Abstract
Acute calcific tendinitis (ACT) is a relatively uncommon disorder of the hand and wrist. ACT is a well-known condition of the shoulder, but it often goes unrecognized when occurring in the hand or wrist. The overall lack of familiarity along with the non-specific symptoms associated with ACT frequently leads to misdiagnosis or delay in diagnosis. We report a case of acute calcific tendinitis occurring in the carpal tunnel which is a rare presentation.
Keywords: Calcific tendinitis, Peritendinitis, Tenosynovitis
Introduction
Acute calcific tendinitis (ACT) is an inflammatory condition that manifests itself as pain in the hand or wrist. Symptoms generally include pain, tenderness, edema, and erythema often localized near a joint [12]. While calcific tendonitis is well documented in the shoulder, it is relatively less well known in the hand and frequently misdiagnosed. Acute calcific tendonitis has been mistaken for other diagnoses such as acute infection, gout, or fracture [2–4, 7–9, 11]. Patients are often inappropriately treated with antibiotics or even surgery [4].
Acute calcific tendinitis of the hand has been described occurring at many of the small joints of the hand and wrist involving both the flexor and extensor tendons. Most commonly, ACT occurs at the insertion of the FCU tendon at the pisiform [2]. We describe a case of acute calcific tendinitis occurring within the carpal tunnel. This is a somewhat rare presentation with only one other case of ACT occurring within the carpal tunnel described in the current literature [5]. We feel this case illustrates the difficulty of making the diagnosis and may help others by increasing awareness of ACT in the hand.
Case Report
A 45-year-old woman presented to the emergency department complaining of exquisite right hand pain. Three days prior to presentation, the patient underwent electromyography (EMG) as part of an evaluation for carpal tunnel syndrome. In the ensuing 3 days the patient developed severe pain and swelling throughout the hand and wrist. The patient denied any fevers, chills, history of trauma, arthritis, or inflammatory disease.
On physical examination the hand was moderately swollen and warm when compared to the other side. The patient was tender to palpation along both the dorsal and volar wrist, and had pain with passive motion of both the wrist and digits. The compartments of the forearm were soft and non-tender and there was no erythema or evidence of trauma. Plain radiographs of the hand were obtained and were unremarkable as were white blood cell count and serum electrolytes.
At the time of examination, it was felt that the patient’s constellation of symptoms and physical examination findings were suggestive of complex regional pain syndrome perhaps brought about by the mild trauma of her recent EMG. The patient was sent for further testing which consisted of a bone scan, quantitative sudomotor axon reflex test, and comparative sweat and temperature testing. Test results were normal with the exception of the bone scan which showed increased uptake along the radial aspect of the carpus suggestive of possible scaphoid fracture.
Computed tomography scan of the wrist was obtained and revealed ossification within the carpal canal (Fig. 1). The diagnosis of calcific tendinitis was entertained, but given the recent EMG which was positive for median neuropathy at the wrist, the patient was scheduled for exploration of the wrist with release of the carpal tunnel.
Figure 1.
Computed tomography scan of the wrist showing ossification volar to the lunate (arrow).
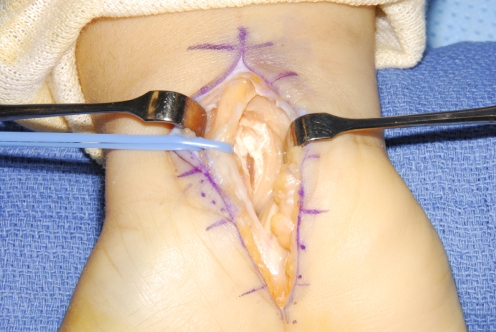
Upon exploration, there was substantial inflammation and synovitis within the carpal tunnel. The median nerve appeared normal; however, there was a white paste-like substance beneath the median nerve surrounding the flexor pollicis longus tendon (Fig. 2). The tissue was removed and sent to pathology for evaluation. The carpal tunnel was irrigated and the skin closed. The patient was placed in a volar splint for comfort postoperatively.
Figure 2.
Median nerve retracted revealing calcification within the carpal canal.
The patient was seen back in 3 days with significant improvement in her symptoms. Pathologic evaluation of the specimen confirmed calcific tendinitis. Follow-up examination at 3 months demonstrated resolution of the wrist and median nerve symptoms.
Discussion
Cohen first described acute calcific tendinitis in the hand in 1924 [3]. Since that time there have been several reports describing cases of acute calcification surrounding joints and tendons of the hand and wrist. While thought to be a rare condition, two case series of over 100 patients by Yelton and Carroll suggest otherwise [2, 12]. It may be that lack of familiarity with the disorder actually leads to under-recognition and misdiagnosis [4]. There is little published on ACT in the hand outside of the medical and rheumatologic literature. Hand surgeons are likely to see the acute presentations of ACT, but there are few published reports in the hand surgery literature [5, 8, 13, 14].
The literature describes acute calcific tendinitis in the hand and wrist as being frequently misdiagnosed. Calcific tendonitis has been mistaken for acute fracture, septic arthritis, tenosynovitis, and gout [2–4, 7–9, 11]. Serologic testing is not generally helpful in making the diagnosis. Radiographic studies will often allow the correct diagnosis to be made; however, special views may be necessary. Rarely, calcifications may not be visible on plain radiographs [12]. At times, it is not until surgical intervention occurs that the correct diagnosis is made.
Acute calcific tendinitis is a self-limiting process and often will resolve without treatment over the course of several weeks [2]. Immobilization along with aspirin or non-steroidal anti-inflammatory drugs may shorten the duration of symptoms to roughly 7 days [8]. Radiation and surgical evacuation were treatment options used in the past, but are no longer advocated. Steroid injection, colchicine, and prednisone have also been used with success [6]. The calcifications found on radiographs tend to disappear over the course of several weeks [4, 8].
The etiology of calcific tendinitis is not yet completely clear. Some feel that the calcification is a result of local tissue hypoxia, while others believe that it is a result of trauma [1, 2]. The symptoms of ACT are not thought to be a result of the calcification itself, but rather the rupture of a calcific deposit into the adjacent soft tissue [2]. The presence of the calcific material in the soft tissues results in an acute inflammatory response causing localized pain, edema, and occasionally erythema.
In the case that we present, the diagnosis was not made until the patient underwent operative exploration. The patient’s pre-existing carpal tunnel syndrome, recent EMG, and broad constellation of symptoms confounded the clinical picture making a proper diagnosis difficult. Imaging studies, while diagnostic for a calcific deposit in the carpal tunnel was suggestive of ACT, but the severity of the patient’s symptoms along with confirmed median neuropathy made non-operative treatment difficult.
While the symptoms of ACT may have resolved with conservative treatment, her acute pain and pre-existing carpal tunnel syndrome responded well to surgical treatment. This case confirms how elusive the final diagnosis can be with ACT in the hand and wrist. We hope that by presenting this case we will increase awareness of ACT leading to improved diagnosis and treatment of the process.
References
- 1.Ali AN, Kelly JL. Acute Calcific tendinitis of the finger—a case report. Hand Surg. 2004;9:105–7. doi:10.1142/S0218810404001954. [DOI] [PubMed]
- 2.Carroll RE, Sinton W, Garcia A. Acute calcium deposits in the hand. J Am Med Assoc 1955;157:422–6. [DOI] [PubMed]
- 3.Cohen I.. Calcareous deposit at the insertion of flexor carpi ulnaris tendon following trauma. Am J Surg. 1924;38:172–3.
- 4.Dilley DE, Tonkin MA. Acute calcific tendonitis in the hand and wrist. J Hand Surg. 1991;16B:215–6. [DOI] [PubMed]
- 5.Greene TL, Louis DS. Calcifying tendinitis in the hand. Ann Emerg Med 1980;9:438–40. doi:10.1016/S0196-0644(80)80160-0. [DOI] [PubMed]
- 6.Moyer RA, Bush DC, Harrington TM. Acute calcific tendinitis of the hand and wrist: a report of 12 cases and a review of the literature. J Rheumatol 1989;16:198–202. [PubMed]
- 7.Omololu B, Alonge TO, Ogunlade SO. Acute calcific tendonitis simulating tendon sheath infection. West Afr J Med 2001;20:73–4. [PubMed]
- 8.Sandstrom C.. Peritendinitis calcarea: a common disease of middle life: its diagnosis, pathology, and treatments. Am J Rheumatol. 1938;40:1–21.
- 9.Seiler JG, Kerwin GA. Adolescent trigger finger secondary to post-traumatic chronic calcific tendinitis. J Hand Surg. 1995;20A:425–7. [DOI] [PubMed]
- 10.Selby CL. Acute calcific tendonitis of the hand. An infrequently recognized frequently misdiagnosed form of periarthritis. Arth Rheum. 1984;27:337–40. doi:10.1002/art.1780270314. [DOI] [PubMed]
- 11.Thompson GR, Ting YM, Riggs GA, et al. Calcific tendonitis and soft tissue calcification resembling gout. JAMA 1968;203:464–72. doi:10.1001/jama.203.7.464. [DOI] [PubMed]
- 12.Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendonitis. A new concept of its pathogenesis. Clin Orthop Relat Res. 1976;118:164–8. [PubMed]
- 13.Verfaillie S, De Smet L, Leemans A, et al. Acute carpal tunnel syndrome caused by hydroxyapatite crystals: a case report. J Hand Surg. 1996;21A:360–2. [DOI] [PubMed]
- 14.Yelton CL, Dickey LE. Calcification about the hand and wrist. South Med J 1958;51:489–95. doi:10.1097/00007611-195804000-00014. [DOI] [PubMed]
- 15.Yosipovitch G, Yosipovitch Z.. Acute calcific periarthritis of the hand and elbows in women. A study and review of the literature. J Rheumatol 1993;20:1533–8. [PubMed]