Abstract
Background
Is living alone a risk factor for depression among older adults? Previous research is mixed and inconclusive, and it is unclear whether living alone influences psychological distress independently of other interrelated risk factors for depression. We reexamine this association and evaluate whether it is contingent on gender, physical disability, social support, and Hispanic ethnicity.
Methods
We analyze data from a multiethnic sample of older disabled and nondisabled adults residing in Miami-Dade County, Florida (n = 947). We employ descriptive and multivariate analyses stratified by Hispanic ethnicity to assess the relationship between living alone and depressive symptoms and evaluate whether any association is conditioned by gender, physical disability, and social support.
Results
Living alone is associated with higher levels of depressive symptoms among Hispanics but not among non-Hispanics. Variations in social support did not account for the higher overall levels of depression reported by Hispanics living alone relative to their counterparts living with a spouse, partner, or others. However, social support moderated the association between living alone and depression among both Hispanics and non-Hispanics.
Conclusions
We discuss the implications of our findings for future research, especially as they relate to observed ethnic differences in the relationship between living alone and depressive symptoms.
Keywords: Living arrangements, Depression, Hispanic, Physical disability, Gender, Social support
AN increasing proportion of older adults now live alone (Fields, 2004; Saluter, 1994). In light of this trend, it is surprising that little is known about whether living alone increases risk for depression among this segment of the population. The limited research on this matter has produced mixed results, underscoring the need to better understand the psychosocial circumstances that underlie this relationship. For instance, some studies show that living alone is positively associated with mental health problems such as anxiety, depression, dementia, and cognitive decline (Dean, Kolody, Wood, & Matt, 1992; Joutsenniemi et al., 2006; van Gelder, Tijhuis, Kalmijn, Giampaoli, Nissinen, & Kromhout, 2006; Ramos & Wilmoth, 2003; Sibley et al., 2002; Waite & Hughes, 1999), whereas other studies find that living alone decreases the frequency of feelings of anger and emotional distress (Glick, 1994; Ng et al., 2004; Osborn et al., 2003; Schieman, 1999).
It is also unclear whether living alone influences psychological distress net of other relevant social characteristics. Many common attributes of older persons living alone tend to be associated with depressive symptoms. For example, older adults who live alone are more likely to be female and widowed (Dean et al., 1992; Victor, Scambler, Bond, & Bowling, 2000), characteristics that are risk factors for depression (Carnelley, Wortman, & Kessler, 1999; Cole & Dendukuri, 2003). In addition, elders living alone with physical limitations and low financial resources report lower levels of psychological well-being than those with higher incomes and better health (Hays & George, 2002; Mills & Henretta, 2001). These studies demonstrate the importance of taking into account gender, marital history, and socioeconomic resources when examining the influence of living alone on depression. Similarly, stressful life events, particularly age-related losses and the onset of serious health problems, are linked with experiences of depression and loneliness in samples of older adults (Dean et al., 1992; Victor et al., 2000). Thus, research is needed to better estimate whether the potential association between living alone and depressive symptoms is independent of recent exposure to undesirable life events (Victor et al., 2000).
Scholars have also noted the importance of distinguishing the influence of living alone on psychological distress from the detrimental effects of low levels of social support (Dean et al., 1992) because perceptions of emotional support tend to be correlated with marital status and the social composition of the household (Alwin, Converse, & Martin, 1985; Hughes & Waite, 2002; Yeh & Lo, 2004). Married older adults tend to perceive higher levels of social support than unmarried adults, and much of the positive effect of marriage on psychological well-being is attributable to the supportive benefits of living with one's spouse (Ross, 1995; Turner & Marino, 1994). Living alone, in contrast, is often linked with social isolation (Hughes & Gove, 1981; Klinenberg, 2001) and reliance on interactions with friends and relatives outside the household for emotional support (Rogers, 1996; Sarason & Sarason, 2001). Living alone can impede social integration among older adults by structurally increasing social isolation and limiting the development of close social relationships (Hughes & Gove, 1981). Thus, the association between living alone and psychological distress may be mediated through variations in social support across household composition.
In addition to potential mediating factors, more research is needed to identify social characteristics that may moderate the association between living alone and psychological distress. Previous research indicates that living alone is more detrimental for the mental health of men than for women (Dean et al., 1992; Hughes & Waite, 2002; Jeon, Jang, Rhee, Kawachi, & Cho, 2007). Although some ethnographic investigations suggest that older adults living alone are more vulnerable to social isolation due to estrangement from their social networks (Klinenberg, 2001), other research indicates that women living alone are neither socially isolated nor at increased risk for declines in mental health and that they actually report superior psychological functioning relative to women living with a spouse (Michael, Berkman, Colditz, & Kawachi, 2001). Living alone may be less consequential for the well-being of women because they maintain more active social ties to friends and relatives and tend to report higher levels of social support, regardless of their marital status (Michael et al., 2001; Reissman, 1990; Turner & Marino, 1994). It follows from this prior work that variations in social support between men and women living alone may account for the potential conditional relationships between gender, living alone, and depressive symptoms.
Living alone is also likely to be more harmful to the psychological well-being of older adults with a physical disability. Physical disability represents a source of chronic stress that involves lasting difficulties in managing everyday instrumental and social activities (Turner & Noh, 1988) and is strongly linked to depression in studies of older adults (Adams, Sanders, & Auth, 2004; Mills & Henretta, 2001). As a consequence of involuntary isolation from others, physically disabled older adults who live alone may experience greater psychological distress than their nondisabled counterparts.
In addition to gender and physical disability, social support may also moderate the relationship between living alone and depressive symptoms. The social support networks of older adults who live alone often differ from those of their counterparts who live with their spouse or partner, containing more friends and remote family members (Barrett, 1999). The substitution of social support from friends and distant relatives in place of closer ties to kin and family members may affect the psychological benefits of perceiving high emotional support. As a consequence of differences in the composition of their social networks, perceptions of social support may be less protective against experiences of depression among older adults living alone compared with their counterparts who live with a spouse or partner.
Finally, there is evidence that the relationship between living alone and depressive symptoms varies by ethnicity. Previous research indicates that Hispanics who live alone report higher levels of depression than other ethnic groups in similar living arrangements (Waite & Hughes, 1999). Living alone may be more damaging to the emotional health of Hispanics because of cultural preferences for family closeness and extended family living arrangements (Waite & Hughes, 1999). Hispanic culture is differentiated from other ethnic groups by strong kinship bonds and frequent interactions between extended family members, which can buffer the effects of stress exposure on psychological distress (Ross, Mirowsky, & Cockerham, 1983; Wilmoth, 2001). Older Hispanics living alone, especially immigrants, may be more disengaged from protective features associated with their culture and therefore may be more susceptible to depression relative to other ethnic groups.
Research Objectives
In the present study, we attempt to address these issues by reexamining the association between living alone and psychological distress among a sample of Hispanic and non-Hispanic older adults (60 years of age and older). We hypothesize that (a) living alone is positively associated with level of depressive symptoms and that this association is independent of other individual and social characteristics; (b) living alone has a greater effect on depressive symptoms among men and older adults with a physical disability; (c) variations in social support will mediate gender differences in the relationship between living alone and depressive symptoms; (d) the magnitude of the protective influence of social support on depressive symptoms is weaker among older adults living alone than for those living with their spouse or partner; and (e) Hispanics living alone, especially men, those with a physical disability, and those who perceive their family and friends as unsupportive, are more vulnerable to depression relative to non-Hispanics.
METHODS
Sample
Data for this paper are drawn from a community-based study undertaken to examine the social antecedents and correlates of mental health and substance problems among individuals with and without a physical disability. The sampling frame for this survey was developed by screening 10,000 households within Miami-Dade County, Florida. The details of this sampling procedure have been presented elsewhere (Turner, Lloyd, & Taylor, 2006). The sampling frame was stratified such that there were even numbers of women and men, even numbers of people screened as having a physical disability and those not, and even numbers of four major ethnic groups in Miami-Dade County (Cubans, other Hispanics, African Americans, and non-Hispanic Whites). Excluded were those disabled solely due to psychiatric or developmental disabilities and those who, although community residing, were receiving significant nursing care.
All interviews were computer assisted and offered in English or Spanish at the preference of each participant. Interviewers, two thirds of whom were bilingual, all held bachelor degrees. Although many had prior field interviewing experience, all received extensive training on interviewing techniques, on the responsible conduct of research, and on the process of obtaining truly informed consent from participants. Signed consent was obtained prior to each interview and following detailed coverage of each topic addressed within the consent form, including the fact that a Certificate of Confidentiality had been obtained from the federal government assuring the confidentiality of reports of illegal behavior.
A total of 1,986 interviews were completed in 2004 (a success rate of 82%), including 1,086 adults who screened as having no activity limitations and 900 individuals who screened as having a disability. Of the 900 who, within the screening process, were reported by a family member as having activity limitations, only 559 confirmed this status within the face-to-face interview that followed. The oversampling of individuals with physical disabilities produced a greater proportion of older individuals in this sample than in the general population. Respondent ages in the sample ranged from 18 to 93 with a median of 59.
For the purposes of the present study, we limit the sample to adults 60 years of age and older. We chose this age cut-off point because it has been employed in previous research (Dean et al., 1992) and allowed us to retain approximately half of the original sample. Of the 968 respondents who met this age criterion, 947 (97.8%) reported complete data on all study variables. An analysis of respondents with missing data (n = 21) revealed that the majority did not have information on race/ethnicity (n = 14) and were less likely to be female compared with those with complete data (33% compared with 54%, p = .054). Respondents with incomplete or missing data on any of the study variables are excluded from the analysis.
Measures
Depressive Symptoms.—
Level of depression is assessed with 20 items from the Center for Epidemiologic Studies Depression scale (CES-D). The CES-D scale is a widely used and highly reliable index of depressive symptoms (Radloff, 1977). Our measure differed from the original in addressing experiences over the preceding month rather than the preceding week and by employing response categories of “not at all,” “occasionally,” “frequently,” and “almost all the time.” The use of a 1-month time frame provides a larger sample of recent experience and may reduce the possible influence of short-term mood variations on responses. A scale (alpha = .89) was created by summing responses to each of the 20 questions. Descriptive statistics for this measure as well as all other study variables are presented in Table 1.
Table 1.
Descriptive Statistics for All Study Variables (n = 947)
| Study variables | Means and proportions | SD | Range (min, max) |
| Dependent variable | |||
| Depressive symptoms | 10.14 | 8.82 | 0, 46 |
| Living arrangements | |||
| Living alone | 0.36 | 0, 1 | |
| Living with partner/spouse | 0.43 | 0, 1 | |
| Living with children/others | 0.21 | 0, 1 | |
| Study covariates | |||
| Hispanic | 0.38 | 0, 1 | |
| Female | 0.54 | 0, 1 | |
| Physical disability | 0.34 | 0, 1 | |
| Age | 72.26 | 7.69 | 60, 93 |
| Socioeconomic status | 0.00 | 1.00 | −2.13, 2.70 |
| Never married | 0.04 | 0, 1 | |
| Widowed | 0.29 | 0, 1 | |
| Recent life events | 0.00 | 1.00 | −.64, 3.34 |
| Social support | 0.01 | 0.76 | −3.42, .76 |
Living Arrangements.—
The living arrangements of respondents were determined from the household roster section of the study questionnaire. Respondents were asked to give the age, sex, and relationship of each individual living in the household with them. From this information, we distinguished between three different living arrangements: living alone (n = 337), living with a spouse or partner (n = 410), and living with children, extended family members, or unrelated others (n = 200). We recognize that treating “living alone” as a single category obscures potential disparities in depression between older adults who have lived alone for different lengths of time and who vary in their level of adjustment to living alone. However, a series of sensitivity analyses revealed no differences in the results when the living alone measure was collapsed into separate groups distinguishing between those who have presumably lived alone for different lengths of time (e.g., never married, recently widowed), suggesting that the duration of time living alone is not an important predictor of depressive symptoms in this sample. Further, we chose to combine older adults living with children (n = 127) with those living with relatives or unrelated others (n = 73), as preliminary analyses revealed no significant difference in depressive symptoms between these two groups.
Gender.—
A dichotomous measure of gender is employed that distinguishes women (n = 519) from men (reference category, n = 428).
Physical Disability.—
During the face-to-face interview, study participants were asked: “Do you have a physical or health problem that limits or interferes with the amount or kind of day to day work or recreational activities you can engage in?” Consistent with the operational definition employed in most prior research, the criterion for physical disability status is based on respondent self-reports. Those who self-identified as disabled (n = 323) are compared with nondisabled adults (the reference category, n = 624) in all analyses.
Social Support.—
Because evidence suggests its primary significance for health outcomes (Turner & Marino, 1994; Turner & Turner, 1999), we focus on perceived social support. Our selection of measures for this domain recognizes three relatively distinct sources: spouse/partner (six items, alpha = .88), relatives or other family members (eight items, alpha = .89), and friends (eight items, alpha = .95). Examples of these items include “I feel very close to my husband/wife/partner,” “You have family who would always take the time to talk over your problems, should you want to,” and “You feel that your friends really care about you.” The response categories for all items, in order from high to low, included “very true for you,” “moderately true for you,” “somewhat true for you,” and “not at all true for you.” To simplify analyses, a single measure of perceived social support was constructed by standardizing scores on each dimension (with a mean value of 0 and SD of 1), summing the scores, and dividing by the number of sources on which each participant reported information. An alternative method would be to sum the three separate standardized scores, assigning individuals with missing data a value of “0” for that particular source of support. We contrasted results obtained using these alternative measurement strategies and found no observable differences.
Sociodemographic Controls.—
We control for several demographic factors that are likely to influence depressive symptoms among older adults. Age is coded in years. Socioeconomic status was estimated using a composite score based on household income level, occupational category (Hollingshead, 1957), and educational attainment. In total, 181 respondents (19%) were missing data on income and 49 respondents did not report information on their occupation history (5%). All respondents reported complete data on educational attainment. Scores on the three status dimensions were standardized with a mean of 0 and an SD of 1, summed, and divided by the number of status dimensions for which data were available We also include controls for whether respondents are widowed (yes = 1, n = 281) or have never been married (yes = 1, n = 42).
Recent Life Events.—
Exposure to life events occurring over the 12 months preceding the interview was assessed with a 23-item inventory that considered events happening to significant others as well as to the respondent (Turner & Avison, 2003; Turner & Lloyd, 1999). Examples of these events include the onset of a serious illness, spousal/partner loss, accident/injury, and financial crisis. Positive responses to these items were summed and standardized with a mean of 0 and SD of 1. Higher scores reflect greater exposure to life events.
Race/Ethnicity.—
Scholars have called for greater clarity in the use of race and ethnicity as variables in health research, especially when the analysis involves treating race and ethnicity as separate, overlapping constructs (Bhopal & Donaldson, 1998; Senior & Bhopal, 1994). In the present study, we are primarily interested in the moderating role of Hispanic ethnicity in the relationship between living alone and depressive symptoms. As such, we distinguish between Hispanics (n = 362) and non-Hispanics (n = 585) in all descriptive and multivariate analyses. Non-Hispanics include those who self-identified as African American (n = 313) and non-Hispanic White (n = 272). Preliminary analyses revealed that Black and White variations in depressive symptoms across living arrangements were more similar than dissimilar and each sharply contrasted with the pattern of findings observed among Hispanics. We believed that these preliminary findings necessitated analyses stratified by Hispanic ethnicity. A control for racial differences in depressive symptoms (African American = 1) is included in the multivariate analyses among non-Hispanics. Although we considered including a control for race in the Hispanic sample, we were only able to identify one individual who self-identified as a Hispanic of African descent. The relatively small number of African Americans in this sample who reported Hispanic ethnicity is consistent with the 2006 population estimates for Miami-Dade County (see Table B03002; U.S. Census Bureau). Thus, the multivariate analyses limited to Hispanics do not include a control for race.
Analytic Strategy
As mentioned previously, we decided to stratify all analyses by Hispanic ethnicity based on preliminary findings and present separate results for Hispanics and non-Hispanics. We divide the analysis into two components. A first set of descriptive analyses reports mean levels of depressive symptoms across living arrangements, gender, physical disability, and social support (high social support ≥75th percentile). The t-test and one-way analysis of variance are employed to detect significant social group differences in depressive symptoms within and across living arrangements. A second set of analyses presents multivariate results examining the hypothesized mediating and moderating effects. A first equation includes categorical indicators for living alone and living with others (living with spouse or partner is the reference category) and controls for social characteristics and exposure to recent life events. The second equation includes interaction terms between living arrangements, gender, and physical disability. The third model controls for social support. A final equation includes interaction terms between living arrangements and social support. Post hoc equality tests (Paternoster et al., 1998) are employed to identify significant differences between coefficients in the non-Hispanic and Hispanic regression models. More specifically, we examine whether the magnitude of the association between living arrangements and depressive symptoms, as well as the interaction with social support, is equivalent across the Hispanic and non-Hispanic subgroups.
RESULTS
The results of descriptive analyses examining variations in depression across living arrangements are presented in Table 2. The first row of these results indicates that mean levels of depressive symptoms vary substantially by Hispanic ethnicity. In general, Hispanics report higher levels of depression than non-Hispanics. The relative difference is much greater for Hispanics living alone, who differ significantly from non-Hispanics living alone and Hispanics who live with their spouse/partner or others. This pattern of findings is especially pronounced among Hispanic men. Older Hispanic men who live alone report higher levels of psychological distress than Hispanic men living with their spouse/partner or with children/others. In contrast to our expectations, the gender difference in depressive symptoms among Hispanics living alone is not statistically significant. However, these findings suggest that physically disabled older adults living alone tend to report higher levels of depression than those without a physical limitation. Interestingly, the difference in level of depression between those with and without a physical disability is only statistically significant among individuals who live alone. In addition to physical disability, mean depression scores also differ by the level of perceived social support. Older adults living alone who view their family and friends as less supportive report significantly higher levels of depression than those living alone who perceive their social networks as more supportive. The relative magnitude of this contrast is greatest among Hispanics living alone; however, the difference is also significant among non-Hispanics within all three living arrangements.
Table 2.
Mean Levels of Depressive Symptoms Across Living Arrangements by Hispanic Ethnicity
| Hispanics |
Non-Hispanics |
|||||
| Living Alone | Living with Partner | Living with Others | Living Alone | Living with Partner | Living with Others | |
| Total sample | 15.950a,b | 12.966b | 12.378b | 8.261 | 7.246 | 8.199 |
| (10.619, 130) | (10.544, 158) | (9.147, 74) | (6.241, 207) | (6.934, 252) | (7.040, 126) | |
| Gender | ||||||
| Male | 17.871a,b | 12.114b | 11.970 | 8.321 | 6.752 | 8.167 |
| (11.580, 37) | (10.137, 100) | (9.159, 18) | (7.136, 70) | (6.341, 176) | (6.803, 27) | |
| Female | 15.186b | 14.435b | 12.509b | 8.230 | 8.389 | 8.207 |
| (10.177, 93) | (11.149, 58) | (9.222, 56) | (5.758, 137) | (8.074, 76) | (7.137, 99) | |
| Physical disability | ||||||
| Physically disabled | 19.952a,b,c | 14.596b | 14.185b | 10.136c | 8.344 | 9.827 |
| (11.335, 40) | (10.105, 54) | (8.866, 27) | (7.158, 77) | (7.280, 83) | (8.644, 42) | |
| Nondisabled | 14.172b | 12.120b | 11.340b | 7.151 | 6.706 | 7.385 |
| (9.836, 90) | (10.716, 104) | (9.237, 47) | (5.354, 130) | (6.713, 169) | (5.977, 84) | |
| Social support | ||||||
| Higher social supporte | 10.033b,d | 9.292b | 9.626b | 6.953a,d | 5.173d | 5.642d |
| (6.588, 30) | (8.994, 23) | (6.949, 20) | (4.871, 65) | (4.194, 66) | (4.979, 51) | |
| Lower social support | 17.726a,b | 13.592b | 13.397b | 8.859 | 7.981 | 9.938 |
| (10.974, 100) | (10.690, 135) | (9.696, 54) | (6.707, 142) | (7.548, 186) | (7.708, 75) | |
Notes: Values in parentheses are (SD, cell size).
Significant contrast (p < .05) in depressive symptoms across living arrangements.
Significant contrast (p < .05) in depressive symptoms across Hispanic ethnicity.
Significant contrast (p < .05) in depressive symptoms across physical disability.
Significant contrast (p < .05) in depressive symptoms across level of social support.
Higher social support ≥75th percentile.
Separate multivariate models for Hispanics (n = 362) and non-Hispanics (n = 585) are presented in Tables 3 and 4, respectively. These tables, which report the results of ordinary least squares regression analyses, address the issue of whether the hypothesized individual and social characteristics mediate and/or moderate the association between living alone and depressive symptoms. The first equation (Model 1, Table 3) assesses this relationship while controlling for gender, physical disability, age, marital history (never married, widowed), socioeconomic status, and exposure to recent life events. Model 1 indicates that Hispanics living alone report significantly higher levels of depression relative to Hispanics living with their spouse/partner net of individual and social characteristics. This finding suggests that living alone is an independent risk factor for psychological distress among older Hispanic adults. Additional analyses (not shown) confirmed that the difference in depressive symptoms between Hispanics living alone and Hispanics living with others is also significant at the p < .01 level.
Table 3.
Depressive Symptoms Regressed on Living Arrangements and Covariates (Hispanics)
| Study Variables | 1 | 2 | 3 | 4 |
| Living arrangements | ||||
| Living alonea | 3.331* (1.416) | 5.424* (2.136) | 4.529* (1.927) | 5.039* (1.942) |
| Living with children/others | −0.924 (1.638) | −1.763 (3.070) | −3.456 (2.772) | −2.427 (2.809) |
| Covariates | ||||
| Female | 0.353 (1.159) | 2.045 (1.666) | 1.948 (1.501) | 1.867 (1.492) |
| Physical disability | 3.337** (1.141) | 2.389 (1.695) | 2.190 (1.527) | 2.168 (1.517) |
| Social support | −5.115*** (0.565) | −6.857*** (0.909) | ||
| Age | −0.057 (0.078) | −0.062 (0.079) | −0.041 (0.071) | −0.062 (0.071) |
| Socioeconomic status | −1.059† (0.553) | −1.043† (0.555) | −1.054* (0.499) | −1.241* (0.502) |
| Never married | −1.335 (2.280) | −1.477 (2.287) | −.195 (2.065) | −.292 (2.053) |
| Widowed | −.558 (1.535) | −.274 (1.549) | −.663 (1.396) | −.283 (1.407) |
| Recent life events | 1.504** (0.563) | 1.495** (0.563) | 1.816*** (0.508) | 1.840*** (0.506) |
| Interaction terms | ||||
| Female × Living alone | −5.169* (2.600) | −3.721 (2.347) | −3.912 (2.335) | |
| Female × Living with others | 0.005 (3.286) | 2.947 (2.978) | 2.064 (3.030) | |
| Disabled × Living alone | 3.007 (2.567) | 2.135 (2.314) | 2.256 (2.302) | |
| Disabled × Living with others | 0.259 (3.054) | 0.160 (2.751) | 0.179 (2.734) | |
| Support × Living alone | 2.515* (1.268) | |||
| Support × Living with otherst | 3.545* (1.567) | |||
| Constant | 15.439 | 15.474 | 13.153 | 14.285 |
| R2 | .079 | .095 | .268 | .281 |
| n | 362 | 362 | 362 | 362 |
Notes: Unstandardized ordinary least square regression coefficients (standard errors).
Reference category is older adults living with their partner/spouse.
*p < .05; **p < .01; ***p < .001; †p < .10.
Table 4.
Depressive Symptoms Regressed on Living Arrangements and Covariates (Non-Hispanics)
| Study Variables | 1 | 2 | 3 | 4 |
| Living arrangements | ||||
| Living alonea | 0.164 (0.768) | 0.527 (1.079) | −0.319 (1.058) | −0.242 (1.058) |
| Living with children/others | 0.532 (0.890) | 0.871 (1.480) | 0.833 (1.437) | 1.302 (1.458) |
| Covariates | ||||
| Female | 0.282 (0.607) | 1.256 (0.900) | 1.244 (0.874) | 1.265 (0.872) |
| Physical disability | 2.269*** (0.578) | 1.599† (0.887) | 1.416 (0.862) | 1.350 (0.861) |
| Social support | −2.349*** (0.396) | −3.306*** (0.717) | ||
| Age | −0.006 (0.040) | −0.001 (0.040) | 0.001 (0.039) | 0.007 (0.039) |
| Socioeconomic status | −0.650* (0.325) | −0.674* (0.326) | −0.601† (0.317) | −0.521 (0.318) |
| Never married | 2.208 (1.647) | 2.135 (1.655) | 2.499 (1.609) | 2.193 (1.610) |
| Widowed | 0.449 (0.790) | 0.494 (0.794) | 0.876 (0.774) | 0.709 (0.775) |
| Recent life events | 1.278*** (0.265) | 1.285*** (0.266) | 1.203*** (0.258) | 1.133*** (0.259) |
| African American | −1.850** (0.644) | −1.838** (0.646) | −1.509* (0.630) | −1.283* (0.638) |
| Interaction terms | ||||
| Female × Living alone | −1.897 (1.317) | −0.986 (1.288) | −1.345 (1.293) | |
| Female × Living with others | −1.324 (1.693) | −1.515 (1.645) | −1.594 (1.640) | |
| Disabled × Living alone | 1.417 (1.284) | 0.972 (1.249) | 1.305 (1.253) | |
| Disabled × Living with others | 0.580 (1.525) | 0.938 (1.483) | 1.055 (1.479) | |
| Support × Living alone | 1.923* (.916) | |||
| Support × Living with others | .003 (1.135) | |||
| Constant | 7.857 | 7.471 | 7.472 | 6.970 |
| R2 | .084 | .089 | .142 | .151 |
| n | 585 | 585 | 585 | 585 |
Notes: Unstandardized ordinary least square regression coefficients (standard errors).
Reference category is older adults living with their partner/spouse.
*p < .05; **p < .01; ***p < .001; †p < .10.
Model 2 includes four interaction terms between the two living arrangement categories and gender and physical disability. These results reveal that living alone is significantly more distressing for Hispanic men relative to Hispanic women, suggesting that the protective benefits of living with a spouse or partner are greater for Hispanic men. The interaction term coefficient for disability status is in the expected direction but does not approach a level of statistical significance (p = .242), lending limited support for our hypothesis that the presence of a physical limitation modifies the effect of living alone on psychological distress.
The issue of whether variations in psychological distress across living arrangements are independent of social support is addressed in Model 3. When social support is entered into this equation, the interaction coefficient between gender and living alone is partly explained and reduced to a level of statistical insignificance. Approximately 28%, (−5.169 − [−3.721]/−5.169 = .280), of this moderation effect is mediated through variations in social support across gender and living arrangements. Additional analyses (not shown) reveal that Hispanic women living alone report higher levels of social support than men in the same living situation, suggesting that Hispanic women's higher perceptions of support from family and friends avert them from experiencing levels of depression similar to Hispanic men. Support for the moderating effect of social support on living alone is found in Model 4. The interaction term between social support and living alone (as well as the interaction term for the comparison category) is positive and significant, indicating that the protective effect of social support is greater for Hispanics who live with their spouse or partner compared with Hispanics living alone (and those living with others).
Parallel regression analyses were conducted among non-Hispanics and are presented in Table 4. In contrast to the pattern of findings observed among Hispanics (yet consistent with the descriptive results), living alone is not a significant independent risk factor for depressive symptoms. The magnitude of living alone and depressive symptoms relationship is significantly greater (z = 4.38, p < .001) for Hispanics, indicating that ethnicity is an important modifier of this association. One consistency across the Hispanic and non-Hispanic multivariate results is the significant interaction effect between social support and living alone. Similar to the Hispanic subsample, social support is more protective against depression among non-Hispanics living with a spouse or partner than for those who live alone (equation 4).
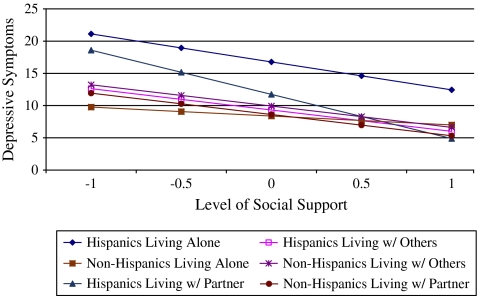
In an effort to better understand how this conditional relationship affects levels of psychological distress among Hispanic and non-Hispanic older adults, we present predicted depression scores across social support values by living arrangements and ethnicity in Figure 1. Among those who perceive family and friends as relatively supportive, Hispanics living alone report the highest levels of depression. At lower levels of social support, Hispanics living alone report similar levels of depression compared with Hispanics living with their spouse or partner. The importance of social support for depression among Hispanic study participants is also demonstrated by the difference in R2 values across the Hispanic and non-Hispanic samples. The amount of variance accounted for in the final Hispanic model (R2 = .281) is nearly twice as high as that of the non-Hispanic model (R2 = .151). Much of this difference is attributable to ethnic variations in the simple main effects of social support, which are significantly more protective against depressive symptoms among Hispanics than among non-Hispanics (z = 16.20, p < .001).
Figure 1.
Predicted depression scores across level of social support by living arrangements and Hispanic ethnicity. These predicted scores are computed based on the regression coefficients presented in Model 4 (Tables 3 and 4). With the exception of living arrangements, social support, and Hispanic ethnicity, mean values are imputed for each of the independent variables in this equation.
DISCUSSION
In the present study, we reexamined the association between living alone and depressive symptoms among a sample of Hispanic and non-Hispanic older adults. We extended previous research by focusing on whether gender, physical disability, social support, and Hispanic ethnicity modify the influence of living alone on mental health. One of the more robust social status contingencies identified in this study was the elevated levels of depression observed among Hispanics living alone. This finding is consistent with the results of one previous study (Hays & George, 2002) and suggests that Hispanic ethnicity moderates the influence of living alone on depression. This finding may be attributable to cultural variations in the strength of family ties and preference for living with kin (Burr & Mutchler, 1993; Himes, Hogan, & Eggebeen, 1996; Wilmoth, 2001). The higher levels of depressive symptoms observed among Hispanics who live alone may reflect dissatisfaction with their current household arrangement and/or an unmet desire for increased family closeness. Although perceptions of emotional support from family and friends are more negatively associated with depressive symptoms among Hispanics than non-Hispanics (i.e., a larger simple main effect), our results suggest that social support plays an important moderating role in the relationship between living arrangements and depression among both ethnic groups. We find that perceptions of social support are less protective against experiences of depression among older adults living alone compared with their counterparts who live with a spouse or partner.
The nativity distribution of the Hispanic subsample limits our ability to generalize these findings to U.S.-born Hispanics because 99% (358 of 362) of the Hispanics in our sample were not born in the United States. Hispanic immigrants living alone may experience greater difficulty with this living arrangement due to language and cultural barriers that limit community integration and activities outside the household. Prior research suggests that these potential obstacles may vary by immigrant generation and length of time in the United States. For instance, Mills and Henretta (2001) find that level of acculturation distinguishes those most at risk for experiencing symptoms of depression. In additional analyses (not shown), we examined whether time in the United States accounted for the association between living alone and depressive symptoms observed among Hispanics. Results indicated that this was not the case. Time in the United States was not associated with depression, net of other social characteristics, and did not explain the relationship between living alone and depressive symptoms. Further, we recognize that the Hispanics in our sample are not a homogenous group in terms of national origin. The three largest groups in the Hispanic sample were of Cuban, Colombian, and Nicaraguan descent. Analyses (not shown) revealed that variations in depressive symptoms across living arrangements were very similar for all Hispanics, regardless of their nationality. These results led us to the decision to combine all Hispanic study participants into a single ethnic category. Based upon these observations, we are confident that the findings presented here generalize to Hispanics in South Florida, but we are much less confident that they extend to Hispanic populations residing in different geographical regions. Additional research is needed to assess whether the pattern of findings presented here extend to Hispanics residing in other regions of the country and to untangle the influence of nativity status on variations in depression across different living arrangements.
Earlier investigations have shown that men living alone are more depressed than their female counterparts (Dean et al., 1992; Hughes & Waite, 2002; Jeon et al., 2007). Multivariate analyses revealed that living alone was significantly more distressing for Hispanic men relative to Hispanic women. However, variations in perceived social support partially explained the moderating effect of gender on living alone, suggesting that differences in the level of perceived social support between Hispanic men and women underlie this conditional relationship. These results differ from those of Dean et al., who found that the greater psychological distress observed among men living alone was independent of emotional support. This inconsistency may be attributable to differences between the measure of social support employed in our study and that of the study of Dean et al., which limited their assessment of support to the respondent's friends. Our analyses suggest that perceptions of support from one's relatives and spouse/partner may be equally, if not more, important in protecting against depression in older adulthood.
We received limited empirical support for our hypothesis that living alone is more detrimental to the psychological well-being of older adults with a physical disability. Although descriptive results indicated that Hispanics with a physical limitation who live alone reported higher levels of depression than their nondisabled counterparts, the interaction between physical disability and living alone was not significant in multivariate models with controls for demographic characteristics and exposure to recent life events. One potential explanation for this finding is that the physically disabled who live alone are healthier, have fewer activity limitations, and are better able to deal with the day-to-day challenges associated with living alone compared with disabled persons living with others. To support this positive selection hypothesis, one would need to observe more health problems and activity limitations among the disabled group living with others compared with the disabled group living alone. In analyses not shown (available upon request), we compared the level of health problems and activity limitations between these two groups and found that there were no differences in either of these indicators across living arrangements. These additional analyses suggest that disabled persons living alone have similar levels of physical limitation as those who live with others. An additional potential explanation is that the physically disabled may receive assistance with household tasks and labor from others who live outside the household, thus allowing them to better cope with their living situation. This possibility remains to be examined by future research.
One important limitation of our study is the cross-sectional design. Ideally, we would have examined changes in psychological well-being as people remain in, move out of, and move into different living arrangements over time. An important topic for future research is the mental health impact of these transitions. For example, transitions into living alone, such as after the death of a spouse, are likely to be associated with decreases in social support and greater vulnerability to stressors, such as financial strains and household management difficulties (Umberson, Wortman, & Kessler, 1992). Transitions into living alone may have different implications for the mental health of older men and women. There is some evidence to suggest that women cope with, and adapt to, independent living more favorably than their male counterparts (Van Grootheest, Beekman, Broese Van Groenou, & Deeg, 1999). Although the data analyzed here were limited to Wave 1 of a two-wave panel study, there was not enough change in living arrangements among study participants across waves of data collection to make these longitudinal analyses meaningful.
Future research should also consider how selection processes influence the results of this study. Social selection explanations emphasize the role of individual personality characteristics, predispositions, and psychological pathology in conditioning status differences in mental health. From this perspective, adults with a history of physical and mental health problems and low socioeconomic resources are, by virtue of these challenges, more likely to be selected into situations where they live alone. Few studies have addressed this possibility with direct empirical tests (Umberson & Williams, 1999).
CONCLUSION
Recent demographic and social changes have provided impetus for additional research that examines the implications of living alone for individual psychological distress. The results from this study indicate that living alone independently contributes to depression, although certain social groups are more adversely affected by this living arrangement than others. Hispanics living alone experienced the highest levels of depression relative to African American and non-Hispanic White respondents. This contingency was independent of social support, and a range of other important characteristics may reflect certain cultural or social disadvantages of independent living experienced by immigrants and minority elders. The results of this study suggest that cultural differences in the desirability of living with others place some ethnic groups at elevated risk for psychological distress. Further, our findings support policy interventions designed to emphasize the role of families in alleviating emotional distress among older adults living alone (Rook, 1984).
FUNDING
This study was supported by two research grants (DA16429-01 and 5 R01 DA 10772-03) from the National Institute of Drug Abuse awarded to R. Jay Turner as well as by a Postdoctoral Fellowship from the National Institute of Mental Health awarded to D.R.
Acknowledgments
The authors also thank Amy Blank, Deborah Carr, Aparna Kalbag, David Mechanic, Jennifer Tanner, and three anonymous reviewers for their helpful comments on an earlier version of this paper. D.R. planned the study, conducted all data analyses, and wrote the paper. J.T. contributed suggestions for, and assistance with, revising the manuscript.
References
- Adams KB, Sanders S, Auth EA. Loneliness and depression in independent living retirement communities: Risk and resilience factors. Aging & Mental Health. 2004;8:475–485. doi: 10.1080/13607860410001725054. [DOI] [PubMed] [Google Scholar]
- Alwin DF, Converse PE, Martin SS. Living arrangements and social integration. Journal of Marriage and the Family. 1985;47:319–334. [Google Scholar]
- Barrett AE. Social support and life satisfaction among the never married. Research on Aging. 1999;21:46–72. [Google Scholar]
- Bhopal R, Donaldson L. White, European, Western, Caucasian, or what? Inappropriate labeling in research on race, ethnicity, and health. American Journal of Public Health. 1998;88:1303–1307. doi: 10.2105/ajph.88.9.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burr J, Mutchler JE. Ethnic living arrangements: Cultural convergence or cultural manifestation. Social Forces. 1993;72:169–179. [Google Scholar]
- Carnelley KB, Wortman CB, Kessler RC. The impact of widowhood on depression: Findings from a prospective study. Psychological Medicine. 1999;29:1111–1123. doi: 10.1017/s0033291799008971. [DOI] [PubMed] [Google Scholar]
- Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. American Journal of Psychiatry. 2003;160:1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- Dean A, Kolody B, Wood P, Matt GE. The influence of living alone on depression in elderly persons. Journal of Aging and Health. 1992;4:3–18. [Google Scholar]
- Fields J. America's families and living arrangements: 2003. Current population reports: P20-553. Washington, DC: U.S. Census Bureau; 2004. [Google Scholar]
- Glick PC. Living alone during middle adulthood. Sociological Perspectives. 1994;37:445–457. [Google Scholar]
- Hays JC, George LK. The life-course trajectory toward living alone. Research on Aging. 2002;24:283–307. [Google Scholar]
- Himes CL, Hogan DP, Eggebeen DJ. Living arrangements of minority elders. Journals of Gerontology: Social Sciences. 1996;51B:S42–S48. doi: 10.1093/geronb/51b.1.s42. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Two factor index of social position. New Haven, CT: Hollingshead; 1957. [Google Scholar]
- Hughes M, Gove WR. Living alone, social integration, and mental health. American Journal of Sociology. 1981;87:48–74. doi: 10.1086/227419. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ. Health in household context: Living arrangements and health in late middle age. Journal of Health and Social Behavior. 2002;43:1–21. [PMC free article] [PubMed] [Google Scholar]
- Jeon GS, Jang SN, Rhee SJ, Kawachi I, Cho SI. Gender differences in correlates of mental health among elderly Koreans. Journals of Gerontology: Social Sciences. 2007;62B:S323–S329. doi: 10.1093/geronb/62.5.s323. [DOI] [PubMed] [Google Scholar]
- Joutsenniemi K, Martelin T, Martikainen P, Pirkola S, Koskinen S. Living arrangements and mental health in Finland. Journal of Epidemiology and Community Health. 2006;60:468–475. doi: 10.1136/jech.2005.040741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinenberg E. Dying alone: The social production of urban isolation. Ethnography. 2001;2:501–531. [Google Scholar]
- Michael YL, Berkman LF, Colditz GA, Kawachi I. Living arrangements, social integration, and change in functional health status. American Journal of Epidemiology. 2001;153:123–131. doi: 10.1093/aje/153.2.123. [DOI] [PubMed] [Google Scholar]
- Mills TL, Henretta JC. Racial, ethnic, and sociodemographic differences in the level of psychosocial distress among older Americans. Research on Aging. 2001;23:131–152. [Google Scholar]
- Ng KM, Lee T, Chi I. Relationship between living arrangements and the psychological well-being of older people in Hong Kong. American Journal on Ageing. 2004;23:167–171. [Google Scholar]
- Osborn DPJ, Fletcher AE, Smeeth L, Stirling S, Bulpitt CJ, Breeze E, Ng E, Nunes M, Jones D, Tulloch A. Factors associated with depression in a representative sample of 14,217 people aged 75 and over in the United Kingdom: Results from the MRC trial of assessment and management of older people in the community. International Journal of Geriatric Psychiatry. 2003;18:623–630. doi: 10.1002/gps.896. [DOI] [PubMed] [Google Scholar]
- Paternoster R, Brame R, Mazerolle P, Piquero A. Using the correct statistical test for the equality of regression coefficients. Criminology. 1998;36:859–866. [Google Scholar]
- Radloff LS. The CES-D scale: A new self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ramos M, Wilmoth J. Social relationships and depressive symptoms among older adults in Southern Brazil. Journals of Gerontology: Social Sciences. 2003;58B:S253–S261. doi: 10.1093/geronb/58.4.s253. [DOI] [PubMed] [Google Scholar]
- Reissman CK. Divorce talk: Women and men make sense of personal relationships. New Brunswick, NJ: Rutgers University Press; 1990. [Google Scholar]
- Rogers RG. The effects of family composition, health, and social support linkages on mortality. Journal of Health and Social Behavior. 1996;37:326–338. [PubMed] [Google Scholar]
- Rook K. Promoting social bonding: Strategies for helping the lonely and socially isolated. American Psychologist. 1984;39:1389–1407. [Google Scholar]
- Ross CE. Re-conceptualizing marital status as a continuum of social attachment. Journal of Marriage and the Family. 1995;57:129–140. [Google Scholar]
- Ross CE, Mirowsky J, Cockerham WC. Social class, Mexican culture, and fatalism: Their effects on psychological distress. American Journal of Community Psychology. 1983;11:383–399. doi: 10.1007/BF00894055. [DOI] [PubMed] [Google Scholar]
- Saluter AF. Marital status and living arrangements. Current population reports: P20-484. Washington, DC: U.S. Census Bureau; 1994. [Google Scholar]
- Sarason BR, Sarason IG. Ongoing aspects of relationships and health outcomes: Social support, social control, companionship, and relationship meaning. In: Harvey J, Wenzel A, editors. Close romantic relationships: Maintenance and enhancement. Mahwah, NJ: Lawrence Erlbaum; 2001. pp. 277–298. [Google Scholar]
- Schieman S. Age and anger. Journal of Health and Social Behavior. 1999;40:273–289. [PubMed] [Google Scholar]
- Senior PA, Bhopal R. Ethnicity as a variable in epidemiological research. British Medical Journal. 1994;309:327–330. doi: 10.1136/bmj.309.6950.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The effect of the living situation on the severity of dementia at diagnosis. Dementia and Geriatric Cognitive Disorders. 2002;13:40–45. doi: 10.1159/000048632. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Avison WR. Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior. 2003;44:488–505. [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. The stress process and the social distribution of depression. Journal of Health and Social Behavior. 1999;40:374–404. [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA, Taylor J. Physical disability and mental health: An epidemiology of psychiatric and substance disorders. Rehabilitation Psychology. 2006;51:214–223. [Google Scholar]
- Turner RJ, Marino F. Social support and social structure: A descriptive epidemiology. Journal of Health and Social Behavior. 1994;35:193–212. [PubMed] [Google Scholar]
- Turner RJ, Noh S. Physical disability and depression: A longitudinal analysis. Journal of Health and Social Behavior. 1988;29:23–27. [PubMed] [Google Scholar]
- Turner RJ, Turner JB. Social integration and support. In: Aneshensel CS, Phelan JC, editors. Handbook of the sociology of mental health. New York: Springer; 1999. pp. 301–319. [Google Scholar]
- Umberson D, Williams K. Family status and mental health. In: Aneshensel CS, Phelan JC, editors. Handbook of the sociology of mental health. New York: Springer; 1999. pp. 225–253. [Google Scholar]
- Umberson D, Wortman CB, Kessler RC. Widowhood and depression: Explaining long-term gender differences in vulnerability. Journal of Health and Social Behavior. 1992;33:10–24. [PubMed] [Google Scholar]
- Van Gelder BM, Tijhuis M, Kalmijn S, Giampaoli S, Nissinen A, Kromhout D. Marital status and living situation during a 5-year period are associated with a subsequent 10-year cognitive decline in older men: The FINE study. Journals of Gerontology: Psychological Sciences. 2006;61B:P213–P219. doi: 10.1093/geronb/61.4.p213. [DOI] [PubMed] [Google Scholar]
- Van Grootheest DS, Beekman ATF, Broese Van Groenou MI, Deeg DJH. Sex differences in depression after widowhood: Do men suffer more. Social Psychiatry and Psychiatric Epidemiology. 1999;34:391–398. doi: 10.1007/s001270050160. [DOI] [PubMed] [Google Scholar]
- Victor C, Scambler SJ, Bond J, Bowling A. Being alone in later life: Loneliness, social isolation, and living alone. Reviews in Clinical Gerontology. 2000;10:407–417. [Google Scholar]
- Waite LJ, Hughes ME. At risk at the cusp of old age: Living arrangements and functional status among black, white, and Hispanic adults. Journals of Gerontology: Social Sciences. 1999;54B:S136–S144. doi: 10.1093/geronb/54b.3.s136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmoth JM. Living arrangements among older immigrants in the United States. The Gerontologist. 2001;41:228–238. doi: 10.1093/geront/41.2.228. [DOI] [PubMed] [Google Scholar]
- Yeh SJ, Lo SK. Living alone, social support, and feeling lonely among the elderly. Social Behavior and Personality. 2004;32:129–138. [Google Scholar]