Abstract
The purpose of this study is to present our operative technique and postoperative results of the hand replantation with proximal row carpectomy in cases of complete amputation at the level of wrist joint. From May 2003 to April 2005, five patients suffered from complete amputation of the hand due to industrial trauma. Amputation level was radiocarpal joint in three cases and midcarpal joint in two cases. Three cases represented guillotine type and two cases with local crush type injuries. All were men and the mean age was 26.6 years. The mean follow-up period was 26.8 months. At the time of replantation, the wrist joint was stabilized with transarticular fixation using three to four Kirschner’s wires after performing proximal row carpectomy. Postoperatively, functional results such as muscle strength, range of motion of the wrist and fingers, and sensory recovery were assessed according to Chen’s criteria. Joint width and arthritic changes of the radio-capitate joint were evaluated with radiologic tools. According to Chen’s criteria, the overall results in five cases were classified as grade II. Intrinsic muscle power of hands was found to be grade 4. The mean grip and pinch powers were 41% and 45%, respectively, compared to contralateral hand. The mean arc of flexion–extension of wrist was 53°. Total mean active motion of fingers was 215 degrees. Static two-point discrimination of fingertip ranged from 8 to 13 mm. On the follow-up, computerized tomography showed well-preserved radio-capitate joint space without any arthritic changes. While performing hand replantation after amputation at the radiocarpal or midcarpal level, proximal row carpectomy is a useful procedure to preserve joint motion of the wrist in selected cases.
Keywords: Hand replantation, Proximal row carpectomy
Introduction
Successful replantation following complete amputation at the wrist joint is undoubtedly worthwhile as it has an excellent potential for functional recovery. None of the presently available prosthetic devices can replace the replanted hand in both function and cosmesis [3, 6, 10, 11, 12, 18, 20, 23, 25]. During the operative sequences of replantation, bone shortening and stable bone fixation are very critical steps to achieve the final functional recovery. Anatomically, the wrist joint is composed of carpometacarpal joint, midcarpal joint, and radiocarpal joint. In cases of amputation at the level of wrist joint, there is no consensus over the selection of the method for bone fixation. It is hard for the surgeons to determine whether to preserve motion or totally immobilize the wrist joint [4, 11, 18, 25]. However, if there is no serious damage to the articular surfaces of distal radius or carpal bones, one should try to preserve the joint so as to achieve active wrist motion after replantation.
The authors focused on preserving joint using proximal row carpectomy (PRC) instead of wrist fusion in limited number of cases of complete amputation at the level of wrist. We analyzed five such cases retrospectively. Our indications for the procedure, a detailed description of the surgical technique as well as postoperative functional results are discussed.
Materials and Methods
Materials
In the last 3 years from May 2003 to April 2005, 24 cases of complete amputation of the upper limb underwent replantation at our center. Among these, there were five cases of complete amputation at the wrist level, which underwent hand replantation along with PRC. All patients were males with a mean age of 26.6 (19 to 34) years. The mean follow-up period after surgery was 26.8 (21 to 35) months.
The causative injuries were industrial-related cutter and crusher in all five cases. The amputation margins were three guillotine and two local crushing types. The level of amputation was radiocarpal joint in three cases and midcarpal joint in two cases.
Operative Techniques
As the routine sequence of the replantation, after thorough irrigation, any nonviable tissue was debrided from the stump and the amputated part. A healthy lunate fossa on the distal radius was identified and PRC was performed. Since carpal height was shortened due to PRC, we were able to perform an aggressive debridement of transected vessel, nerve, and tendon ends. Afterwards, capitate was precisely repositioned on the lunate fossa of the radius. Three or four Kirschner’s wires were used for transarticular fixation. Passage of wires through the lunate fossa was avoided. The remnant of the joint capsule of the wrist and extensor retinaculum was strongly repaired with 1-0 or 2-0 nonabsorbable braided suture materials employing multiple “figure of 8” method. Tendon sheath along with paratenon were preserved during dissection, and adequate tension was maintained while repairing flexor and extensor tendons with modified Becker’s technique [2, 14]. Both radial and ulnar arteries were anastomosed primarily. Median nerve, ulnar nerve, superficial branch of the radial nerve, and dorsal sensory branch of the ulnar nerve were also coapted without using any nerve grafts. Three or four superficial veins were anastomosed in each case. Skin closure was performed without any tension. Prophylactic fasciotomy was not required. Long-arm splint was applied after dressing. The circulation of replanted hand was closely monitored postoperatively, and anticoagulation therapy was administered with 60 μg of prostaglandin E1 and a 5,000 unit of heparin for about 1 week and a 100-mg of baby aspirin for 1 month.
Postoperative Rehabilitation and Secondary Operation
On the seventh postoperative day, rehabilitation therapy of the fingers was started with dynamic splint in a fixed neutral position of the wrist. To prevent adhesion of the tendons and intrinsic minus-deformity of the hand, we adopted crane-type dynamic splint which was proposed by Scheker et al. [20]. Combined passive and active motion and assisted active range of motion of the fingers was started on the seventh day after operation. Active range of motion of the wrist was initiated after removal of Kirschner’s wires on the sixth to eighth postoperative week. Night splint was applied for 6 months in neutral position of wrist.
In four cases, split-thickness skin graft was applied to cover the skin defect on the dorsal aspect of the wrist. Opponensplasty was performed in two cases by staged reconstruction with silicone rod and tendon graft using palmaris longus.
Postoperative Assessment
Based on the Chen’s criteria (Table 1) [5], postoperative evaluation was performed to measure total active motion of the wrist and all fingers. Pinch and grip power was measured by pinch meter and hydraulic hand dynamometer (DeRoyal, Irvington, NY, USA) and compared with contralateral side. Recovery of the muscle strength was assessed according to the criteria of British Medical Research Council [22]. Static two-point discrimination of all fingers was checked with disc-criminator (Mackinnon-Dellon, USA). Computerized tomogram and magnetic resonance images were obtained for evaluation of the degenerative changes of the radiocapitate joint or maintenance of the joint space.
Table 1.
Chen’s criteria of functional evaluation after replantation.
| Grade I (Excellent) |
| A. Ability to resume original work with a critical contribution from the reattached parts |
| B. Collective range of joint motion exceeds 60% of normal, including the joint immediately proximal to the reattached part |
| C. Recovery of sensibility to a high grade without excessive intolerance of cold |
| D. Muscular power of 4 to 5 on a scale of 1 to 5 |
| Grade II (Good) |
| A. Ability to resume some gainful work but not original employment |
| B. Range of joint motion exceeds 40% of normal |
| C. Recovery of near normal sensibility in the median and ulnar nerve distributions without severe intolerance of cold |
| D. Muscular power of grade 3 to 4 |
| Grade III (Fair) |
| A. Independence in activities of daily living |
| B. Range of motion of joints exceeds 30% of normal |
| C. Poor but useful recovery of sensibility |
| D. Muscular power of grade 3 |
| Grade IV (Poor) |
| A. Tissue survival with no recovery of useful function |
Results
All five hands were replanted successfully. There was no serious complication. After a mean follow-up period of 26.8 (21–35) months, all five cases resulted in grade II as per Chen’s criteria. Muscle strength achieved M4, making possible all synergistic and independent movements of the replanted hand. Pinch power averaged 45% (32–55) of the contralateral side. Mean grip power was 52 lb, which was 41% (28–50) of the opposite side. Average flexion and extension of wrist was 26° and 27° respectively. Total active range of motion of the wrist in flexion and extension was 53°, which is 40% of the normal side. Total active range of motion of all fingers averaged 225°, which was 90% of the contralateral hand and that of the thumb averaged 150°. Static two-point discrimination of the median and ulnar nerve area averaged 8 to 13 mm.
On the magnetic resonance imaging (MRI), computerized tomography (CT), and plain X-ray, there was no evidence of degenerative changes of the articular surfaces of both head of the capitate and lunate facet of the radius in most of the cases. Also, alignment of the joint was well preserved in most of the cases. Postoperative functional results were evaluated (Table 2).
Table 2.
Patients’ data and post-operative functional results.
| Case | Sex/age | Injury type | Secondary procedure | F/U (months) | Chen’s grade | Grip (%) | Pinch (%) | S-2PD (mm) | Wrist ROM (degrees) |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | M/29 | Guillotine | STSG Opponensplasty | 21 | II | 48 | 45 | 10–12 | F20/E30 |
| Case 2 | M/26 | Guillotine | STSG Opponensplasty | 24 | II | 39 | 52 | 12–15 | F20/E35 |
| Case 3 | M/19 | Guillotine | None | 26 | II | 34 | 35 | 8–10 | F40/E10 |
| Case 4 | M/25 | Local crushing | STSG | 28 | II | 43 | 40 | 9–11 | F30/E30 |
| Case 5 | M/34 | Local crushing | STSG | 35 | II | 28 | 32 | 10–13 | F20/E30 |
Case Reports
Case 1
A 29-year-old man, who sustained a complete amputation of the right wrist by a screw propeller of steamship, presented with guillotine-type amputation at the level of radiocarpal joint. Radiological evaluation excluded any fracture of the carpal or distal forearm bones. Replantation surgery started 6 h after initial injury and lasted for 8 h under brachial plexus block. There was no serious complication. Secondary procedures involved were skin graft to the dorsum of the wrist for resurfacing necrosed skin and staged opponensplasty with palmaris tendon graft.
After a follow-up period of 21 months, postoperative evaluation revealed that a “good” result was achieved as per Chen’s criteria. Muscle strength was M4. The key-pinch was 13 lbs, and the grip power was 40 lbs, which was 48% and 45% of the intact contralateral side, respectively. The static two-point discrimination of the fingers averaged 10 to 12 mm. Active range of motion of the wrist was 45°, with 20° of flexion and 25° of extension. Total active range of motion of all fingers averaged 225° and that of the thumb was 160°. On the final follow-up, the patient did not complain of any pain. On the MRI, CT, and plain X-ray, there was no evidence of degenerative changes on the articular surface of both the head of capitate and lunate facet of the radius. Minimal displacement of capitate toward ulnar side was noted (Fig. 1).
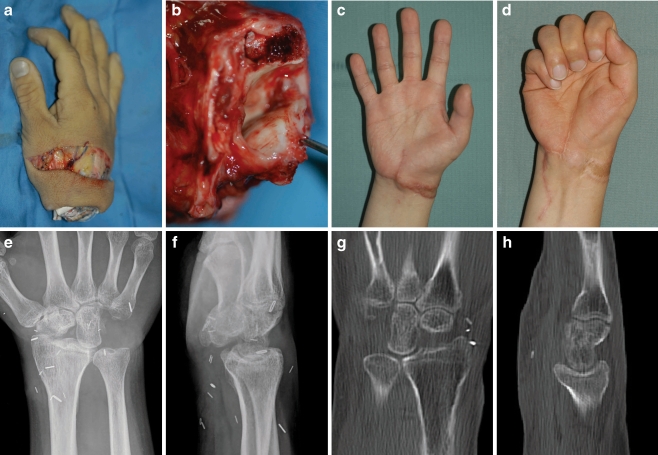
Figure 1.
a–d Preoperative view of a guillotine-type amputation of the wrist at the radio-carpal joint. e, f Postoperatively, radiograph shows wrist joint fixation using 3-Kirschner’s wires after proximal row carpectomy. g–j Appearance of the replanted wrist 21 months postoperatively. k & l, MRI demonstrates intact radio-capitate joint without any arthritic changes and perseverance of 1 mm width.
Case 2
A 26-year-old, right-hand-dominant male presented with guillotine-type amputation at the right wrist by a mill saw. The level of amputation was radiocarpal joint. Proximal parts of the lunate and trapezium were found to be fractured. Cold ischemic time was 3 h. Replantation procedure lasted for 9 h. To cover open wound of the wrist, split-thickness skin graft was applied on the dorsum of the wrist. One year after primary surgery, secondary opponensplasty was performed.
After a follow-up period of 24 months, postoperative evaluation revealed achievement of “good” results as per Chen’s criteria. Muscle strength was M4. The key-pinch was 12 lb and the grip power was 35 lb, which was 52% and 39% of the normal contralateral side, respectively.
The static two-point discrimination of all fingers averaged 12 to 15 mm. Active range of motion of the wrist was 55°, with 20° of flexion and 35° of extension. Total active range of motion of all fingers averaged 220° and that of the thumb was 150°. On the final follow-up, the patient did not complain of any pain. On the MRI, CT, and plain X-ray, there was no evidence of degenerative changes on the articular surfaces of both the head of capitate and lunate facet of the radius (Fig. 2).
Figure 2.
a, b Preoperative view of the amputation of the wrist by a food-mixing machine. Amputation at the level of radiocarpal joint with triquetrum fracture and scapholunate dissociation. c, d Appearance of the replanted wrist 24 months postoperatively. e–h Simple X-ray and computer tomography shows intact articular surface of the radio-capitate joint with a joint width 1–2 mm.
Discussion
Since the first clinical success of replantation of the upper arm in 1962 [17], with persistent development of microsurgical instruments and microscope, replantation surgery is regarded as the first option in the selected cases of amputation of the extremity [3, 10–12, 18, 23, 25]. Technological development in the field of prosthesis is reported to replace replantation surgery [8, 15, 16]. However, in cases of hand replantation after amputation at the level of the wrist, postoperative functional results of the replanted hand have been reported to be highly satisfactory due to following two reasons. Firstly, extrinsic neuromuscular motor units which control fine motion of the hand are well preserved in the proximal portion of the forearm. Secondly, the amputated part mainly lacks muscles which render it least susceptible to infection and ischemia [6, 11, 18, 25]. After a thorough literature search, we did not find many reports relating to operative technique or postoperative results of hand replantation only in the cases of amputation at the level of wrist [11]. Most of published reports relate to replantation at several different levels following major limb amputation.
Both bone shortening and fixation are critical steps to achieve successful replantation. There is no consensus about how to shorten or fix the bone in cases of complete amputation at the level of wrist [5, 11, 24]. Generally, in cases of amputation around distal forearm, plate and screw fixation is preferred. Multiple Kirschner’s wire fixation is good following amputation at the radiocarpal level. In cases of amputation at the level of intercarpal joint with or without fractures of proximal carpal row, PRC is recommended. In cases of extensive bone fractures around radiocarpal joint, wrist arthrodesis may be selected [4]. Meyer et al. [18] suggested wrist fusion or PRC in cases of amputation around intercarpal or radiocarpal amputation. However, details of the procedure were not explained. Vanstraelen et al. [25] reported arthrodesis of the wrist joint with Steinman pin fixation of the third metacarpal bone and radius. Theoretically, it seemed unstable due to rationale of forces but no complications were reported. Recently, Hoang et al. [11] performed cross fixation of the wrist joint with two or three Kirschner’s wires in case of wrist amputation. The wires were removed on the tenth week after operation.
The authors could get an overall shortening effect of 2–3 cm by PRC, and it facilitated radical debridement of the soft tissue as well as direct repair of the vessels and nerves without any graft. Also, it saved overall operative time and facilitated early regeneration of the replanted tissues as well as their early rehabilitation. In the authors’ opinion, strong repair of the joint capsule and connective tissues around the wrist joint also preserved the function of the reconstructed wrist joint between lunate fossa of the radius and capitate after removal of the Kirschner’s wires.
PRC is not a salvage procedure but a reconstructive option in cases with degenerative joint arthritis of the radiocarpal joint caused by scapholunate advanced collapse, scaphoid nonunion advanced collapse, trans-scaphoid perilunate fracture dislocations, lunate dislocations, and Kienbock’s disease. It relieves pain as well as preserves some range of motion of the wrist [4, 9, 13, 24]. According to a recently published paper [13], the authors reviewed 10 years follow-up of 22 cases after PRC due to advanced Kienböck’s disease, scapholunate advanced collapse, and scaphoid nonunion advanced collapse. Range of motion of the wrist in flexion and extension was 60%, and grip power was 80% of the contralateral intact side. The gap of the joint between capitate and lunate fossa of the radius was maintained about 1 mm. Other authors have also reported good long-term functional results following PRC [22, 24].
Anatomically, two thirds of radial aspect of the lunate articulates with lunate fossa of the radius and one third of the ulnar side with triangular fibrocartilage in neutral position of the wrist [21]. It is important that there is no damage to the articular surfaces of both capitate and lunate fossa of the radius prior to PRC. From the biomechanical point of view, there is one disadvantage of PRC. The differences of adjacent curvatures between lunate fossa of the radius and capitate may cause some rotation or displacement resulting in progressive cartilage damage and degenerative osteoarthritic changes [4, 9]. On the long-term follow-up radiologic view, capitate may gradually displace in ulnar direction and finally dislocate from the lunate fossa of the radius [7]. Utmost precaution is taken so as not to pass the Kirschner’s wires through the articular surface of the neo-joint between capitate and lunate fossa of the radius. An injury to articular surface can lead to early degenerative changes. The joint capsule of the wrist and extensor retinaculum should be repaired in a strong and secure way [4, 13].
The final goal of the replantation surgery after amputation at the wrist level is to restore function and appearance (Table 1). Maximum restoration of intrinsic muscle function can be achieved to a certain limit. The use of dynamic splint after replantation helps to prevent intrinsic minus deformity caused by muscle atrophy. Also, rehabilitation therapy aims to prevent tendon adhesions of both extrinsic flexor and extensor tendons. The strength of flexor and extensor tendon repair using modified Becker’s technique is strong enough to bear the active motion at the early postoperative period [1, 14]. Based on the strong repair of the tendons, it was possible to start assisted active motion with crane-typed dynamic splint [20]. It enabled achievement of almost full range of motion of the fingers and prevented adhesions of the extrinsic tendons in our cases.
In cases of major limb replantation at the level of elbow or proximal forearm, prophylactic fasciotomy has been recommended to prevent compartment syndrome. But in cases of amputation at the level of distal forearm or wrist or less than 4 to 6 h of ischemic time, the need of prophylactic fasciotomy is decreased. In authors’ cases, prophylactic fasciotomy was not performed, and no signs of compartment syndrome of intrinsic muscles were noted in the replanted hands [6, 19].
This paper has a limitation of the short period of follow-up and limited number of cases. In cases of complete amputation at the level of wrist joint among many cases of major limb replantation, PRC is a promising procedure to achieve functional restoration of the wrist and hand. This procedure has limited set of indications and may be successfully applied in a selected group of cases.
Conclusion
We achieved good functional results in selected cases of young individuals after hand replantation following complete amputation at the level of the wrist joint. Skeletal shortening was achieved by PRC, which facilitated primary repair of neurovascular structures and tendons initially and provided acceptable range of motion of the wrist on a short follow-up period. In case of development of degenerative arthritis in the future, total wrist arthrodesis as a salvage procedure may be opted.
References
- 1.Angeles JG, Heminger H, Mass DP. Comparative biomechanical performances of 4-strand core suture repairs for zone II flexor tendon lacerations. J Hand Surg [Am]. 2002;27:508–17. doi:10.1053/jhsu.2002.32619. [DOI] [PubMed]
- 2.Becker H, Orak F, Duponselle E. Early active motion following a beveled technique of flexor tendon repair: report on fifty cases. J Hand Surg [Am]. 1979;4:454–60. [DOI] [PubMed]
- 3.Beris AE, Soucacos PN, Malizos KN, Mitsionis GJ, Soucacos PK. Major limb replantation in children. Microsurgery. 1994;15:474–8. doi:10.1002/micr.1920150708. [DOI] [PubMed]
- 4.Cannon DL, Urbaniak JR. Transcarpal and radiocarpal wrist amputation and replantation. In: Watson HK, Weinzweig J, editors. The wrist. 1st ed. New York: Lippincott Williams & Wilkins; 2001. p. 269–76.
- 5.Chen ZW, Meyer VE, Kleinert HE, Beasley RW. Present indications and contra-indications for replantation as reflected by long-term functional results. Orthop Clin North Am. 1981;12:849–70. [PubMed]
- 6.Chuang DC, Lai JB, Cheng SL, Jain V, Lin CH, Chen HC. Traction avulsion amputation of the major upper limb: a proposed new classification, guidelines for acute management, and strategies for secondary reconstruction. Plast Reconstr Surg. 2001;108:1624–38. doi:10.1097/00006534-200111000-00030. [DOI] [PubMed]
- 7.Chung DW, Kim KB, Chun SW. Proximal row carpectomy for management of the post-traumatic arthritis of the carpus. J Korean Soc Surg Hand. 2001;6:69–74.
- 8.Cupo ME, Sheredos SJ. Clinical evaluation of a new, above-elbow, body-powered prosthetic arm: a final report. J Rehabil Res Dev. 1998;35:431–46. [PubMed]
- 9.DiDonna ML, Kiefhaber TR, Stem PJ. Proximal row carpectomy: study with a minimum of ten years of follow-up. J Bone Joint Surg Am. 2004;86:2359–65. [PubMed]
- 10.Graham B, Adkins P, Tsai TM, Firrell J, Breidenbach WC. Major replantation versus revision amputation and prosthetic fitting in the upper extremity: a late functional outcomes study. J Hand Surg [Am]. 1998;23:783–91. doi:10.1016/S0363-5023(98)80151-2. [DOI] [PubMed]
- 11.Hoang NT. Hand replantations following complete amputations at the wrist joint: first experiences in Hanoi, Vietnam. J Hand Surg [Br]. 2006;31:9–17. doi:10.1016/j.jhsb.2005.09.018. [DOI] [PubMed]
- 12.Ipsen T, Lundkvist L, Barfred T, Pless J. Principles of evaluation and results in microsurgical treatment of major limb amputations: a follow-up study of 26 consecutive cases 1978–1987. Scand J Plast Reconstr Hand Surg. 1990;24:75–80. doi:10.3109/02844319009004524. [DOI] [PubMed]
- 13.Jebson PJ, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study. J Hand Surg [Am]. 2003;28:561–9. doi:10.1016/S0363–5023(03)00248-X. [DOI] [PubMed]
- 14.Kim KC, Ha SH, Lee GJ, Kim JS, Woo SH. Modified Becker’s repair in zone II flexor tendon injury followed by early active mobilization. J Korean Soc Surg Hand. 2004;9:257–61.
- 15.Kuiken T. Targeted reinnervation for improved prosthetic function. Phys Med Rehabil Clin N Am. 2006;17:1–13. doi:10.1016/j.pmr.2005.10.001. [DOI] [PubMed]
- 16.Lake C, Dodson R. Progressive upper limb prosthetics. Phys Med Rehabil Clin N Am. 2006;17:49–72. doi:10.1016/j.pmr.2005.10.004. [DOI] [PubMed]
- 17.Malt RA, McKhann CF. The classic Replantation of severed arms. Clin Orthop Relat Res. 1978;133:3–10. [PubMed]
- 18.Meyer VE. Hand amputations proximal but close to the wrist joint: prime candidates for reattachment (long-term functional results). J Hand Surg [Am]. 1985;10:989–91. [DOI] [PubMed]
- 19.Pederson WC. Replantation. Plast Reconstr Surg. 2001;107:823–41. doi:10.1097/00006534-200103000-00027. [DOI] [PubMed]
- 20.Scheker LR, Chesher SP, Netscher DT, Julliard KN, O’Neill WL. Functional results of dynamic splinting after transmetacarpal, wrist, and distal forearm replantation. J Hand Surg [Br]. 1995;20:584–90. doi:10.1016/S0266-7681(05)80115-9. [DOI] [PubMed]
- 21.Schuind F, Linscheid RL, An KN, Chao EY. A normal data base of posteroanterior roentgenographic measurements of the wrist. J Bone Joint Surg Am. 1992;74:1418–29. [PubMed]
- 22.Smith P. Lister’s The hand: Diagnosis and Indications, 4th Ed. London, Edinburgh: Churchill Livingstone; 2002. pp 224–226.
- 23.Tark KC, Kim YW, Lee YH, Lew JD. Replantation and revascularization of hands: clinical analysis and functional results of 261 cases. J Hand Surg [Am]. 1989;14:17–27. doi:10.1016/0363-5023(89)90054-3. [DOI] [PubMed]
- 24.Tomaino MM, Delsignore J, Burton RI. Long-term results following proximal row carpectomy. J Hand Surg [Am]. 1994;19:694–703. doi:10.1016/0363-5023(94)90284-4. [DOI] [PubMed]
- 25.Vanstraelen P, Papini RP, Sykes PJ, Milling MA. The functional results of hand replantation: the Chepstow experience. J Hand Surg [Br]. 1993;18:556–64. doi:10.1016/0266-7681(93)90003-X. [DOI] [PubMed]