Abstract
Background
The health pessimism hypothesis suggests that Black elders are more pessimistic about health than Whites and therefore tend to report lower self-rated health (SRH) at comparable health status. The current analysis examined the factors associated with SRH and tested the health pessimism hypothesis among older adults at similar levels of physical functioning.
Methods
The study example included 2,729 Health, Aging, and Body Composition study participants aged 70–79 years. We used hierarchical logistic regression to examine the association between race and SRH while adjusting for demographic, physical health, and psychosocial factors. The analyses were repeated for participants at similar levels of objective functioning to test the health pessimism hypothesis.
Results
The association between race and SRH remained independent of physical and psychosocial health variables, with Whites being 3.7 times more likely than Black elders to report favorable SRH. This association was significant at each level of physical functioning and greater at the higher (odds ratio [OR] = 5.5) versus lower (OR = 2.2) levels of functioning.
Conclusions
The results suggest greater health pessimism among Black elders and expand previous work by including objective functioning in multidimensional models to deconstruct race variations in the SRH of older adults.
Keywords: Self-rated health, Health pessimism, Objective measures, Physical functioning
ELIMINATING health disparities is a major goal of Healthy People 2010, and understanding racial differences in health is a critical step in reaching this goal (Dressler, Oths, & Gravlee, 2005). For more than 50 years, self-rated health (SRH) has been one of the most widely used measures for assessing health disparities (see review by Ferraro, 1993). It is typically measured with a single item asking respondents to rate their health on a 5-point Likert-type scale. SRH is a consistent predictor of mortality independent of medical, behavioral, and psychosocial factors (Benyamini, Blumstein, Lusky, & Modan, 2003; Idler & Benyamini, 1997; Idler, Hudson, & Leventhal, 1999; McGee, Liao, Cao, & Cooper, 1999). In longitudinal analyses of the National Population Health Survey in Canada, Bailis, Segall, and Chipperfield (2003) found that SRH coincided with changes in health status over time. Previous studies also suggest that SRH might be more strongly related to disability than morbidity (Ferraro, 1980), and longitudinal analyses of the SRH–disability association found that these factors might exert a mutual influence on one another (Ferraro, Farmer, & Wybraniec, 1997). Overall, SRH provides researchers in the field of aging with an inexpensive way to characterize health status (Schulz et al., 1994) and because of its predictive utility is an important indicator of overall health in older adulthood.
Racial differences in SRH have been well documented in multiple studies of large, nationally representative samples. According to age- and sex-adjusted estimates from the 2006 National Health Interview Survey, 69.4% of White adults reported excellent or good health compared with 56.4% of Black adults (U.S. Department of Health and Human Services, 2007). Black adults consistently report poorer SRH than White adults even after controlling for a number of sociodemographic and self-reported health correlates (e.g., Borrell & Crawford, 2006; National Center for Health Statistics, 2006; Ren & Amick, 1996). In fact, adjusted models indicate that Black adults are approximately twice as likely as Whites to report fair or poor SRH (Boardman, 2004; Ferraro, 1993).
Two interpretations have been proposed to clarify between-group variations in SRH (Boardman, 2004). The first is “spontaneous assessment,” which suggests that SRH reflects an individual's self-evaluation and is a direct measurement of health status (Bailis et al., 2003). In the context of racial disparities, spontaneous assessment would suggest that poorer SRH among Blacks is a simple and direct indication of poorer health status. However, this does not explain the finding that these differences persist even after controlling for other factors. The second interpretation, “enduring self-concept,” relates more to an individual's health beliefs (Bailis et al., 2003). Enduring self-concept would suggest that Black adults might have different beliefs about health, which might lead to more negative health assessments. These two views of SRH provide researchers with a conceptual framework for understanding racial differences in SRH (Boardman, 2004).
One hypothesis for these differences that was first described by Ferraro (1993) as a way to explain his findings suggests that Black older adults are more pessimistic about health than Whites and therefore tend to evaluate health more negatively. This negative assessment persists even when the health status of Black and White older adults is similar. Boardman (2004) defined this concept of health pessimism as “a notable mismatch between subjective and objective health status” (p. 2523). This hypothesis is consistent with the enduring self-concept interpretation of SRH. However, a limitation of previous work on health pessimism is that the “objective” indicators of health status have typically been based on self-report data, making it difficult to adequately examine the mismatch between objective and subjective health assessments. A second limitation is that few studies consider that the factors which influence health might differ between groups. For example, Whites might consider physical functioning as a more salient factor when defining health than do Black older adults (Krause & Jay, 1994). In addition to these possible cultural differences in SRH assessments, physical functioning is an important quality of life indicator that has not, to our knowledge, been used to test the health pessimism hypothesis.
The 1985 Constitution of the World Health Organization defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” Consistent with this definition, numerous factors must be included in order to adequately deconstruct SRH (Schulz et al., 1994) and explore what factors best explain the observed racial differences. The goal of the current analysis was to examine the role of multiple health indicators, including objective physical functioning, as predictors of SRH in a racially diverse sample of community-dwelling older adults. Physical functioning is a widely accepted indicator of overall physical health status (Newman et al., 2006) and, to our knowledge, has not been examined as it relates to SRH. We tested the health pessimism hypothesis by determining whether racial differences in SRH persisted at similar levels of objective physical functioning, as measured by a multidimensional physical performance battery, after adjusting for known predictors of SRH. We hypothesized that health-related variables would only partially explain racial differences in SRH. We also hypothesized that Black elders would report poorer SRH than Whites with comparable functional status, which might be indicative of greater health pessimism among Black elders.
METHODS
Study Population
The data for this analysis were from the Health, Aging, and Body Composition (Health ABC) study, a prospective cohort study of 3,075 Black and White men and women aged 70–79 years at baseline. Only those participants with complete data on all key variables were included in the current analyses (N = 2,729), with 346 (11.25%) having incomplete data. Health ABC was designed to examine the relationship between changes in body composition and development of functional difficulties in a sample of initially well-functioning older adults. Participants were recruited using designated zip codes in or around Pittsburgh, Pennsylvania, and Memphis, Tennessee, and deemed eligible if they had no difficultly walking one-quarter mile, going up 10 steps without resting, or performing basic activities of daily living. In addition, eligible participants did not need walking aids, reported no history of active treatment of cancer in the prior 3 years, and did not plan on moving out of the area in the next 3 years. All of the Health ABC participants were Medicare recipients living in the designated zip codes. White participants were recruited based on a random sample of Medicare-eligible adults, whereas Black participants were oversampled to ensure a sufficient number by recruiting from 100% of all age-eligible Medicare recipients. The data used in the current analysis were collected during the baseline home interview and clinic assessment, between April 1997 and June 1998.
Measures
SRH, our dependent variable, was assessed with a single item, “How would you rate your overall health?” with response categories of excellent, very good, good, fair, and poor. To ensure sufficient cell sizes, SRH was dichotomized as favorable SRH (excellent + very good + good) versus unfavorable SRH (fair + poor) for the regression analyses. In order to better understand racial variations in SRH, factors known to be associated with SRH were collapsed into conceptual domains and included as potential confounders.
Race was categorized according to the participant's self-identification as Black or White. Three conceptual domains were used to categorize predictor variables, including demographics (four variables), physical health (six variables), and psychosocial factors (three variables). All variables were selected based on their conceptual and statistical associations with SRH, with the goal of limiting the amount of missing data. “Demographic” variables in the first domain included sex (men vs. women), age (continuous variable, measured in years), site (Memphis vs. Pittsburgh), and highest education level (high school graduate vs. less than high school). Income was not included in the analyses due to a large amount of missing data for this variable (n = 316) and because it showed a moderate/high correlation with education (r = .47).
Six variables were included under the “physical health” domain, including our measure of physical functioning, which was selected a priori to examine the health pessimism hypothesis. (1) The Health ABC physical performance battery (PPB) is an objective, composite score based on the participant's ability to complete four tasks: five repeated chair stands, timed standing balance across four positions (feet parallel, semitandem, tandem, and single-leg stance), gait speed based on 6-m walk, and a narrow walk test for balance. Continuous scores on the PPB ranged from 0 to 4, with higher scores indicating better physical functioning (Simonsick et al., 2001). (2) The count of prescribed medications was based on an inventory during the clinic assessment. Participants were asked to bring in the medications they used within the past 2 weeks, and clinic staff recorded the name of the medication and the prescribed dosage. (3) Self-reported ease of walking one-quarter mile was assessed with a single item, with response categories of not that easy, somewhat easy, and very easy. (4) To assess comorbidity, participants were asked whether a doctor had ever told them they had a given condition. The comorbid-conditions variable was a simple tally of 10 chronic conditions that are common in older adulthood: cancer, heart attack, congestive heart failure, diabetes, hypertension, knee osteoarthritis, osteoporosis, chronic obstructive pulmonary disease, stroke, and angina due to heart disease. (5) Global pain was a continuous variable measured using a single item, “During the past 30 days, how often have you had pain?” with the following response options: 0 = no pain, 1 = once or twice, 2 = a few times, 3 = fairly often, 4 = very often, and 5 = every day or nearly every day. (6) Finally, body mass index was calculated by dividing the participant's weight (kilograms) by height (meters) squared, both of which were assessed during the baseline clinic visit.
The final conceptual domain of psychosocial health included depressive symptomatology, personal mastery, and satisfaction with social support. (1) Depressive symptomatology was assessed with the 20-item Center for Epidemiologic Studies Depression Scale (CES-D, Radloff, 1977), a multidimensional screening instrument for acute depressive symptoms experienced over a 7-day period. For this continuous variable, respondents indicated how often they felt each way during the past week: rarely, sometimes, occasionally, or most times. (2) Personal mastery was measured using two items from the Personal Mastery Scale of Pearlin and Schooler (1978). Participants were asked whether they agreed or disagreed with the following statements: “I often feel helpless in dealing with the problems of life” and “I can do just about anything I really set my mind to do,” with response categories of disagree strongly, disagree somewhat, agree somewhat, and agree strongly. (3) Finally, satisfaction with social support was assessed with a single yes/no item adapted from the Lubben Social Network Scale (Lubben, 1988): “In the past year, could you have used more social support than you received?”
Statistical Analyses
Descriptive statistics, χ2 for categorical variables and t-tests or analyses of variance for continuous variables, were used to describe and compare demographic and health characteristics between racial categories, stratified by sex. Simple contingency tables were used to examine racial variations in the proportion of participants who nominated each SRH category. We also used bivariate correlations to examine the association between SRH and the four components of the PPB: repeated chair stands, timed standing balance, gait speed, and the narrow walk test.
The association between race and SRH, as well as the predictive utility of the variables across the three domains, was examined with logistic regression. The models were built using hierarchical block entry of variable domains to test the association between these domains and the dichotomized (favorable vs. unfavorable) SRH outcome. Five models were fitted to examine the variable associations adjusted for (a) race only, with Black adults as the reference group; (b) race + other demographic variables, including a Sex × Race interaction term; (c) race + demographics + physical health; (d) race + demographics + physical health + psychosocial health; and (e) race + demographics + physical health + psychosocial health + the Race × PPB interaction. Addition of the Race × PPB interaction term allowed us to determine if the relationship between PPB and SRH varied by race. Moreover, entering the interaction term after the other domains allowed us to interpret how the race coefficient changed above and beyond the influence of other variables in the model. To determine if any information was lost by dichotomizing the dependent variable, we reran the five models using multinomial logistic regression with a three-group split on SRH: excellent/very good versus good versus fair/poor.
Incongruence between objective functioning and SRH was examined using a two-tiered approach. First, we interpreted the results of the Race × PPB interaction term in the fully adjusted regression model to test for racial differences in the association between physical functioning and SRH. The second strategy was to examine this association among participants at the same level of physical functioning. To do this, we stratified the scores of the PPB into tertiles and compared participants with PPB scores in the same tertile (described as high, medium, and low levels of physical functioning). Additional logistic regression analyses were then conducted to examine the association between race and SRH within each tertile of physical functioning. Variable domains were entered in hierarchical order as previously described: race, additional demographic characteristics, physical health, and psychosocial health. All analyses were carried out using SPSS Version 15® statistical software.
RESULTS
Sample Characteristics
Table 1 illustrates the demographic characteristics of the sample, stratified by sex to provide a more detailed description of the health profile of participants. Compared with those included in the analyses, the participants eliminated due to missing data did not differ on the majority of sample characteristics. They were, however, more likely to have lower education levels and report needing more social support over the past year (data not shown). The mean age for the entire sample (N = 2,729) was 73.6 years (SD = 2.9, range = 68–80). Slightly over half (51.3%) of the participants were women and 41.3% were Black. Across both sexes, Black elders had lower educational levels, reported lower satisfaction with social support, and had lower scores on the PPB than Whites. Black men and women were also less likely to report that walking one-quarter mile was “very easy” compared with Whites. The no difference finding for depressive symptoms must be interpreted with caution due to the low reliability of the CES-D in the current sample (Cronbach's α = .54). Among women, Black participants had significantly higher personal mastery, higher body mass index, and more self-reported chronic conditions than Whites. Finally, White men reported higher global pain and were significantly older than the Black men in the sample.
Table 1.
Demographic and Health Characteristics of Health, Aging, and Body Composition Participants by Race and Sex (N = 2,729)
| Women |
Men |
|||||
| Black (n = 646) |
White (n = 755) |
Black (n = 481) |
White (n = 847) |
|||
| Variable (range for total sample) | % (n) or M (SD) | p Value (within sex) | % (n) or M (SD) | p Value (within sex) | ||
| Age** (years) (68–80)a | 73.34 (2.94) | 73.57 (2.78) | .136 | 73.51 (2.75) | 73.91 (2.94) | .016 |
| Education*** (%) | <.001 | <.001 | ||||
| Less than high school | 37.0 (239) | 10.3 (78) | 49.5 (238) | 13.9 (118) | ||
| High school graduate | 35.8 (231) | 44.5 (336) | 24.5 (118) | 26.6 (225) | ||
| Postsecondary | 27.2 (176) | 45.2 (341) | 26.0 (125) | 59.5 (504) | ||
| Site*** | <.001 | .211 | ||||
| Memphis, TN | 45.0 (291) | 55.2 (417) | 48.0 (231) | 51.6 (437) | ||
| Pittsburgh, PA | 55.0 (355) | 44.8 (338) | 52.0 (250) | 48.4 (410) | ||
| Physical performance battery*** (0–4) | 1.89 (0.53) | 2.17 (0.50) | <.001 | 2.14 (0.53) | 2.42 (0.50) | <.001 |
| Prescribed medications (0–29)a | 3.37 (2.74) | 3.32 (2.88) | .758 | 3.01 (3.06) | 2.76 (2.49) | .106 |
| Ease of walking one-quarter mile*** (%) | <.001 | <.001 | ||||
| Very easy | 58.4 (377) | 75.2 (568) | 73.2 (352) | 81.7 (692) | ||
| Somewhat easy | 31.4 (203) | 22.0 (166) | 22.2 (107) | 16.4 (139) | ||
| Not that easy | 10.2 (66) | 2.8 (21) | 4.6 (22) | 1.9 (16) | ||
| Comorbid conditions** (0–10) | 1.45 (1.18) | 1.27 (1.12) | .004 | 1.35 (1.18) | 1.26 (1.12) | .192 |
| Global pain score* (0–5) | 2.26 (1.88) | 2.35 (1.94) | .384 | 1.74 (1.84) | 1.97 (1.93) | .036 |
| Body mass index*** (kg/m2) (14.59–51.99)a | 29.69 (5.81) | 26.11 (4.60) | <.001 | 27.20 (4.41) | 27.00 (3.70) | .372 |
| Depressive symptoms (0–60) | 5.01 (5.27) | 5.38 (6.02) | .232 | 4.41 (5.19) | 3.98 (4.87) | .127 |
| Personal mastery** (1–8) | 7.09 (1.19) | 6.81 (1.38) | <.001 | 7.01 (1.31) | 7.01 (1.30) | .929 |
| Needs more support*** | .004 | <.001 | ||||
| Yes | 33.9 (219) | 26.9 (203) | 31.8 (153) | 18.7 (158) | ||
Notes: Racial differences detected for entire sample: *p ≤ .05; **p ≤ .01; ***p ≤ .001.
Actual range for entire sample.
SRH
Results of bivariate analyses revealed that the five-level SRH measure was significantly correlated (p ≤ .01) with each of the individual components of the PPB. The magnitude of the association was highest for the repeated chair stands task (Spearman's rho = 0.23), followed by the narrow walk test (Spearman's rho = 0.17), gait speed (Spearman's rho = 0.14), and the timed standing balance task (Spearman's rho = 0.10). Because the magnitude of the association was higher for the PPB composite score (Spearman's rho = 0.29) than for any of the individual scale components, the composite score was used in the logistic regression models.
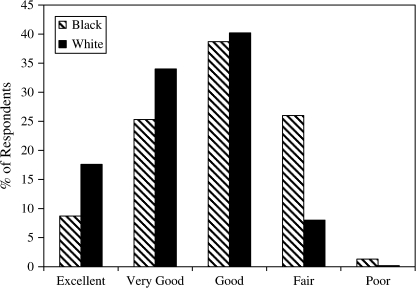
As shown in Figure 1, a greater proportion of Black participants rated their health as fair or poor compared with Whites (27.3% vs. 8.2%, respectively). A greater proportion of Whites (17.6%) rated their health as excellent compared with only 8.7% of Blacks, and 34.0% of Whites reported very good health compared with 25.3% of Blacks. The proportion of older adults reporting good health was similar across race (38.7% of Blacks and 40.2% of Whites).
Figure 1.
Self-rated health of older men and women stratified by race. χ2(4, N = 2,726) = 203.43, p < .001.
A logistic regression analysis was performed on SRH (favorable vs. unfavorable) as the outcome with the five hierarchically ordered variable domains. In the unadjusted model, White elders were 4.18 times more likely than Black elders to report favorable SRH (Table 2). When additional demographic predictors were included in the model at Step 2 (Negelkerke R2 = .15), the relationship between race and SRH remained significant but was attenuated, with Whites being 3.45 times more likely than Black elders to report favorable SRH. A Race × Sex interaction was not detected. The significant race association persisted when physical health variables at Step 3 (odds ratio [OR] = 3.36, 95% confidence interval [CI] = 2.35–4.82) and psychosocial health variables at Step 4 (OR = 3.74, 95% CI = 2.59–5.40) were included in the model. SRH was significantly predicted by all variables in the physical health domain with the exception of body mass index. Two of the psychosocial health variables—depressive symptomology and personal mastery—were significantly associated with SRH (Negelkerke R2 = .28), but satisfaction with social support was not. Finally, the Race × PPB interaction was statistically significant in the fully adjusted model, which justified a more in-depth exploration of the relationship between race and SRH at each level of objective physical functioning.
Table 2.
Odds Ratios (ORs) and 95% Confidence Intervals (CIs) for Logistic Regression Predicting Favorable Self-Rated Health (SRH)a
| Conceptual Domains and Select Predictor Variables | Step 1 Race Only |
Step 2 + Demographics |
Step 3 + Physical Health |
Step 4 + Psychosocial Health |
Step 5 + Interaction Term |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Race (White vs. Black) | 4.18 (3.35–5.21)*** | 3.45 (2.47–4.80)*** | 3.36 (2.35–4.82)*** | 3.74 (2.59–5.40)*** | 1.42 (0.57–3.52) |
| Demographics | |||||
| Sex (men vs. women) | 1.02 (0.78–1.34) | 0.76 (0.56–1.03) | 0.75 (0.55–1.02) | 0.80 (0.58–1.08) | |
| Age (years) | 0.97 (0.94–1.01) | 1.00 (0.96–1.04) | 1.00 (0.96–1.05) | 1.00 (0.96–1.04) | |
| Education (graduate vs. less than high school) | 2.46 (1.94–3.11)*** | 2.39 (1.86–3.08)*** | 2.28 (1.77–2.95)*** | 2.32 (1.80–3.00)*** | |
| Site (Memphis, TN vs. Pittsburgh, PA) | 1.20 (0.96–1.50) | 1.22 (0.97–1.55) | 1.23 (0.97–1.56) | 1.24 (0.97–1.57) | |
| Race × Sex | 0.89 (0.57–1.40) | 0.85 (0.53–1.37) | 0.78 (0.48–1.27) | 0.68 (0.42–1.13) | |
| Physical health | |||||
| Physical performance battery (PPB)b | 1.73 (1.38–2.16)*** | 1.63 (1.30–2.05)*** | 1.33 (1.00–1.77) | ||
| Number of medications | 0.88 (0.84–0.91)*** | 0.88 (0.85–0.92)*** | 0.88 (0.84–0.92)*** | ||
| Ease of walking one-quarter mile (easy vs. not easy) | 2.07 (1.35–3.18)*** | 1.97 (1.28–3.05)** | 1.99 (1.29–3.06)** | ||
| Comorbidity | 0.86 (0.77–0.95)** | 0.86 (0.78–0.96)** | 0.86 (0.78–0.96)** | ||
| Global pain | 0.85 (0.80–0.91)*** | 0.88 (0.83–0.94)*** | 0.88 (0.83–0.94)*** | ||
| Body mass index | 1.02 (1.00–1.05) | 1.01 (0.99–1.04) | 1.02 (0.99–1.04) | ||
| Psychosocial health | |||||
| Depressive symptoms | 0.95 (0.93–0.97)*** | 0.95 (0.93–0.97)*** | |||
| Personal mastery | 1.10 (1.00–1.20)* | 1.10 (1.00–1.20)* | |||
| Needs support (yes vs. no) | 0.86 (0.67–1.11) | 0.86 (0.67–1.11) | |||
| Race × PPB | 1.66 (1.07–2.57)* | ||||
| Omnibus χ2 statistic | 176.09*** | 70.10*** | 189.72*** | 45.36*** | 5.19 |
| Negelkerke R2 | 0.11 | 0.15 | 0.25 | 0.28 | 0.28 |
Notes: *p ≤ .05; **p ≤ .01; ***p ≤ .001.
Favorable = excellent, very good, or good SRH.
Health, Aging, and Body Composition PPB.
Results of the fully adjusted model that used the alternate, multinomial approach revealed that the association between race and SRH was driven by the proportional Black versus White difference in the excellent/very good versus fair/poor SRH groups. Specifically, Whites compared with Blacks were more likely to report excellent/very good SRH than fair/poor SRH (OR = 2.67, 95% CI = 1.15–6.18; p = .02), but there was not a significant race–SRH association when comparing the excellent/very good versus good SRH groups (OR = 1.98, 95% CI = 0.89–4.42; p = .10). Because this approach did not provide any new information and for ease of interpretation, we decided to use the dichotomized SRH outcome to further examine the health pessimism hypothesis.
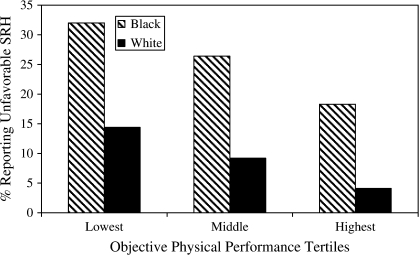
Stratification by Objective Physical Functioning
To further explore the Race × PPB interaction, the PPB was first divided into tertiles in order to examine racial differences in SRH at varying levels of PPB. As shown in Figure 2, at each level of objective physical functioning, Black elders were significantly more likely to report unfavorable SRH than Whites. The percent of those reporting unfavorable SRH for each racial group decreased with progressively higher levels of physical functioning, but the racial disparity (e.g., the proportion of Black to White older adults reporting unfavorable SRH) increased from the lowest to the highest tertile. In order to determine the adjusted odds for reporting favorable SRH at each level of functioning, we then performed a series of logistic regression analyses parallel to the one previously described (Step 5) at each tertile.
Figure 2.
Percent of Black and White older adults who report unfavorable self-rated health (SRH) (unfavorable = fair or poor SRH) at each level of objective physical functioning. Significant differences by race and tertile (p ≤ .001).
As shown in Table 3, results of the fully adjusted models suggest that after stratifying by objective physical functioning, the association between race and SRH became stronger. For participants in the lowest tertile of functioning, the fully adjusted model indicated that White elders were more than twice as likely (OR = 2.20, 95% CI = 1.48–3.28) as Black elders to report favorable SRH. White elders in the middle tertile were 3.77 times more likely to report favorable SRH compared with Black elders (95% CI = 2.43–5.83), and among the highest functioning participants, Whites were 5.54 times more likely than Black elders to report favorable SRH (95% CI = 2.92–10.54). These results indicate that after adjustment, the Black versus White disparity increased with higher levels of objective physical functioning.
Table 3.
Odds of Reporting Favorable Self-Rated Health (SRH)a in White Compared With Black Participants at Similar Levels of Objective Physical Functioningb
| Hierarchical Block Entry of Variables |
n per Tertilec |
Odds Ratio | 95% Confidence Interval | |
| Black | White | |||
| Lowest tertile of objective functioning | 514 | 388 | ||
| Race only | 2.79*** | 1.99–3.91 | ||
| Model A + demographics | 2.09*** | 1.44–3.04 | ||
| Model B + physical health | 2.15*** | 1.45–3.18 | ||
| Model C + psychosocial health | 2.20*** | 1.48–3.28 | ||
| Middle tertile of objective functioning | 384 | 523 | ||
| Race only | 3.54*** | 2.43–5.14 | ||
| Model A + demographics | 3.07*** | 2.07–4.55 | ||
| Model B + physical health | 3.46*** | 2.26–5.30 | ||
| Model C + psychosocial health | 3.77*** | 2.43–5.83 | ||
| Highest tertile of objective functioning | 229 | 691 | ||
| Race only | 5.32*** | 3.21–8.81 | ||
| Model A + demographics | 4.42*** | 2.56–7.62 | ||
| Model B + physical health | 4.78*** | 2.61–8.72 | ||
| Model C + psychosocial health | 5.54*** | 2.92–10.54 | ||
Notes: ***p ≤ .001.
Favorable = excellent, very good, or good SRH.
Based on mean score on the Health, Aging, and Body Composition physical performance battery.
Some error in the distribution of tertiles due to rounding.
DISCUSSION
In our analyses, the addition of physical and psychosocial health variables attenuated, but did not eliminate, the association between race and SRH (i.e., Whites were still 3.7 times more likely than Blacks to report favorable SRH). When participants were compared at the same level of objective physical functioning, Whites were significantly more likely to report favorable SRH compared with Black elders after adjusting for differences in demographics, physical health, and psychosocial health. Even among those participants with the best performance scores across several physical domains, Whites were 5.5 times more likely to report favorable SRH than Black elders. These data are consistent with the hypothesis of greater health pessimism among Black elders. It also suggests that enduring self-concept might be the most accurate way to view SRH, whereby cultural differences exist in how health is interpreted and the extent to which individual factors influence SRH assessments.
Information gained from our analysis supports the notion that SRH taps into multiple dimensions of health (Idler & Benyamini, 1997). The association between race and SRH persisted after adjusting for multiple health-related variables, suggesting that the factors which influence SRH are complex and not readily captured with standard subjective and objective measures. In the Cardiovascular Health Study of the Elderly, Schulz et al. (1994) found that from an extensive list of 70 predictors, it was the health-related factors which participants were aware of that had the strongest association with SRH (e.g., prescription medications, known illnesses, etc.). Our work expands on this by demonstrating that objective physical function is also important to the SRH of older adults. The observation that multiple factors predict SRH supports previous literature, but the finding that racial differences exist at similar levels of functioning warrants further discussion.
Research suggests that definitions of what constitutes good (and poor) health differ across diverse populations because the meaning of “healthy” is often related to group referents and lifetime experiences (Damron-Rodriguez, Frank, Enriquez-Haass, & Reuben, 2005; Krause & Jay, 1994). In a study of 114 older adults with chronic illness, Blacks tended to focus more on the presence or absence of conditions, whereas Whites focused more on functioning (Silverman, Smola, & Musa, 2000). Krause and Jay found that Whites used physical functioning as a frame of reference, whereas non-Whites (Black and Hispanic) might think more about health problems when interpreting SRH. Results from these studies support our finding of comparatively greater concordance between SRH and physical functioning among Whites (i.e., high functioning corresponded with higher SRH ratings among Whites but not Blacks). It is possible that in the current study, high levels of functioning were responsible for elevated SRH among Whites but did not influence ratings of health to the same extent among Black elders due to different definitions of health.
An alternate explanation is that factors not included in the current analyses might better explain SRH among Black elders. McMullen and Luborsky (2006) recently suggested that Black older adults might be using more than biomedical and physical health criteria when defining health as a way to maintain health identity. Although our models of SRH included some psychosocial measures, these constructs were not exhaustive and tend to be less well-measured than standard physical health variables. The addition of a more diverse set of health and psychosocial variables might show a greater attenuation of the race difference than was observed in the current analyses.
The hypothesis of health pessimism among Black elders was explored in the current analysis in a way that has not been previously described. Prior studies have shown that racial differences in SRH persist after controlling for a number of demographic and health-related variables. However, none to our knowledge have examined the health pessimism hypothesis by using objective physical functioning as the standard on which physical health is gauged. Using objective indicators in research on health pessimism has implications for the development of screening instruments to identify older adults who are at risk for poor outcomes. Hong, Oddone, Dudley, and Bosworth (2005) found that among older veterans with hypertension, health pessimists had less control over their blood pressure than elders in any other health congruence group (good health realists, poor health realists, or health optimists). If health pessimists are at heightened risk for poor health outcomes, future research could address whether health pessimism is a stable trait based on a history of poor health or whether health pessimism in older adulthood could be modified with targeted behavioral interventions.
The underlying reasons for racial group differences in health pessimism are not well understood. As previously suggested, these differences in health pessimism might be due to cultural or psychosocial variations in how individuals conceptualize the global construct of SRH. In our study, for example, self-reported pain was higher among White men compared with Black men, which might also suggest differences in how these groups view, interpret, and report physical symptoms. Another intriguing possibility which has some support in the social science literature is the idea that lifetime experiences have resulted in more negative health appraisals among Black individuals. In a sample of 1,106 Blacks and Whites age 18 years and older, interpersonal maltreatment (defined as perceived maltreatment from others in daily life) explained racial differences in health pessimism (Boardman, 2004). It is possible, then, that perceived maltreatment might lead to elevated health pessimism among racial minority elders, although the data are currently unavailable to test this in the Health ABC cohort.
The present study has limitations which must be acknowledged. First, the data were cross-sectional, which limited our ability to understand the directionality of the relationships between variables. It is possible that health pessimism in the baseline Health ABC sample could lead to poor health outcomes and accelerated health decline over time. Although our results were consistent with the literature, generalizability may be limited because Health ABC participants were relatively high functioning at baseline. Also, factors which are unaccounted for in our analyses might be influencing SRH. Finally, although performance on the multidimensional PPB seems to be a strong measure of functioning, participants in future analyses should be equated on additional measures (e.g., grip strength, 400 m walk, etc.) to see if the health pessimism hypothesis holds across other dimensions of physical functioning.
Understanding SRH in minority populations could have important clinical and policy implications because of its widespread use and its predictive utility (Damron-Rodriguez et al., 2005; Ferraro & Kelley-Moore, 2001). SRH is not only strongly related to health but also provides information about well-being that is not explained by other measures. We demonstrated that racial differences in SRH did not coincide with differences in functioning nor were these differences explained by a variety of demographic, physical, and psychosocial factors. SRH is perhaps the most commonly used measure of global health in national surveillance surveys. For example, Healthy People 2010 uses SRH to measure health-related quality of life and describe overall health across a range of demographic characteristics. However, many of these surveys lack the data necessary for developing an in-depth understanding of racial variations in SRH. The current analysis makes a unique contribution by including objective physical functioning as one of these factors in a large and diverse sample of community-dwelling older adults.
FUNDING
Postdoctoral support for Dr. S.M.S. is provided by the Kellogg Health Scholars Program, funded by the W. K. Kellogg Foundation (P0117943), University of Pittsburgh Center for Minority Health site (NIH-5P60MD000207-07). Health ABC is funded by N01-AG-6-2101, N01-AG-6-2103, N01-AG-6-2106, and R01 AG18037. This research was supported in part by the Intramural Research program of the National Institutes of Health, National Institute on Aging.
Acknowledgments
Thanks to Dr Robert Boudreau at the University of Pittsburgh for his statistical expertise and to the Pittsburgh Claude D. Pepper Center Junior Scholars Working Group (P30 AG024827) for their comments on the manuscript. S.M.S., A.B.N., and R.S. were responsible for the study design. S.M.S., A.B.N., and S.M.A. performed all statistical analyses and S.M.S. drafted the original research article. A.B.N., S.M.A., R.N.R., R.J.T., Jr., G.A.B., T.B.H., A.K., S.S., and H.N.A. provided critical revision of the article for important intellectual content. A.B.N. provided administrative, technical, and logistic support. None of the authors had any possible conflicts of interest.
References
- Bailis DS, Segall A, Chipperfield JG. Two views of self-rated general health status. Social Science & Medicine. 2003;56:203–217. doi: 10.1016/s0277-9536(02)00020-5. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Blumstein T, Lusky A, Modan B. Gender differences in the self-rated health–mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? The Gerontologist. 2003;43:396–405. doi: 10.1093/geront/43.3.396. [DOI] [PubMed] [Google Scholar]
- Boardman JD. Health pessimism among black and white adults: The role of interpersonal and institutional maltreatment. Social Science & Medicine. 2004;59:2523–2533. doi: 10.1016/j.socscimed.2004.04.014. [DOI] [PubMed] [Google Scholar]
- Borrell LN, Crawford ND. Race, ethnicity, and self-rated health status in the Behavioral Risk Factor Surveillance System Survey. Hispanic Journal of Behavioral Sciences. 2006;28:387–403. [Google Scholar]
- Damron-Rodriguez J, Frank JC, Enriquez-Haass VL, Reuben DB. Definitions of health among diverse groups of elders: Implications for health promotion. Generations. 2005, Summer;29:11–16. [Google Scholar]
- Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: Models to explain health disparities. Annual Review of Anthropology. 2005;34:231–252. [Google Scholar]
- Ferraro KF. Self-ratings of health among the old and the old-old. Journal of Health and Social Behavior. 1980;21((4)):377–383. [PubMed] [Google Scholar]
- Ferraro KF. Are Black older adults health-pessimistic? Journal of Health and Social Behavior. 1993;34:201–214. [PubMed] [Google Scholar]
- Ferraro KF, Farmer MM, Wybraniec JA. Health trajectories: Long-term dynamics among Black and White adults. Journal of Health and Social Behavior. 1997;38:38–54. [PubMed] [Google Scholar]
- Ferraro KF, Kelley-Moore JA. Self-rated health and mortality among Black and White adults: Examining the dynamic evaluation thesis. Journals of Gerontology: Social Sciences. 2001;56:S195–S205. doi: 10.1093/geronb/56.4.s195. [DOI] [PubMed] [Google Scholar]
- Hong TB, Oddone EZ, Dudley TK, Bosworth HB. Subjective and objective evaluations of health among middle-aged and older veterans with hypertension. Journal of Aging and Health. 2005;17:592–608. doi: 10.1177/0898264305279780. [DOI] [PubMed] [Google Scholar]
- Idler EL. Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Idler EL, Hudson SV, Leventhal H. The meanings of self-ratings of health: A qualitative and quantitative approach. Research on Aging. 1999;21:458–476. [Google Scholar]
- Krause NM, Jay GM. What do global self-rated health items measure? Medical Care. 1994;32:930–942. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- Lubben JE. Assessing social networks among elderly populations. Family & Community Health. 1988;11:42–52. [Google Scholar]
- McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic US cohort. American Journal of Epidemiology. 1999;149:41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- McMullen CK, Luborsky MR. Self-rated health appraisal as cultural and identity process: African American elders' health and evaluative rationales. The Gerontologist. 2006;46:431–438. doi: 10.1093/geront/46.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. NCHS, 2006. Respondent-assessed health by age, sex, and race/ethnicity: United States, 1982–2006 [Google Scholar]
- Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, Pahor M, Satterfield S, Brach JS, Studenski SA. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. Journal of the American Medical Association. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19:2–21. [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ren XS, Amick BC. Racial and ethnic disparities in self-assessed health status: Evidence from the National Survey of Families and Households. Ethnicity & Health. 1996;1:293–304. doi: 10.1080/13557858.1996.9961798. [DOI] [PubMed] [Google Scholar]
- Schulz R, Mittelmark M, Kronmal R, Polak JF, Hirsch CH, German P, Bookwala J. Predictors of perceived health status in elderly men and women. Journal of Aging and Health. 1994;6:419–447. doi: 10.1177/089826439400600401. [DOI] [PubMed] [Google Scholar]
- Silverman M, Smola S, Musa D. The meaning of healthy and not healthy: Older African Americans and whites with chronic illness. Journal of Cross-Cultural Gerontology. 2000;15:139–156. doi: 10.1023/a:1006794215571. [DOI] [PubMed] [Google Scholar]
- Simonsick EM, Newman AB, Nevitt MC, Kritchevsky SB, Ferrucci L, Guralnik JM, Harris T. Measuring higher level physical function in well-functioning older adults: Expanding familiar approaches in the Health ABC. Journals of Gerontology: Biological and Medical Sciences. 2001;56A:M644–M649. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2007. Early release of selected estimates based on data from the 2006 National Health Interview Survey. [Google Scholar]