Abstract
Objectives
Experience Corps (EC) places older volunteers in public elementary schools in 20 cities across the country. The EC program in Baltimore is a health promotion intervention designed to improve the academic outcomes of children and increase older adult volunteer physical activity. We sought to determine if there were sustained increases in physical activity with participation in EC.
Methods
Seventy-one African American women volunteers in the Baltimore EC were compared with 150 African American women in the Women's Health and Aging Studies (WHAS) I and II; all were aged 65–86 years with comparable Social Economic Status, frailty, and self-reported health status. Using a regression model, we evaluated physical activity adjusting for a propensity score and time of follow-up over 3 years.
Results
EC volunteers reported a sustained increase in physical activity as compared with the comparison cohort. Baseline physical activity for individuals with a median propensity score was 420 kcal/wk for both groups. At 36 months, EC volunteers reported 670 kcal/week compared with 410 kcal/week in WHAS (p = .04).
Discussion
These findings suggest that high-intensity senior service programs that are designed as health promotion interventions could lead to sustained improvements in physical activity in high-risk older adults, while simultaneously addressing important community needs.
Keywords: African Americans, Community-based participatory research, Elderly, Health disparity, Intergenerational social contract, Physical activity, Volunteerism, Women
PHYSICAL inactivity is a leading cause of preventable death (Mokdad, Marks, Stroup, & Gerberding, 2005), but, despite evidence that even moderate physical activity remains important to health outcomes through the oldest ages (Barnes, 2007; Nelson et al., 2007; Prohaska et al., 2006), 53% of Americans over the age of 65 years report no regular physical activity (Barnes, 2007). “Healthy People 2010,” a national public health framework designed to promote health and eliminate health disparities, identified older women, African Americans, Hispanics, and people with disabilities, lower incomes, and less education as at particular risk of low activity levels (Healthy People 2010: Understanding and Improving Health, 2000; King, Rejeski, & Buchner, 1998). As most successful physical activity interventions have recruited healthier and higher functioning individuals from more financially well off predominantly White communities (Katula et al., 2007; Stewart et al., 2001), health disparities are likely to continue or worsen unless new public health interventions specifically target individuals at highest risk (Adler, 2003). We must therefore develop, implement, and evaluate new community-based approaches that support a physically active lifestyle for all older adults, before the Baby Boom generation begins to retire en masse in 2010.
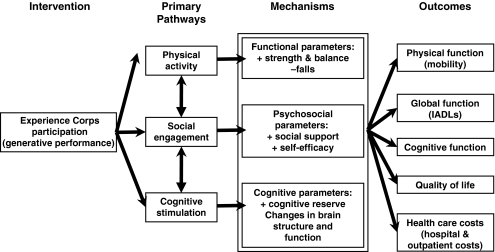
The Task Force on Community Preventive Services conducted a systematic review of “community interventions to increase physical activity” and strongly recommended approaches that (a) were community based, (b) promoted individually adapted behavioral change, (c) provided social support in the community setting, and (d) offered enhanced access to activity Centers for Disease Control and Prevention, 2001. These approaches were designed into the Baltimore Experience Corps (EC) program, which is an older adult public health intervention embedded in a community-based volunteer program that places older adults in the public elementary school system in support of improved academic outcomes for children (Fried, Carlson, et al., 2004; Glass et al., 2004; Martinez et al., 2006; Rebok et al., 2004; Tan, Xue, Li, Carlson, & Fried, 2006). The designers of the EC program theorized that a program that required 3–5 days of service a week during the school year (for a minimum of 15 hr a week) would promote physical activity through both travel to and from and activity within the school and that the increased social activity associated with volunteer participation would promote continued long-term adherence (see Figure 1; Fried, Carlson, et al.). The EC program in Baltimore has also demonstrated an ability to recruit and attract older African American women, suggesting that this model of public health intervention could potentially address an at-risk group of older adults (Fried, Carlson, et al., 2004).
Figure 1.
Conceptual framework of the Experience Corps Program (Fried, Carlson, et al., 2004).
The EC program in Baltimore is the first volunteer program to demonstrate short-term increases in physical activity (Fried, Carlson, et al., 2004; Tan et al., 2006). As previously published elsewhere, EC participants in a pilot trial of EC participation versus wait-listed controls reported increased physical activity over a 4- to 8-month follow-up, among the subgroup of participants who did not initially meet Healthy People 2010 physical activity goals (Tan et al., 2006). This report now seeks to determine if there were sustained increases in physical activity over time with continued participation in EC. To do this, we carefully evaluated a subset of the older African American women enrolled in EC, observed them longitudinally, and compared them with a matched group of African American women participating in a prospective observational cohort study in the same city, both with three years of follow-up.
METHODS
This report analyzes data from the Baltimore EC Extended Pilot Study, a longitudinal observational study of EC volunteers in Baltimore, Maryland as compared with similar women from the Baltimore Women's Health and Aging Study (WHAS) cohorts I and II.
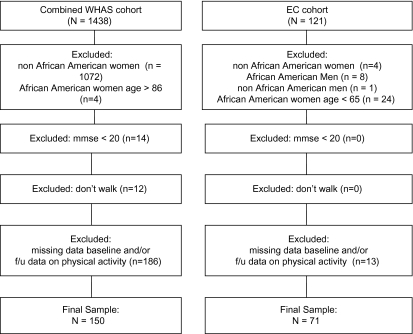
Volunteers were recruited for the Baltimore EC Extended Pilot Study over a two-year period. Eligibility requirements for EC included age ≥60 years, a Mini-Mental State Examination (MMSE) score >24 (or 20–23 among those with a high school education or less; Folstein, Folstein, & McHugh, 1975), a minimum fifth-grade reading level, and passing a criminal background check conducted by the Baltimore City Public School System. Recruitment strategies for the EC program's initial four years in Baltimore have been previously published (Martinez et al., 2006). Because 95% of the female EC volunteers aged 65 years and older were African American, we limited our analysis to African American women. Of the 112 EC participants of the Baltimore EC Extended Pilot Study, 84 were African American women aged 65 years or older. Of these 84 African American women, 13 women were excluded due to missing physical activity data, leaving 71 African American EC volunteers in this analysis, each participating in the study for three years (see Figure 2).
Figure 2.
Sample selection for the Experience Corps and Women's Health and Aging Cohorts.
WHAS I and II are longitudinal observational studies of older women in 12 Zip code areas in eastern Baltimore City and County selected through a stratified random sample from the Health Care Financing Administration Medicare eligibility files. From this sampling frame, WHAS I recruited 1,002 women aged 65 years and older who, at baseline in 1992, represented the one-third most disabled older women living in the community (Guralnik, Fried, Simonsick, Kasper, & Lafferty, 1995). WHAS II recruited 436 women initially from among the two-thirds least disabled women aged 70–79 years in the community and who had a baseline MMSE score of 24 or greater (Fried, Bandeen-Roche, Chaves, & Johnson, 2000). Of the 1,438 combined WHAS I and II participants, there were 366 African American women. Four women were excluded for being older than age 86 years, 14 women were excluded for an MMSE score <20, and 12 women were excluded because they were nonambulatory. Of those remaining, 186 African American women in the combined sample were missing physical activity data and were excluded from this analysis, leaving 150 African American WHAS study participants within the same age range as the EC participants (see Figure 2).
Details of data collection in the EC Pilot Trial and WHAS I and II have been previously published (Fried et al., 2000; Fried, Carlson, et al., 2004; Fried, Ferrucci, Darer, Williamson, & Anderson, 2004; Guralnik et al., 1995; Martinez et al., 2006). Standardized evaluations for follow-up were done every 6 months for WHAS I in the homes of participants, every 18 months for WHAS II in a field center, and for EC in a field center at baseline and the end of the academic school year. Measures in EC were standardized to WHAS. They included (a) self-reported age, race, education level, income, fatigue, physical activity, mobility difficulty, and health status; (b) self-reports of a physician diagnosis of any of 14 chronic diseases; and (c) objective measures of strength, walking speed, MMSE, height, weight, frailty (Bandeen-Roche et al., 2006; Fried et al., 2001), and fatigue.
The primary outcome, physical activity, was measured at baseline and follow-up in all studies using the modified Minnesota leisure time physical activity questionnaire (LTA) (Taylor, Jacobs, & Schuker, 1978), which measures the frequency and duration of participation, in the past two weeks, in physical activities that older adults are likely to engage in. We categorized these activities as walking, household chores (both outdoor and indoor), recreational activities (dancing and bowling), and exercise, and we calculated kilocalories expended per week based on the frequency of engagement, summarizing across activities (Taylor et al., 1978).
Analyses
An analysis, stratified by study assignment, was done comparing the baseline characteristics of the African American women who participated for three years in EC (n = 71) versus WHAS (n = 150). Physical activities were compared between the two groups, analyzing change from baseline to follow-up in log kilocalories expended per week to account for a nonnormal distribution. Mean physical activity per week was calculated as kilocalories per week using the geometric mean, which is the arithmetic mean of the logarithmically transformed values. Geometric means were used to discount the effect of outliers on the measurement of central tendency. In the initial analysis, baseline and three-year follow-up data were analyzed using an unadjusted t test. This initial analysis did not utilize the interval data collected between the baseline evaluation and the final three-year follow-up.
To utilize the multiple measurements of physical activity collected throughout the 36 months of follow-up, we developed an unadjusted GEE (generalized estimating equations) model of physical activity as measured by kilocalories per week as a function of WHAS versus EC membership. To account for differential distribution in observed baseline characteristics (including differences in age and baseline frailty) of participants enrolling in the two studies, we estimated the propensity score (Rosenbaum & Rubin, 1983) for enrolling in EC as a function of the following observed baseline characteristics: age, education, income range, marital status, health status, osteoarthritis, stroke, MMSE, mobility disability (as measured by difficulty walking several blocks), and frailty category (robust or prefrail) at baseline. When data were missing for items in the propensity score, an indicator variable was substituted for categorical and nominal variables, whereas mean data were substituted for continuous variables. This score has the property that among individuals with a common score value, those who enrolled in WHAS and those who enrolled in EC have the same distribution in all observed characteristics used in the propensity score. This property was checked empirically. After estimation of the score, we fitted a regression model of the probability of being physically active at follow-up as a function of WHAS versus EC membership (common effect across propensity score classes), adjusting for the propensity score and time of follow-up, with a working correlation matrix to capture the anticipated correlation of physical activity across time for a given individual. The model was chosen based on the log likelihood and goodness of fit confirmed through marginal model plots.
Results were stratified by four subcategories: (a) walking for exercise, (b) household chores, (c) exercise, and (d) recreational activity, and were analyzed using an unadjusted t test, the unadjusted model, and the adjusted model.
RESULTS
The characteristics of the older African American women who volunteered for WHAS or EC in Baltimore and were included in this analysis are shown in Table 1. EC participants were 65–86 years of age, with a mean age of 71 years, whereas WHAS participants were 65–86 years of age, with a mean age of 73 years. EC volunteers tended on average to have completed more years of education but had a lower average MMSE score than the WHAS participants. A higher percentage of the EC participants reported having excellent or very good health than did those who were participants in WHAS.
Table 1.
Baseline Characteristics of the Experience Corps and Women's Health and Aging Cohorts
| EC (n = 71) | WHAS (n = 154) | p Value | ||
| Age | Mean (SD) | 71.2 (4.3) | 73.0 (4.4) | .003 |
| Range | 65–86 | 65.0–86 | ||
| Gender | Female | 100% | 100% | — |
| Race | African American | 100% | 100% | — |
| Education | Mean highest grade completed (SD) | 11.2 (2.1) | 9.9 (3.5) | <.001 |
| High school or less | 86.9 | 84.7 | .66 | |
| Income categories | <$6,000 | 22.5 | 18.0 | .14 |
| $6,000 to <$8,000 | 11.3 | 16.0 | ||
| $8,000 to <$15,000 | 26.7 | 19.3 | ||
| ≥$15,000 | 25.4 | 19.3 | ||
| Missing | 14.1 | 27.3 | ||
| Income | <$15,000 per year | 72.7 | 76.6 | .55 |
| Marital status | Married | 14.1 | 22.7 | .14 |
| Mini-mental | Mean (SD) | 25.4 (2.6) | 27.1 (2.7) | <.001 |
| Health status (self-assessed) | Excellent | 16.2 | 6.1 | .04 |
| Very good | 29.4 | 23.0 | ||
| Good | 30.9 | 35.8 | ||
| Fair | 23.5 | 35.1 | ||
| Poor | — | — | ||
| Chronic diseases | Hypertension | 62.5 | 64.0 | .83 |
| Osteoarthritis | 56.5 | 69.3 | .06 | |
| Pulmonary disease | 9.1 | 12.1 | .52 | |
| Coronary heart disease | 8.9 | 13.3 | .36 | |
| Diabetes | 26.9 | 20.7 | .31 | |
| Cancer | 2.9 | 13.3 | .02 | |
| Stroke | 2.9 | 10.7 | .05 | |
| Parkinson's disease | 0 | 0.67 | .51 | |
| Mobility disability | Difficulty walking several blocks | 25.7 | 36.7 | .11 |
| IADL disability | Difficulty with any Instrumental Activity of Daily Livinga | 15.9 | 19.3 | .55 |
| Frailty at baseline | Frail | — | — | .96 |
| Prefrail | 61.7 | 61.3 | ||
| Nonfrail | 38.3 | 38.7 | ||
| Physical activity | Kcal/week (geometric means) | 760 | 550 | .09 |
Notes: EC = Experience Corps; WHAS = Women's Health and Aging Studies; IADL = instrumental activity of daily living; BL = baseline; SD = standard deviation.
Using a phone, shopping, preparing a meal, and managing medications or money.
Although African American women in EC reported higher mean physical activity at baseline as compared with the WHAS sample, this was not statistically significant. The mean physical activity among EC participants increased from an average 760 kcals/wk at baseline to 860 kcals/wk at three years, whereas the mean physical activity among WHAS participants decreased from an average 550 kcals/wk at baseline to 490 kcals/wk at three years. This change in physical activity between the two groups was not statistically different in the initial analysis using an unadjusted t test to physical activity at the baseline evaluation to physical activity at the final three-year follow-up (see Table 2).
Table 2.
Unadjusted Analysis of Physical Activity at the Baseline Evaluation and at the Final 3-Year Follow-Up
| EC Participants (n = 71) |
Controls (n = 150) | p Value of Unadjusted t Test | |||
| Baseline | At 3-Year Follow-Up | Baseline | At 3-Year Follow-Up | ||
| Physical activity/week in minutes/wk, mean (SD) | 135 (298) | 109 (228) | 133 (239) | 114 (299) | .85 |
| Physical activity/week in kcal/wk, mean (SD) | 760 (2,446) | 860 (2,184) | 550 (970) | 490 (1,227) | .25 |
| Walking/week in kcal/wk, mean (SD) | 356 (719) | 371 (371) | 340 (642) | 240 (824) | .05 |
| Household chores/week in kcal/wk, mean (SD) | 239 (931) | 422 (1,440) | 345 (822) | 338 (1,066) | .48 |
| Leisure activity/week in kcal/wk, mean (SD) | 327 (1,267) | 149 (424) | 157 (475) | 141 (327) | .36 |
| Exercise/wk in kcal/wk, mean (SD) | 465 (1,853) | 549 (2,039) | 305 (286) | 277 (512) | .40 |
Notes: EC = Experience Corps.
Means were calculated as geometric means.
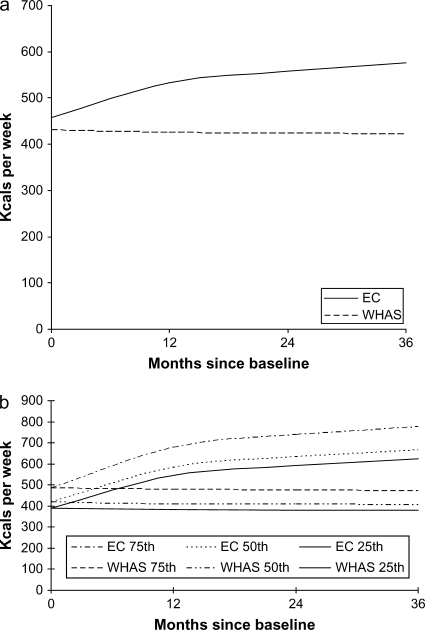
Further analyses using the unadjusted regression model demonstrated a statistically significant increase in physical activity (p < .01) (see Table 3 and Figure 3a). When using the propensity score to account for differences in baseline characteristics such as age and frailty, there was a statistically significant increase in physical activity among EC volunteers as compared with WHAS participants over three years of follow-up (p = .04, adjusted). When the model was adjusted using a propensity score, the baseline physical activity level for individuals with a 50th (median) percentile score was 420 kcals/wk for both the EC volunteers and the WHAS group. Among these individuals who had a median propensity score at baseline, EC volunteers were modeled to expend 670 kcals in physical activity per week at 36 months compared with 410 kcals/wk for the WHAS group. This amounted to a long-term increase of 250 kcals/wk for EC volunteers with a median propensity score and no meaningful change for those in WHAS (see Table 3 and Figure 3b). There was no significant difference in the propensity score between the two groups over time (p = .15).
Table 3.
Kilocalories per Week at Baseline and 12-, 24-, and 36-Month Follow-Up: Experience Corps (n = 71) Versus WHAS (n = 150), Results of Unadjusted and Adjusted Models
| Model | Baseline | 12 Months | 24 Months | 36 Months | p Value | |
| Unadjusted model | EC | 457 | 532 | 559 | 575 | <.01 |
| WHAS | 431 | 425 | 424 | 422 | ||
| Adjusted model, 25th percentile | EC | 390 | 540 | 590 | 620 | .04 |
| WHAS | 390 | 380 | 380 | 380 | ||
| Adjusted model, 25th percentile | EC | 420 | 580 | 630 | 670 | |
| WHAS | 420 | 410 | 410 | 410 | ||
| Adjusted model, 25th percentile | EC | 490 | 680 | 740 | 780 | |
| WHAS | 490 | 480 | 470 | 470 |
Note: EC = Experience Corps; WHAS = Women's Health and Aging Studies.
Figure 3.
(a) Kilocalories per week over a 36-month follow-up: Experience Corps (n = 71) versus Women's Health and Aging Studies (n = 150), results of the unadjusted model, p < .01. (b) Kilocalories per week over a 36-month follow-up: Experience Corps (n = 71) versus Women's Health and Aging Studies (n = 150), results of the adjusted model, 25th, 50th, and 75th percentile propensity scores, p = .04.
The results of the subgroup analyses showed a large degree of variability as measured by the standard deviation (see Table 2). Although there was statistically significant increase in walking for exercise among EC participants compared with WHAS for the unadjusted t test (p = .05), there was no statistical difference in the unadjusted model (p = .06) and the adjusted model (p = .25). Analyses for all other subgroup analyses showed no statistical significance.
DISCUSSION
The sustained increases in physical activity observed over three years in this cohort of older urban African American women enrolled in EC compared with a matched cohort not enrolled in EC suggest that a high-intensity senior service program that is designed as a health promotion intervention can lead to significant long-term improvements in the level of physical activity in high-risk older adults. Although the unadjusted t test of physical activity before and after the intervention did not show a significant difference in total physical activity between the two groups, this initial analysis utilized data collected only at the baseline evaluation and at the final three-year follow-up. The unadjusted and adjusted regression models, which were able to utilize the interval data collected across the 36 months of follow-up, showed a statistically significant increase in physical activity in the EC group as compared with the WHAS comparison group. An analysis using an unadjusted t test also showed a statistically significant increase in walking for exercise in the EC group at three years, but there was no statistical difference for any of the subcategory analyses on subsequent analyses using the unadjusted or adjusted models. The variability observed in the results of the subgroup analyses, as measured by the standard deviation, suggests that this study was insufficiently powered to evaluate the hypothesis that walking would promote physical activity through both travel to and from and activity within the school. Further studies, with either a larger sample size or a direct measure walking, are needed to better understand how volunteer activities such as EC might increase physical activity.
EC was designed to simultaneously improve psychosocial outcomes such as social support and self-efficacy (see Figure 1). Consequently, positive effects in these areas may have played a role in retaining individuals in the program and may be a key component to the observed sustained increases in physical activity (Fried, Carlson, et al., 2004; Tan et al., 2006). A report by the Corporation for National and Community Service notes that year-to-year retention rises as volunteer time commitment rises (Foster-Bey, Grimm, & Dietz, 2007); the EC program in Baltimore experienced only a 2%–3% dropout rate during any given school year and 80% returned from one year to the next (Fried, Carlson, et al., 2004). In addition to satisfaction from the roles that volunteers themselves selected and the potential impact on the children, we also hypothesize that the social relationships with students and other volunteers were a strong motivation for adherence to volunteering and promoted long-term retention. The volunteers also received small stipends, often as quarter-time AmeriCorps volunteers, that helped to offset costs associated with the intervention such as transportation and made volunteering a more viable option for financially challenged older adults. This combination of a high rate of retention and a high-intensity commitment of 15 hr a week provided volunteers the potential for prolonged exposure to health-promoting behaviors. Notably, although the AmeriCorps stipend required only 15 hr/week of activity in the schools, EC participants reported 10 additional hours a week on average or 25 hr/wk of volunteer time throughout the school year (Fried, Carlson, et al.). This is consistent with a previously published report associating volunteer hours with increased life satisfaction in older volunteers (Van Willigen, 2000). The EC program in Baltimore is the first volunteer program to demonstrate the potential for sustained increases in physical activity among older adult participants.
EC was designed to increase access to opportunities for national and community service to older adults who traditionally have had lower access to both volunteer opportunities and exercise interventions (Eyler et al., 2002; Wilson, 2000). The cohort of African American women described in this analysis have a history of limited financial and educational opportunities and were between the ages of 20 and 41 years when the Supreme Court Decision Brown vs. Board of Education initiated the desegregation of all American public schools. Although African Americans are reported to be less likely to volunteer in secular settings (USDL 07-0019, 2007), they are also less likely to be asked to volunteer (Wilson, 2000). However, African Americans who do volunteer are more likely to engage in youth mentoring as one of their volunteer activities (Foster-Bey, Dietz, & Grimm, 2006), which suggests that intergenerational service programs like EC could appeal to these same individuals and communities which are at higher risk of physical inactivity.
Our study has several limitations. This was a comparison between two observational studies and involved a small sample size. Also, the older adults who enrolled in the Baltimore EC program had higher rates of physical activity at baseline as compared with the WHAS cohort, which was a random sample of older women in Baltimore City and the surrounding counties. Although the use of the propensity score mathematically balanced the EC and WHAS participants on observed baseline covariates to get a more accurate estimate of the effects of intervention, it is possible that the relationship between EC participation and physical activity was confounded by variables that were not measured and were therefore not included in the propensity score. The observed increase in physical activity could be caused by these unmeasured characteristics that are associated with EC participation, as volunteering has been associated, in observational studies, with lower mortality and disability rates and improved self-assessed health (Gruenewald, Karlamangla, Greendale, Singer, & Seeman, 2007; Harris & Thoresen, 2005; Lum & Lightfoot, 2005; Luoh & Herzog, 2002; Morrow-Howell, Hinterlong, Rozario, & Tang, 2003; Musick, Herzog, & House, 1999; Musick & Wilson, 2003; Oman, Thoresen, & McMahon, 1999; Shmotkin, Blumstein, & Modan, 2003) and could simply be a marker for other characteristics that are predictive of good health outcomes. For example, given that the EC program was designed to increase social support and self-efficacy (see Figure 1), it is possible that these psychosocial characteristics were higher in the EC group at baseline and that these differences at baseline or differences in motivations for entering the WHAS and EC studies contributed to the observed differences in physical activity at follow-up. There was also no direct observation of physical activity, and although the LTA has been used extensively in physical activity research, it was designed for men aged 40–60 years and has been shown to underestimate physical activity in older adults (Starling, Matthews, Ades, & Poehlman, 1999). Because the great majority of EC participants were African American, and only older adult women were enrolled in WHAS, this analysis was limited to African American women. However, there is no reason to believe that the potential health benefits of the EC model are limited to this demographic group. Finally, although there is evidence of sustained, long-term increases in physical activity in the EC participants, an adequately powered randomized controlled trial is required to determine if EC participation increases physical activity and if increased walking activity is the mechanism for this increased physical activity. Such a trial has been funded by the National Institute on Aging to determine the potential for this model of civic engagement to contribute to a compression of the morbidity associated with aging, as postulated by the designers of the EC program (Fried, Carlson, et al., 2004).
Increased access to national and community service may have the potential to address certain health disparities in African American and other disadvantaged older adults, while simultaneously addressing important social needs and supporting the creation of a sustainable intergenerational social contract (Cassel, 2007). Civic engagement has a long history in the United States (De Tocqueville, 1945), and approximately one quarter of Americans over the age of 65 years engage in some volunteer work (USDL 07-0019, 2007). As the Baby Boom generation ages, America will face increased medical and retirement costs, and some have argued that we will need to choose between the needs of older adults and the funding of other priorities. Intergenerational national and community service programs such as EC demonstrate that there is a “third way,” through programs that simultaneously benefit both old and young. There are concerns that older adult civic engagement can be framed in a context in which older adults are required to be economically “useful” to justify the cost of projected increases in need for older adult services (Martinson & Minkler, 2006). We instead propose that increased access to national and community service programs that have also been designed as health promotion interventions could serve as a sustainable component of a societywide physical activity promotion campaign. America must develop, implement, and evaluate meaningful roles for older adults that are sustainable and promote increased physical activity and social engagement before the Baby Boom generation begins to retire. The time to act is now.
FUNDING
Funding support for this manuscript was provided in part by the National Institute on Aging and the John A. Hartford Foundation and by the Johns Hopkins Older Americans Independence Center under contracts P30-AG02133 and R37-AG19905 from the National Institute on Aging, National Institutes of Health.
Acknowledgments
The authors would like to thank the Greater Homewood Community Corporation, Civic Ventures, the Baltimore City Public School System, and the City of Baltimore for ongoing vision and support, as well as Raymond P. Burchfield for all his assistance with EC throughout the years and the staff and volunteers of the Baltimore EC who have made this all possible. Erwin J. Tan, MD, planned the study, supervised the data analysis, and wrote the paper. George W. Rebok, MA, PhD, participated in planning the study and contributed to revising the paper. Qilu Yu, PhD, participated in planning the study, supervised the data analysis, and contributed to revising the paper. Constantine E. Frangakis, PhD, participated in planning the study, planned the data analysis, and contributed to revising the paper. Michelle C. Carlson participated in planning the study and contributed to revising the paper. Tao Wang, MS, performed statistical analyses and contributed to revising the paper. Michelle Ricks, MS, performed statistical analyses and contributed to revising the paper. Elizabeth K. Tanner, RN, PhD, participated in planning the study and contributed to revising the paper. Sylvia McGill participated in planning the study and contributed to revising the paper. Linda P. Fried, MD, MPH, participated in planning the study, reviewed statistical analyses, and contributed to revising the paper.
References
- Adler NE. Community preventive services. Do we know what we need to know to improve health and reduce disparities? American Journal of Preventive Medicine. 2003;24(Suppl. 3):10–11. doi: 10.1016/s0749-3797(02)00649-9. [DOI] [PubMed] [Google Scholar]
- Bandeen-Roche K, Xue QL, Ferrucci L, Walston J, Guralnik JM, Chaves P, Zeger SL, Fried LP. Phenotype of frailty: Characterization in the Women's Health and Aging Studies. Journals of Gerontology: Biological and Medical Science. 2006;61:262–266. doi: 10.1093/gerona/61.3.262. [DOI] [PubMed] [Google Scholar]
- Barnes P. Physical activity among adults: United States, 2000 and 2005. 2007. [Google Scholar]
- Cassel CK. Medicare matters: What geriatric medicine can teach American health care. Berkeley, CA: University of California Press; 2007. [Google Scholar]
- Centers for Disease Control and Prevention. Increasing physical activity: A report on recommendations of the Task Force on Community Preventive Services. MMWR Morbidity and Mortality Weekly Report. 2001;50:1–14. [PubMed] [Google Scholar]
- De Tocqueville A. In: Democracy in America. Bowen Trans F., translator. New York: Knopf; 1945. [Google Scholar]
- Eyler AE, Wilcox S, Matson-Koffman D, Evenson KR, Sanderson B, Thompson J, Wilbur J, Wilcox S, Young DR. Correlates of physical activity among women from diverse racial/ethnic groups. Journal of Women's Health and Gender Based Medicine. 2002;11:239–253. doi: 10.1089/152460902753668448. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of the American Psychiatric Association Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Foster-Bey J, Dietz N, Grimm R., Jr. Volunteers mentoring youth: Implications for closing the mentoring gap. Washington, DC: Corporation for National & Community Service; 2006. [Google Scholar]
- Foster-Bey J, Grimm R., Jr. Dietz N. Keeping Baby Boomers volunteering: A research brief on volunteer retention and turnover. Washington, DC: Corporation for National & Community Service; 2007. [Google Scholar]
- Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. Journals of Gerontology: Biological and Medical Sciences. 2000;55:M43–M52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- Fried LP, Carlson MC, Freedman M, Frick KD, Glass TA, Hill J, McGill S, Rebok GW, Seeman T, Tielsch J, et al. A social model for health promotion for an aging population: Initial evidence on the Experience Corps model. Journal of Urban Health. 2004;81:64–78. doi: 10.1093/jurban/jth094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. Journals of Gerontology: Biological and Medical Science. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J. Frailty in older adults: Evidence for a phenotype. Journals of Gerontology: Biological and Medical Sciences. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- Glass TA, Freedman M, Carlson MC, Hill J, Frick KD, Ialongo N, McGill S, Rebok GW, Seeman T, Tielsch JM, et al. Experience Corps: Design of an intergenerational program to boost social capital and promote the health of an aging society. Journal of Urban Health. 2004;81:94–105. doi: 10.1093/jurban/jth096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald TL, Karlamangla AS, Greendale GA, Singer BH, Seeman TE. Feelings of usefulness to others, disability, and mortality in older adults: The MacArthur Study of Successful Aging. Journal of Gerontology: Biological and Medical Science. 2007;62:P28–P37. doi: 10.1093/geronb/62.1.p28. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Linda LP, Simonsick EM, Kasper JD, Lafferty ME. The Women's Health and Aging Study: Health and social characteristics of older women with disability. Bethesda, MD: National Institute on Aging/National Institute on Health; 1995. [Google Scholar]
- Harris AHS, Thoresen CE. Volunteering is associated with delayed mortality in older people: Analysis of the longitudinal study of aging. Journal of Health Psychology. 2005;10:739–752. doi: 10.1177/1359105305057310. [DOI] [PubMed] [Google Scholar]
- Katula JA, Kritchevsky SB, Guralnik JM, Glynn NW, Pruitt L, Wallace K, et al. Lifestyle interventions and independence for elders pilot study: Recruitment and baseline characteristics. Journal of the American Geriatrics Society. 2007;55:674–683. doi: 10.1111/j.1532-5415.2007.01136.x. [DOI] [PubMed] [Google Scholar]
- King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults. A critical review and recommendations. American Journal of Preventive Medicine. 1998;15:316–333. doi: 10.1016/s0749-3797(98)00085-3. [DOI] [PubMed] [Google Scholar]
- Lum TY, Lightfoot E. The effects of volunteering on the physical and mental health of older people. Research on Aging. 2005;27:31–55. [Google Scholar]
- Luoh MC, Herzog AR. Individual consequences of volunteer and paid work in old age: Health and mortality. Journal of Health and Social Behavior. 2002;43:490–509. [PubMed] [Google Scholar]
- Martinez IL, Frick K, Glass TA, Carlson M, Tanner E, Ricks M, Fried LP. Engaging older adults in high impact volunteering that enhances health: Recruitment and retention in the Experience Corps™ Program in Baltimore. Journal of Urban Health. 2006;83:941–953. doi: 10.1007/s11524-006-9058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinson M, Minkler M. Civic engagement and older adults: A critical perspective. Gerontologist. 2006;46:318–324. doi: 10.1093/geront/46.3.318. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2005;293:293–294. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- Morrow-Howell N, Hinterlong J, Rozario PA, Tang F. Effects of volunteering on the well-being of older adults. Journals of Gerontology: Biological and Medical Sciences. 2003;58:S137–S145. doi: 10.1093/geronb/58.3.s137. [DOI] [PubMed] [Google Scholar]
- Musick MA, Herzog AR, House JS. Volunteering and mortality among older adults: Findings from a national sample. Journals of Gerontology: Social Sciences. 1999;54:S173–S180. doi: 10.1093/geronb/54b.3.s173. [DOI] [PubMed] [Google Scholar]
- Musick MA, Wilson J. Volunteering and depression: The role of psychological and social resources in different age groups. Social Science and Medicine. 2003;56:259–269. doi: 10.1016/s0277-9536(02)00025-4. [DOI] [PubMed] [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Macera CA, Castaneda-Sceppa C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- Oman D, Thoresen CE, McMahon K. Volunteerism and mortality among the community-dwelling elderly. Journal of Health Psychology. 1999;4:301–316. doi: 10.1177/135910539900400301. [DOI] [PubMed] [Google Scholar]
- Prohaska T, Belansky E, Belza B, Buchner D, Marshall V, McTigue K, Satariano W, Wilcox S. Physical activity, public health, and aging: Critical issues and research priorities. Journals of Gerontology: Social Sciences. 2006;61:S267–S273. doi: 10.1093/geronb/61.5.s267. [DOI] [PubMed] [Google Scholar]
- Rebok GW, Carlson MC, Glass TA, McGill S, Hill J, Wasik BA, Ialongo N, Frick KD, Fried LP, Rasmussen MD. Short-term impact of Experience Corps participation on children and schools: Results from a pilot randomized trial. Journal of Urban Health. 2004;81:79–93. doi: 10.1093/jurban/jth095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- Shmotkin D, Blumstein T, Modan B. Beyond keeping active: Concomitants of being a volunteer in old-old age. Psychology and Aging. 2003;18:602–607. doi: 10.1037/0882-7974.18.3.602. [DOI] [PubMed] [Google Scholar]
- Starling RD, Matthews DE, Ades PA, Poehlman ET. Assessment of physical activity in older individuals: A doubly labeled water study. Journal of Applied Physiology. 1999;86:2090–2096. doi: 10.1152/jappl.1999.86.6.2090. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. Physical activity outcomes of CHAMPS II: A physical activity promotion program for older adults. Journals of Gerontology: Biological and Medical Science. 2001;56:M465–M470. doi: 10.1093/gerona/56.8.m465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan EJ, Xue QL, Li T, Carlson MC, Fried LP. Volunteering: A physical activity intervention for older adults-the Experience Corps® Program in Baltimore. Journal of Urban Health. 2006;83:954–969. doi: 10.1007/s11524-006-9060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor H, Jacobs D, Schuker B. A questionnaire for the assessment of leisure-time physical activities. Journal of Chronic Disease. 1978;31:745–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- USDL 07-0019. Volunteering in the United States, 2006. 2007. [Google Scholar]
- Van Willigen M. Differential benefits of volunteering across the life course. Journals of Gerontology: Social Sciences. 2000;55:S308–S318. doi: 10.1093/geronb/55.5.s308. [DOI] [PubMed] [Google Scholar]
- Wilson J. Volunteering. Annual Review of Sociology. 2000;26:215–240. [Google Scholar]