians and mental health practitioners will be needed to insure such veterans receive the treatment they require and deserve.
Acknowledgments
This study was supported by the National Academy of Sciences (subcontract NAS-VA-5124-98-001), by USPHS grants CA-17613, CA-68384, CA-91401, by The American Legion and The American Cancer Society. Dr. Koenen was supported by a National Research Service Award (NRSA) postdoctoral training grant in psychiatric epidemiology (5T32MH13043) and by NIH K08 MH070627. We gratefully acknowledge the efforts of Tracy Weber, Francine Benjamin, and Carrie Tomasallo in carrying out the follow-up.
Contributor Information
Karestan C. Koenen, Departments of Society, Human Development, and Health and Epidemiology, Harvard School of Public Health, Boston, MA and Department of Psychiatry, Boston University School of Medicine, Boston, MA
Steven D. Stellman, Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY
John F. Sommer, Jr., The American Legion, Washington, DC
Jeanne Mager Stellman, Department of Preventive Medicine and Community Health, SUNY-Downstate Medical Center, Brooklyn, NY.
REFERENCES
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed. Author; Washington, DC: 1980. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed. Author; Washington, DC: 1987. [Google Scholar]
- Beckham JC. Smoking and anxiety in combat veterans with chronic posttraumatic stress disorder: A review. Journal of Psychoactive Drugs. 1999;31:103–110. doi: 10.1080/02791072.1999.10471731. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Posttraumatic stress disorder and physical illness: Results from clinical and epidemiologic studies. Annals of the New York Academy of Sciences. 2004;1032:141–153. doi: 10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Annals of Epidemiology. 2006;16:248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Caselli LT, Motta RW. The effect of PTSD and combat level on Vietnam veterans’ perceptions of child behavior and marital adjustment. Journal of Clinical Psychology. 1995;51:4–12. doi: 10.1002/1097-4679(199501)51:1<4::aid-jclp2270510102>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Cohany S. The Vietnam-era cohort: Employment and earnings. Monthly Labor Review. 1992 June;:3–15. [Google Scholar]
- Dohrenwend BP, Shrout PE, Egri G, Mendelsohn FS. Nonspecific psychological distress and other dimensions of psychopathology: Measures for use in the general population. Archives of General Psychiatry. 1980;37:1229–1236. doi: 10.1001/archpsyc.1980.01780240027003. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313:979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen SA, Griffith KH, Xian H, Scherrer JF, Fischer ID, Chantarujikapong S, et al. Lifetime and 12-month prevalence of psychiatric disorders in 8,169 male Vietnam War era veterans. Military Medicine. 2004;169:896–902. doi: 10.7205/milmed.169.11.896. [DOI] [PubMed] [Google Scholar]
- Ferrada-Noli M, Asberg M, Ormstad K, Lundin T, Sundbom E. Suicidal behavior after severe trauma. Part 1: PTSD diagnoses, psychiatric comorbidity, and assessments of suicidal behavior. Journal of Traumatic Stress. 1998;11:103–112. doi: 10.1023/A:1024461216994. [DOI] [PubMed] [Google Scholar]
- Figley CR. Stress disorders among Vietnam veterans. Brunner/Mazel; New York: 1978. [Google Scholar]
- Fischer V, Boyler JM, Bucuvalas M, Schulman MA. Myths and realities: A study of attitudes toward Vietnam veterans. Louis Harris and Associates; Washington, D.C: 1980. [Google Scholar]
- Frye JS, Stockton RA. Discriminant analyses of post-traumatic stress disorder among a group of Vietnam veterans. American Journal of Psychiatry. 1982;139:52–56. doi: 10.1176/ajp.139.1.52. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, et al. Problems in families of male Vietnam veterans with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1992;60:916–926. doi: 10.1037//0022-006x.60.6.916. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Hitsman B, Lyons MJ, Stroud L, Niaura R, McCaffery J, et al. Posttraumatic stress disorder and late-onset smoking in the Vietnam era twin registry. Journal of Consulting and Clinical Psychology. 2006;74:186–190. doi: 10.1037/0022-006X.74.1.186. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Stellman JM, Stellman SD, Sommer JF., Jr. Risk factors for course of posttraumatic stress disorder among Vietnam veterans: A 14-year follow-up of American Legionnaires. Journal of Consulting and Clinical Psychology. 2003;71:980–986. doi: 10.1037/0022-006X.71.6.980. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Stellman SD, Sommer JF, Jr., Dohrenwend BP, Stellman JM. Consistency of combat exposure reporting and course of PTSD in Vietnam veterans. Journal of Traumatic Stress. 2007;20:3–13. doi: 10.1002/jts.20191. [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Koenen KC, Spiro A, 3rd, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Archives of General Psychiatry. 2007;64:109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment study. Bruner/Mazel; New York: 1990. [Google Scholar]
- McFarlane AC, Atchison M, Rafalowicz E, Papay P. Physical symptoms in post- traumatic stress disorder. Journal of Psychosomatic Research. 1994;38:715–726. doi: 10.1016/0022-3999(94)90024-8. [DOI] [PubMed] [Google Scholar]
- Neria Y, Gross R, Olfson M, Gameroff MJ, Wickramaratne P, Das A, et al. Posttraumatic stress disorder in primary care one year after the 9/11 attacks. General Hospital Psychiatry. 2006;28:213–222. doi: 10.1016/j.genhosppsych.2006.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio AM, Weathers FW, King LA, King DW. Male war-zone veterans’ perceived relationships with their children: The importance of emotional numbing. Journal of Traumatic Stress. 2002;15:351–357. doi: 10.1023/A:1020125006371. [DOI] [PubMed] [Google Scholar]
- Samper RE, Taft CT, King DW, King LA. Posttraumatic stress disorder symptoms and parenting satisfaction among a national sample of male Vietnam veterans. Journal of Traumatic Stress. 2004;17:311–315. doi: 10.1023/B:JOTS.0000038479.30903.ed. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Ford JD, Friedman MJ, Green BL, Dain BJ, Sengupta A. Predictors and outcomes of posttraumatic stress disorder in World War II veterans exposed to mustard gas. Journal of Consulting and Clinical Psychology. 2000;68:258–268. [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Sengupta A, Jankowski MK, Holmes T. PTSD and utilization of medical treatment services among male Vietnam veterans. Journal of Nervous and Mental Disease. 2000;188:496–504. doi: 10.1097/00005053-200008000-00004. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Hayes AF, Lunney CA, McFall M, Uddo M. Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74:707–713. doi: 10.1037/0022-006X.74.4.707. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Spiro AI. Combat disorder, posttraumatic stress disorder symptoms, and health behaviors as predictors of self-reported physical health in older veterans. Journal of Nervous and Mental Disease. 1999;187:353–359. doi: 10.1097/00005053-199906000-00004. [DOI] [PubMed] [Google Scholar]
- Snow BR, Stellman JM, Stellman SD, Sommer JF., Jr. Post-traumatic stress disorder among American Legionnaires in relation to combat experience in Vietnam: Associated and contributing factors. Environmental Research. 1988;47:175–192. doi: 10.1016/s0013-9351(88)80040-9. [DOI] [PubMed] [Google Scholar]
- Stellman SD, Garfinkel L. Smoking habits and tar levels in a new American Cancer Society prospective study of 1.2 million men and women. Journal of the National Cancer Institute. 1986;76:1057–1063. [PubMed] [Google Scholar]
- Stellman SD, Stellman JM, Sommer JF., Jr. Combat and herbicide exposure in Vietnam among a sample of American Legionnaires. Environmental Research. 1988a;47:112–128. doi: 10.1016/s0013-9351(88)80037-9. [DOI] [PubMed] [Google Scholar]
- Stellman SD, Stellman JM, Sommer JF., Jr. Health and reproductive outcomes among American Legionnaires in relation to combat and herbicide exposure in Vietnam. Environmental Research. 1988b;47:150–174. doi: 10.1016/s0013-9351(88)80039-2. [DOI] [PubMed] [Google Scholar]
- Stellman SD, Stellman JM, Sommer JF., Jr. Social and behavioral consequences of combat and herbicide exposure in Vietnam among American Legionnaires. Environmental Research. 1988c;47:129–149. doi: 10.1016/s0013-9351(88)80038-0. [DOI] [PubMed] [Google Scholar]
- Stellman SD, Stellman JM, Sommer JF., Jr. Utilization, attitudes, and experiences of Vietnam era veterans with veterans administration health facilities: The American Legion experience. Environmental Research. 1988d;47:193–209. doi: 10.1016/s0013-9351(88)80041-0. [DOI] [PubMed] [Google Scholar]
- Taft CT, Pless AP, Stalans LJ, Koenen KC, King LA, King DW. Risk factors for partner violence among a national sample of combat veterans. Journal of Consulting and Clinical Psychology. 2005;73:151–159. doi: 10.1037/0022-006X.73.1.151. [DOI] [PubMed] [Google Scholar]
- Taft CT, Stern AS, King LA, King DW. Modeling physical health and functional health status: the role of combat exposure, posttraumatic stress disorder, and personal resource attributes. Journal of Traumatic Stress. 1999;12:3–23. doi: 10.1023/A:1024786030358. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, et al. Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. American Journal of Psychiatry. 1997;154:1690–1695. doi: 10.1176/ajp.154.12.1690. [DOI] [PubMed] [Google Scholar]


