Abstract
Congenital duodenal obstruction is rare in adulthood. An unusual presentation of this condition has led to difficult preoperative diagnosis. We present a case of proximal jejunal obstruction by a congenital band in an adult and review the literature.
Keywords: Malrotation, Duodenal obstruction, Surgical procedures, Congenital band, Adult
INTRODUCTION
Midgut malrotation is an anomaly of fetal intestinal rotation that usually presents in the first month of life. It is rare in adulthood. Congenital duodenal obstruction (atresia or stenosis) is associated with various congenital anomalies[1,2]. Midgut malrotation is a congenital anomaly referring to either lack of or incomplete rotation of the fetal intestines around the axis of the superior mesenteric artery during fetal development[3]. Most patients present with bilious vomiting in the first month of life because of duodenal obstruction or a volvulus. The true incidence in adults is difficult to estimate because most patients remain asymptomatic and their conditions are, therefore, never diagnosed. A literature review by von Flüe et al[4] cites 40 cases from 1923 to 1992. Approximately 90% of patients with malrotation are diagnosed within the first year of life, of whom 80% are diagnosed within the first month of life[4]. Surgical therapy remains the mainstay of treatment regardless of age at presentation. The most commonly used approach is the Ladd procedure, which involves counterclockwise reduction of the volvulus if present, division of any coloduodenal bands, widening of the mesenteric base to prevent repeated volvulus, and prophylactic appendectomy[5]. We present a case of malrotation in an adult who presented with chronic abdominal pain.
CASE REPORT
A 21-year-old woman was admitted to our hospital with a 15-year history of postprandial epigastric pain. Pain relieved after vomiting. The presentations since her teenage years with similar symptoms had failed to identify the cause of her pain. She had no changes in bowel habits, and no significant past medical history. On physical examination, the patient’s vital signs were pulse 72, and regular, blood pressure 108/76, respirations 18, and temperature 36.8°C. She was a normally-developed and in no acute distress. Her abdomen was minimally distended on inspection. A succession splash was readily elicited. Normal bowel sounds were auscultated. She exhibited no peritoneal signs. She denied any history of disease and no history of abdominal surgery; her family history was negative for GI disease. She was on no current medications and denied alcohol or tobacco use. On admission, her rectal examination was normal, and her stool occult test was negative. Hemoglobin, white blood cell count, and basic chemical panel were all within normal values. Abdominal X-ray showed dilatation of the stomach and the proximal part of the duodenum. A computed abdominal tomography taken 6 mo before was normal. Upper gastrointestinal contrast studies showed the duodenum not crossing the lumbar spine. The entire small bowel was noted to be sequestered on the right side of the abdomen (Figure 1) Abdominal decompression was accomplished after placement of a nasogastric tube. The patient underwent aggressive fluid and electrolyte resuscitation, and parenteral nutrition was instituted for a suspected partial duodenal obstruction. On day 4 after admission to the hospital, the patient underwent abdominal exploration through a midline laparotomy, and was found to have a massively dilated stomach and proximal duodenum, and intestinal malrotation was confirmed. The small bowel and duodenum were on the right, with the transverse and descending colon positioned in the right upper quadrant. The duodenum was not posterior to the superior mesenteric artery, compressed between the peritoneal bands superiorly. Cecal bands attaching to the duodenum were immediately noted (Figure 2). The cecum was subsequently returned to the left abdomen. The appendix was not removed. The patient underwent the Ladd’s procedure. Upon entering the abdomen, bands were lysed, and the duodenum and right colon were mobilized. Adhesions surrounding the superior mesenteric artery were also lysed (Figure 3). Postoperatively, the patient did well, tolerated a regular diet on postoperative day 4. The patient’s postoperative course was uncomplicated. She was discharged from hospital on postoperative day 8. There were no complications with the surgery and the patient made a full and uneventful recovery and no recurrence was found after 4 mo of follow-up.
Figure 1.
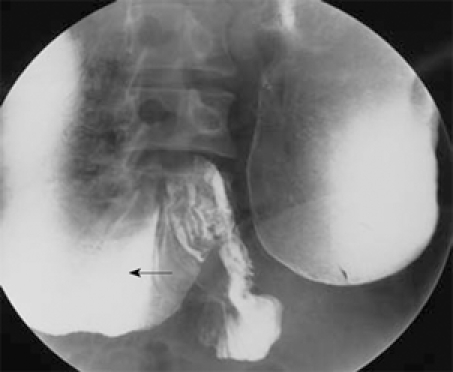
Barium image from upper gastrointestinal series reveals duodenal obstruction, demonstrating high-grade stenosis of the fourth portion of the duodenum and extreme dilation of proximal duodenum (arrow).
Figure 2.

CT scan shows duodenum does not cross behind the superior mesenteric artery and the superior mesenteric vein, and extreme dilation of proximal duodenum (arrow).
Figure 3.
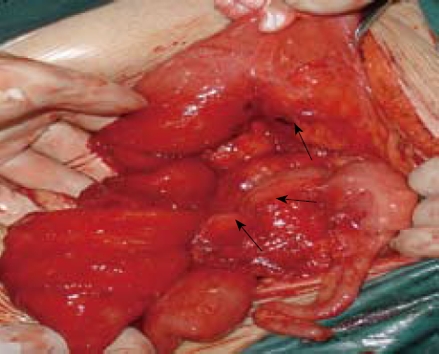
One band running from the anti-mesenteric wall of proximal jejunum to cecum has been lysed (arrows) and no Treitz’s ligament is found.
DISCUSSION
The embryology of malrotation was described by Mall in 1898[6]. It was decribed in detail in 1923 by Dott. Intestinal malrotation was further classified by the specific embryologic abnormalities. Rotational abnormalities of the intestine occur when the normal embryologic rotation and fixation of the intestinal mesentery fail to take place[7]. Although the true incidence of intestinal rotation disorders is unknown, autopsy studies estimate that it may be as high as 1% of the total population[8]. Congenital anomalies of intestinal rotation are often seen in infants and children; however, they are uncommon in adults[9]. Yanez and Spitz[10] reported that only 50%-70% of patients actually present during the first 4 wk of life. In either event, there are a substantial number of discovered cases of malrotation that present after the neonatal period. In adults, it may cause chronic, but nebulous symptoms that are often difficult to diagnose. Adult presentation of malrotation is a difficult diagnosis because of the low incidence of the disorder. Patients with intestinal malrotation who were not diagnosed until adulthood may present with a variety of chronic symptoms, including nausea, vomiting, diarrhea, vague abdominal pain, early satiety and bloating, dyspepsia, and peptic or duodenal ulcer disease. Unfortunately, many patients never receive surgical referral and are instead labeled with functional or psychiatric disorders[11]. There may be a significant number of patients with malrotation who were undetected in the neonatal period either because they were asymptomatic, or because their symptoms were mild and misinterpreted. As these patients grow into adolescence and adulthood, they may continue to have misinterpreted symptoms, remain asymptomatic, or present with new onset of acute or chronic symptoms later in life, as did our patient. Adults, however, present with vague symptoms such as vomiting (bilious or non-bilious), weight loss, and recurrent or colicky abdominal pain (often postprandial)[10,12,13]. Intestinal obstruction, diarrhea, malabsorption, peritonitis, and septic shock also have been reported in the adult group[12]. Timing and frequency of the pain also can be variable[14]. It is these vague symptoms along with the relative rarity of adult presentation of malrotation that often lead to a delay in diagnosis. In recent years, there has been increasing recognition of the various CT findings associated with malrotation in adults, leading to enhanced diagnostic accuracy[15]. In addition, the number of adults with malrotation misdiagnosed with non-abdominal (including psychiatric) pathology only reinforces the importance of obtaining routine imaging studies when the cause of chronic intermittent abdominal pain is unclear[16]. Generally, barium duodenography may still play an important role in the diagnosis of duodenal disorders. For the best management of duodenal diseases, barium studies in combination with cross-sectional imaging modalities may offer detailed evaluation of the duodenum and its surrounding organs. However, CT, US and MRI all provide excellent cross-sectional anatomic orientation, which allows accurate pre-operative evaluation[17]. Surgical therapy remains the mainstay of treatment regardless of age at presentation. For this reason, it is crucial that all surgeons operating on adult patients have firm knowledge of intestinal embryology and its anatomic variations. The most commonly used approach is the Ladd procedure, which involves counterclockwise reduction of the volvulus if present, division of any coloduodenal bands, widening of the mesenteric base to prevent repeated volvulus, and prophylactic appendectomy[5]. Although symptomatic malrotation after infancy requires prompt recognition and treatment, many patients with malrotation may remain asymptomatic into adulthood. Symptomatic or autopsy findings of malrotation were identified at a rate of 3 per 10 000 (0.03%) in a population-based birth defects study[18]. In 1996, a minimally invasive laparoscopic method was developed for performing Ladd’s procedure in the case of malrotation without vo1vu1us[19].
Peer reviewer: Atsushi Nakajima, Professor, Division of Gastroenterology, Yokohama City University Graduate School of Medicine, 3-9 Fuku-ura, Kanazawa-ku, Yokohama 236-0004, Japan
S- Editor Li JL L- Editor Ma JY E- Editor Yin DH
References
- 1.Kimble RM, Harding J, Kolbe A. Additional congenital anomalies in babies with gut atresia or stenosis: when to investigate, and which investigation. Pediatr Surg Int. 1997;12:565–570. doi: 10.1007/BF01371900. [DOI] [PubMed] [Google Scholar]
- 2.Bailey PV, Tracy TF Jr, Connors RH, Mooney DP, Lewis JE, Weber TR. Congenital duodenal obstruction: a 32-year review. J Pediatr Surg. 1993;28:92–95. doi: 10.1016/s0022-3468(05)80364-1. [DOI] [PubMed] [Google Scholar]
- 3.Zissin R, Rathaus V, Oscadchy A, Kots E, Gayer G, Shapiro-Feinberg M. Intestinal malrotation as an incidental finding on CT in adults. Abdom Imaging. 1999;24:550–555. doi: 10.1007/s002619900560. [DOI] [PubMed] [Google Scholar]
- 4.von Flüe M, Herzog U, Ackermann C, Tondelli P, Harder F. Acute and chronic presentation of intestinal nonrotation in adults. Dis Colon Rectum. 1994;37:192–198. doi: 10.1007/BF02047549. [DOI] [PubMed] [Google Scholar]
- 5.Matzke GM, Dozois EJ, Larson DW, Moir CR. Surgical management of intestinal malrotation in adults: comparative results for open and laparoscopic Ladd procedures. Surg Endosc. 2005;19:1416–1419. doi: 10.1007/s00464-004-8249-7. [DOI] [PubMed] [Google Scholar]
- 6.Mall FT. Development. of the human intestine and its position in the adult. Bull Johns Hopkins Hosp. 1898;9:197–208. [Google Scholar]
- 7.Dott NM. Anomalies of intestinal rotation: Their embryology and surgical aspects: With report of five cases. Br J Surg. 1923;11:251–286. [Google Scholar]
- 8.Kapfer SA, Rappold JF. Intestinal malrotation-not just the pediatric surgeon's problem. J Am Coll Surg. 2004;199:628–635. doi: 10.1016/j.jamcollsurg.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Wang CA, Welch CE. Anomalies of intestinal rotation in adolescents and adults. Surgery. 1963;54:839–955. [PubMed] [Google Scholar]
- 10.Yanez R, Spitz L. Intestinal malrotation presenting outside the neonatal period. Arch Dis Child. 1986;61:682–685. doi: 10.1136/adc.61.7.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gamblin TC, Stephens RE Jr, Johnson RK, Rothwell M. Adult malrotation: a case report and review of the literature. Curr Surg. 2003;60:517–520. doi: 10.1016/S0149-7944(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 12.Spigland N, Brandt ML, Yazbeck S. Malrotation presenting beyond the neonatal period. J Pediatr Surg. 1990;25:1139–1142. doi: 10.1016/0022-3468(90)90749-y. [DOI] [PubMed] [Google Scholar]
- 13.Powell DM, Othersen HB, Smith CD. Malrotation of the intestines in children: the effect of age on presentation and therapy. J Pediatr Surg. 1989;24:777–780. doi: 10.1016/s0022-3468(89)80535-4. [DOI] [PubMed] [Google Scholar]
- 14.Gohl ML, DeMeester TR. Midgut nonrotation in adults. An aggressive approach. Am J Surg. 1975;129:319–323. doi: 10.1016/0002-9610(75)90249-4. [DOI] [PubMed] [Google Scholar]
- 15.Delaney CP, Lavery IC. Malrotation of the small intestine with volvulus. J Am Coll Surg. 2001;193:103. doi: 10.1016/s1072-7515(01)00915-2. [DOI] [PubMed] [Google Scholar]
- 16.Devlin HB, Williams RS, Pierce JW. Presentation of midgut malrotation in adults. Br Med J. 1968;1:803–807. doi: 10.1136/bmj.1.5595.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reeders JW, Bakker AJ, Rosenbusch G. Contemporary radiological examination of the lower gastrointestinal tract. Baillieres Clin Gastroenterol. 1994;8:701–727. doi: 10.1016/0950-3528(94)90020-5. [DOI] [PubMed] [Google Scholar]
- 18.Forrester MB, Merz RD. Epidemiology of intestinal malrotation, Hawaii, 1986-99. Paediatr Perinat Epidemiol. 2003;17:195–200. doi: 10.1046/j.1365-3016.2003.00480.x. [DOI] [PubMed] [Google Scholar]
- 19.Gross E, Chen MK, Lobe TE. Laparoscopic evaluation and treatment of intestinal malrotation in infants. Surg Endosc. 1996;10:936–937. doi: 10.1007/BF00188488. [DOI] [PubMed] [Google Scholar]


