Abstract
Limited research has examined the ways in which changes in self-rated health experienced by aging spouses affect depressive symptoms of both members of the dyad. Longitudinal data from 315 older couples in which one partner had end-stage renal disease were analyzed using multilevel modeling. Results indicate that for both patients and spouses, own mean self-rated health was associated with own depressive symptoms, and change in self-rated health had a significant negative association with change in own depressive symptoms. Both mean self-rated health of the patient and change in patient's self-rated health had negative relationships with spouse depressive symptoms, with changes in patient's self-rated health having a stronger impact on spouse depressive symptoms than changes in spouse's own self-rated health. Results suggest the importance of understanding physical and mental health in the context of the marital dyad.
Keywords: Depressive symptoms, Marital dyad, Multilevel models, Self-rated health
THERE is compelling evidence that the emotional well-being (Bookwala & Schulz, 1996; Butterworth & Rodgers, 2006; Goodman & Shippy, 2002; Meyler, Stimpson, & Peek, 2007; Peek, Stimpson, Townsend, & Markides, 2006; Siegel, Bradley, Gallo, & Kasl, 2004; Tower & Kasl, 1995, 1996a, 1996b; Townsend, Miller, & Guo, 2001) and to some extent, the physical health (Bookwala & Schulz, 1996; Monden, van Lenthe, de Graff, & Kraaykamp, 2003; Peek & Markides, 2003; Speers, Kasl, Freeman, & Ostfeld, 1986) of spouses are similar to one another, yet the genesis of these effects remains largely unknown. In the later years of a marriage, with increased incidences of chronic illness making it likely that both spouses will experience threats to their own physical health, changes in the health of husband and wife should have important implications for the well-being of the self as well as the partner (Berg & Upchurch, 2007; Carstensen, Gottman, & Levenson, 1995; Goodman & Shippy, 2002; Revenson, Kayser, & Bodenmann, 2005). The analyses that follow are among the first to use multilevel models to examine longitudinal patterns of self-rated health and depressive symptoms of older couples, investigating cross-partner effects across three points in time, while controlling for individual change.
Self-rated health, how healthy one feels, is a powerful cognition (Winter, Lawton, Langston, Ruckdeschel, & Sando, 2007) predicting mortality (Benyamini & Idler, 1999; Deeg & Bath, 2003; Idler & Benyamini, 1997; Schoenfeld, Malmrose, Blazer, Gold, & Seeman, 1994) and physical disability (Idler & Kasl, 1995) better than objective health indicators. Recent studies focusing on the dynamic aspect of self-rated health find that change in self-rated health is a stronger predictor of mortality than self-rated health measured either at baseline or at the most recent observation (Ferraco & Kelly-Morre, 2001; Han et al., 2005).
The relationship between self-rated health and depressive symptoms has been observed in a wide variety of cross-sectional studies (Han, 2002; Han, Small, & Haley, 2001; Molarius & Janson, 2002), yet the mechanisms and direction of causality remain enigmatic (Kosloski, Stull, Kercher, & Van Dussen, 2005). Building on conceptual work by Liang (1986) and Lewinsohn, Hoberman, Teri, and Hautzinger (1985), we posit that self-rated health is a precursor of depressive symptoms. Although few longitudinal studies have empirically tested the directionality of this relationship with sufficient times of measurement, Kosloski et al. (2005), using five waves of data from the Health and Retirement Survey, found that self-rated health had a modest but consistent statistically significant effect on depressive symptoms. In contrast, level of depressive symptoms did not predict self-rated health. Similar findings are reported by Aneshensel, Frerichs, and Huba (1984).
Research investigating the influence of cross-partner effects of self-rated health on depressive symptoms finds that they are significant in clinical samples (Coyne et al., 1987; Fultz et al., 2005) and in general community samples (Galbaud du Fort, Kovess, & Bouvin, 1994; McLeod, 1993). In one of the first studies of the relationship between spouse health and respondent depressive symptoms among older couples, Simonsick (1993) found that husbands’ physical health was associated with wives’ depressive symptoms. However, this study relied on wives’ reports of their husbands’ health. Using data collected separately from husbands and wives, Hagedoorn et al. (2001) found that one's own chronic diseases as well as the chronic diseases of the spouse were independently related to psychological distress among older women. More recently, Peek et al. (2006) found that both husbands’ and wives’ own self-rated health was associated with partner's self-rated health even after accounting for other's demographic, health, and stress characteristics, and Stimpson, Eschbach, and Peek (2007) found that the level of spouse's chronic conditions, but not own conditions, was significantly associated with higher levels of depressive symptoms.
In one of the few longitudinal studies to examine health characteristics of both members of the marital dyad, Wallhagen, Strawbridge, Shema, and Kaplan (2004) found that hearing loss of one spouse affected the well-being of the partner five years later. Similarly, Strawbridge, Wallhagen, and Shema (2007) found that vision problems of one partner had significant effects on the spouse's well-being and marital quality over a five-year period, independent of own vision problems.
THE CONTEXT OF END-STAGE RENAL DISEASE
End-stage renal disease (ESRD) provides an important lens through which to understand the relationship between changing health and depressive symptoms experienced by patients and their spouses. As in many chronic illnesses, patients with ESRD experience significant levels of depressive symptoms (Drayer et al., 2006; Finkelstein & Finkelstein, 2000; Lopes et al., 2002). ESRD is a chronic illness in which the kidneys permanently fail. According to the U.S. Renal Data System (2008), each year in the United States over 400,000 people with ESRD are treated with hemodialysis, a life-sustaining invasive treatment in which waste materials are removed from the blood through a machine, compensating for loss of kidney function.
There is evidence that ESRD affects the well-being of spouses as well as patients (Daneker, Kimmel, Ranich, & Peterson, 2001; Devins, Hunsley, Mandin, Taub, & Paul, 1997). Couples in which one partner has ESRD and is on hemodialysis must accommodate to an illness that requires patients to adhere to a strict treatment schedule. They also face health crises that are often unpredictable. In one of the few studies to examine the relationship between patient and spouse depressive symptoms in this population, Daneker et al. (2001) found a significant positive association between patient and spouse symptoms.
Our analyses address the following questions:
Do ESRD patients and their spouses experience similar patterns of change in depressive symptoms over time?
Are changes in ESRD patients’ and their spouses’ self-rated health associated with changes in their own depressive symptoms?
Are there cross-partner effects of self-rated health on depressive symptoms?
How do variables known to influence depressive symptoms affect patterns of change in these symptoms, controlling for self-rated health?
Based on existing literature, we posit that cross-partner effects of self-rated health on depressive symptoms will be greater when patients are men (Wallhagen et al., 2004; Strawbridge et al., 2007), on dialysis for shorter periods of time (Kimmel, Cukor, Cohen, & Peterson, 2007), and when couples are Black (Skarupski et al., 2005), older (Fiske, Gatz, & Pedersen, 2003), married for longer periods of time (Proulx, Helms, & Buehler, 2007), and have more health conditions (Mills, 2001). It is particularly important to understand the nature of the associations between self-rated health and depressive symptoms in couples in later life because these characteristics have known associations with morbidity and mortality (Blazer, 2003; DeSalvo, Bloser, Reynolds, He, & Muntner, 2006; Idler & Benyamini, 1997; Reynolds, Haley, & Kozlenko, 2008), even after controlling for demographic and clinical characteristics.
METHODS
Sample
The Opinions and Preferences for Treatment in Older Nephrology Patients and Spouses (OPTIONS) study was designed to gain better understanding of the preferences for end of life treatment within the context of the marital dyad. Participants were recruited through advertisements in newspapers and newsletters, referral from staff at dialysis centers, and a one-time mailing to a random sample of beneficiaries receiving financial assistance for dialysis treatment from the Centers for Medicare and Medicaid Services. Preliminary analyses revealed that participants identified through various recruitment strategies did not significantly differ on any of the focal variables in the current research. More detailed information regarding recruitment is described in Feild, Pruchno, Bewley, Lemay, and Levinsky (2006). Data were collected from a national sample between May 2001 and June 2006.
Inclusion criteria stipulated that patients be 55 years of age or older, receiving hemodialysis for at least 6 months, and married or partnered, cohabitating for at least 5 years. Age was a criterion both because older people represent a growing segment of the ESRD population and because it is within this age group that decisions about withdrawal from dialysis are most common. Both the patient and the spouse had to agree to participate. Patients and spouses had to be English speaking and free of cognitive, hearing, and speech impairments that would preclude their ability to answer questions on the phone. Cognitive status was determined using the Short Portable Mental Status Questionnaire (Pfeiffer, 1975). More than 50% incorrect responses (five or more errors) rendered a person ineligible. Hearing and speech abilities were considered adequate if the screener was able to successfully complete the screening process. Similar screens for cognitive, hearing, and speech abilities were used at each follow-up.
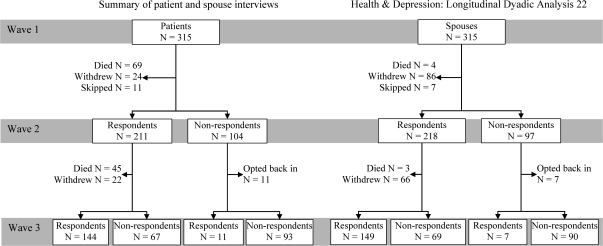
Each patient and his or her spouse completed a baseline interview (Time 1), and each was subsequently contacted for telephone interviews 12 (Time 2) and 24 months (Time 3) following the initial interview. Information about the number of people completing interviews at each time of assessment is presented in Figure 1. Results from analyses contrasting couples who completed the final interview (N = 145), those in which the patient died during the course of the study (N = 114), and those in which the patient, spouse, or both persons voluntarily withdrew from the study (N = 56) revealed that there were no statistically significant differences among the three groups at baseline in terms of patient gender, χ2(2, N = 315) = 3.88, time on hemodialysis, F(2, 309) = 0.07, number of years married, F(2, 312) = 1.03), income F(2, 261) = 0.46, patient age, F(2, 312) = 1.84, spouse age, F(2, 312) = 2.27, spouse education, F(2, 310) = 1.93, and spouse depressive symptoms, F(2, 312) = 0.61. There were statistically significant differences among the groups on patient education, F(2, 311) = 3.77, p = .02, race, χ2(2, N = 315) = 8.02, p = .02, patient depressive symptoms, F(2, 311) = 3.70, p = .03, patient subjective health, F(2, 312) = 7.24, p = .001, and spouse subjective health, F(2, 312) = 3.64, p = .03. Couples completing the final interview included better educated patients and fewer Black couples than either those in which patient died or the couple withdrew. Those completing the final interview included patients who were less depressed and those reporting better health than couples in which the patient died. Couples who withdrew included spouses reporting poorer health than those in which the patient died. Table 1 presents baseline demographic characteristics of the sample.
Figure 1.
Summary of patient and spouse interviews.
Table 1.
Respondent Baseline Demographic Characteristics (N = 315 patients and 315 spouses)
| M (SD) | Minimum | Maximum | |
| Patient age (years) | 69.8 (8.2) | 55 | 91 |
| Spouse age (years) | 67.9 (9.0) | 38 | 87 |
| Patient education (years) | 14.2 (3.2) | 3 | 20 |
| Spouse education (years) | 13.7 (2.6) | 3 | 20 |
| Years married | 41.2 (13.2) | 2 | 64 |
| Household income (annual) | $43,942 ($26,090) | $1,500 | $110,000 |
| Time on hemodialysis (months) | 70.8 (65.4) | 6 | 418 |
| Patient sex (female, %) | 27 | ||
| Patient race (White, %) | 85.1 | ||
| Spouse race (White, %) | 85.1 | ||
| Patient race (African American, %) | 10.8 | ||
| Spouse race (African American, %) | 10.5 |
Procedures and Measures
Data were obtained from structured individual interviews conducted by telephone. Prior to conducting each interview, the verbal informed consent process approved by the University of Medicine and Dentistry of New Jersey's institutional review board was reviewed. Respondents were told that participation was voluntary, that information would be treated confidentially, and that they could refuse to answer any question or discontinue the interview at any time. In order to protect confidentiality, patients and spouses were interviewed separately by different interviewers. Participants were asked to refrain from sharing their responses with their spouses. The mean time lapse between individual patient and spouse interviews was 6.77 days (SD = 21.60) at Time 1, 11.69 days (SD = 19.36) at Time 2, and 8.97 days (SD = 20.49) at Time 3.
Self-reported depressive symptomatology experienced by patients and spouses was measured with the 20-item Center for Epidemiologic Studies–Depression Scale (CESD). The instrument was administered and scored (each item was rated from 0 to 3) according to the procedures suggested by Radloff (1977), with higher scores indicating more depressive symptoms. Cronbach's alpha for patients ranged from .82 to .86 and those for spouse ranged from .87 to .88.
Patient and spouse self-rated health was assessed by asking each: “In general, would you say your health is: excellent (5), very good (4), good (3), fair (2), or poor (1)?”
Overview of Analyses
Data were analyzed using the multivariate two-level model for longitudinal data (Lyons & Sayer, 2005a, 2005b; Lyons, Sayer, Archbold, Hornbrook, & Stewart, 2007; Raudenbush, Brennan, & Barnett, 1995) enabling simultaneous estimation of the unique effects for each dyad member as well as cross-partner effects while controlling for interdependencies in the data. These effects, if not adequately modeled, may lead to misleading or incomplete understanding of self-reported depressive symptomatology in couples (Davey, Fincham, Beach, & Brody, 2001).
A means-only model, followed by a model assessing the effects of time, was tested. Because analyses provided support for modeling the effect of time using the linear model (compared with the means-only model, χ2(9) = 24.7, p < .004, we adopted it as the baseline model. Self-rated health was included as a time-varying covariate with the model specified as follows:
 |
(1) |
Ytp is the depressive symptom score Y(t = 1, … k outcome responses per dyad and time of measurement) for dyad p; β1p and β4p represent the intercepts for patient and spouse; β2p and β5p represent the time effect (linear) for the patient and spouse of self-reported depressive symptomatology. The indicator variable (patient) takes on a value of “1” if the outcome response was obtained from a patient and “0” if it was obtained from a spouse (the opposite is true for the spouse indicator variable).
The values represented by β3p and β6p are the time-varying self-rated health scores for the patient and spouse, respectively. Within-person centering, deviations at each point of measurement of each individual's health score from own mean health score (averaged over three points of measurement), was used to create the time-varying components (Raudenbush et al., 1995; Singer and Willett, 2003). These deviations capture the fluctuations in the individual's self-rated health over the 2 years of the study. The time-invariant component of the self-rated health scores is the degree to which mean health averaged over time (three measurement points) relates to mean depressive symptoms (modeled at Level 2 grand mean centered).
The six Level 1 coefficients (β1p … β6p) can take on different magnitudes within and across dyads and serve as Level 2 outcomes in subsequent analyses. The between-dyad model provides estimates of the population averages for the intercept (,10) and linear change (,20) in depressive symptoms for the patient and for the intercept (,40) and linear rate of change (,50) in depressive symptom change for the spouse. Mean self-rated health is included at Level 2 with ,11 and ,41 representing the effect of each individual's mean health on own level of mean depressive symptoms. As β3p and β6p represent fluctuations in self-rated health for the patient and spouse, respectively, ,30 and ,60 capture the average time-varying effect of health across dyads. The random effects (u1p, u2p, u4p, u5p) represent the deviation of each member from the average intercept and linear effect for patient and spouses, respectively. Significant variability in these parameters indicates that the introduction of additional predictors is appropriate in an effort to explain the variability.
Random effects for the time-varying covariates (,30 and ,60 are specified as fixed) (Lyons et al., 2007; Singer and Willett, 2003) were not included because we did not a priori have reason to expect residual random variation in these components. Moreover, only three waves of data boundary constraints may make reliable detection of inter-dyad fluctuations suspect (Singer & Willett, 2003, p. 169).
The initial explanatory Level 2 model was
| (2) |
| (3) |
| (4) |
| (5) |
| (6) |
| (7) |
After testing models including the effect of the individual's own self-rated health on his or her own depressive symptomatology, we tested for cross-partner effects. This model included the additional time-varying covariates (Level 1) representing (a) the effect of patient self-rated health on spouse depressive symptoms and (b) the effect of spouse self-rated health on patient depressive symptoms and the time-invariant effects (Level 2) representing (c) the effect of mean patient self-rated health on mean spouse depressive symptoms and (d) the effect of mean spouse self-rated health on mean patient depressive symptoms.
Additional Level 2 predictors (sex, race, age, length of time on ESRD treatment, length of time married, number of own health conditions; last four variables all grand mean centered) were assessed. Models were estimated using full information maximum likelihood (FIML) via HLM 6.04 (Raudenbush, Bryk & Congdon, 2004) using all available data from all patients and spouses. Multivariate hypothesis testing was conducted in the hierarchical linear modeling (HLM) context to examine differences in patient and spouse initial status and rates of change over time on self-reported depressive symptomatology. These tests were also used to examine differences in the strength of the relationship between patient and spouse self-rated health and self-reported depressive symptomatology. Multivariate hypotheses control the Type I error rate and have a large sample chi-square distribution (Raudenbush & Bryk, 2002).
RESULTS
Do ESRD Patients and Their Spouses Experience Similar Patterns in Depressive Symptoms Over Time?
Over the course of the study, patient mean depressive symptoms increased from 9.5 (SD = 8.2) at baseline to 8.7 (SD = 7.1) at Time 2 to 10.1 (SD = 7.3) at Time 3. Spouse mean depressive symptoms increased from 8.7 (SD = 8.2) at baseline to 8.9 (SD = 7.1) at Time 2 to 9.7 (SD = 8.2) at Time 3. Means for patient self-rated health were 2.8 (SD = 1.1), 2.8 (SD = 1.0), and 2.7 (SD = 1.0) and those for spouses were 3.6 (SD = 1.1), 3.4 (SD = 1.0), and 3.4 (SD = 1.0). Examination of the bivariate correlations depicted in Table 2 indicates that the correlations between depressive symptoms experienced by patients and their spouses were significant, yet modest across time (0.23 at Time 1, 0.17 at Time 2, and 0.18 at Time 3).
Table 2.
Correlations Between Patient and Spouse Depressive Symptoms and Health at Each Time of Measurement
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| (1) Baseline patient CESD | 1.00 | |||||||||||
| (2) Baseline spouse CESD | 0.23*** | 1.00 | ||||||||||
| (3) Baseline patient health | −0.28*** | −0.15** | 1.00 | |||||||||
| (4) Baseline spouse health | −0.04 | −0.20*** | −0.04 | 1.00 | ||||||||
| (5) 12-month patient CESD | 0.62*** | 0.10 | −0.21** | −0.05 | 1.00 | |||||||
| (6) 12-month spouse CESD | 0.34*** | 0.66*** | −0.14* | −0.17* | 0.17* | 1.00 | ||||||
| (7) 12-month patient health | −0.22*** | −0.14* | 0.50*** | 0.12 | −0.27*** | −0.13 | 1.00 | |||||
| (8) 12-month spouse health | −0.09 | −0.22*** | 0.02 | 0.65*** | 0.01 | −0.29*** | 0.14* | 1.00 | ||||
| (9) 24-month patient CESD | 0.50*** | 0.07 | −0.13 | −0.13 | 0.54*** | 0.19* | −0.09 | −0.19* | 1.00 | |||
| (10) 24-month spouse CESD | 0.22** | 0.58*** | −0.09 | −0.29*** | 0.13 | 0.60*** | −0.05 | −0.32*** | 0.18* | 1.00 | ||
| (11) 24-month patient health | −0.23** | −0.10 | 0.53*** | 0.21** | −0.17* | −0.03 | 0.53*** | 0.16 | −0.29*** | −0.08 | 1.00 | |
| (12) 24-month spouse health | −0.10 | −0.23** | 0.00 | 0.68*** | −0.12 | −0.21** | 0.10 | 0.61*** | −0.22** | −0.28*** | 0.13 | 1.00 |
Notes: CESD = Center for Epidemiologic Studies–Depression Scale. *p < .05; **p < .01; ***p < .001.
Columns 1 and 2 of Table 3 are the FIML estimates and standard errors for the linear model. There was a significant positive linear slope for depressive symptoms for both patients (,20 = 0.72, p < .05) and spouses (,50 = 0.49, p < .05), with an increase in depressive symptomatology of 1.4 (0.72 patient beta multiplied by 2 for the 2 years) and 0.98 (0.49 patient beta multiplied by 2 for the 2 years) on average for patients and spouses, respectively, over the 2 years. A multivariate hypothesis test suggests that the rate of increase in patient depressive symptoms was not significantly greater than that for the spouses, χ2(1) = 0.45, p > .05. Moreover, there is significant variation around the average depressive symptom scores for patients (u1p = 39.8, p < .001) and spouses (u4p = 45.2, p < .001). Variation around the average trajectory for change in depressive symptoms was not significant for either patients (u2p = 2.4) or spouses (u5p = 2.7). Tau correlations indicate a modest association between average patient and spouse depressive symptoms (0.37) and a strong correlation between the linear rates of change for patient and spouse depressive symptoms (0.74).
Table 3.
Multilevel Models Predicting Patient and Spouse Depressive Symptoms With Own and Cross-Partner Health
| Time (Linear) Only |
Own Health |
Own and Cross-Partner Health |
||||
| Patient |
Spouse |
Patient |
Spouse |
Patient |
Spouse |
|
| Parameter Estimate (SE) | Parameter Estimate (SE) | Parameter Estimate (SE) | Parameter Estimate (SE) | Parameter Estimate (SE) | Parameter Estimate (SE) | |
| Fixed effects | ||||||
| Intercept | 9.04 (0.52)*** | 9.02 (0.54)*** | 9.2 (0.50)*** | 9.1 (0.56)*** | 9.2 (0.52)*** | 9.2 (0.52)*** |
| Time | 0.72 (0.27)* | 0.49 (0.21)* | 0.57 (0.25)* | 0.36 (0.28) | 0.58 (0.28)* | 0.21 (0.28) |
| Patient mean health | −1.4 (0.49)*** | −1.6 (0.44)*** | −0.84 (0.44)* | |||
| Spouse mean health | −1.8(0.57)*** | −0.47 (0.43) | −1.9 (0.54)*** | |||
| Patient time-varying health | −1.6 (0.37)*** | −1.5 (0.38)*** | −1.3 (0.38)*** | |||
| Spouse time-varying health | −0.93 (0.45)* | −0.14 (0.43) | −1.0 (0.43)* | |||
| Covariate own health conditions | 1.11 (0.18)*** | 0.82 (0.22)*** | 0.90 (0.20)*** | 0.33 (0.29) | 0.89 (0.19)*** | 0.24 (0.26) |
| Random effects | ||||||
| Residual | 22.3 (1.6) | 22.0 (1.6) | 21.6 (1.6) | |||
| Intercept | 39.8 (5.0)*** | 45.2 (5.4)*** | 37.2(5.1) *** | 43.7 (5.3)*** | 37.5 (4.8)*** | 41.2 (5.1)*** |
| Time | 2.4 (1.7) | 2.7 (1.6) | 1.5 (1.6) | 2.8 (.1.7) | 2.2 (1.7) | 1.8 (1.7) |
| Estimated parameters | 27 | 31 | 35 | |||
| Deviance statistic | 9033.4 | 8992.7 | 8723.0 | |||
| Model comparison χ2(df) | 24.7 (9)*** | 40.8 (4)*** | 269.6 (4)*** | |||
Notes: The linear model deviance statistic is computed in reference to the means-only model, data not shown. The “own health” model was compared with the deviance statistic from the linear model. The “cross-partner health” model was compared with the deviance statistic from the own health model. All models run with covariates included age, length of time married, sex, race (Black), time on hemodialysis, and number of health conditions.
*p < .05; **p < .01; ***p < .001. Full information maximum likelihood, HLM 6.0.
Are Changes in ESRD Patients and Their Spouses’ Self-Rated Health Associated With Changes in Their Own Depressive Symptoms?
Columns 3 and 4 of Table 3 are the FIML estimates and standard errors for the own health only multilevel model. They reveal that there was a significant association between own mean self-rated health and depressive symptoms for both patients (,11p = −1.4, p < .001) and spouses (,41p = −1.8, p < .001). Decline in own self-rated health was associated with an increase in own depressive symptoms for both patients (,30p = −1.6, p < .001) and spouses (,60p = −0.93, p < .05). Multivariate hypotheses testing suggests that the magnitude of the mean, χ2(1) = 0.34, p > .50, and time-varying, χ2(1) = 0.13, p > .25, self-rated health associations were not significantly different for patients and spouses. This model finds an average depressive symptom score for patients of 9.2 and an increase in that score of 0.57 each year of the study (1.14 increase in CESD score over 2 years). It also indicates that better average health reduces depressive symptoms (−1.4 on CESD score), as does better health over time (−1.6 on CESD score). For the spouses, the average depressive symptom score was 9.1. They experienced nonsignificant increase in that score of 0.36 each year of the study. The model indicates that for spouses, better average health reduces depressive symptoms (−1.8 on CESD score), as does better health over time (−0.93 on CESD score).
Are There Cross-Partner Effects of Self-Rated Health on Depressive Symptoms?
Columns 5 and 6 of Table 3 are the FIML estimates and standard errors for the multilevel model, including own and cross-partner self-rated health. These analyses revealed that for patients, own mean self-rated health (,11p = –1.6, p < .001) was associated with their own mean depressive symptoms, but the mean self-rated health of the spouse (,12p = −0.47, p > .05) was not associated with mean patient depressive symptoms. For spouses, both their own mean self-rated health (,41p = –1.9, p < .001) and the mean self-rated health of the patient (,22p = −0.84, p < .05) were associated with mean depressive symptoms, this latter relationship representing a cross-partner effect.
For patients (,30p = –1.5, p < .001) as well as for spouses (,60p = –1.0, p < .05), decline in own self-rated health was associated with an increase in own depressive symptoms. Changes in spouse self-rated health were not significantly associated with changes in patient depressive symptoms (,61p = −0.14, p > .05). In contrast, declines in patient self-rated health were significantly associated with an increase in spouse depressive symptoms (,31p = −1.3, p < .001), representing another cross-partner effect. Multivariate hypothesis testing suggests that mean spouse self-rated health (,41p = −1.9) is more strongly related to spouse depressive symptoms than is mean patient self-rated health (,12p = −0.84), χ2(2) = 20.6, p < .01. These findings suggest that declines in patient self-rated health (,31p = −1.3) are more strongly related to increases in spouse depressive symptoms than are declines in spouse's own self-rated health (,60p = –1.0), χ2(1) = 3.8, p < .05.
How Do Variables Known to Influence Depressive Symptoms Affect Patterns of Change in These Symptoms, Controlling for Self-Rated Health?
Number of own health conditions was significant for the patient in the means-only (b = 1.09, p < .001), linear (b = 1.11, p < .001), own (b = 0.90, p < .001), and cross-partner (b = 0.89, p < .001) models. Analysis of other Level 2 variables indicated that patient's sex, t(303) = 0.94, p > .05, race, t(303) = 0.49, p > .05, age, t(303) = 0.42, p > .05, length of time on hemodialysis, t(303) = 0.0003, p > .05, and length of time married, t(303) = 0.008, p > .05, were not significantly associated with patient mean depressive symptoms in any model tested. For the spouses, number of own health conditions was significant in the means-only (b = 0.80, p < .01) and linear (b = 0.82, p < .001) models. Spouse sex, t(303) = −1.3, p > .05, race, t(303) = −0.92, p > .05, age, t(303) = 0.69, p > .05, patient's length of time on ESRD treatment, t(303) = −0.38, p > .05, and length of time married, t(303) = −1.7, p > .05, were not significantly associated with mean spouse depressive symptoms in any model tested. In sum, number of health conditions was the sole moderating variable consistently related to depressive symptoms.
DISCUSSION
These analyses are among the first to simultaneously examine the longitudinal relationship between self-rated health and depressive symptoms reported by patients with ESRD and their spouses using data collected from both individuals and analyses that account for the paired nature of the data. Consistent with earlier research (Bookwala & Schulz, 1996; Daneker et al., 2001; Townsend et al., 2001), we find a positive association between the levels of depressive symptoms experienced by patients and their spouses. Moreover, our data, in contrast to those reported by Druley, Stephens, Martire, Ennis, and Wojno (2003), indicate that there is a strong, positive, and stable association in the rate of change in level of depressive symptoms experienced by patients and their spouses. The average levels of depression in the patients (9.04) and spouses (9.02) do not meet standard cutoffs for clinical levels of depression. However, the significant variation in average depressive symptoms and the fact that some patients and spouses scored in the maximum range on the CESD suggest that the risk of serious emotional difficulty exists.
Not surprisingly, our analyses find that own mean self-rated health was associated with own mean depressive symptoms for both patients and spouses. Moreover, change in own self-rated health over time had a significant negative association with change in own level of depressive symptoms for both patients and spouses. These findings are consistent with the report of Aneshensel, Frerichs, and Huba (1984) that illness has a large, contemporaneous effect, increasing depressive symptomatology over previous levels, and that depressive symptoms have a smaller, lagged effect on health. The negative association that we found between health and depressive symptoms held even after controlling for the effect of the partner's health.
The pattern of cross-partner effects in our data is important. For patients, the mean health of their spouse was not associated with depressive symptoms. Moreover, changes in spouse's health over time were not associated with patient depressive symptoms. However, both mean health of the patient and changes in the patient's health over time had significant negative relationships with spouse depressive symptoms. Most important is the finding that changes in patient's health had a stronger impact on spouse depressive symptoms than did changes in spouse's own health. These cross-partner effects suggest that for spouses, not only is their own health an important predictor of their depressive symptoms but so too is the health experienced by their partner.
This finding is notable for two reasons. First, few studies have modeled patient and spouse health and depressive symptoms simultaneously over time using methods that control for the interdependencies in the data. Second, unlike many studies, ours includes a non-demented sample of patients. In the situation where the patient is deteriorating cognitively, the unidirectional influence of the patient's deteriorating state is readily understood. Our data shed light on marital dyads in which neither partner suffers from cognitive impairment and find that even in these situations, the spouse bears the brunt not only of his or her own health but also that of the patient. The patient, on the other hand, suffers no additional negative impact from fluctuations in the spouse's health. These analyses suggest that examining both enduring and fluctuating effects of the health experienced by patients and spouses on depressive symptoms increases our understanding of the contextual nature of the marital relationship.
Our findings add to the burgeoning literature supporting the critical role played by self-rated health. That self-rated health maintains its central role in our analyses even controlling for number of chronic illnesses experienced by patients and spouses speaks to its independent and powerful effects. It also adds to a rich and growing literature, suggesting that clinicians can rely on self-rated health to provide important and unique information regarding patient health status (Idler & Benyamini, 1997; Winter et al., 2007).
Although the direction of the hypotheses we sought to test was based on our interest in how the complexities of self-rated health predict depressive symptoms, the combination of empirical evidence suggesting that depressive symptoms may affect self-rated health (Han, 2002; Han & Jylha, 2006; Miller et al., 1996) and our available data enabled us to test a series of models in which self-rated health of patients and of spouses were the outcomes, and depressive symptoms the predictors. These analyses yielded findings similar to those reported in Table 3, with own depressive symptoms predicting own self-rated health for both patients and spouses. However, neither the mean nor time-varying cross-partner effects from patient to spouse were significant. Because we did not capture our couples at a signature point in time (e.g., the beginning of the relationship, beginning of the illness), our data are characterized by irresolvable endogenaity, a circumstance that does not afford us the opportunity to disentangle the causal flow between self-reported health and depressive symptoms.
Although our data provide evidence of significant variation around the average experience of depressive symptoms for both patients and spouses, the covariates we tested were not significant. This may be due to the relatively homogeneous nature of our sample (predominantly white couples in long-term marriages), as Townsend et al. (2001) found that the effects of similar covariates varied as a function of the ethnic makeup of the sample. Future studies measuring both individual- and couple-level covariates will advance knowledge regarding the cause of the significant relationship between patient and spouse depressive symptoms.
Although these findings are provocative, there are limitations regarding the extent to which they can be generalized. First, the measure of self-rated health was a single item. Although this item is widely used and has been found to have high predictive power (Idler & Benyamini, 1997), it is not clear whether a multi-item scale would have produced different results. Our reliance on the CESD as a measure of depressive symptoms requires caution both because it is a self-report measure and because it includes somatic symptoms (e.g., poor appetite, restless sleep) that may be confounded with symptoms of ESRD. Second, it is not clear whether findings from this sample of patients, which was disproportionately male and white, would generalize to the more ethnically diverse population of patients with ESRD, to samples consisting of more women with ESRD, or to samples in which patients had conditions other than ESRD. Third, because patients had been married for close to 40 years and had been on dialysis for an average of 7 years when the study began, questions could be raised regarding why changes in depressive symptoms should be experienced for this sample of chronically ill patients and their spouses. Because the inception of the study was not timed to capture a specific health event or crisis, there was really no defined start point from which to examine change in depressive symptoms. Moreover, because the study followed couples for only a 2-year window, we are unable to conclude that these changes in depressive symptoms represent true linear increases in depressive symptoms that would be expected to continue at a similar rate moving forward in time or that they are temporal fluctuations which trend upward due to the difficult nature of the disease condition. Finally, inclusion of data from couples at only three points in time makes it difficult to understand trends characterizing the data.
Future research could address some of the limitations of this study by following dyads coping with chronic illness for longer periods of time. Moreover, studies that included more closely spaced times of measurement could provide added insight regarding how changes in one spouse's health affect outcomes experienced by the other spouse. Finally, greater insight into the ways in which the physical and mental health of spouses are connected could be increased by designing a study that would capture a meaningful start point to a chronic health experience and examining the effects of this illness on both spouses over time.
Results from this study have important clinical implications, as they suggest the importance of considering the partner when treating an older person with chronic illness. Although the current medical model focuses almost exclusively on the patient, these analyses suggest that the effects of poor health may go beyond the individual patient to affect the partner as well. As such, actively involving both members of the marital dyad in treatment and rehabilitation services is important.
As we seek to understand how chronic illnesses affect both patient and spouses of long-term marriages, it is critical that the integrity of the marital dyad be maintained at the levels of theory, data collection, and analysis. Although some research has begun to collect and analyze data at the level of the dyad (Lyons et al., 2007; Pruchno, Wilson-Genderson, & Cartwright, 2008; Wilson-Genderson, Pruchno, & Cartwright, 2008), there remains much to be learned, yet it is clear that advances made regarding multilevel modeling strengthen our ability to conduct such research. Research focused on explaining the mechanisms underlying the relationship between spouse well-being, for example, has only scratched the surface. Analyses focused on cross-partner effects are relatively new, yet they provide unique information regarding the complexities underlying long-term marriages. Studies that examine the ways in which husbands and wives affect one another's well-being, those focused on the ways in which characteristics of the marital dyad (e.g., marital satisfaction, cohesion, quality) affect couple well-being, and those examining how similar and discrepant perceptions held by husbands and wives affect outcomes are important directions to pursue.
FUNDING
This study was funded by a grant from the National Institute of Nursing Research (RO1 NR-05237).
Acknowledgments
The authors gratefully acknowledge Robert Brennan and David Kenny for input on the application of the dyadic longitudinal multilevel models.
References
- Aneshensel CS, Frerichs RR, Huba GJ. Depression and physical illness: A multiwave, nonrecursive causal model. Journal of Health and Social Behavior. 1984;25:350–371. [PubMed] [Google Scholar]
- Benyamini Y, Idler EL. Community studies reporting association between self-rated health and mortality. Research on Aging. 1999;21:392–401. [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Depression in late life: Review and commentary. Journal of Gerontology: Medical Science. 2003;58A:M249–M265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Schulz R. Spousal similarity in subjective well-being: The cardiovascular health study. Psychology and Aging. 1996;11:582–590. doi: 10.1037//0882-7974.11.4.582. [DOI] [PubMed] [Google Scholar]
- Butterworth P, Rodgers B. Concordance in the mental health of spouses: Analysis of a large national household panel survey. Psychological Medicine. 2006;36:685–697. doi: 10.1017/S0033291705006677. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Gottman JM, Levenson RW. Emotional behavior in long-term marriage. Psychology & Aging. 1995;10:140–149. doi: 10.1037//0882-7974.10.1.140. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Kessler RC, Tal M, Turnbull J, Wortman CB, Greden J. Living with a depressed person. Journal of Clinical and Consulting Psychology. 1987;55:186–193. doi: 10.1037//0022-006x.55.3.347. [DOI] [PubMed] [Google Scholar]
- Daneker B, Kimmel PL, Ranich T, Peterson RA. Depression and marital dissatisfaction in patients with end-stage renal disease and in their spouses. Journal of Kidney Disease. 2001;38:839–846. doi: 10.1053/ajkd.2001.27704. [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question: A meta-analysis. Journal of General Internal Medicine. 2006;21:267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey A, Fincham FD, Beach SRH, Brody GH. Attributions in marriage: Examining the entailment model in dyadic context. Journal of Family Psychology. 2001;15:721–734. doi: 10.1037//0893-3200.15.4.721. [DOI] [PubMed] [Google Scholar]
- Deeg DJH, Bath PA. Self-rated health, gender, and mortality in older persons: Introduction to a special section. The Gerontologist. 2003;43:369–371. doi: 10.1093/geront/43.3.369. [DOI] [PubMed] [Google Scholar]
- Devins GM, Hunsley J, Mandin H, Taub KJ, Paul LC. The marital context of end-stage renal disease: Illness intrusiveness and perceived changes in the family environment. Annals of Behavioral Medicine. 1997;19:325–332. doi: 10.1007/BF02895149. [DOI] [PubMed] [Google Scholar]
- Drayer RA, Piraino B, Reynolds CF, Houck PR, Mazumdar S, Bernardini J, Shear MK, Rollman BL. Characteristics of depression in hemodialysis patients: Symptoms, quality of life, and mortality risk. General Hospital Psychiatry. 2006;28:306–312. doi: 10.1016/j.genhosppsych.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Druley JA, Stephens MAP, Martire LM, Ennis N, Wojno WC. Emotional congruence in older couples coping with wives’ osteoarthritis: Exacerbating effects of pain behavior. Psychology and Aging. 2003;18:406–414. doi: 10.1037/0882-7974.18.3.406. [DOI] [PubMed] [Google Scholar]
- Feild L, Pruchno RA, Bewley J, Lemay EP, Levinsky NG. Using probability vs. non-probability sampling to identify hard-to-access participants for health-related research: Costs and contrasts. Journal of Aging and Health. 2006;18:565–583. doi: 10.1177/0898264306291420. [DOI] [PubMed] [Google Scholar]
- Ferraco KF, Kelly-Morre JA. Self-rated health and mortality among Black and White adults: Examining the dynamic evaluation thesis. Journals of Gerontology: Social Sciences. 2001;56B:S195–S205. doi: 10.1093/geronb/56.4.s195. [DOI] [PubMed] [Google Scholar]
- Finkelstein FO, Finklestein SH. Depression in chronic dialysis patients: Assessment and treatment. Nephrology Dialysis Transplantation. 2000;15:1911–1913. doi: 10.1093/ndt/15.12.1911. [DOI] [PubMed] [Google Scholar]
- Fiske A, Gatz M, Pedersen NL. Depressive symptoms and aging: The effects of illness and non-health related events. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2003;58:P320–P328. doi: 10.1093/geronb/58.6.p320. [DOI] [PubMed] [Google Scholar]
- Fultz NH, Jenkins KR, Ostbye T, Taylor DH, Kabeto MU, Langa KM. The impact of own and spouse's urinary incontinence on depressive symptoms. Social Science & Medicine. 2005:2537–2548. doi: 10.1016/j.socscimed.2004.11.019. [DOI] [PubMed] [Google Scholar]
- Galbaud du Fort G, Kovess G, Bouvin JF. Spouse similarity for psychological distress and well-being: A population study. Psychological Medicine. 1994;24:431–447. doi: 10.1017/s0033291700027409. [DOI] [PubMed] [Google Scholar]
- Goodman CR, Shippy RA. Is it contagious? Affect similarity among spouses. Aging and Mental Health. 2002;6:266–274. doi: 10.1080/13607860220142431. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Ranchor AV, Brilman EI, Kempen GI, Ormel J. Chronic disease in elderly couples: Are women more responsive to their spouses’ health condition than men? Journal of Psychosomatic Research. 2001;51:693–696. doi: 10.1016/s0022-3999(01)00279-3. [DOI] [PubMed] [Google Scholar]
- Han B. Depressive symptoms and self-rated health in community-dwelling older adults: A longitudinal study. Journal of the American Geriatrics Society. 2002;50:1549–1556. doi: 10.1046/j.1532-5415.2002.50411.x. [DOI] [PubMed] [Google Scholar]
- Han B, Jylha M. Improvement in depressive symptoms and changes in self-rated health among community-dwelling disabled older adults. Aging & Mental Health. 2006;10:599–605. doi: 10.1080/13607860600641077. [DOI] [PubMed] [Google Scholar]
- Han B, Phillips C, Ferrucci L, Bandeen-Roche K, Jylha M, Kasper J, Guralink JM. Change in self-rated health and mortality among community-dwelling disabled older women. The Gerontologist. 2005;45:216–221. doi: 10.1093/geront/45.2.216. [DOI] [PubMed] [Google Scholar]
- Han B, Small BJ, Haley WE. The structure of self-rated health among community-dwelling older adults with stroke. Home Health Care Services Quarterly. 2001;20:1–15. doi: 10.1300/J027v20n04_01. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Idler EL, Kasl SV. Self-ratings of health: Do they also predict change in functional ability? Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1995;50:S344–S353. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- Joiner T, Coyne J. The interactional nature of depression: Advances in interpersonal approaches. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- Kimmel PL, Cukor D, Cohen SD, Peterson RA. Depression in end-stage renal disease patients: A critical review. Advances in Chronic Kidney Disease. 2007;14:328–334. doi: 10.1053/j.ackd.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Kosloski K, Stull DE, Kercher K, Van Dussen DJ. Longitudinal analysis of the reciprocal effects of self-assessed global health and depressive symptoms. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60:P296–P303. doi: 10.1093/geronb/60.6.p296. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hoberman H, Teri L, Hautzinger M. An integrative theory of depression. In: Reiss S, Bootzin R, editors. Theoretical issues in behavior therapy. New York: Academic Press; 1985. pp. 331–359. [Google Scholar]
- Liang J. Self-reported health among aged adults. Journal of Gerontology. 1986;41:248–260. doi: 10.1093/geronj/41.2.248. [DOI] [PubMed] [Google Scholar]
- Lopes AA, Bragg J, Young E, Goodkin D, Mapes D, Combe C, Piera L, Held P, Gillespie B, Port FK. Dialysis Outcomes and Practice Patterns Study (DOPPS): Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney International. 2002;62:199–207. doi: 10.1046/j.1523-1755.2002.00411.x. [DOI] [PubMed] [Google Scholar]
- Lyons KS, Sayer AG. Longitudinal dyad models in family research. Journal of Marriage and the Family. 2005a;67:1048–1060. [Google Scholar]
- Lyons KS, Sayer AG. Using multilevel modeling in caregiving research. Aging and Mental Health. 2005b;9:189–195. doi: 10.1080/13607860500089831. [DOI] [PubMed] [Google Scholar]
- Lyons KS, Sayer AG, Archbold PG, Hornbrook MC, Stewart BJ. The enduring and contextual effects of physical health and depression on care-dyad mutuality. Research in Nursing & Health. 2007;30:84–98. doi: 10.1002/nur.20165. [DOI] [PubMed] [Google Scholar]
- McLeod JD. Spouse concordance for depressive disorders in a community sample. Journal of Affective Disorders. 1993;27:43–52. doi: 10.1016/0165-0327(93)90096-3. [DOI] [PubMed] [Google Scholar]
- Meyler D, Stimpson JP, Peek MK. Health concordance within couples: A systematic review. Social Science & Medicine. 2007;64:2297–2310. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Mills T. Comorbid depressive symptomatology: Isolating the effects of chronic medical conditions on self-reported depressive symptoms among community-dwelling older adults. Social Science & Medicine. 2001;53:569–578. doi: 10.1016/s0277-9536(00)00361-0. [DOI] [PubMed] [Google Scholar]
- Miller MD, Schulz R, Paradis C, Houck PR, Mazumdar S, Frank E, Dew MA, Reynolds CF. Changes in perceived health of depressed elderly patients treated until remission. American Journal of Psychiatry. 1996;153:1350–1352. doi: 10.1176/ajp.153.10.1350. 3rd. [DOI] [PubMed] [Google Scholar]
- Molarius A, Janson S. Self-rated health, chronic diseases, and symptoms among middle-aged and elderly men and women. Journal of Clinical Epidemiology. 2002;55:364–370. doi: 10.1016/s0895-4356(01)00491-7. [DOI] [PubMed] [Google Scholar]
- Monden CWS, van Lenthe F, de Graff ND, Kraaykamp G. Partner's and own education: Does who you live with matter for self-assessed health, smoking, and excessive alcohol consumption? Social Science & Medicine. 2003;57:1901–1912. doi: 10.1016/s0277-9536(03)00055-8. [DOI] [PubMed] [Google Scholar]
- Peek MK, Markides KS. Blood pressure concordance in older Mexican-American couples. Journal of the American Geriatrics Society. 2003;51:1655–1659. doi: 10.1046/j.1532-5415.2003.51520.x. [DOI] [PubMed] [Google Scholar]
- Peek MK, Stimpson JP, Townsend AL, Markides KS. Well-being in older Mexican American spouses. The Gerontologist. 2006;46:258–266. doi: 10.1093/geront/46.2.258. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. A Short Portable Mental Status Questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Proulx CM, Helms HH, Buehler C. Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family. 2007;69:576–593. [Google Scholar]
- Pruchno RA, Wilson-Genderson M, Cartwright FP. Depressive symptoms and marital satisfaction in the context of chronic disease: A longitudinal dyadic analysis. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Raudenbush SW, Brennan RT, Barnett RC. A multivariate hierarchical model for studying change within married couples. Journal of Family Psychology. 1995;9:161–174. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. Hierarchical linear and non-linear modeling. Lincolnwood, IL: SSI; 2004. [Google Scholar]
- Revenson TA, Kayser K, Bodenmann G. Couples coping with stress: Emerging perspectives on dyadic coping. Washington, DC: American Psychological Association; 2005. [Google Scholar]
- Reynolds SL, Haley WE, Kozlenko N. The impact of depressive symptoms and chronic diseases on active life expectancy in older Americans. American Journal of Geriatric Psychiatry. 2008;16:425–432. doi: 10.1097/JGP.0b013e31816ff32e. [DOI] [PubMed] [Google Scholar]
- Schoenfeld DE, Malmrose LC, Blazer DG, Gold DT, Seeman TE. Self-rated health and mortality in the high-functioning elderly—a closer look at healthy individuals: MacArthur field study of successful aging. Journal of Gerontology: Medical Sciences. 1994;49:M109–M115. doi: 10.1093/geronj/49.3.m109. [DOI] [PubMed] [Google Scholar]
- Siegel MJ, Bradley EH, Gallo WT, Kasl SV. The effect of spousal mental and physical health on husbands’ and wives’ depressive symptoms, among older adults: Longitudinal evidence from the Health and Retirement Survey. Journal of Aging and Health. 2004;16:398–425. doi: 10.1177/0898264304264208. [DOI] [PubMed] [Google Scholar]
- Simonsick E. Relationship between husband's health status and the mental health of older women. Journal of Aging and Health. 1993;5:319–337. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Skarupski KA, Mendes de Leon CF, Bienias JL, Barnes LL, Everson-Rose SA, Wilson RS, Evans DA. Black–White differences in depressive symptoms among older adults over time. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60:P136–P142. doi: 10.1093/geronb/60.3.p136. [DOI] [PubMed] [Google Scholar]
- Speers MA, Kasl SV, Freeman DH, Jr., Ostfeld AM. Blood pressure concordance between spouses. American Journal of Epidemiology. 1986;123:818–829. doi: 10.1093/oxfordjournals.aje.a114311. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Wallhagen MI, Shema SJ. Impact of spouse vision impairment on partner health and well-being: A longitudinal analysis of couples. Journals of Gerontology: Social Sciences. 2007;62B:S315–S322. doi: 10.1093/geronb/62.5.s315. [DOI] [PubMed] [Google Scholar]
- Stimpson JP, Eschbach I, Peek MK. Effect of immigrant status on risk of depressive symptoms associated with spouse's chronic conditions. Journal of Immigrant Health. 2007;9:29–34. doi: 10.1007/s10903-006-9012-z. [DOI] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses and the moderating effect of marital closeness. Psychology and Aging. 1995;10:625–638. doi: 10.1037//0882-7974.10.4.625. [DOI] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses: Longitudinal influences. Psychology and Aging. 1996a;11:683–697. doi: 10.1037//0882-7974.11.4.683. [DOI] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Gender, marital closeness, and depressive symptoms in elderly couples. Journals of Gerontology: Psychological Sciences. 1996b;51B:P115–P129. doi: 10.1093/geronb/51b.3.p115. [DOI] [PubMed] [Google Scholar]
- Townsend A, Miller B, Guo S. Depressive symptomatology in middle-aged and older married couples: A dyadic analysis. Journals of Gerontology: Psychological Sciences. 2001;56:S352–S364. doi: 10.1093/geronb/56.6.s352. [DOI] [PubMed] [Google Scholar]
- U.S. Renal Data System. Annual data report: Atlas of end-stage renal disease in the United States [data file] Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive Kidney Diseases; 2008. [Google Scholar]
- Wallhagen MI, Strawbridge WJ, Shema SJ, Kaplan G. Impact of self-assessed hearing loss on a spouse: A longitudinal analysis of couples. Journals of Gerontology: Social Sciences. 2004;59B:S190–S196. doi: 10.1093/geronb/59.3.s190. [DOI] [PubMed] [Google Scholar]
- Wilson-Genderson M, Pruchno RA, Cartwright FP. Effects of burden and satisfaction on psychological well-being of older ESRD patients and their spouses. 2008. [Google Scholar]
- Winter L, Lawton MP, Langston CA, Ruckdeschel K, Sando R. Symptoms, affects, and self-rated health: Evidence for a subjective trajectory of health. Journal of Aging and Health. 2007;19:453–469. doi: 10.1177/0898264307300167. [DOI] [PubMed] [Google Scholar]