Abstract
Magnetic resonance arthrography (MRA) has become the preferred modality for imaging patients with internal derangement of the wrist. However, several aspects of MRA use need to be clarified before a standardized approach to the imaging of internal derangement of the wrist can be developed. The objective of the study is to evaluate the efficiency of different magnetic resonance (MR) sequences in the detection of lesions of the triangular fibrocartilage complex (TFCC) and scapholunate and lunotriquetral ligaments on direct MRA. Thirty-one consecutive direct magnetic resonance arthrographic examinations of the wrist using a wrist surface coil were performed for the assessment of the TFCC and intrinsic ligaments on a 1.5-T MR imaging system (Signa; 16 channel, Excite, GE Healthcare, Milwaukee, WI, USA). All patients had wrist pain, and in six cases, there was associated clinical carpal instability. The presence, location, and extent of TFCC, scapholunate ligament (SLL), and lunotriquetral ligament (LTL) lesions on T1 fat-saturated, multiplanar gradient recalled (MPGR) and short tau inversion recovery (STIR) images were identified, compared, and analyzed. Forty-one lesions of the TFCC, SLL, and LTL were visualized on contrast-sensitive (T1 fat-saturated) images in 23/31 (74.2%) patients. Twenty-one lesions of the TFCC and intrinsic ligaments were visualized on noncontrast-sensitive (MPGR and STIR) images (15 tears of the TFCC and six tears of the SLL and LTL). All of these lesions were seen on T1 fat-saturated images; 48.8% (20/41) lesions seen on T1 fat-saturated images (eight tears of TFCC and 12 tears of SLL and LTT) were not seen on MPGR and/or STIR images. Superior contrast resolution, joint distention, and the flow of contrast facilitate the diagnosis of lesions of the TFCC and intrinsic ligaments on contrast-sensitive sequences making MRA the preferred modality for imaging internal derangements of the wrist. Little agreement exists regarding the value and location of perforations of the intrinsic ligaments given that both traumatic and degenerative perforations may be symptomatic. Noncommunicating defects of the ulnar attachments of the triangular fibrocartilage (TFC), tears of the dorsal segment of the SLL, and defects at the lunate attachment of the SLL have a higher likelihood of being symptomatic and caused by trauma rather than by degenerative perforation. Although no consensus exists, it would appear that most arthrographies should be started with a radiocarpal injection. Injection into the distal radioulnar joint should be added if no communicational defects are visualized following radiocarpal injection in patients with ulnar-sided wrist pain.
Keywords: Magnetic resonance imaging, Arthrography, Wrist
Introduction
More than 40 years have passed since wrist arthrography was suggested for the evaluation of the intrinsic carpal ligaments [18]. However, even wrist arthrography performed with the three-compartment injection with digital subtraction for precision [26] was criticized for its low specificity and accuracy [54].
Combination of the advantages of conventional arthrography with the direct visualization of structures on magnetic resonance (MR) imaging made magnetic resonance arthrography (MRA) the preferred modality for imaging patients with internal derangement of the wrist in some of the centers [13, 46].
Joint distension by contrast injection, visualization of contrast leak, or contrast imbibition allows better evaluation of subtle abnormalities such as a partial ligamentous tear or cartilage defects. Studies have shown excellent accuracy of direct MRA for tears of the triangular fibrocartilage complex (TFCC), scapholunate (SLL), and lunotriquetral ligaments (LTL) [30, 42, 44]. However, there are several issues that require clarification before a standardized approach to the imaging of internal derangements of the wrist can be developed. These controversial issues include: the clinical value of diagnosis of communicating and noncommunicating defects of the triangular fibrocartilage (TFC); the clinical value of diagnosis of communicating defects of the SLL and LTL; the clinical value of diagnosis of tears of extrinsic ligaments; the clinical value of medial leakage of contrast into the sheath of the extensor carpi ulnaris (ECU) tendon and through ulnar collateral ligament defects; and single vs multiple compartment injections and direct MR arthrography vs multidetector computed tomography (CT) arthrography.
Objectives
The objectives of the study were to evaluate the diagnostic efficiency of different MR sequences in the detection of tears of the triangular fibrocartilage, scapholunate ligament and lunotriquetral ligament on direct MRA and to review the literature regarding the clinical value of the diagnosis of tears of the TFCC and intrinsic and extrinsic ligaments as well as the utility of single vs multiple compartment injections.
Methods and Materials
Thirty-one consecutive direct MR arthrographic examinations of the wrist using a wrist surface coil were performed for assessment of the TFCC and intrinsic ligaments on a 1.5-T MR imaging system (Signa; 16 channel, Excite, GE Healthcare, Milwaukee, WI, USA). Wrist MRA included axial 483.332/11 (repetition time ms/echo time ms), coronal 400/12 (repetition time ms/echo time ms), and sagittal T1 533.332/11 (repetition time ms/echo time ms) fat-saturated, axial short tau inversion recovery STIR; 4400/39.16 (repetition time ms/echo time ms) and coronal multiplanar gradient recalled MPGR; 617/23 (repetition time ms/echo time ms) images. The age of patients ranged from 17 to 57 years (mean age, 40 years). All patients had wrist pain. In six cases, there was associated clinical carpal instability. Examinations were read by a musculoskeletal fellow and one of two musculoskeletal radiologists (4 and 2 years experience in MSK radiology). Findings were reported by consensus. The presence, location, and extent of TFCC, SLL, and LTL lesions on T1 fat-saturated, MPGR and STIR images, were identified, compared, and analyzed.
Results
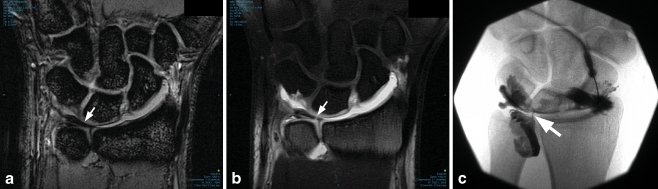
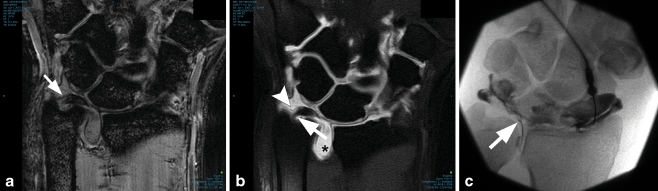
Forty-one lesions of the TFCC, SLL, and LTT were visualized on contrast-sensitive (T1 fat-saturated) images in 23 (74.2%) of 31 patients (Table 1). Communicating tears of the body of the TFC were diagnosed in nine (29%) of 31 patients (Fig. 1); noncommunicating tears were seen in two (6.5%) of 31 patients. Communicating tears of the ulnar attachments of the TFC were diagnosed in three (9.7%) patients; noncommunicating tears in four (12.9%) of 31 patients (Fig. 2).
Table 1.
Lesions detected on direct MR arthrography of the wrist.
| TFC | Ulnar attachments of TFC | SLL | LTL | ECU tendon sheath tears | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Communicating defects | Noncommunicating defects | Communicating defects | Noncommunicating defects | Dorsal portion | Ventral portion | Central portion | Complete tear | |||
| Lesions visualized on T1 fat-saturated images | 9 | 2 | 3 | 4 | 5 | 3 | 1 | 2 | 7 | 5 |
| Lesions visualized on MPGR and/or STIR images | 6 | 2 | 2 | 2 | 1 | 0 | 0 | 2 | 3 | 3 |
TFCC triangular fibrocartilage complex, SLL scapholunate ligament, LTL lunotriquetral ligament, ECU extensor carpi ulnaris
Figure 1.
A 29-year-old male with ulnar-sided wrist pain. a Coronal MPGR image demonstrates intact TFC (arrow). b Coronal T1 fat-saturated image in the location corresponding to (a) demonstrates defect in the central portion of TFC (arrow). c Arthrographic image demonstrating the flow of contrast through the TFC defect (arrow).
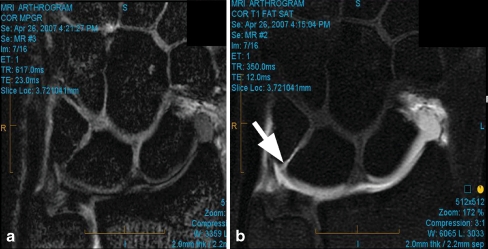
Figure 2.
A 44-year-old male with ulnar-sided wrist pain. a Coronal MPGR image does not demonstrate abnormality of ulnar attachments of TFC (arrow). b Coronal T1 fat-saturated image in the location corresponding to (a) demonstrates tear of styloid attachment (arrowhead) and intact foveal attachment of TFC (arrow). Contrast in DRUJ (asterisk) is due to the tear of TFC. c Arthrographic image demonstrating the flow of contrast through the TFC defect (arrow).
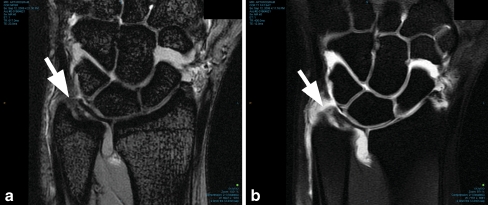
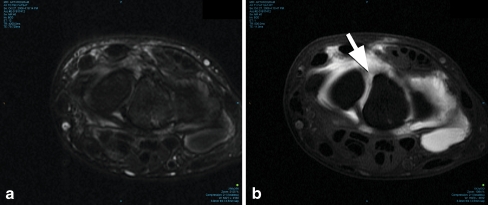
Tears of the SLL were found in 11 (35.5%) patients. Two (2/11—18.2%) were complete tears with widening of the scapholunate interval. Five (5/11—45.5%) tears were visualized in the dorsal (Fig. 3), two (2/11—18.2%) in the volar, and one (1/11—9.1%) in the central portions of the SLL. Tears of the LTL were diagnosed in seven (22.6%) of 31 patients (Fig. 4).
Figure 3.
A 40-year-old female with ulnar-sided wrist pain. a Coronal MPGR image does not clearly demonstrate abnormality of ulnar attachments and of UCL (arrow). b Flow of contrast seen on coronal T1 fat-saturated image in the location corresponding to (a) delineates (arrow) tear of ulnar attachments and tear in UCL.
Figure 4.
A 35-year-old male with wrist pain. a Axial STIR image. Scapholunate ligament cannot be reliably assessed. b Axial T1 fat-saturated image in the location corresponding to (a) demonstrates tear of dorsal portion of scapholunate ligament (arrow).
Medial capsular flow of contrast was seen in three (9.7%) of 31 patients. In all of these patients there was an associated tear of the LTL.
One (3.2%) patient had a tear of the extensor carpi ulnaris tendon sheath associated with a communicating tear of ulnar attachments of the TFC (Fig. 5). In one (3.2%) patient, a tear of the LTL was associated with a partial tear of the ECU tendon.
Figure 5.
A 30-year-old male with wrist pain. a Coronal MPGR image does not demonstrate abnormality of intrinsic ligaments. b Coronal T1 fat-saturated image in the location corresponding to (a) demonstrates flow of contrast through the tear of lunotriquetral ligament (arrow).
Twenty-one lesions of the TFCC and intrinsic ligaments were visualized on noncontrast-sensitive (MPGR and STIR) images (15 tears of the TFCC and six tears of the SLL and LTT). All of these lesions were seen on T1 fat-saturated images. Twenty (48.8%) of the 41 lesions seen on T1 fat-saturated images (eight tears of TFCC and 12 tears of SLL and LTT) were not seen on MPGR and/or STIR images.
Discussion
Despite the initial enthusiasm, magnetic resonance imaging in the absence of intra-articular contrast has not become the ultimate tool for diagnosis of internal derangement of the wrist. Hobby et al. [17] reviewed 11 publications on the diagnostic performance of MRI and found that standard MRI is highly specific but not sensitive, demonstrating an overall accuracy of 85%, a sensitivity of 70%, and a specificity of 90% if compared to arthroscopy as the gold standard. Their conclusion was that MRI without intra-articular contrast medium is unreliable in excluding tears of the intrinsic ligaments. Moreover, despite showing a high accuracy of 97% for central and radial sided TFC tears [30, 35, 50, 59] (Palmer’s class IA, ID and class II tears), MRI is only 64% accurate [15, 50] for peripheral tears of the ulnar attachment (Palmer’s class IB and IC). The poor performance of MR for these tears was attributed to the presence of high-signal vascularized fibrous tissue between the two ulnar attachments, the ligamentum subcruentum [3, 15], which can mimic a tear.
The diagnostic performance of MR is improved by MRA making lesions more conspicuous when they are outlined by contrast material in a distended joint space [19]. Braun et al. [7] concluded that MRA was of equal value when compared to diagnostic arthroscopy in detecting complete defects of the SLL and LTL ligaments and has the potential to replace the diagnostic arthroscopy. In our series, intra-articular contrast helped to diagnose 20 of 41 lesions which were not visualized on noncontrast-sensitive sequences. It was particularly helpful in the diagnosis of noncommunicating defects of ulnar attachments of the TFC, partial tears of the SLL, tears of the LTL, and tears of ECU tendon sheath and ulnar collateral ligament (UCL).
However, the clinical significance of imaging findings of TFC and ligamental tears is controversial. Multiple studies have indicated that communicating defects in the TFC and intrinsic ligaments can be frequently found on arthrography of asymptomatic wrists in 50–80% of people [8, 10, 16, 20, 27, 57]. Cadaveric and arthrographic studies have demonstrated that TFC, SLL, and LTL defects occur in asymptomatic wrists as senescent changes within the substance of the ligaments, as well as within the triangular fibrocartilage [8, 10, 18, 31, 51, 52, 55–57]. Thus, the finding of a communicating defect through any of the ligaments or TFC could represent either a symptomatic tear or an asymptomatic perforation as the result of degeneration.
To complicate the issue, even the designation of an asymptomatic wrist is problematic. Most people have wrist injuries at many times throughout their lives and asymptomatic wrist at the time of the examination cannot exclude that the wrist was previously traumatized. Moreover, there is little agreement in the literature if both symptomatic and degenerative perforations of the intrinsic ligaments and TFC can be symptomatic.
Interestingly, TFC lesions near the radial attachment of the TFC, considered to be traumatic by Palmer [38], were found to be commonly present in asymptomatic wrists [8, 57, 58] and were frequently found as congenital perforations on cadaveric study of the TFC in fetuses and in infants [47]. TFC degeneration and perforations at the central or radial portion increase with age [22]. Rüegger et al. [41] found that noncommunicating tears of the ulnar attachment of the TFC on MRA are more likely to be symptomatic than communicating tears in the radial or central aspects of the TFC. The differentiation of these peripheral tears of ulnar attachments of the TFC from central tears may be clinically important. Peripheral tears have a good vascular supply and can be associated with instability of the distal radioulnar joint (DRUJ) [38, 39] while central lesions are avascular [12, 37].
The forearm and distal carpal row are fixed units, connected by the proximal row which is referred to as the ‘‘intercalated kinematic segment’’. Disruption of the SLL causes the development of scapholunate dissociation [14], rotatory subluxation of the scaphoid, and perilunate instability [29] with consequent scapholunate advanced collapse [53].
Tears of different portions of the SLL and LTT have been shown to have varying clinical significance. This can be explained by differences in the anatomy of the ligamentous portions. The dorsal and volar portions of SLL and LTT are true ligaments, consisting of closely packed collagen fibers [6]. The dorsal portion of SLL and volar portion of LTL are the main contributors to stability. The central portions of the SLL and LTT are a thin fibrocartilaginous membrane that contributes little to wrist stability [5]. Degenerative perforations in the middle segments of the SLL and LTL are common, increase with age, are often asymptomatic, and correlate poorly with patients’ symptoms [24, 31, 57].
In contradistinction, most of the communicating defects involving the dorsal segment of the SLL and at the lunate attachment of SLL were frequently symptomatic which may be an indicator of a traumatic tear rather than a degenerative perforation [24]. Linkous et al. [24] hypothesized that the involvement of the fibrous dorsal segment produces symptomatic instability and that defects that extend into this segment (which, unlike the central segment contains nerve fibers) are more likely to be painful. The volar segment of the SLL is strengthened by the adjacent strong extracapsular volar extrinsic ligamentous complex and by the radioscapholunate ligament, which terminates at the junction of the volar and central segments of the SLL [4]. This explains why isolated communicating defects of the volar portion of the SLL are very infrequent.
Relatively little attention was paid in the literature to the evaluation of the tears of extrinsic ligaments of the wrist. Extrinsic ligaments between the radius, ulna, and carpal bones or between carpal and metacarpal bones have an important role in the maintenance of carpal stability [32, 40]. Extrinsic ligaments are intracapsular in location and include the palmar and dorsal groups of ligaments. The palmar extrinsic ligaments include the radiolunotriquetral ligament (RLTL), radioscaphocapitate ligament (RSCL), radial collateral ligament (RCL), ulnolunate ligament, palmar ulnotriquetral ligament, and scaphotriquetral ligament. The RLTL and RSCL are the most important for carpal stability [34]. The RLTL maintains the load transference and prevents ulnar translation, whereas the RSCL primarily keeps the scaphoid in position [34].
The dorsal extrinsic ligaments include the dorsal radiotriquetral ligament, dorsal scaphotriquetral ligament, and dorsal ulnotriquetral ligament. The dorsal radiocarpal and intercarpal ligaments play a role in the prevention of volar and dorsal intercalated segment instability [32].
Theumann et al. [49] confirmed that carpal instability was associated with tears of the extrinsic RSCL, RLTL, and RCL. In their series, no tears of dorsal extrinsic ligaments were noted. Based on this study, carpal instability was related to the association of tears of intrinsic and extrinsic ligaments rather than to the presence of intrinsic ligament tears alone.
Tears involving the tendon sheath of the extensor carpi ulnaris tendon and tears of ulnar collateral ligament are other issues which are only sparsely described in the literature. Machiels et al. [25] described dorsal peripheral detachment of the TFCC as a tear located at the dorsoulnar peripheral attachments of the TFCC and extending into the floor of the ECU tendon sheath. The tear can extend further into the ulnar collateral ligament. Disruption of ECU tendon sheath results in tendon instability. The authors concluded that in patients with a history of trauma and without rheumatoid arthritis who present with pain in the dorsal aspect of the wrist near the ulnar styloid along the trajectory of the ECU, contrast opacification of the tendon sheath, extravasation of contrast into the dorsal ulnar and peristyloid soft tissue are pathognomonic features of dorsal peripheral detachment of the TFCC.
Interestingly, the UCL itself is a controversial topic. In 1970, Spinner and Kaplan [45] defined the UCL as a periosteum/ECU fibro-osseous sheath. Kleinman [21] described a vestigial ulnar collateral ligament. Buterbaugh [9] defined UCL as the floor of the ECU tendon sheath. However, Osterman [36] stated that there is no true UCL. Arons et al. [2] described the defect of UCL distal to the intact TFC and exiting into the floor of the ECU tendon sheath. Such cases of “ulnar capsular leak” were described by Palmer’s group on arthrography [23]. Tears of the UCL without associated injury of the TFC or ulnal attachments of the TFC could be seen with and without ECU tenosynovitis. Repair of these disruptions at surgery leads to disappearance of the symptoms. In our series, no isolated lesions of the UCL or ECU tendon sheath were seen. All UCL tears and partial tear of ECU tendon were associated with tears of LTL. Tear of the extensor carpi ulnaris tendon sheath was associated with communicating tears of the ulnar attachments of the TFC.
No consensus exists regarding single vs multiple compartment injections of contrast on MRA. Each technique has its proponents and advantages. Mann et al. [28] concluded that the first injection of three-compartment arthrography shows unidirectional communications to the best advantage. Amrami [1] considered the single compartment arthrography to be more definitive and that the interpretation of multicompartment injections on the static MRI images obtained after arthrography is complex, since there is no available “subtraction” technique and it can be difficult to sort out which ligaments are completely or partially torn and what the direction of contrast flow has been. This author [1] preferred a single compartment injection planned with the referring surgeon, performing a single injection in the most clinically relevant compartment and then adding additional injections if a tear is not seen on the conventional arthrogram preceding MRI examination.
Zanetti et al. [58] and Rüegger et al. [41] consider noncommunicating defects of ulnar attachments of TFC to be frequently symptomatic. To diagnose these tears, the authors recommended including an injection of contrast material into the DRUJ in wrists with no communicating defects of the TFC following radiocarpal injection. They reported an accuracy of 80% and a sensitivity of 85% for peripheral TFC tears. Khouri et al. [19] suggested tailoring the examination to a one or two compartment injection when there is spontaneous intercompartmental communication and/or when the clinical query is precise (e.g., a DRUJ injection is omitted if there are no ulnar-sided symptoms).
Cerezal et al. [11] recommended performing triple compartment MRA in patients with chronic pain of unclear origin or instability of the wrist. In cases of suspected TFCC or intrinsic ligament lesions, the authors use conventional MR imaging with radiocarpal MRA. If a lesion of the ulnar attachment of the TFC is suspected at conventional MR imaging, they perform two compartment (radiocarpal and DRUJ) MRA.
A number of authors advocate using CT arthrography (CTA) for the assessment of SLL and LTL tears [11, 43, 48, 60]. Schmid et al. [43] compared CTA to standard MRI for the evaluation of SLL and LTL tears and found that CTA is also able to evaluate the different ligament segments individually and was superior to MR imaging in the detection of dorsal segment tears. Moser et al. [33] showed that CTA is more sensitive than MRA in the diagnosis of wrist ligament tears, particularly for partial tears of the SLL and LTT, which were not reliably detected [7, 33]. An additional advantage of CTA is its ability to identify cartilage defects and thinning [60]. Khoury et al. [19] suggested that CTA has an advantage over MRA as it is less prone to motion artifact due to the much shorter duration of the examination, resulting more consistently in a high diagnostic quality scan. Moser et al. [33] suggested that CTA should be used as the primary modality for the examination of intrinsic ligament tears with sensitivities, specificities, and accuracies similar or improved compared with MRA.
The limitation of this study is that the comparison was made between contrast-sensitive and noncontrast-sensitive sequences following intra-articular contrast injection. However, while gadolinium has low signal on STIR images, it is not shown to alter the tissue contrast and visualization of the anatomical structures.
Conclusions
Superior contrast resolution, joint distention, and flow of contrast facilitate diagnosis of lesions of the TFCC and intrinsic ligaments on contrast-sensitive as opposed to noncontrast-sensitive sequences of MRA. Little agreement exists regarding the clinical value and location of symptomatic perforations of the intrinsic ligaments. Although no consensus exists, it seems that most arthrographies should be started with a radiocarpal injection, adding injection into the DRUJ, in cases of ulnar-sided pain, when no communicational defects are visualized following radiocarpal injection.
Acknowledgments
Authors heartily thank Monika Ferrier, BA and Wayne B. Patola, RTR RTMR for thier very valuable assistance and advice.
References
- 1.Amrami KK. Magnetic resonance arthrography of the wrist: case presentation and discussion. J Hand Surg Am. 2006;31:669–72. [DOI] [PubMed]
- 2.Arons MS, Fishbone G, Arons JA. Communicating defects of the triangular fibrocartilage complex without disruption of the triangular fibrocartilage: a report of two cases. J Hand Surg Am. 1999;24:148–51. [DOI] [PubMed]
- 3.Benjamin M, Evans EJ, Pemberton DJ. Histological studies on the triangular fibrocartilage complex of the wrist. J Anat. 1990;172:59–67. [PMC free article] [PubMed]
- 4.Berger RA. The gross and histologic anatomy of the scapholunate interosseous ligament. J Hand Surg Am. 1996;21:170–8. [DOI] [PubMed]
- 5.Berger RA. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;383:32–40. [DOI] [PubMed]
- 6.Berger RA, Imeada T, Berglund L, An KN. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg Am. 1999;24:953–62. [DOI] [PubMed]
- 7.Braun H, Kenn W, Schneider S, Graf M, Sandstede J, Hahn D. Direct MR arthrography of the wrist: value in detecting complete and partial defects of intrinsic ligaments and the TFCC in comparison with arthroscopy. Rofo. 2003;175:1515–24. [DOI] [PubMed]
- 8.Brown JA, Janzen DL, Adler BD, et al. Arthrography of the contralateral, asymptomatic wrist in patients with unilateral wrist pain. Can Assoc Radiol J. 1994;45:292–6. [PubMed]
- 9.Buterbaugh GA. Radiocarpal arthroscopy portals and normal anatomy. Hand Clin. 1994;10:567–76. [PubMed]
- 10.Cantor RM, Stern PJ, Wyrick JD, Michaels SE. The relevance of ligament tears or perforations in the diagnosis of wrist pain: an arthrographic study. J Hand Surg Am. 1994;19:945–53. [DOI] [PubMed]
- 11.Cerezal L, Abascal F, García-Valtuille R, Del Piñal F. Wrist MR arthrography: how, why, when. Radiol Clin North Am. 2005;43:709–31. [DOI] [PubMed]
- 12.Chidgey LK. Histologic anatomy of the triangular fibrocartilage. Hand Clin. 1991;7:249–62. [PubMed]
- 13.Elentuck D, Palmer WE. Direct magnetic resonance arthrography. Eur Radiol. 2004;14:1956–67. [DOI] [PubMed]
- 14.Gelberman RH, Cooney WP III, Szabo RM. Carpal instability. Instr Course Lect. 2001;50:123–34. [PubMed]
- 15.Haims AH, Schweitzer ME, Morrison WB, et al. Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. Am J Roentgenol. 2002;178:419–22. [DOI] [PubMed]
- 16.Herbert TJ, Faithful RG, McCann DJ, Ireland J. Bilateral arthrography of the wrist. J Hand Surg Br. 1990;15:233–5. [DOI] [PubMed]
- 17.Hobby JL, Tom BD, Bearcroft PW, Dixon AK. Magnetic resonance imaging of the wrist: diagnostic performance statistics. Clin Radiol. 2001;56:50–7. [DOI] [PubMed]
- 18.Kessler I, Silberman Z. An experimental study of the radiocarpal joint by arthrography. Surg Gynecol Obstet. 1961;112:33–44. [PubMed]
- 19.Khoury V, Harris PG, Cardinal E. Cross-sectional imaging of internal derangement of the wrist with arthroscopic correlation. Semin Musculoskelet Radiol. 2007;11:36–47. [DOI] [PubMed]
- 20.Kirschenbaum D, Sieler S, Solonick D, Loeb DM, Cody RP. Arthrography of the wrist: assessment of the integrity of the ligaments in young asymptomatic adults. J Bone Joint Surg Am. 1995;77:1207–9. [DOI] [PubMed]
- 21.Kleinman WB. Scapho-trapezio-trapezoid joint arthrodesis. In: Blair WF, editor. Techniques in hand surgery. Baltimore: Williams & Wilkins; 1996. p. 835–48.
- 22.Lee DH, Dickson KF, Bradley EL. The incidence of wrist interosseous ligament and triangular fibrocartilage articular disc disruptions: a cadaveric study. J Hand Surg Am. 2004;29:676–84. [DOI] [PubMed]
- 23.Levinsohn EM, Rosen ID, Palmer AK. Wrist arthrography: value of the three-compartment injection method. Radiology 1991;179:231–9. [DOI] [PubMed]
- 24.Linkous MD, Pierce SD, Gilula LA. Scapholunate ligamentous communicating defects in symptomatic and asymptomatic wrists: characteristics. Radiology 2000;216:846–50. [DOI] [PubMed]
- 25.Machiels F, Moermans JP, Brutus JP. Arthrographic and CT arthrographic findings in dorsal peripheral detachment of the triangular fibrocartilaginous complex. JBR-BTR. 2001;84:114–7. [PubMed]
- 26.Manaster BJ. Digital wrist arthrography: precision in determining the site of radiocarpal–midcarpal communication. Am J Roentgenol. 1986;147:563–6. [DOI] [PubMed]
- 27.Manaster BJ, Mann RJ, Rubenstein S. Wrist pain: correlation of clinical and plain film findings with arthrographic results. J Hand Surg Am. 1989;14:466–73. [DOI] [PubMed]
- 28.Mann FA, Wildon AJ, Gilula LA. Triple-injection wrist arthrography: unidirectional communications are due to technical factors. J Hand Surg Am. 1998;23:82–8. [DOI] [PubMed]
- 29.Mayfield JK. Wrist ligamentous anatomy and pathogenesis of carpal instability. Orthop Clin North Am. 1984;15:209–16. [PubMed]
- 30.Meier R, Schmitt R, Krimmer H. Wrist lesions in MRI arthrography compared with wrist arthroscopy. Handchir Mikrochir Plast Chir. 2005;37:85–9. [DOI] [PubMed]
- 31.Metz VM, Mann FA, Gilula LA. Lack of correlation between site of wrist pain and location of noncommunicating defects shown by three-compartment wrist arthrography. Am J Roentgenol. 1993;160:1239–43. [DOI] [PubMed]
- 32.Mitsuyasu H, Patterson RM, Shah MA, Buford WL, Iwamoto Y, Viegas SF. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg Am. 2004;29:279–88. [DOI] [PubMed]
- 33.Moser T, Dosch JC, Moussaoui A, Dietemann JL. Wrist ligament tears: evaluation of MRI and combined MDCT and MR arthrography. Am J Roentgenol. 2007;188:1278–86. [DOI] [PubMed]
- 34.Nowalk MD, Logan SE. Distinguishing biomechanical properties of intrinsic and extrinsic human wrist ligaments. J Biomech Eng. 1991;113:85–93. [DOI] [PubMed]
- 35.Oneson SR, Timins ME, Scales LM, Erickson SJ, Chamoy L. MR imaging diagnosis of triangular fibrocartilage pathology with arthroscopic correlation. Am J Roentgenol. 1997;168:1513–8. [DOI] [PubMed]
- 36.Osterman AL. Atlas of right wrist arthroscopy. Hand Clin. 1995;11:103–13.
- 37.Osterman AL, Terrill RG. Arthroscopic treatment of TFCC lesions. Hand Clin. 1991;7:277–81. [PubMed]
- 38.Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594–606. [DOI] [PubMed]
- 39.Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;187:26–35. [PubMed]
- 40.Reicher M. Normal wrist anatomy, biomechanics, basic imaging protocol, and normal multiplanar MRI of the wrist. In: Reicher MA, editor. MRI of the wrist and hand. New York, NY: Raven; 1990. p. 17–48.
- 41.Rüegger C, Schmid MR, Pfirrmann CW, Nagy L, Gilula LA, Zanetti M. Peripheral tear of the triangular fibrocartilage: depiction with MR arthrography of the distal radioulnar joint. Am J Roentgenol. 2007;188:187–92. [DOI] [PubMed]
- 42.Scheck RJ, Kubitzek C, Hiener R, et al. The scapholunate interosseous ligament in MR arthrography of the wrist: correlation with non-enhanced MRI and wrist arthroscopy. Skeletal Radiol. 1997;26:263–71. [DOI] [PubMed]
- 43.Schmid MR, Schertler T, Pfirrmann CW, et al. Interosseous ligament tears of the wrist: comparison of multi-detector row CT arthrography and MR imaging. Radiology 2005;237:1008–13. [DOI] [PubMed]
- 44.Schmitt R, Christopoulos G, Meier R, et al. Direct MR arthrography of the wrist in comparison with arthroscopy: a prospective study on 125 patients. Rofo 2003;175:911–9. [DOI] [PubMed]
- 45.Spinner M, Kaplan EB. Extensor carpi ulnaris: its relationship to the stability of the distal radio-ulnar joint. Clin Orthop. 1970;68:124–9. [PubMed]
- 46.Steinbach LS, Palmer WWE, Schweitzer ME. Special focus session. MR arthrography. Radiographics 2002;22:1223–46. [DOI] [PubMed]
- 47.Tan AB, Tan SK, Yung SW, Wong MK, Kalinga M. Congenital perforations of the triangular fibrocartilage of the wrist. J Hand Surg Br. 1995;20:342–5. [DOI] [PubMed]
- 48.Theumann N, Favarger N, Schnyder P, Meuli R. Wrist ligament injuries: value of post-arthrography computed tomography. Skeletal Radiol. 2001;30:88–93. [DOI] [PubMed]
- 49.Theumann NH, Etechami G, Duvoisin B, et al. Association between extrinsic and intrinsic carpal ligament injuries at MR arthrography and carpal instability at radiography: initial observations. Radiology 2006;238:950–7. [DOI] [PubMed]
- 50.Totterman SM, Miller RJ, McCance SE, Meyers SP. Lesions of the triangular fibrocartilage complex: MR findings with a three-dimensional gradient-recalled-echo sequence. Radiology 1996;199:227–32. [DOI] [PubMed]
- 51.Trumble TE, Gilbert M, Vedder N. Isolated tears of the triangular fibrocartilage: management by early arthroscopic repair. J Hand Surg Am. 1997;22:57–65. [DOI] [PubMed]
- 52.Viegas SF, Ballantyne G. Attritional lesions of the wrist joint. J Hand Surg Am. 1987;12:1025–9. [DOI] [PubMed]
- 53.Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9:358–65. [DOI] [PubMed]
- 54.Weiss AP, Akelman E, Lambiase R. Comparison of the findings of triple-injection cinearthrography of the wrist with those of arthroscopy. J Bone Joint Surg Am. 1996;78:348–56. [DOI] [PubMed]
- 55.Wilson AJ, Gilula LA, Mann FA. Unidirectional joint communications in wrist arthrography: an evaluation of 250 cases. Am J Roentgenol. 1997;157:105–9. [DOI] [PubMed]
- 56.Wright TW, Del Charco M, Wheeler D. Incidence of ligament lesions and associated degenerative changes in the elderly wrist. J Hand Surg Am. 1994;19:313–8. [DOI] [PubMed]
- 57.Yin YM, Evanoff B, Gilula LA, Pilgram TK. Evaluation of selective wrist arthrography of contralateral asymptomatic wrists for symmetric ligamentous defects. Am J Roentgenol. 1996;166:1067–73. [DOI] [PubMed]
- 58.Zanetti M, Linkous MD, Gilula LA, Hodler J. Characteristics of triangular fibrocartilage defects in symptomatic and contralateral asymptomatic wrists. Radiology 2000;216:840–5. [DOI] [PubMed]
- 59.Zanetti M, Saupe N, Nagy L. Role of MR imaging in chronic wrist pain. Eur Radiol. 2007;17:927–38. [DOI] [PubMed]
- 60.Zeitoun F, Dumontier C, Dubert T, et al. Arthrography and computed tomography arthrography of the wrist. Ann Radiol (Paris). 1997;40:78–91. [PubMed]