Abstract
Background
Previous studies have indicated that gait patterns in older people may be affected by concern about falling. The aim of this study was to examine the effects of concern about falling and physiological falls risk on gait performance using a paradigm in which concern about falling was experimentally induced.
Methods
Forty-four community-living older adults (17 men, 27 women) with a mean age of 76.8 (standard deviation = 5.2) years walked at self-selected speeds on the floor and on a 60-cm elevated walkway in normal and dim lighting conditions. Temporal and spatial gait parameters, muscle activity, measures of physiological arousal, physiological falls risk, and concern about falls were assessed.
Results
Physiological falls risk was associated with slower walking speeds in all conditions including the optimal (floor) condition (p = .029). In the elevated walkway conditions, concern about falls (both self-report and as indicated by physiological arousal) was increased and participants walked more slowly, took shorter steps, decreased their cadence, and spent more time in double support (p < .005). Disproportionately large reductions in walking speed were evident in participants with greater concern about falling (p = .018).
Conclusions
These findings suggest that walking performance is influenced by both physiological and psychological factors. Physiological falls risk appears to determine walking speed under optimal conditions, whereas concern about falling elicits greater (possibly excessive) gait adjustments under conditions of postural threat.
Keywords: Fear of falling, Aging, Elderly, Walking, Behavior
POOR walking performance has previously been associated with older age, increased risk of falling, and greater concern about falling. Changes in spatial and temporal gait parameters in older people due to concern about falling have been demonstrated via reduced speed (1–6), shorter stride length (1–4), prolonged double-support time (1,4), and increased gait variability (4,7). Similar changes have been associated with older age (8) and increased physiological falls risk (9). The question arises whether a combination of the aforementioned factors might further induce changes in walking performance, such that excessive concern could lead to extreme carefulness and adoption of overly cautious behaviors to reduce a perceived high risk of falling.
By manipulating the environment in a way that exacerbates the potential consequences of a fall, it is possible to investigate whether concern about falls induces gait adaptations. Several studies have suggested that environmental manipulations can induce concern regarding the possibility of a fall (10–22). Some studies have demonstrated decreased sway while standing on an elevated platform, which was mediated by a stiffening strategy at the ankle joint (10–18). Brown and colleagues also described significant changes in gait parameters on an elevated walkway as evidenced by (a) a slowed speed, a shorter stride length, and longer time spent in double support; (b) reduced joint angles and reduced variability of joint kinematics; and (c) an increased level of muscle activation in the lower leg musculature (19–22).
Although work to date has provided valuable insights regarding the potential influence of concern about falling on gait, it has been limited in two ways. First, the method of inducing fall-related concern during walking by environmental manipulation (i.e., narrow beam walking), in effect, changed the nature of the task (restricted stride width), making it difficult to identify the cause of the subsequent gait alterations (19–22). Second, previous work has been restricted to healthy older adults without a concern about falling (10–17,19–22). In this study, we aimed to address these issues. We provided an environmental manipulation without constraining the participant or the support surface. This comprised an elevated walkway, dimmed lighting, and no provision of protective devices such as a harness. We also studied older people with a range of physiological falls risk and levels of concern about falling to investigate the effect of both physiological and psychological factors on walking performance.
METHODS
Participants
Forty-four older adults were recruited from a cohort of 1,042 community-dwelling men and women living in eastern Sydney aged 70 years and older (study in progress, please see Acknowledgments). Participants for this study were randomly selected from subgroups with high and low levels of concern about falls, and high and low physiological fall risk scores, defined below while matched for gender. This provided four groups of at least 10 participants with the following combinations of concern and risk: high concern/high risk, high concern/low risk, low concern/high risk, and low concern/low risk. Exclusion criteria were neurological, cardiovascular, or major musculoskeletal impairments (determined at a baseline physiological assessment) that precluded participants to walk for 20 m without a walking aid. Information pertaining to previous falls, medical conditions, medication use, levels of functioning during daily activities, and mental status was also obtained and is presented in Table 1. Levels of disability were assessed using the 12-item World Health Organization Disability Assessment Schedule (23). This is a multidimensional questionnaire that provides a general disability score on a 4-point scale (1 = none to 5 = extreme/cannot do; total score range 0–36) across six domains (ie, understanding and communicating, getting around, self-care, getting along with others, household and work activities, and participation in society). Mental status was assessed using the Mini-Mental State Examination. The study was approved by the University of New South Wales Human Studies Ethics Committee and all participants provided informed consent prior to participation.
Table 1.
Demographic, Fall Risk, Falls Efficacy, Fall History, Health, and Medical Characteristics of the Study Population
| Mean (SD) or Number (%) | |
| Age (y) | 76.9 (5.1) |
| Female gender (%) | 27 (61.4) |
| One or more falls in previous year (%) | 9 (20.5) |
| Two or more chronic medical conditions* (%) | 12 (27.3) |
| Four or more medications (%) | 5 (13.6) |
| Cardiovascular system medications (%) | 19 (43.2) |
| Central nervous system medications (%) | 5 (13.6) |
| Height (cm) | 168.1 (9.1) |
| Physiological Profile Assessment falls risk score (z score) | 0.80 (0.83) |
| Falls Efficacy Scale International score (range 16–64) | 22.2 (5.6) |
| World Health Organisation Disability Assessment Schedule score (range 0–36) | 16.4 (5.0) |
| Mini-Mental State Examination score (range 0–30) | 28.0 (1.4) |
Baseline Measures
The Physiological Profile Assessment (PPA) was used to gain an estimate of physiological falls risk (9). The PPA contains five validated measures of physiological function: (a) visual contrast sensitivity—assessed using the Melbourne Edge Test; (b) proprioception—measured using a lower limb–matching task, where errors in degrees are recorded using a protractor inscribed on a vertical clear acrylic sheet placed between the legs; (c) quadriceps strength—measured isometrically in the dominant leg, while participants are seated with the hip and knee flexed to 90°; (d) simple reaction time—measured using a light stimulus and a finger press as the response; and (e) postural sway (area as a product of maximum anteroposterior and mediolateral displacements)—measured using a sway meter recording displacements of the body at the level of the pelvis, while participants stood on a foam rubber mat with eyes open. In multivariate models, weighted contributions from these five variables (standardized canonical coefficients = −.33 for visual contrast sensitivity, .20 for lower limb proprioception, .47 for hand reaction time to a visual cue, −.16 for quadriceps strength, and .51 for postural sway) provide a fall risk score that can predict community-dwelling people at risk of multiple falling with 75% accuracy for a 12-month period (9). Clinically, fall risk scores of less than 1 can be interpreted as being at a low to mild risk of falling, and fall risk scores of 1 and above as being at a moderate to high risk of falling (9).
Concern about falling was evaluated using the Falls Efficacy Scale International (FES-I) (24). FES-I provides information on level of concern on a 4-point scale (1 = not at all concerned to 4 = very concerned; total score range 16–64) across 16 activities of daily living (eg, cleaning the house, simple shopping, walking on uneven surface). The FES-I has excellent reliability (Cronbach's alpha = .97, test-retest = .94) (24). For purposes of this study, FES-I scores of less or equal to 22 were interpreted as a low to moderate level of concern, and scores of 23 and above were interpreted as a high level of concern. This cutoff point categorized people as having a high level of concern if they recorded at least some concern on seven or more items but also allowed for people who were very concerned only with regard to the most hazardous activity, that is, walking on a slippery surface, to be classified as having a low or moderate concern. Using this criterion, 33% of the larger community sample from which this subgroup was drawn would be classified as having a high level of concern about falls—a figure consistent with other published studies (25).
Protocol
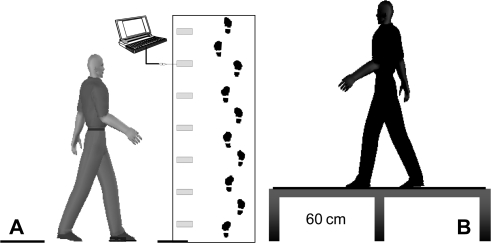
Participants were instructed to walk at their usual, comfortable walking speed. The trials were conducted in two light (bright and dim; 700 and 5 lux [TENMA light meter; TENMA, TW, Taiwan]) and two level (floor and 60-cm height) conditions, for a total of four different conditions: floor bright, floor dim, height bright, and height dim. The elevated walkway was 720 cm long and 120 cm wide, as illustrated in Figure 1. Participants were required to walk within a 40-cm-wide strip of the walkway (a distance that did not restrict stride width) adjacent to the mat/platform edge. Condition presentation order was randomized. No practice was provided and participants did not wear a safety harness. To enhance safety, two experimenters were present at all times and observed the participants throughout the study, and participants were reminded that they could withdraw from the study at any time if they felt unsafe. Four trials were recorded for each condition and data were averaged for subsequent analyses.
Figure 1.
Schematic representation of two extreme testing conditions: (A) floor light (700 lux), (B) height dim (5 lux).
Spatial and temporal gait parameters were measured with a GAITRite® system (CIR Systems Inc., Clifton, NJ). The standard GAITRite system is a mat of 460-cm length with an active sensor area of 366-cm long and 61-cm wide. Gait parameters were obtained from GAITRite Gold Software Version 3.3 and included speed (cm/s), step length (cm), cadence (steps/min), double-support time—time spent with both feet in stance (s)—and stride width (cm).
Participants were asked to indicate their level of concern regarding the task before and immediately following each condition on a 10-point Likert scale (1 = not at all concerned; 10 = most concern imaginable).
Mean galvanic skin conductance and mean blood pressure were used to indicate any change in physiological arousal imposed by the different testing conditions. Bipolar finger electrodes were placed on the third and fourth digits of the left hand to measure the galvanic skin response. An infrared photoelectric sensor was attached to the second digit of the left hand, to record changes in pulsatile blood flow and provide an indication of blood pressure. To minimize movement artifact (noise) in these records, the left arm was stabilized against the torso. Muscle activity electromyography (EMG) was recorded during each trial from tibialis anterior and medial gastrocnemius. Two Ag-AgCl surface electrodes were placed over the muscle belly, in series with the major muscle line of action. Cables to the system trailed behind participants and were suspended to minimize disruption to normal gait. Data were collected via a PowerLab bioamplifier at 2 kHz (ADInstruments, Colorado Springs, CO). Data were full-wave rectified and low-pass filtered with a cutoff frequency of 50 Hz using Chart Pro software (ADInstruments, Bella Vista, Australia).
Statistical Analyses
Statistical analyses were performed using SPSS 14.0 for Windows (SPSS Inc., Chicago, IL). After a square root transformation of galvanic skin conductance and a logarithmic transformation of blood pressure and double-support time, assumptions regarding normality of sampling distributions, homogeneity of variance-covariance matrices, linearity, and multicollinearity were met. There were no univariate or multivariate outliers. Main effects and interaction effects were investigated using a mixed four-factor (Physiological Falls Risk [low PPA/high PPA] × Concern About Falling [low FES-I/high FES-I] × Height [floor/height] × Light [bright/dim]) repeated measures multivariate analysis of variance. Factors found significant in the multivariate analyses were followed by univariate post hoc analyses. Only the main effect of height is described considering a possible confounding effect of reduced light on the level of difficulty on the task. Physiological arousal, level of concern regarding the task, spatiotemporal gait parameters, and muscle activity were entered into separate analyses.
RESULTS
Table 1 indicates that the study sample comprised a group of relatively healthy older people without cognitive impairment. All participants completed all trials, with no stumbles or falls.
Physiological Arousal
Physiological arousal was confirmed by a significant Height × Light interaction effect (Wilks = .69, F2,38 = 8.41, p = .001) across all participants, as described by increased blood pressure (F1,39 = 17.02, p < .001) and increased galvanic skin conductance (F1,39 = 3.56, p = .067) in the height dim condition (Table 2). Self-reported levels of concern regarding the task also showed a strong main effect for height (Wilks = .83, F1,40 = 8.50, p = .006). There were no significant interaction effects of physiological falls risk and concern about falling with height. These findings indicate that the environmental manipulations were sufficient to increase fall-related concern for all participants.
Table 2.
Blood Pressure and Galvanic Skin Conductance Increased in the Most Challenging Condition
| Floor bright |
Floor dim |
Height bright |
Height dim |
pb | |||||
| Mean | SEMa | Mean | SEMa | Mean | SEMa | Mean | SEMa | ||
| Blood pressure (mmHg) | 73.26 | 5.90 | 71.63 | 5.90 | 71.98 | 5.18 | 82.86 | 4.99 | <.001 |
| Galvanic skin conductance (μΩ) | 16.29 | 1.51 | 16.02 | 1.61 | 16.32 | 1.47 | 17.30 | 1.55 | .067 |
Notes: aStandard error of the mean.
Level of significance of the interaction effect for Height × Light.
Gait Parameters
Effects of surface height.—
A main effect of height (Wilks = .44, F5,35 = 8.84, p < .001) confirmed that all participants altered their gait patterns in elevated walking conditions. As indicated in Table 3, in the height conditions, participants had a slower walking speed (F1,39 = 38.64, p < .001), a shorter step length (F1,39 = 41.04, p < .001), a longer double-support time (F1,39 = 23.77, p < .001), and reduced cadence (F1,39 = 9.57, p = .004). Stride width (F1,39 = 3.26, p = .079) was not significantly affected by walking on the elevated walkway. Analyses of a main effect of height on the average EMG in tibialis anterior or medial gastrocnemius muscles did not reveal significant differences across the four conditions.
Table 3.
Main Effects for Height on Gait Parameters: Walking Speed, Step Length, Double-Support Time, Cadence, and Stride Width
| Floor bright |
Floor dim |
Height bright |
Height dim |
pb | |||||
| Mean | SEMa | Mean | SEMa | Mean | SEMa | Mean | SEMa | ||
| Walking speed (cm/s) | 108.52 | 4.01 | 104.53 | 4.21 | 99.06 | 4.36 | 90.95 | 4.39 | <.001 |
| Step length (cm) | 59.01 | 1.60 | 56.84 | 1.69 | 55.21 | 1.85 | 51.02 | 1.97 | <.001 |
| Double-support time (s) | 0.31 | 0.01 | 0.32 | 0.01 | 0.34 | 0.02 | 0.34 | 0.01 | <.001 |
| Cadence (steps/min) | 109.41 | 1.69 | 109.27 | 1.79 | 106.47 | 1.86 | 104.67 | 2.32 | .004 |
| Stride width (cm) | 9.56 | 0.51 | 9.85 | 0.58 | 9.41 | 0.52 | 9.28 | 0.56 | .079 |
Notes: aStandard error of the mean.
Level of significance of the interaction effect for Height.
Effect of physiological falls risk and concern about falling.—
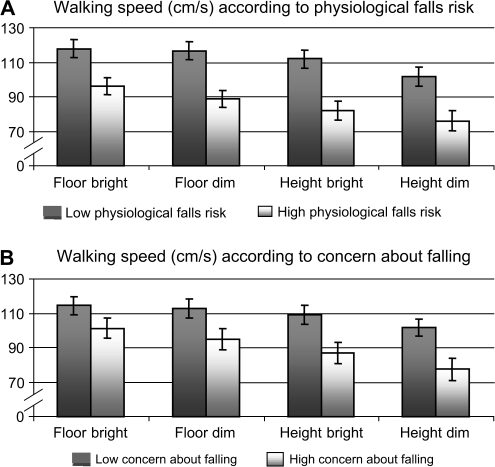
Figure 2 provides a graphical representation of walking speed in the four conditions for the participants categorized in terms of low and high physiological falls risk (panel A) and low and high concern about falling (panel B). There was a main effect for physiological falls risk (Wilks = .71, F5,35 = 2.87, p = .029) and an interaction effect between Height × Concern About Falling (Wilks = .69, F5,35 = 3.18, p = .018). The main effect for concern about falling (Wilks = .80, F5,35 = 1.78, p = .143) and the interaction effect between Height × Physiological Falls Risk (Wilks = .78, F5,35 = 1.95, p = .111) were not significant, and neither were the Physiological Falls Risk × Concern About Falling interaction effects. Univariate post hoc analyses indicated that participants with a high physiological falls risk walked slower (F1,39 = 11.23, p = .002), took shorter steps (F1,39 = 9.69, p = .003), spent more time in double support (F1,39 = 6.64, p = .014), and showed a reduced cadence (F1,39 = 6.31, p = .016) in all four conditions including the optimal (floor) conditions compared with participants with a low physiological falls risk. In contrast, participants with a high concern about falling showed similar gait characteristics on the floor compared with participants with a low concern about falling but walked significantly slower (F1,39 = 6.00, p = .019), took shorter steps (F1,39 = 9.02, p = .005), and spent more time in double support (F1,39 = 5.62, p = .023) in the height conditions.
Figure 2.
Graphical representation of walking speed across the four conditions in older people with a high physiological falls risk (A) and in older people with a high concern about falling (B). Data are means ± Standard Error.
DISCUSSION
To date, the link between concern about falling and gait performance has been primarily investigated in epidemiological studies (25). The aim of this study was to provide a complementary picture of the effect of both physiological falls risk and concern about falling on gait performance using a paradigm in which concern about falling was experimentally induced. We successfully induced fall-related concern, which was shown both by self-report and measures of physiological arousal.
On the elevated walkway, participants walked more slowly, took shorter steps, decreased their cadence, and spent more time in double support. These results are in accord with previous findings by Brown and colleagues (19). However, we did not find a change in muscle activity, which may relate to differences in the experimental conditions. In the study by Brown and colleagues, the experimental condition constrained the participant (ie, harness) and support surface (ie, walking on a beam), which would necessitate a change in gait mechanics. Therefore, the cause for a co-contraction of the lower leg musculature as well as the change in gait kinematics may not have been solely attributed to concern. By using an elevated walkway, dimmed lights, and not providing a harness, our setup allowed for unrestrained gait. We confirmed that older people adopt a more cautious gait pattern with the environmental context of increased fall-related concern; however, there was no evidence for muscle co-contraction.
Winter and colleagues (26) highlighted a conundrum regarding the reasons underlying slowed gait speed in older age, that is, does it result from physical limitations or an adaptation to achieve a more cautious gait pattern. We found that participants with a greater physiological falls risk had slower walking speeds across all conditions including the optimal (floor) conditions compared with those with a low physiological falls risk. In contrast, concern about falling was not associated with walking speed in the floor conditions. These findings suggest that the primary cause for slower gait in older people is physical limitation and not adaptation, that is, concern about falling.
Previous studies have shown that concern about falling can cause changes in spatial and temporal gait parameters (1–6). The current study is the first to suggest that greater levels of concern about falling primarily cause additional adaptations in more challenging situations. We found that concern about falling imposed larger alterations in walking speed and the related measures of step length and double-support time in the elevated walkway conditions that posed a postural threat. It is possible that this protective strategy may reduce dynamic stability as previous studies have shown that walking at speeds slower than the usual (self-selected) speed decreases walking stability (27,28). Therefore, when concern about falls is excessive, the associated adaptive behaviors might actually increase falls risk, rather than protect against it.
Many studies have suggested that concern about falling has a detrimental effect on an older person's activity level and well-being, although their physical capacities are still sufficient for maintaining an active lifestyle (25). Further work is required in large samples of older people to determine whether behaviors associated with high levels of concern about falling, relative to the physiological falls risk, increase or decrease the risk of future falls. Future work should also address the limitations of the current study. Our sample comprised healthy older people and the findings may not generalize to frail older people. Further, it is possible that our experimental protocol, which required participant's left arm to be stabilized, and the use of a wired system may have influenced gait patterns.
In conclusion, these findings suggest that walking performance is influenced by both physiological and psychological factors. In older people, physiological falls risk appears to determine walking speed under optimal conditions, whereas concern about falling elicits greater gait adjustments under conditions of postural threat.
Acknowledgments
The participants in this study were drawn from the Memory and Ageing Study of the Brain and Ageing Program, School of Psychiatry, University of New South Wales, funded by an NH&MRC Program Grant (No. 350833) to Professors P. Sachdev, H. Brodaty, and G. Andrews. We are grateful to the many researchers involved in this study.
References
- 1.Chamberlin ME, Fulwider BD, Sanders SL, Medeiros JM. Does fear of falling influence spatial and temporal gait parameters in elderly persons beyond changes associated with normal aging? J Gerontol A Biol Sci Med Sci. 2005;60:1163–1167. doi: 10.1093/gerona/60.9.1163. [DOI] [PubMed] [Google Scholar]
- 2.Giladi N, Herman T, Reider-Griswasser, Gurevich T, Hausdorff JM. Clinical characteristics of elderly patients with a cautious gait of unknown origin. J Neurol. 2005;252:300–306. doi: 10.1007/s00415-005-0641-2. [DOI] [PubMed] [Google Scholar]
- 3.Rosengren KS, McAuley E, Mihalko SL. Gait adjustments in older adults: activity and efficacy influences. Psychol Aging. 1998;13:375–386. doi: 10.1037//0882-7974.13.3.375. [DOI] [PubMed] [Google Scholar]
- 4.Maki BE. Gait changes in older adults: predictors of falls or indicators of fear? J Am Geriatr Soc. 1997;45:313–320. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 5.Myers AM, Powell LE, Maki BE, et al. Psychological indicators of balance confidence: relationship to actual and perceived abilities. J Gerontol A Biol Sci Med Sci. 1996;51:37–43. doi: 10.1093/gerona/51a.1.m37. [DOI] [PubMed] [Google Scholar]
- 6.Brouwer B, Musselman K, Culham E. Physical function and health status among seniors with and without fear of falling. Gerontology. 2004;50:135–141. doi: 10.1159/000076771. [DOI] [PubMed] [Google Scholar]
- 7.Herman T, Giladi N, Gurevich T, Hausdorff JM. Gait instability and fractal dynamics of older adults with a cautious gait: why do certain older adults walk fearfully? Gait Posture. 2005;21:178–185. doi: 10.1016/j.gaitpost.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 8.Prince F, Corriveau H, Hebert R, Winter DA. Gait in the elderly. Gait Posture. 1997;5:128–135. [Google Scholar]
- 9.Lord SR, Menz HB, Tiedemann A. A physiological profile approach to falls risk assessment and prevention. Phys Ther. 2003;83:237–252. [PubMed] [Google Scholar]
- 10.Brown LA, Frank JS. Postural compensations to the potential consequences of instability: kinematics. Gait Posture. 1997;6:89–97. [Google Scholar]
- 11.Carpenter MG, Frank JS, Silcher CP. Surface height effects on postural control: a hypothesis for a stiffness strategy for stance. J Vestib Res. 1999;9:277–286. [PubMed] [Google Scholar]
- 12.Adkin AL, Frank JS, Carpenter MG, Peysar GW. Postural control is scaled to level of postural threat. Gait Posture. 2000;12:87–93. doi: 10.1016/s0966-6362(00)00057-6. [DOI] [PubMed] [Google Scholar]
- 13.Carpenter MG, Frank JS, Silcher CP, Peysar GW. The influence of postural threat on the control of upright stance. Exp Brain Res. 2001;138:210–218. doi: 10.1007/s002210100681. [DOI] [PubMed] [Google Scholar]
- 14.Adkin AL, Frank JS, Carpenter MG, Peysar GW. Fear of falling modifies anticipatory postural control. Exp Brain Res. 2002;143:160–170. doi: 10.1007/s00221-001-0974-8. [DOI] [PubMed] [Google Scholar]
- 15.Brown LA, Sleik RJ, Polych MA, Gage WH. Is the prioritization of postural control altered in conditions of postural threat in younger and older adults? J Gerontol A Biol Sci Med Sci. 2002;57:785–792. doi: 10.1093/gerona/57.12.m785. [DOI] [PubMed] [Google Scholar]
- 16.Carpenter MG, Adkin AL, Brawley LR, Frank J. Postural, physiological and psychological reactions to challenging balance: does age make a difference? Age Ageing. 2006;35:298–303. doi: 10.1093/ageing/afl002. [DOI] [PubMed] [Google Scholar]
- 17.Brown LA, Polych MA, Doan JB. The effect of anxiety on the regulation of upright standing among younger and older adults. Gait Posture. 2006;24:397–405. doi: 10.1016/j.gaitpost.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 18.Laufer YY, Barak Y, Chemel I. Age-related differences in the effect of a perceived threat to stability on postural control. J Gerontol A Biol Sci Med Sci. 2006;61:500–504. doi: 10.1093/gerona/61.5.500. [DOI] [PubMed] [Google Scholar]
- 19.Brown LA, Gage WH, Polych MA, Sleik RJ, Winder TR. Central set influences on gait—age-dependent effects of postural threat. Exp Brain Res. 2002;145:286–296. doi: 10.1007/s00221-002-1082-0. [DOI] [PubMed] [Google Scholar]
- 20.Gage WH, Sleik RJ, Polych MA, McKenzie NC, Brown LA. The allocation of attention during locomotion is altered by anxiety. Exp Brain Res. 2003;150:385–394. doi: 10.1007/s00221-003-1468-7. [DOI] [PubMed] [Google Scholar]
- 21.McKenzie NC, Brown LA. Obstacle negotiation kinematics: age-dependent effects of postural threat. Gait Posture. 2004;19:226–234. doi: 10.1016/S0966-6362(03)00060-2. [DOI] [PubMed] [Google Scholar]
- 22.Brown LA, Doan JB, McKenzie NC, Cooper SA. Anxiety-mediated gait adaptations reduce errors of obstacle negotiation among younger and older adults: implications for fall risk. Gait Posture. 2006;24:418–423. doi: 10.1016/j.gaitpost.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 23.Home page for the World Health Organization Disability Assessment Schedule II (WHODAS II) Available at http://www.who.int/icidh/whodas/index.html April 16, 2008. [Google Scholar]
- 24.Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I) Age Ageing. 2005;34:614–619. doi: 10.1093/ageing/afi196. [DOI] [PubMed] [Google Scholar]
- 25.Legters K. Fear of falling. Phys Ther. 2002;82:264–272. [PubMed] [Google Scholar]
- 26.Winter DA, Petla AE, Frank JS, Walt SE. Biomechanical walking pattern changes in the fit and healthy elderly. Phys Ther. 1990;70:340–347. doi: 10.1093/ptj/70.6.340. [DOI] [PubMed] [Google Scholar]
- 27.Menz HB, Lord SR, Fitzpatrick RC. A structural equation model relating impaired sensorimotor function, fear of falling and gait patterns in older people. Gait Posture. 2007;25:243–249. doi: 10.1016/j.gaitpost.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 28.Latt MD, Menz HB, Fung VS, Lord SR. Walking speed, cadence and step length are selected to optimize the stability of head and pelvis accelerations. Exp Brain Res. 2008;184:201–209. doi: 10.1007/s00221-007-1094-x. [DOI] [PubMed] [Google Scholar]