Abstract
Interventions aimed at preventing viral spread have the potential to effectively control influenza virus in all age groups, thereby reducing the burden of influenza illness. For this reason, we have examined the efficacy of vaccination in blocking the transmission of influenza viruses between guinea pigs. Three modes of immunization were compared: (i) natural infection; (ii) intramuscular administration of whole, inactivated influenza virus in 2 doses; and (iii) intranasal inoculation with live attenuated influenza virus in 2 doses. The ability of each immunization method to block the spread of a homologous (A/Panama/2007/99) H3N2 subtype and a heterologous (A/Wisconsin/67/05) H3N2 subtype influenza virus was tested. We found that previous infection through a natural route provided sterilizing immunity against both homologous and heterologous challenges; thus, no transmission to or from previously infected animals was observed. Vaccination with an inactivated influenza virus vaccine, in contrast, did not prevent guinea pigs from becoming infected upon challenge with either virus. Thus, both intranasal inoculation and exposure to an acutely infected guinea pig led to the infection of vaccinated animals. Vaccination with inactivated virus did, however, reduce viral load upon challenge and decrease the number of secondary transmission events from vaccinated animals to naïve cage mates. Vaccination with a live attenuated virus was found to be more efficacious than vaccination with inactivated virus, resulting in sterilizing immunity against homologous challenge and full protection against the transmission of the homologous and heterologous viruses to naïve contacts. In conclusion, we have shown that the guinea pig model can be used to test influenza virus vaccines and that the efficiency of transmission is a valuable readout when vaccine efficacy is evaluated.
The cumulative morbidity and mortality caused by seasonal influenza are substantial, partly due to the relatively high attack rate. In the United States, seasonal influenza viruses infect an estimated 10 to 15% of the population (16, 18) and are associated with approximately 30,000 deaths each year (2, 48). Worldwide, influenza may kill as many as 250,000 to 500,000 people annually (http://www.who.int/mediacenter/factsheets/fs211/en/). In addition to annual epidemics, influenza viruses are the cause of infrequent pandemics. Due to the lack of preformed immunity against the major viral antigen (hemagglutinin), pandemic influenza can affect greater than 50% of the population in a single year and can cause more severe disease than epidemic influenza. The most severe influenza pandemic of the 20th century claimed an estimated 50 million lives (23, 44).
Vaccination is considered by far to be the most cost-effective medical intervention to combat seasonal influenza (11). However, certain population groups, notably, the elderly and immunocompromised, do not respond well to influenza virus vaccination. These groups are furthermore at high risk of suffering severe complications of influenza. Thus, there is an identified need for more effective vaccination strategies to improve protection of at-risk individuals (17, 25).
Current CDC guidelines recommend the vaccination of household contacts of at-risk persons based on the principle of indirect effectiveness of immunization (11). Indeed, clinical trials have demonstrated the value of vaccination aimed at preventing transmission. The widespread vaccination of children with an inactivated influenza virus vaccine has been shown to reduce all-cause mortality in the elderly (39) and the incidence of respiratory illness in adults (33). Similarly, in a clinical trial in which 20 to 25% of children between 1.5 and 18 years of age were vaccinated with a cold-adapted live attenuated influenza virus vaccine (caLAIV), 8 to 18% of adults were protected against medically attended acute respiratory disease (37). Thus, vaccination of the children of a population can offer protection to the adults of the same population simply by limiting transmission.
Nonetheless, the evaluation of new influenza virus vaccines tends to focus on efficacy in preventing disease; the potential of a vaccine to disrupt the chain of transmission is rarely assessed. Licensed influenza virus vaccines are manufactured as inactivated viral preparations (whole inactivated virus, split, or subunit vaccines) or as live attenuated virus vaccines. Such vaccines have been reported to vary in their abilities to provide protection from disease (4, 9, 19, 21, 30, 31, 34-36, 41, 49, 51), but their potential to prevent transmission has not been directly compared. Licensed caLAIV possesses mutations in the PB2, PB1, and NP genes, which confer cold-adapted and temperature-sensitive phenotypes (22). One promising candidate live attenuated influenza virus vaccine (LAIV) expresses a truncated form of the NS1 protein (20, 38, 47). Such NS1-truncated viruses constitute ideal live vaccines for two reasons: (i) they are attenuated in vivo due to their decreased ability to block interferon (IFN) production, and (ii) by inducing high levels of IFN, they may carry intrinsic adjuvant activity. Indeed, NS1 mutant influenza viruses are potent activators of dendritic cells (14, 26) and potent immunostimulators (15). NS1-modified live attenuated vaccines have furthermore been shown to be safe and efficacious in swine, equine, and poultry hosts challenged with homologous or heterologous influenza virus isolates (12, 40, 42, 43, 50).
Herein, we have used the guinea pig model to evaluate three modes of immunization in terms of their potential to reduce the interhost transmission of influenza viruses. Natural infection, vaccination with an inactivated influenza virus, and vaccination with an NS1-truncated LAIV were compared. In previous studies, we have demonstrated that the guinea pig is highly susceptible to infection with low-passage human influenza virus isolates and that the kinetics of virus replication in the respiratory tract of guinea pigs (28) mirrors that in humans (10). Furthermore, we have shown that human influenza viruses transmit efficiently from guinea pig to guinea pig under conditions both where the two animals are in direct contact and when the animals are housed in separate cages (7, 27-29). Herein, we demonstrate that the guinea pig model can be used to test influenza virus vaccines. All three modes of immunization tested were found to reduce transmission to and/or from vaccinated animals. Natural infection was the most effective, followed by vaccination with LAIV and then vaccination with the inactivated virus. Importantly, our results indicate that protection against transmission does not always correlate with protection against infection, highlighting the value of testing vaccines specifically for efficacy in preventing transmission.
MATERIALS AND METHODS
Viruses.
A/Panama/2007/99 (Pan/99) and A/Wisconsin/67/2005 (Wisc/05) influenza viruses were obtained from the CDC. Stocks of Pan/99 and Wisc/05 were produced in Madin-Darby canine kidney (MDCK) cell culture and 10-day-old embryonated chicken eggs, respectively. Titers of virus stocks were determined by plaque assay on MDCK cells.
Animals.
Female Hartley strain guinea pigs weighing 300 to 350 g were obtained from Charles River Laboratories Inc. (Wilmington, MA). Animals were allowed free access to food and water and kept on a cycle of 12 h light/12 h dark. Guinea pigs were anesthetized for intranasal inoculation as well as for the collection of blood and of nasal wash samples using a mixture of ketamine (30 mg/kg of body weight) and xylazine (2 mg/kg) administered intramuscularly. All procedures were performed in accordance with the Institutional Animal Care and Use Committee guidelines. During guinea pig transmission experiments, measures to prevent aberrant cross-contamination between cages were followed: exposed animals were handled before inoculated animals, and gloves were changed between cages.
Immunization through natural infection.
Natural infection of guinea pigs with Pan/99 virus was achieved as follows. A set of guinea pigs was inoculated intranasally with 1,000 PFU Pan/99 virus. At 24 h postinoculation, a second set of guinea pigs was introduced into the same cages as the inoculated guinea pigs. Thus, one acutely infected guinea pig was housed with one naïve guinea pig. In order to monitor for transmission, nasal wash samples were collected in phosphate-buffered saline (PBS), as previously described (28), from all inoculated and exposed animals on days 2, 4, 6, and 8 postinoculation. Titration of these nasal wash samples by plaque assay indicated that all exposed animals became infected. At day 8 postinoculation, the intranasally inoculated animals were euthanized, and the naturally infected (exposed) guinea pigs were kept for a period of 3 weeks prior to challenge.
Vaccination with whole, inactivated influenza virus.
Whole, inactivated Pan/99 virus vaccine preparations were made as follows. Ten-day-old embryonated chicken eggs were inoculated with Pan/99 virus and incubated for 2 days at 37°C. Eggs were then placed at 4°C overnight, and fluid was harvested from the allantoic cavity. Allantoic fluid was clarified by centrifugation for 10 min at 3,000 rpm (Sorvall Legend RT+ table-top centrifuge), followed by centrifugation of the resulting supernatant for 30 min at 10,000 rpm (Sorvall SW28 rotor). The supernatant from the second low-speed spin was then transferred into fresh tubes, and virus therein was pelleted by centrifugation for 2.5 h at 25,000 rpm (Sorvall SW28 rotor) through a 30% sucrose cushion. Virus pellets were resuspended in PBS, and a sample was removed for plaque assay. The remaining virus was inactivated through the addition of 0.05% formalin and incubation at 4°C for 4 days. Plaque assay of the virus preparation prior to inactivation indicated a titer of 2 × 109 PFU/ml, and plaque assay following inactivation confirmed the absence of live virus.
Guinea pigs were vaccinated through intramuscular injection into the gluteal muscles of the hind limb. Each animal received of 1 × 109 PFU (corresponding to 60 μg total protein as determined by a Bradford assay) (7a) of vaccine in two 250-μl injections. This dose was administered twice, on days 0 and 21 of the experiment. The rationale for using a dose of 1 × 109 PFU was as follows: two human doses of 15 μg hemagglutinin protein per virus are normally obtained from one 10-day-old embryonated hen egg, and infection of one egg with a high-growth influenza virus yields approximately 2 × 109 PFU; thus, we estimate the human dose of inactivated vaccine to be roughly 1 × 109 PFU. Mock-vaccinated animals were given two 250-μl injections of PBS alone. We found that it was important not to include bovine serum albumin in the vaccine preparations, as repeated exposure to this antigen led to hypersensitivity responses in guinea pigs upon challenge.
Vaccination with live attenuated influenza virus.
The live attenuated vaccine strain used, Pan/99 HA NA:PR8 NS1-73, was a recombinant virus comprising the HA and NA genes of Pan/99 and the remaining six genes of influenza A/Puerto Rico/8/34 virus. The NS1 open reading frame of this virus was truncated through the insertion of four stop codons (at least one in each reading frame) and a 220-nucleotide deletion, essentially as previously described (42). Pan/99 HA NA:PR8 NS1-73 virus was generated by reverse genetics through the transfection of two viral RNA expression plasmids (pPOL1 Pan/99 HA and pPOL1 Pan/99 NA) and six ambisense plasmids for the expression of both viral RNA and protein (pDZ PR8 NS 1-73, pDZ PR8 M, pDZ PR8 NP, pDZ PR8 PA, pDZ PR8 PB1, and pDZ PR8 PB2) into 293T cells. The recovered virus was amplified in 8-day-old embryonated eggs and titrated by plaque assay on MDCK cells, followed by immunostaining.
Guinea pigs were vaccinated through the intranasal inoculation of 106 PFU of Pan/99 HA NA:PR8 NS1-73 virus in 300 μl PBS (150 μl per nostril). This dose was administered twice, on days 0 and 21 of the experiment. Mock-vaccinated animals were given 300 μl of PBS alone. Again, the inclusion of bovine serum albumin in the vaccine preparations was avoided, as repeated exposure to this antigen led to hypersensitivity responses upon challenge.
Challenge.
Vaccinated guinea pigs were separated into two groups for challenge. The first group was challenged through the intranasal inoculation of 1,000 PFU of either Pan/99 virus (for homologous challenge) or Wisc/05 virus (for heterologous challenge). Virus was administered in 300 μl PBS. At 24 h after inoculation, each challenged guinea pig was placed into the same cage as a single naïve guinea pig; in this way, the potential for transmission from vaccinated and challenged guinea pigs to naïve contacts could be assessed. The second group of vaccinated animals was challenged through exposure to an acutely infected guinea pig. Thus, naïve animals were infected intranasally with 1,000 PFU of either Pan/99 virus (for homologous challenge) or Wisc/05 virus (for heterologous challenge), and at 24 h postinoculation, one infected guinea pig was then placed into the same cage with each vaccinated guinea pig. To monitor for transmission, nasal wash samples were collected in PBS, as previously described (28), on days 2, 4, 6, and 8 postinoculation from all guinea pigs in both challenge groups.
The results of the challenge experiments are represented in Fig. 2 to 5, 7, and 8 using the following color scheme. Regardless of the mode of challenge, all immunized animals (including those immunized through prior infection) are shown in red, and the contacts of the immunized guinea pigs are shown in blue. Conversely, mock-immunized guinea pigs are shown in black, and their contacts are shown in white. In addition, regardless of their immune statuses, the nasal wash titers of all intranasally inoculated animals are shown with dashed lines, while those of exposed guinea pigs are shown with solid lines.
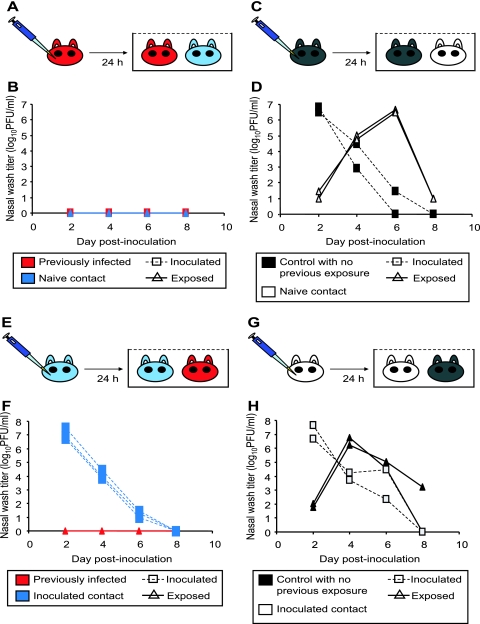
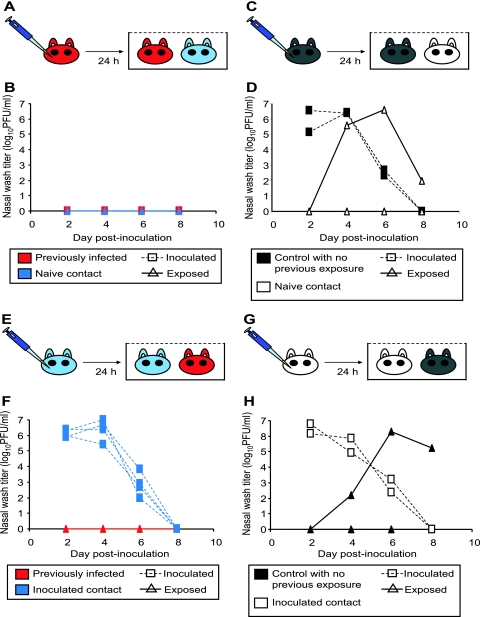
FIG. 2.
Previously infected guinea pigs exhibit sterilizing immunity to homologous challenge. (A) Schematic representation of challenge by the intranasal route. Three previously infected guinea pigs (red) were challenged intranasally with Pan/99 virus. At 24 h postinoculation, a naïve contact animal (blue) was cocaged with each of the three inoculated guinea pigs. (B) Results of homologous challenge by the intranasal route. No virus was detected in the nasal washings of challenged guinea pigs (red squares with dashed lines), and no virus was detected in the naïve contact animals (blue triangles with solid lines). (C) Schematic representation of challenge of control guinea pigs by the intranasal route. Two control animals with no previous exposure (black) were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, a naïve contact guinea pig (white) was cocaged with each of the two inoculated guinea pigs. (D) Results of Pan/99 challenge of control guinea pigs by the intranasal route. Animals with no previous exposure were productively infected through inoculation (black squares with dashed lines) and transmitted efficiently to naïve contact animals (white triangles with solid lines). (E) Schematic representation of challenge through exposure to an infected guinea pig. Three naïve guinea pigs were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, each of the three acutely infected animals (blue) was placed into the same cage with one previously infected guinea pig (red). (F) Results of homologous challenge through exposure to an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (blue squares with dashed lines); however, guinea pigs with previous exposure to Pan/99 virus (red triangles with solid lines) did not become infected through contact with the infected animals. (G) Schematic representation of challenge of control animals through exposure to an infected guinea pig. Two naïve contact animals were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, two control guinea pigs with no previous exposure were each placed into the same cage with one infected animal. (H) Results of control challenge through contact with an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (white squares with dashed lines), and control guinea pigs with no previous exposure to Pan/99 virus (black triangles with solid lines) became infected through contact with the infected animals.
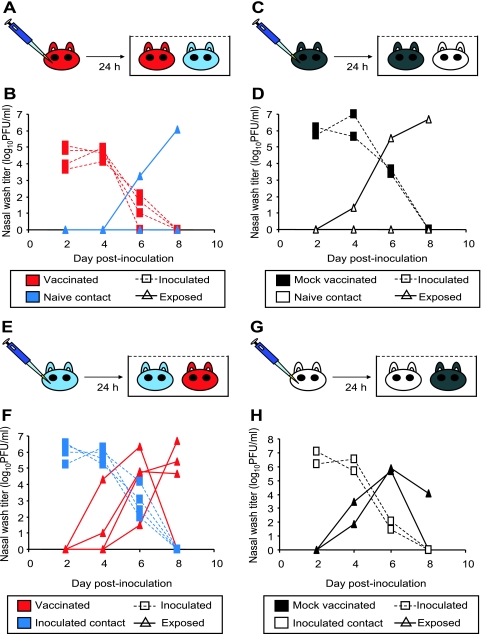
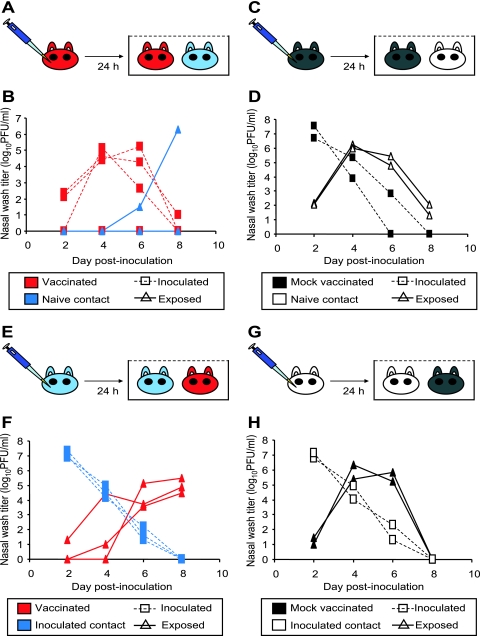
FIG. 5.
Vaccination with inactivated virus limits secondary transmission but does not protect against initial infection with heterologous virus. (A) Schematic representation of challenge by the intranasal route. Four guinea pigs previously vaccinated with inactivated Pan/99 virus (red) were challenged intranasally with Wisc/05 virus. At 24 h postinoculation, a naïve contact animal (blue) was cocaged with each of the four inoculated guinea pigs. (B) Results of heterologous challenge by the intranasal route. All four previously vaccinated guinea pigs became infected upon challenge (red squares with dashed lines); however, only one of four naïve contact animals (blue triangles with solid lines) contracted infection. (C) Schematic representation of challenge of mock-vaccinated guinea pigs by the intranasal route. Two previously mock-vaccinated animals (black) were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, a naïve contact guinea pig (white) was cocaged with each of the two inoculated guinea pigs. (D) Results of Wisc/05 challenge of mock-vaccinated guinea pigs by the intranasal route. Mock-vaccinated guinea pigs were productively infected through inoculation (black squares with dashed lines). Transmission to one of two naïve contact animals was observed (white triangles with solid lines). (E) Schematic representation of heterologous challenge through exposure to an infected guinea pig. Three naïve guinea pigs were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, each acutely infected animal (blue) was placed into the same cage with one vaccinated guinea pig (red). (F) Results of heterologous challenge through exposure to an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (blue squares with dashed lines); all four animals vaccinated with killed Pan/99 virus (red triangles with solid lines) became infected through the transmission of Wisc/05. (G) Schematic representation of challenge of control animals through exposure to an infected guinea pig. Two naïve contact animals were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, one mock-vaccinated guinea pig was placed into the same cage with each infected animal. (H) Results of control challenge through contact with a Wisc/05-infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (white squares with dashed lines), and both of the mock-vaccinated guinea pigs (black triangles with solid lines) became infected through contact with an infected animal.
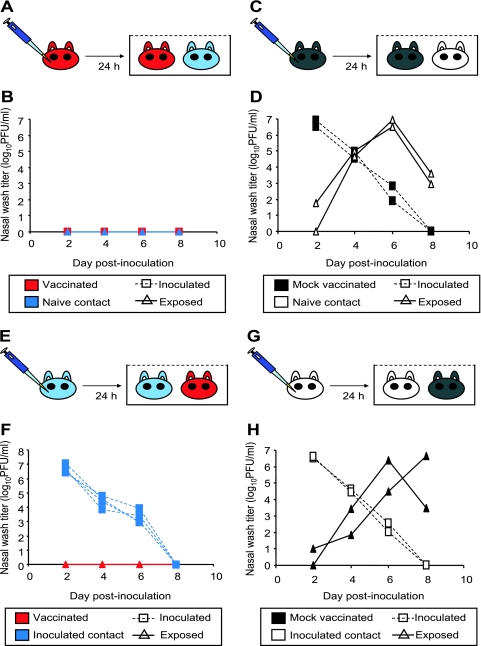
FIG. 7.
Vaccination with an NS1-truncated LAIV provides sterilizing immunity against homologous challenge. (A) Schematic representation of challenge by the intranasal route. Four guinea pigs previously vaccinated with LAIV (red) were challenged intranasally with 1,000 PFU of Pan/99 virus. At 24 h postinoculation, a naïve contact animal (blue) was cocaged with each of the inoculated guinea pigs. (B) Results of homologous challenge by the intranasal route. No virus was detected in the nasal washings of challenged guinea pigs (red squares with dashed lines) or of the naïve contact animals (blue triangles with solid lines). (C) Schematic representation of challenge of mock-vaccinated guinea pigs by the intranasal route. Two previously mock-vaccinated control animals (black) were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, a naïve contact guinea pig (white) was cocaged with each of the inoculated guinea pigs. (D) Results of Pan/99 challenge of mock-vaccinated guinea pigs by the intranasal route. Mock-vaccinated guinea pigs were productively infected through inoculation (black squares with dashed lines) and transmitted efficiently to naïve contact animals (white triangles with solid lines). (E) Schematic representation of challenge through exposure to an infected guinea pig. Four naïve guinea pigs were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, each acutely infected animal (blue) was placed into the same cage with one previously vaccinated guinea pig (red). (F) Results of homologous challenge through exposure to an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (blue squares with dashed lines); no virus was detected in nasal washes of the four vaccinated animals (red triangles with solid lines). (G) Schematic representation of challenge of mock-vaccinated animals through exposure to an infected guinea pig. Two naïve contact animals were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, two previously mock-vaccinated guinea pigs were each placed into the same cage with one infected animal. (H) Results of control challenge through contact with an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (white squares with dashed lines), and both mock-vaccinated guinea pigs (black triangles with solid lines) became infected through contact with the infected animals.
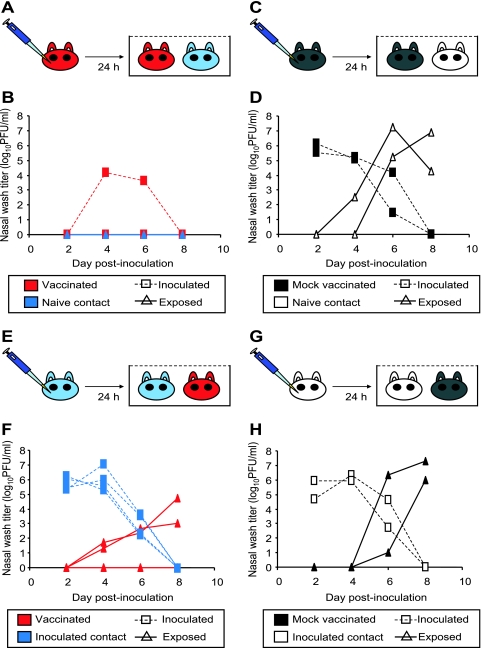
FIG. 8.
Vaccination with NS1-truncated LAIV provides partial protection against initial infection with, and full protection against secondary transmission of, heterologous virus. (A) Schematic representation of challenge by the intranasal route. Four guinea pigs previously vaccinated with LAIV (red) were challenged intranasally with Wisc/05 virus. At 24 h postinoculation, a naïve contact animal (blue) was cocaged with each of the four inoculated guinea pigs. (B) Results of heterologous challenge by the intranasal route. One of four vaccinated guinea pigs became infected upon challenge (red squares with dashed lines); none of the four naïve contact animals (blue triangles with solid lines) contracted infection. (C) Schematic representation of challenge of mock-vaccinated guinea pigs by the intranasal route. Two previously mock-vaccinated animals (black) were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, a naïve contact guinea pig (white) was cocaged with each of the two inoculated guinea pigs. (D) Results of Wisc/05 challenge of mock-vaccinated guinea pigs by the intranasal route. Mock-vaccinated guinea pigs were productively infected through inoculation (black squares with dashed lines), and transmission to both naïve contact animals was observed (white triangles with solid lines). (E) Schematic representation of heterologous challenge through exposure to an infected guinea pig. Four naïve guinea pigs were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, each acutely infected animal (blue) was placed into the same cage with one previously vaccinated guinea pig (red). (F) Results of heterologous challenge through exposure to an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (blue squares with dashed lines); two of four animals previously vaccinated with the LAIV (red triangles with solid lines) became infected through transmission of Wisc/05. (G) Schematic representation of challenge of control animals through exposure to an infected guinea pig. Two naïve contact animals were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, two previously mock-vaccinated guinea pigs were each placed into the same cage with one infected animal. (H) Results of control challenge through contact with a Wisc/05-infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (white squares with dashed lines), and both of the mock-vaccinated guinea pigs (black triangles with solid lines) became infected through contact with an infected animal.
Hemagglutination inhibition (HI) assay.
Blood samples were collected from guinea pigs prior to vaccination (at day 0), prior to challenge (at day 21 for naturally infected guinea pigs or at day 42 for vaccinated guinea pigs), and approximately 2.5 weeks following challenge (days 17 to 19 postchallenge). Trypsin-heat-periodate treatment (as described in WHO guidelines) was used to eliminate nonspecific inhibitors of hemagglutination. Briefly, 1 volume of serum was combined with a 1/2 volume of 8 mg/ml tosylsulfonyl phenylalanyl chloromethyl ketone-treated trypsin (Sigma) in 0.1 M phosphate buffer (pH 8.2) and incubated at 56°C for 30 min. Next, 3 volumes of 0.011 M potassium (meta)periodate was added, and the mixture was incubated at room temperature for 15 min. Three volumes of 1% glycerol saline was then added, and the mixture was incubated at room temperature for 15 min. Finally, 2 volumes of 85% saline was added to give a 1:10 final dilution of the initial sample.
To quantify HI activity, twofold serial dilutions of treated sera in 96-well V-bottom plates were incubated with 4 to 8 hemagglutinating units of MDCK-grown Pan/99 or Wisc/05 viruses at room temperature for 30 min. Chicken (for Pan/99) or turkey (for Wisc/05) red blood cells at 0.5% in PBS were then added, and plates were transferred to 4°C for 3 to 16 h. All serum samples collected during a given vaccine-challenge experiment were evaluated in a single HI assay. HI assays from the six experiments were not, however, performed simultaneously. The HI titer is reported as the reciprocal of the highest dilution of serum that inhibited hemagglutination.
RESULTS
Previous natural infection provides sterilizing immunity against homologous and heterologous challenges. (i) Natural infection.
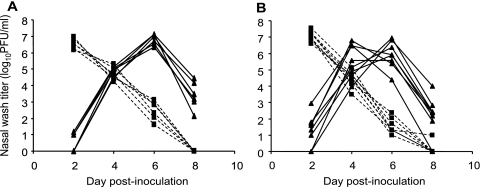
To test whether guinea pigs would be a suitable animal model in which to evaluate influenza virus vaccines, we first assessed the level of protection afforded by natural infection with wild-type influenza virus. Herein, we define natural infection as infection through the transmission of virus from another guinea pig. Thus, naturally infected guinea pigs were produced by first inoculating a set of animals intranasally with Pan/99 virus and then, at 24 h postinoculation, placing each one of these infected guinea pigs in the same cage with one naïve guinea pig. Nasal wash samples were collected from all guinea pigs, and the titers of virus therein were determined by plaque assay in order to confirm that all contact guinea pigs did contract infection (Fig. 1). These contact guinea pigs were then termed “naturally infected” and were kept for 2 weeks prior to challenge.
FIG. 1.
Natural infection through exposure to acutely infected guinea pigs. (A) Natural exposure 3 weeks prior to homologous challenge. Six guinea pigs were inoculated intranasally with 1,000 PFU Pan/99 virus. At 24 h postinoculation, a naïve guinea pig was placed into the same cage with each inoculated guinea pig. Animals were housed in this way for 7 days. (B) Natural exposure 3 weeks prior to heterologous challenge. Eight guinea pigs were inoculated intranasally with 1,000 PFU Pan/99 virus. At 24 h postinoculation, a naïve guinea pig was placed into the same cage with each inoculated guinea pig. Animals were housed in this way for 7 days. Dashed lines with squares represent nasal wash titers of inoculated animals; solid lines with triangles represent nasal wash titers of exposed animals.
(ii) Homologous challenge.
Previously infected guinea pigs and control animals with no prior exposure were challenged with Pan/99 virus through either intranasal inoculation with 1,000 PFU (Fig. 2A to D) or exposure to guinea pigs acutely infected with Pan/99 virus (Fig. 2E to H). In the case of the intranasally challenged guinea pigs, sentinel animals were included in the cage of each challenged guinea pig in order to determine whether the protection provided was sufficient to block secondary transmission. As shown in Fig. 2, previous infection with Pan/99 virus provided sterilizing immunity against both types of challenge: no virus was detected in the nasal washings of previously infected guinea pigs. Thus, no transmission occurred either to or from previously infected guinea pigs (Fig. 2B and F). In contrast, naïve control animals were productively infected and transmitted to naïve cage mates (Fig. 2D and H).
Analysis of guinea pig serum samples collected prior to infection, prior to challenge, and 17 days after challenge indicated that, as expected, animals infected with Pan/99 virus by the natural route all produced hemagglutination-inhibiting antibodies against this virus by 3 weeks postinfection (Table 1). Increases in HI titers following challenge were not observed (except in control animals), most likely due to the failure of the challenge virus to productively infect immunized guinea pigs.
TABLE 1.
Hemagglutination-inhibitory activity against Pan/99 virus of sera from guinea pigs infected naturally with Pan/99 virus
| Treatment and guinea pig | Prior infection | Route of challengec | Titer
|
||
|---|---|---|---|---|---|
| Preimmuned | Postinfectione | Postchallengef | |||
| Natural infection, homologous challengea | |||||
| 1 | None | Inoculation i.n. | ND | 10 | 80 |
| 2 | None | Inoculation i.n. | ND | 20 | 160 |
| 3 | None | Exposure | ND | 10 | 160 |
| 4 | None | Exposure | ND | 10 | 320 |
| 5 | Pan/99 | Inoculation i.n. | 10 | 160 | 160 |
| 6 | Pan/99 | Inoculation i.n. | 10 | 160 | 160 |
| 7 | Pan/99 | Inoculation i.n. | 10 | 160 | 320 |
| 8 | Pan/99 | Exposure | 10 | 160 | 320 |
| 9 | Pan/99 | Exposure | 10 | 320 | 320 |
| 10 | Pan/99 | Exposure | 10 | 320 | 320 |
| Natural infection, heterologous challengeb | |||||
| 11 | None | Inoculation i.n. | ND | 10 | 10 |
| 12 | None | Inoculation i.n. | ND | 10 | 10 |
| 13 | None | Exposure | ND | 10 | <10 |
| 14 | None | Exposure | ND | >10 | 10 |
| 15 | Pan/99 | Inoculation i.n. | 10 | 160 | 160 |
| 16 | Pan/99 | Inoculation i.n. | 10 | 160 | 160 |
| 17 | Pan/99 | Inoculation i.n. | 10 | 160 | 160 |
| 18 | Pan/99 | Inoculation i.n. | <10 | 160 | 160 |
| 19 | Pan/99 | Exposure | <10 | 80 | 160 |
| 20 | Pan/99 | Exposure | <10 | 160 | 160 |
| 21 | Pan/99 | Exposure | 10 | 320 | 320 |
| 22 | Pan/99 | Exposure | <10 | 160 | 320 |
(iii) Heterologous challenge.
Control animals and animals previously infected with Pan/99 virus were challenged either through intranasal inoculation with 1,000 PFU of Wisc/05 virus (Fig. 3A to D) or through exposure to guinea pigs acutely infected with Wisc/05 virus (Fig. 3E to H). Again, in the case of the intranasally challenged guinea pigs, sentinel animals were included in the cage of each challenged guinea pig to allow the detection of secondary transmission. As shown in Fig. 3B and F, previous infection with Pan/99 virus provided sterilizing immunity against both types of challenge with Wisc/05: no virus was detected in the nasal washings of previously infected guinea pigs. Thus, as with the homologous challenge, no transmission occurred either to or from previously infected guinea pigs. In contrast, naïve control animals were productively infected and transmitted to naïve cage mates (Fig. 3D and H).
FIG. 3.
Previously infected guinea pigs exhibit sterilizing immunity to heterologous challenge. (A) Schematic representation of challenge by the intranasal route. Four guinea pigs previously infected with Pan/99 virus (red) were challenged intranasally with Wisc/05 virus. At 24 h postinoculation, a naïve contact animal (blue) was cocaged with each of the four inoculated guinea pigs. (B) Results of heterologous challenge by the intranasal route. No virus was detected in the nasal washings of challenged guinea pigs (red squares with dashed lines), and no virus was detected in the naïve contact animals (blue triangles with solid lines). (C) Schematic representation of challenge of control guinea pigs by the intranasal route. Two control animals with no previous exposure (black) were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, a naïve contact guinea pig (white) was cocaged with each of the inoculated guinea pigs. (D) Results of Wisc/05 challenge of control guinea pigs by the intranasal route. Animals with no previous exposure were productively infected through inoculation (black squares with dashed lines). Transmission to one of two naïve contact animals was observed (white triangles with solid lines). (E) Schematic representation of challenge through exposure to an infected guinea pig. Four naïve guinea pigs were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, each acutely infected animal (blue) was placed into the same cage with one previously Pan/99 virus-infected guinea pig (red). (F) Results of heterologous challenge through exposure to an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (blue squares with dashed lines); however, the four guinea pigs with previous exposure to Pan/99 virus (red triangles with solid lines) did not become infected through contact with the infected animals. (G) Schematic representation of challenge of control animals through exposure to an infected guinea pig. Two naïve contact animals were inoculated intranasally with Wisc/05 virus. At 24 h postinoculation, two control guinea pigs with no previous exposure were each placed into the same cage with one infected animal. (H) Results of control challenge through contact with a Wisc/05-infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (white squares with dashed lines), and one of the two control guinea pigs with no previous exposure (black triangles with solid lines) became infected through contact with an infected animal.
Analysis of serum samples from guinea pigs challenged with Wisc/05 virus indicated that previous infection with Pan/99 virus by the natural route did not induce antibodies capable of inhibiting hemagglutination by Wisc/05 virus (Table 2). As shown in Table 1, these same guinea pigs did produce HI antibodies against Pan/99 virus; thus, the HA antigens of Pan/99 and Wisc/05 are sufficiently distinct to prevent cross-reactivity of immune sera in an HI assay despite the protection from challenge observed. In a manner similar to that of the homologous challenge, increases in HI titers following challenge were not observed (except in control animals), most likely due to the failure of the challenge virus to productively infect immunized guinea pigs.
TABLE 2.
Hemagglutination-inhibitory activity against Wisc/05 virus of sera from guinea pigs infected naturally with Pan/99 virus
| Guinea piga | Prior infection | Route of challengeb | Titer
|
||
|---|---|---|---|---|---|
| Preimmunec | Postinfectiond | Postchallengee | |||
| 11 | None | Inoculation i.n. | ND | <10 | <10 |
| 12 | None | Inoculation i.n. | ND | <10 | 80 |
| 13 | None | Exposure | ND | <10 | 80 |
| 14 | None | Exposure | ND | <10 | 40 |
| 15 | Pan/99 | Inoculation i.n. | <10 | <10 | <10 |
| 16 | Pan/99 | Inoculation i.n. | <10 | <10 | <10 |
| 17 | Pan/99 | Inoculation i.n. | <10 | <10 | <10 |
| 18 | Pan/99 | Inoculation i.n. | <10 | 10 | 10 |
| 19 | Pan/99 | Exposure | <10 | 10 | <10 |
| 20 | Pan/99 | Exposure | <10 | <10 | <10 |
| 21 | Pan/99 | Exposure | <10 | 10 | <10 |
| 22 | Pan/99 | Exposure | <10 | <10 | <10 |
Exposed to natural infection and heterologous challenge (see also Fig. 3).
i.n., intranasally.
ND, not done.
Postinfection blood samples were collected on day 21 after natural infection.
Postchallenge blood samples were collected on day 18 after challenge.
Vaccination with whole, killed influenza virus provides partial protection against secondary transmission but no detectable protection against infection by the natural route.
Having shown that the guinea pig immune response to influenza virus was protective against reinfection and therefore that guinea pigs can, in principle, be used to test the immunogenicity and efficacy of influenza virus vaccines, we next assessed a conventional vaccination approach for blocking transmission.
(i) Homologous challenge.
Guinea pigs vaccinated with 2 doses of intramuscularly administered, inactivated Pan/99 virus and mock-vaccinated animals were challenged with Pan/99 virus either through intranasal inoculation with 1,000 PFU (Fig. 4A to D) or through exposure to guinea pigs acutely infected with Pan/99 virus (Fig. 4E to H). In the former case, a naïve guinea pig was included in the cage of each challenged animal in order to monitor for secondary transmission. As shown in Fig. 4B, three out of four vaccinated guinea pigs became infected following intranasal challenge. The viral load in nasal washes collected from these animals was, however, lower than that of control guinea pigs (the mean peak titer obtained from vaccinated animals was 5.1 × 104 PFU/ml, compared to 1.9 × 107 PFU/ml from mock-vaccinated animals). Secondary transmission from vaccinated and challenged animals to naïve cage mates was furthermore decreased from 100% among control animals to 25%. When challenged through exposure to an infected guinea pig, all three vaccinated animals did contract infection (Fig. 4F). Thus, transmission to animals vaccinated with inactivated Pan/99 virus was of the same efficiency as that of transmission to mock-vaccinated guinea pigs (Fig. 4H).
FIG. 4.
Vaccination with inactivated virus limits secondary transmission but does not protect against initial infection with homologous virus. (A) Schematic representation of challenge by the intranasal route. Four guinea pigs previously vaccinated with inactivated Pan/99 virus (red) were challenged intranasally with 1,000 PFU of Pan/99 virus. At 24 h postinoculation, a naïve contact animal (blue) was cocaged with each of the four inoculated guinea pigs. (B) Results of homologous challenge by the intranasal route. Three of four vaccinated animals (red squares with dashed lines) became infected following intranasal challenge, and one of four naïve contact animals (blue triangles with solid lines) was subsequently infected. (C) Schematic representation of challenge of mock-vaccinated guinea pigs by the intranasal route. Two previously mock-vaccinated control animals (black) were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, a naïve contact guinea pig (white) was cocaged with each of the two inoculated guinea pigs. (D) Results of Pan/99 challenge of mock-vaccinated guinea pigs by the intranasal route. Mock-vaccinated guinea pigs were productively infected through inoculation (black squares with dashed lines) and transmitted efficiently to naïve contact animals (white triangles with solid lines). (E) Schematic representation of challenge through exposure to an infected guinea pig. Three naïve guinea pigs were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, each acutely infected animal (blue) was placed into the same cage with one vaccinated guinea pig (red). (F) Results of homologous challenge through exposure to an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (blue squares with dashed lines); all three vaccinated guinea pigs (red triangles with solid lines) became infected through contact with the infected animals. (G) Schematic representation of challenge of mock-vaccinated animals through exposure to an infected guinea pig. Two naïve contact animals were inoculated intranasally with Pan/99 virus. At 24 h postinoculation, one mock-vaccinated guinea pig was placed into the same cage with each infected animal. (H) Results of control challenge through contact with an infected guinea pig. Intranasally infected contact animals shed high titers of virus into nasal washes (white squares with dashed lines), and both mock-vaccinated guinea pigs (black triangles with solid lines) became infected through contact with the infected animals.
Analysis of guinea pig serum samples collected prior to vaccination, prior to challenge, and 19 days after challenge indicated that animals vaccinated with inactivated Pan/99 virus seroconverted against this virus by day 42 after the initial vaccination (Table 3). Increases in HI titers following challenge were observed in most cases; however, no increase in HI titer was seen for the guinea pig that showed complete protection (guinea pig 30) (Table 3). It should be noted that increases in the HI titer may relate to the kinetics of the antibody response rather than solely resulting from the challenge.
TABLE 3.
Hemagglutination-inhibitory activity against Pan/99 virus of sera from guinea pigs immunized with inactivated Pan/99 vaccine
| Treatment and guinea pig | Vaccined | Route of challengec | Titer
|
||
|---|---|---|---|---|---|
| Preimmune | Postvaccinatione | Postchallengef | |||
| Killed vaccine, homologous challengea | |||||
| 23 | PBS | Inoculation i.n. | <10 | <10 | 320 |
| 24 | PBS | Inoculation i.n. | <10 | <10 | 160 |
| 25 | PBS | Exposure | <10 | <10 | 40 |
| 26 | PBS | Exposure | <10 | <10 | 160 |
| 27 | iPan/99 | Inoculation i.n. | <10 | 640 | 1,280 |
| 28 | iPan/99 | Inoculation i.n. | <10 | 320 | 1,280 |
| 29 | iPan/99 | Inoculation i.n. | <10 | 320 | 640 |
| 30 | iPan/99 | Inoculation i.n. | <10 | 320 | 320 |
| 31 | iPan/99 | Exposure | <10 | 640 | 640 |
| 32 | iPan/99 | Exposure | <10 | 320 | 1,280 |
| 33 | iPan/99 | Exposure | <10 | 320 | ND |
| 34 | iPan/99 | Exposure | <10 | 320 | 640 |
| Killed vaccine, heterologous challengeb | |||||
| 35 | PBS | Inoculation i.n. | 10 | 10 | 10 |
| 36 | PBS | Inoculation i.n. | 10 | 10 | 10 |
| 37 | PBS | Exposure | 10 | 10 | 10 |
| 38 | PBS | Exposure | <10 | 20 | 640 |
| 39 | iPan/99 | Inoculation i.n. | 10 | 5,120 | 5,120 |
| 40 | iPan/99 | Inoculation i.n. | 10 | 640 | 1,280 |
| 41 | iPan/99 | Inoculation i.n. | 10 | 2,560 | 2,560 |
| 42 | iPan/99 | Inoculation i.n. | <10 | 640 | 1,280 |
| 43 | iPan/99 | Exposure | 10 | 1,280 | 1,280 |
| 44 | iPan/99 | Exposure | <10 | 1,280 | 2,560 |
| 45 | iPan/99 | Exposure | 10 | 1,280 | 2,560 |
| 46 | iPan/99 | Exposure | 10 | 1,280 | 2,560 |
(ii) Heterologous challenge.
Guinea pigs vaccinated with inactivated Pan/99 virus or mock vaccinated with PBS alone were challenged with Wisc/05 virus through either intranasal inoculation with 1,000 PFU (Fig. 5A to D) or exposure to animals acutely infected with Wisc/05 virus (Fig. 5E to H). As shown in Fig. 5B, all four Pan/99-vaccinated animals that were challenged intranasally did become infected with Wisc/05 virus. As in the analogous homologous challenge experiment, titers shed by the vaccinated animals were reduced by 10- to 100-fold relative to the those of the corresponding mock-vaccinated guinea pigs. Although transmission of Wisc/05 among control animals was less efficient than transmission of Pan/99 virus (often occurring for only one of two contacts), secondary transmission from vaccinees to naïve cage mates was reduced relative to that from controls. Just one out of four contact animals contracted infection from a vaccinated guinea pig (Fig. 5B). When challenged through exposure to a Wisc/05-infected guinea pig, four of four vaccinated animals became infected (Fig. 5F). Transmission to vaccinated animals occurred with similar kinetics and efficiencies as transmission to mock-vaccinated animals (Fig. 5, compare F to H), indicating that the killed vaccine did not protect against challenge by the natural route.
Analysis of serum samples from this experiment indicated that, again, all Pan/99-vaccinated animals produced hemagglutination-inhibiting antibodies against Pan/99 virus by day 42 postvaccination, whereas mock-vaccinated guinea pigs did not (Table 3). HI assays performed with Wisc/05 virus, in contrast, revealed that only two of the eight vaccinated animals seroconverted (at low titers) against this virus (Table 4). All guinea pigs did seroconvert against Wisc/05 by day 19 after challenge.
TABLE 4.
Hemagglutination-inhibitory activity against Wisc/05 virus of sera from guinea pigs immunized with inactivated Pan/99 vaccine
| Guinea piga | Vaccinec | Route of challengeb | Titer
|
||
|---|---|---|---|---|---|
| Preimmune | Postvaccinationd | Postchallengee | |||
| 35 | PBS | Inoculation I.N. | 10 | 10 | 320 |
| 36 | PBS | Inoculation I.N. | 10 | 10 | 640 |
| 37 | PBS | Exposure | 10 | 10 | 640 |
| 38 | PBS | Exposure | 10 | <10 | 320 |
| 39 | iPan/99 | Inoculation I.N. | 10 | 40 | 5,120 |
| 40 | iPan/99 | Inoculation I.N. | 10 | <10 | 640 |
| 41 | iPan/99 | Inoculation I.N. | 10 | 10 | 320 |
| 42 | iPan/99 | Inoculation I.N. | 10 | <10 | 320 |
| 43 | iPan/99 | Exposure | <10 | <10 | 160 |
| 44 | iPan/99 | Exposure | <10 | <10 | 320 |
| 45 | iPan/99 | Exposure | <10 | 10 | 640 |
| 46 | iPan/99 | Exposure | 10 | 40 | 320 |
Treated with killed vaccine, heterologous challenge (see also Fig. 5).
i.n., intranasally.
iPan/99, inactivated Pan/99 virus.
Postvaccination blood samples were collected 42 days after the initial vaccination dose was given.
Postchallenge blood samples were collected on day 18 after challenge.
Vaccination with a live attenuated influenza virus provides full protection against homologous challenge and partial protection against heterologous challenge.
Next, we wanted to test the efficacy of an LAIV in preventing transmission. For this purpose, we chose a recombinant virus which carries the HA and NA genes of Pan/99 virus and the six internal gene segments of PR8 virus, with mutations introduced into the NS1 open reading frame such that only the N-terminal 73 amino acids are expressed. Influenza viruses encoding truncated NS1 proteins have previously been shown to be highly attenuated in IFN-competent systems (38, 42, 47).
(i) Shedding of the vaccine strain.
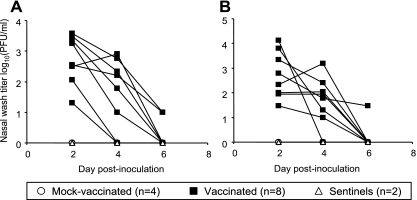
To assess the level of replication of the live attenuated Pan/99 HA NA:PR8 NS1-73 virus, we collected nasal washings from vaccinated and mock-vaccinated animals at 2, 4, and 6 days after the initial dose was administered. In addition, to evaluate the propensity of the vaccine strain to transmit to naïve contacts, we included two sentinel guinea pigs in the experiment. Each sentinel guinea pig was placed into the same cage with two vaccinated guinea pigs 24 h after inoculation with LAIV. Nasal wash samples were collected from the sentinel animals in order to monitor for transmission. As shown in Fig. 6, maximum titers shed by the vaccinated guinea pigs ranged from 20 to 13,000 PFU/ml. No virus was detected in nasal washings obtained from the sentinel guinea pigs, indicating that the Pan/99 HA NA:PR8 NS1-73 virus does not transmit.
FIG. 6.
Shedding titers of NS1-truncated LAIV following initial administration. (A) Nasal wash titers of Pan/99 HA NA:PR8 NS1-73-vaccinated animals 6 weeks prior to challenge with Pan/99 virus. (B) Nasal wash titers of Pan/99 HA NA:PR8 NS1-73-vaccinated animals 6 weeks prior to challenge with Wisc/05 virus. Solid squares show titers shed by vaccinated animals, open circles show titers obtained from mock-vaccinated controls, and open triangles show results from two sentinel guinea pigs, each housed in the same cage with two vaccinated guinea pigs.
The wide range of titers shed by vaccinated guinea pigs was unexpected based on previous results with wild-type influenza virus strains. Although shedding from humans vaccinated with caLAIV is variable, this is most likely due to differences in preexisting adaptive immunity (6), whereas all guinea pigs used herein were serologically negative at the start of the experiment. Given that Hartley strain guinea pigs are outbred, differences in innate immune responses may account for the observed range of titers. This effect may be exacerbated in the case of an NS1-truncated virus relative to strains with an intact IFN antagonist.
(ii) Homologous challenge.
Guinea pigs vaccinated with 2 doses of intranasally administered Pan/99 HA NA:PR8 NS1-73 virus and mock-vaccinated animals were challenged with Pan/99 virus either through intranasal inoculation with 1,000 PFU (Fig. 7A to D) or through exposure to guinea pigs acutely infected with Pan/99 virus (Fig. 7E to H). As described above, a naïve contact animal was placed into the same cage with each intranasally challenged guinea pig in order to evaluate the efficiency of secondary transmission. As shown in Fig. 7B and F, vaccination with this live attenuated virus provided sterilizing immunity against both types of challenge; no transmission was observed either from or to vaccinated animals.
HI assays performed on sera collected from the animals in this experiment showed that all eight vaccinated guinea pigs seroconverted against Pan/99 virus by day 42 postvaccination (Table 5). The HI titers of these guinea pigs did not increase following challenge, most likely due to the lack of replication of the challenge virus. As expected, mock-vaccinated guinea pigs did not seroconvert following vaccination with PBS but did seroconvert by 18 days postchallenge.
TABLE 5.
Hemagglutination-inhibitory activity against Pan/99 virus of sera from guinea pigs immunized with Pan/99-based live attenuated vaccine
| Treatment and guinea pig | Vaccine | Route of challengec | Titer
|
||
|---|---|---|---|---|---|
| Preimmune | Postvaccinationd | Postchallengee | |||
| Live attenuated vaccine, homologous challengea | |||||
| 47 | PBS | Inoculation i.n. | 10 | 10 | 320 |
| 48 | PBS | Inoculation i.n. | 10 | 10 | 320 |
| 49 | PBS | Exposure | 10 | 10 | 320 |
| 50 | PBS | Exposure | 10 | 10 | 160 |
| 51 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | 10 | 320 | 160 |
| 52 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | 10 | 320 | 320 |
| 53 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | 10 | 320 | 320 |
| 54 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | 10 | 160 | 160 |
| 55 | Pan/99 HA NA:PR8 NS1-73 | Exposure | 10 | 320 | 320 |
| 56 | Pan/99 HA NA:PR8 NS1-73 | Exposure | 10 | 320 | 320 |
| 57 | Pan/99 HA NA:PR8 NS1-73 | Exposure | 10 | 160 | 160 |
| 58 | Pan/99 HA NA:PR8 NS1-73 | Exposure | 10 | 160 | 160 |
| Live attenuated vaccine, heterologous challengeb | |||||
| 59 | PBS | Inoculation i.n. | 10 | 10 | 20 |
| 60 | PBS | Inoculation i.n. | 10 | 10 | 20 |
| 61 | PBS | Exposure | 10 | 10 | 10 |
| 62 | PBS | Exposure | 10 | 10 | 80 |
| 63 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | 10 | 1,280 | 1,280 |
| 64 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | 10 | 1,280 | 2,560 |
| 65 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | <10 | 640 | 640 |
| 66 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | 10 | 2,560 | 2,560 |
| 67 | Pan/99 HA NA:PR8 NS1-73 | Exposure | 10 | 1,280 | 5,120 |
| 68 | Pan/99 HA NA:PR8 NS1-73 | Exposure | 10 | 5,120 | 2,560 |
| 69 | Pan/99 HA NA:PR8 NS1-73 | Exposure | 10 | 1,280 | 2,560 |
| 70 | Pan/99 HA NA:PR8 NS1-73 | Exposure | 10 | 1,280 | 2,560 |
(iii) Heterologous challenge.
Guinea pigs vaccinated intranasally with Pan/99 HA NA:PR8 NS1-73 virus or mock vaccinated with PBS were challenged either by intranasal inoculation of 1,000 PFU Wisc/05 virus (Fig. 8A to D) or by exposure to guinea pigs infected with Wisc/05 virus (Fig. 8E to H). As shown in Fig. 8B, no virus was detected in the nasal washings collected from three of four intranasally challenged guinea pigs, while titers shed by the fourth vaccinated animal were decreased relative to those of mock-vaccinated controls (Fig. 8, compare B to D). Furthermore, no transmission from vaccinated and challenged guinea pigs to their naïve cage mates was observed (Fig. 8B). When challenged through contact with infected guinea pigs, two of four LAIV-vaccinated animals became infected (Fig. 8F). As with the intranasally challenged guinea pig, the viral load in these two animals was reduced relative to those of controls (Fig. 8, compare F to H).
HI assays of serum samples collected from LAIV-vaccinated animals indicated that they seroconverted against Pan/99 virus by 3 weeks after the second dose of vaccine was administered (Table 5). The variation in HI titers seen was not found to correlate with the magnitude of virus shedding following the administration of the first vaccine dose. The HI titers were, however, measured following the application of a second dose; thus, the extent of viral growth upon boost may have influenced the level of serum antibodies. The Pan/99 HA NA:PR8 NS1-73-vaccinated animals did not produce antibodies that were cross-reactive with Wisc/05 virus, as determined by HI assay (Table 6). Following challenge, all four mock-vaccinated control guinea pigs seroconverted against Wisc/05 virus, as did two of the vaccinated animals that were challenged intranasally and three of the guinea pigs that were challenged through exposure (Table 6). The vaccinated animals from which virus was isolated following challenge (guinea pigs 64, 67, and 68) (Table 6) were also found to seroconvert by day 17 postchallenge. In addition, two guinea pigs that did not shed Wisc/05 virus in postchallenge nasal washings did seroconvert (guinea pigs 63 and 70) (Table 6).
TABLE 6.
Hemagglutination-inhibitory activity against Wisc/05 virus of sera from guinea pigs immunized with Pan/99-based live attenuated vaccine
| Guinea piga | Vaccine | Route of challengeb | Titer
|
||
|---|---|---|---|---|---|
| Preimmune | Postinfectionc | Postchallenged | |||
| 59 | PBS | Inoculation i.n. | <10 | <10 | 640 |
| 60 | PBS | Inoculation i.n. | <10 | <10 | 320 |
| 61 | PBS | Exposure | <10 | <10 | 80 |
| 62 | PBS | Exposure | <10 | <10 | 160 |
| 63 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | <10 | 20 | 80 |
| 64 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | 10 | <10 | 80 |
| 65 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | <10 | <10 | <10 |
| 66 | Pan/99 HA NA:PR8 NS1-73 | Inoculation i.n. | <10 | 10 | 20 |
| 67 | Pan/99 HA NA:PR8 NS1-73 | Exposure | <10 | <10 | 40 |
| 68 | Pan/99 HA NA:PR8 NS1-73 | Exposure | <10 | <10 | 40 |
| 69 | Pan/99 HA NA:PR8 NS1-73 | Exposure | <10 | <10 | 10 |
| 70 | Pan/99 HA NA:PR8 NS1-73 | Exposure | <10 | <10 | 80 |
Treated with live attenuated vaccine, heterologous challenge (see also Fig. 8).
i.n., intranasally.
Postvaccination blood samples were collected 42 days after the initial vaccination dose was given.
Postchallenge blood samples were collected on day 17 after challenge.
DISCUSSION
By showing that guinea pigs previously infected with Pan/99 influenza virus are immune to reinfection with the same strain, we have established that guinea pigs are, in principle, a suitable animal model for testing the immunogenicity and protective efficacy of influenza virus vaccines. The utility of the guinea pig model was furthermore demonstrated by evaluating the potential of inactivated virus and LAIV vaccines to block transmission. We found that live virus with a truncated NS1 open reading frame was more effective in protecting against both homologous and heterologous H3 subtype challenge than the inactivated vaccine. Although the live vaccine was more effective, both types of vaccination reduced transmission from vaccinated and challenged guinea pigs to their naïve cage mates. In contrast, only the live vaccine, and not the killed vaccine, prevented transmission from acutely infected guinea pigs to vaccinated animals.
For the present studies, we chose to challenge all animals at a single time point of 3 weeks following the final vaccination. The longevity of the protection offered by each type of vaccine was therefore not addressed herein but is an important topic for further research. It is not clear whether live attenuated or inactivated influenza virus vaccines offer longer-lasting protection (1, 3, 24); thus, our findings on the relative efficacy of the LAIV and killed vaccines may have been different at a later time postvaccination. In addition, it is possible that nonspecific immunity induced following infection with wild-type virus or LAIV may still be present at 3 weeks postinfection and could therefore have contributed to the superior protection seen with live-virus vaccination.
Our results with both the inactivated and live attenuated vaccines suggested that challenge through exposure to an infected guinea pig constitutes a more stringent challenge than intranasal inoculation with 1,000 PFU; that is, animals immunized with either vaccine were more likely to become infected if challenge was of the contact exposure type. We hypothesize that the extended exposure of vaccinated guinea pigs to their infected cage mates, in contrast to the defined dose of 1,000 PFU administered intranasally, likely accounts for the increased stringency. An alternative possibility is that virus produced in and expelled from the guinea pig respiratory tract is more infectious to guinea pigs than virus grown in laboratory substrates. The finding that conventional means of challenge are not necessarily representative of natural exposures may be important to take into account in future vaccine-challenge studies.
Although immunization by all three methods tested led to the production of hemagglutination-inhibiting antibodies against Pan/99 virus, protection against challenge did not correlate well with HI titers. In particular, animals vaccinated with the killed virus vaccine developed high HI titers but were protected less well than wild-type- or LAIV-infected animals. Furthermore, full protection against heterologous challenge with Wisc/05 virus was observed in all Pan/99 virus-infected and some Pan/99 HA NA:PR8 NS1-73 virus-infected guinea pigs despite the absence of hemagglutination-inhibiting antibodies. Previous reports indicated that inactivated influenza virus vaccines may induce greater serum HI antibody responses than live vaccines; live vaccines, in contrast, tend to induce higher levels of mucosal immunoglobulin A antibodies (13, 49). The observation that protection afforded by vaccination with live attenuated influenza virus does not always correlate with serum antibody responses has also been previously documented (5). The finding that HI titers were not always predictive of protection following challenge suggests that components of the immune response besides neutralizing antibodies are important to limiting influenza virus infection. The source of the protection afforded to animals without detectable hemagglutination-inhibiting antibodies in serum may have been nonneutralizing antibodies against viral antigens (45) or, particularly in the cases of immunization through infection with wild-type or live attenuated viruses, mucosal antibodies (8) or T-cell-based immunity (32). The basis of the observed cross-reactive immune response will be investigated further in subsequent experiments.
The benefits of reducing person-to-person transmission in the context of either an epidemic or a pandemic are clear. It is therefore appropriate that one of the main aims of vaccination is to limit transmission. Nevertheless, the efficacy of vaccines in blocking viral spread, either to or from the vaccinated individual, is not traditionally assessed in preclinical or clinical trials. Herein, we present an animal model and a systematic approach that can be applied to new or existing vaccines for this purpose. The benefits of evaluating vaccines for their potential to limit transmission are twofold. First, suboptimal vaccines may provide only partial protection against infection but still be very effective at limiting transmission (as seen herein with an inactivated vaccine and in heterologous challenge of LAIV-vaccinated animals). In a situation where an optimal vaccine, which provides sterilizing immunity against the circulating strain, is not available, a vaccine which blocks transmission will be effective in reducing the impact of an epidemic or pandemic. Second, some suboptimal vaccines may reduce symptoms of disease but not prevent transmission (46). In such a case, infection in vaccinated individuals would be difficult to detect, but transmission from those individuals would fuel the outbreak. A vaccine which limits the reproductive rate of influenza virus is more likely to have an impact on the morbidity and mortality attributable to influenza virus.
In conclusion, we have demonstrated the utility and feasibility of evaluating influenza virus vaccines in the guinea pig model specifically in terms of the reduction in viral transmission that each vaccine achieves.
Acknowledgments
We thank Lily Ngai for excellent technical assistance and Natalie Pica for help with preliminary experiments.
This work was supported by funding from the Center for Research on Influenza Pathogenesis (NIAID contract number HHSN266200700010C), the W.M. Keck Foundation, and the Center for Investigating Viral Immunity and Antagonism (grant number 1 UC19 AI062623-023) (to P.P.). A.C.L. is a Parker B. Francis Fellow in Pulmonary Research. S.M. was supported by Sunnybrook Health Sciences Centre, Toronto, Canada, and a Ruth L. Kirschstein Physician Scientist Research Training in Pathogenesis of Viral Diseases award (award number ST32A1007623-07) (Mary Klotman, principal investigator).
We disclose that Mount Sinai School of Medicine owns patent positions for reverse genetics of influenza virus and for NS1-based live attenuated vaccines.
Footnotes
Published ahead of print on 19 January 2009.
REFERENCES
- 1.Belshe, R. B. 2004. Current status of live attenuated influenza virus vaccine in the US. Virus Res. 103177-185. [DOI] [PubMed] [Google Scholar]
- 2.Belshe, R. B. 2007. Translational research on vaccines: influenza as an example. Clin. Pharmacol. Ther. 82745-749. [DOI] [PubMed] [Google Scholar]
- 3.Belshe, R. B., K. M. Edwards, T. Vesikari, S. V. Black, R. E. Walker, M. Hultquist, G. Kemble, and E. M. Connor. 2007. Live attenuated versus inactivated influenza vaccine in infants and young children. N. Engl. J. Med. 356685-696. [DOI] [PubMed] [Google Scholar]
- 4.Belshe, R. B., W. C. Gruber, P. M. Mendelman, I. Cho, K. Reisinger, S. L. Block, J. Wittes, D. Iacuzio, P. Piedra, J. Treanor, J. King, K. Kotloff, D. I. Bernstein, F. G. Hayden, K. Zangwill, L. Yan, and M. Wolff. 2000. Efficacy of vaccination with live attenuated, cold-adapted, trivalent, intranasal influenza virus vaccine against a variant (A/Sydney) not contained in the vaccine. J. Pediatr. 136168-175. [DOI] [PubMed] [Google Scholar]
- 5.Beyer, W. E. P., A. M. Palache, J. C. de Jong, and A. D. M. E. Osterhaus. 2002. Cold-adapted live influenza vaccine versus inactivated vaccine: systemic vaccine reactions, local and systemic antibody response, and vaccine efficacy: a meta-analysis. Vaccine 201340-1353. [DOI] [PubMed] [Google Scholar]
- 6.Block, S. L., R. Yogev, F. G. Hayden, C. S. Ambrose, W. Zeng, and R. E. Walker. 2008. Shedding and immunogenicity of live attenuated influenza vaccine virus in subjects 5-49 years of age. Vaccine 264940-4946. [DOI] [PubMed] [Google Scholar]
- 7.Bouvier, N. M., A. C. Lowen, and P. Palese. 2008. Oseltamivir-resistant influenza A viruses are transmitted efficiently among guinea pigs by direct contact but not by aerosol. J. Virol. 8210052-10058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7a.Bradford, M. M. 1976. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 72248-254. [DOI] [PubMed] [Google Scholar]
- 8.Brandtzaeg, P. 2003. Role of mucosal immunity in influenza. Dev. Biol. (Basel) 11539-48. [PubMed] [Google Scholar]
- 9.Bridges, C. B., W. W. Thompson, M. I. Meltzer, G. R. Reeve, W. J. Talamonti, N. J. Cox, H. A. Lilac, H. Hall, A. Klimov, and K. Fukuda. 2000. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: a randomized controlled trial. JAMA 2841655-1663. [DOI] [PubMed] [Google Scholar]
- 10.Carrat, F., E. Vergu, N. M. Ferguson, M. Lemaitre, S. Cauchemez, S. Leach, and A. J. Valleron. 2008. Time lines of infection and disease in human influenza: a review of volunteer challenge studies. Am. J. Epidemiol. 167775-785. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. 2008. Prevention and control of influenza—recommendations of the Advisory Committee on Immunization Practices. MMWR Morb. Mortal. Wkly. Rep. 571-60.18185492 [Google Scholar]
- 12.Chambers, T. M., M. Quinlivan, T. Sturgill, A. Cullinane, D. W. Horohov, D. Zamarin, S. Arkins, A. García-Sastre, and P. Palese. Influenza A viruses with truncated NS1 as modified live virus vaccines: pilot studies of safety and efficacy in horses. Equine Vet. J., in press. [DOI] [PMC free article] [PubMed]
- 13.Clements, M. L., and B. R. Murphy. 1986. Development and persistence of local and systemic antibody responses in adults given live attenuated or inactivated influenza A virus vaccine. J. Clin. Microbiol. 2366-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diebold, S. S., M. Montoya, H. Unger, L. Alexopoulou, P. Roy, L. E. Haswell, A. Al-Shamkhani, R. Flavell, P. Borrow, and C. Reis e Sousa. 2003. Viral infection switches non-plasmacytoid dendritic cells into high interferon producers. Nature 424324-328. [DOI] [PubMed] [Google Scholar]
- 15.Ferko, B., J. Stasakova, J. Romanova, C. Kittel, S. Sereinig, H. Katinger, and A. Egorov. 2004. Immunogenicity and protection efficacy of replication-deficient influenza A viruses with altered NS1 genes. J. Virol. 7813037-13045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fox, J. P., M. K. Cooney, C. E. Hall, and H. M. Foy. 1982. Influenzavirus infections in Seattle families, 1975-1979. II. Pattern of infection in invaded households and relation of age and prior antibody to occurrence of infection and related illness. Am. J. Epidemiol. 116228-242. [DOI] [PubMed] [Google Scholar]
- 17.Glezen, W. P. 2006. Herd protection against influenza. J. Clin. Virol. 37237-243. [DOI] [PubMed] [Google Scholar]
- 18.Glezen, W. P., and R. B. Couch. 1978. Interpandemic influenza in the Houston area, 1974-76. N. Engl. J. Med. 298587-592. [DOI] [PubMed] [Google Scholar]
- 19.Gross, P. A., A. W. Hermogenes, H. S. Sacks, J. Lau, and R. A. Levandowski. 1995. The efficacy of influenza vaccine in elderly persons. A meta-analysis and review of the literature. Ann. Intern. Med. 123518-527. [DOI] [PubMed] [Google Scholar]
- 20.Hai, R., L. Martinez-Sobrido, K. A. Fraser, J. Ayllon, A. Garcia-Sastre, and P. Palese. 2008. Influenza B virus NS1-truncated mutants: live-attenuated vaccine approach. J. Virol. 8210580-10590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jefferson, T., D. Rivetti, A. Rivetti, M. Rudin, C. Di Pietrantonj, and V. Demicheli. 2005. Efficacy and effectiveness of influenza vaccines in elderly people: a systematic review. Lancet 3661165-1174. [DOI] [PubMed] [Google Scholar]
- 22.Jin, H., B. Lu, H. Zhou, C. Ma, J. Zhao, C. F. Yang, G. Kemble, and H. Greenberg. 2003. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 30618-24. [DOI] [PubMed] [Google Scholar]
- 23.Johnson, N. P. A. S., and J. Mueller. 2002. Updating the accounts: global mortality of the 1918-1920 “Spanish” influenza pandemic. Bull. Hist. Med. 76105-115. [DOI] [PubMed] [Google Scholar]
- 24.Khan, A. S., F. Polezhaev, R. Vasiljeva, V. Drinevsky, J. Buffington, H. Gary, A. Sominina, W. Keitel, H. Regnery, N. L. Lonskaya, E. Doroshenko, A. Gavrilov, I. Ivakhov, N. Arden, L. B. Schonberger, R. Couch, A. Kendal, and N. Cox. 1996. Comparison of US inactivated split-virus and Russian live attenuated, cold-adapted trivalent influenza vaccines in Russian schoolchildren. J. Infect. Dis. 173453-456. [DOI] [PubMed] [Google Scholar]
- 25.Kumar, R., and E. A. Burns. 2008. Age-related decline in immunity: implications for vaccine responsiveness. Expert Rev. Vaccines 7467-479. [DOI] [PubMed] [Google Scholar]
- 26.Lopez, C. B., A. Garcia-Sastre, B. R. Williams, and T. M. Moran. 2003. Type I interferon induction pathway, but not released interferon, participates in the maturation of dendritic cells induced by negative-strand RNA viruses. J. Infect. Dis. 1871126-1136. [DOI] [PubMed] [Google Scholar]
- 27.Lowen, A. C., S. Mubareka, J. Steel, and P. Palese. 2007. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 31470-1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lowen, A. C., S. Mubareka, T. M. Tumpey, A. García-Sastre, and P. Palese. 2006. The guinea pig as a transmission model for human influenza viruses. Proc. Natl. Acad. Sci. USA 1039988-9992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lowen, A. C., J. Steel, S. Mubareka, and P. Palese. 2008. High temperature (30°C) blocks aerosol but not contact transmission of influenza virus. J. Virol. 825650-5652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mangtani, P., P. Cumberland, C. R. Hodgson, J. A. Roberts, F. T. Cutts, and A. J. Hall. 2004. A cohort study of the effectiveness of influenza vaccine in older people, performed using the United Kingdom general practice research database. J. Infect. Dis. 1901-10. [DOI] [PubMed] [Google Scholar]
- 31.Manzoli, L., F. Schioppa, A. Boccia, and P. Villari. 2007. The efficacy of influenza vaccine for healthy children: a meta-analysis evaluating potential sources of variation in efficacy estimates including study quality. Pediatr. Infect. Dis. J. 2697-106. [DOI] [PubMed] [Google Scholar]
- 32.McMichael, A. J., F. M. Gotch, G. R. Noble, and P. A. Beare. 1983. Cytotoxic T-cell immunity to influenza. N. Engl. J. Med. 30913-17. [DOI] [PubMed] [Google Scholar]
- 33.Monto, A. S., F. M. Davenport, J. A. Napier, and T. Francis, Jr. 1970. Modification of an outbreak of influenza in Tecumseh, Michigan by vaccination of schoolchildren. J. Infect. Dis. 12216-25. [DOI] [PubMed] [Google Scholar]
- 34.Negri, E., C. Colombo, L. Giordano, N. Groth, G. Apolone, and C. La Vecchia. 2005. Influenza vaccine in healthy children: a meta-analysis. Vaccine 232851-2861. [DOI] [PubMed] [Google Scholar]
- 35.Nichol, K. L., P. M. Mendelman, K. P. Mallon, L. A. Jackson, G. J. Gorse, R. B. Belshe, W. P. Glezen, and J. Wittes. 1999. Effectiveness of live, attenuated intranasal influenza virus vaccine in healthy, working adults: a randomized controlled trial. JAMA 282137-144. [DOI] [PubMed] [Google Scholar]
- 36.Nichol, K. L., J. D. Nordin, D. B. Nelson, J. P. Mullooly, and E. Hak. 2007. Effectiveness of influenza vaccine in the community-dwelling elderly. N. Engl. J. Med. 3571373-1381. [DOI] [PubMed] [Google Scholar]
- 37.Piedra, P. A., M. J. Gaglani, C. A. Kozinetz, G. Herschler, M. Riggs, M. Griffith, C. Fewlass, M. Watts, C. Hessel, J. Cordova, and W. P. Glezen. 2005. Herd immunity in adults against influenza-related illnesses with use of the trivalent-live attenuated influenza vaccine (CAIV-T) in children. Vaccine 231540-1548. [DOI] [PubMed] [Google Scholar]
- 38.Quinlivan, M., D. Zamarin, A. Garcia-Sastre, A. Cullinane, T. Chambers, and P. Palese. 2005. Attenuation of equine influenza viruses through truncations of the NS1 protein. J. Virol. 798431-8439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reichert, T. A., N. Sugaya, D. S. Fedson, W. P. Glezen, L. Simonsen, and M. Tashiro. 2001. The Japanese experience with vaccinating schoolchildren against influenza. N. Engl. J. Med. 344889-896. [DOI] [PubMed] [Google Scholar]
- 40.Richt, J. A., P. Lekcharoensuk, K. M. Lager, A. L. Vincent, C. M. Loiacono, B. H. Janke, W. H. Wu, K. J. Yoon, R. J. Webby, A. Solorzano, and A. Garcia-Sastre. 2006. Vaccination of pigs against swine influenza viruses by using an NS1-truncated modified live-virus vaccine. J. Virol. 8011009-11018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smith, S., V. Demicheli, C. Di Pietrantonj, A. R. Harnden, T. Jefferson, N. J. Matheson, and A. Rivetti. 2006. Vaccines for preventing influenza in healthy children. Cochrane Database Syst. Rev. 2006CD004879. [DOI] [PubMed] [Google Scholar]
- 42.Solórzano, A., R. J. Webby, K. M. Lager, B. H. Janke, A. García-Sastre, and J. A. Richt. 2005. Mutations in the NS1 protein of swine influenza virus impair anti-interferon activity and confer attenuation in pigs. J. Virol. 797535-7543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Steel, J., A. C. Lowen, L. Pena, M. Angel, A. Solórzano, R. Albrecht, D. R. Perez, A. García-Sastre, and P. Palese. 2009. Live attenuated influenza viruses containing NS1 truncations as vaccine candidates against H5N1 highly pathogenic avian influenza. J. Virol. 831742-1753. [DOI] [PMC free article] [PubMed]
- 44.Steel, J., and P. Palese. 2008. The 1918 influenza pandemic: lessons from the past raise questions for the future, p. 272-286. In H. D. Klenk, M. N. Matrosovich, and J. Stech (ed.), Avian influenza, vol. 27. Karger, Basel, Switzerland. [Google Scholar]
- 45.Straight, T., M. Ottolini, G. Prince, and M. Eichelberger. 2008. Antibody contributes to heterosubtypic protection against influenza A-induced tachypnea in cotton rats. Virol. J. 544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swayne, D. E. 26 April 2008. Avian influenza vaccines and therapies for poultry. Comp. Immunol. Microbiol. Infect. Dis. [Epub ahead of print.] doi: 10.1016/j.cimid.2008.01.006. [DOI] [PubMed]
- 47.Talon, J., M. Salvatore, R. E. O'Neill, Y. Nakaya, H. Zheng, T. Muster, A. Garcia-Sastre, and P. Palese. 2000. Influenza A and B viruses expressing altered NS1 proteins: a vaccine approach. Proc. Natl. Acad. Sci. USA 974309-4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thompson, W. W., D. K. Shay, E. Weintraub, L. Brammer, N. Cox, L. J. Anderson, and K. Fukuda. 2003. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA 289179-186. [DOI] [PubMed] [Google Scholar]
- 49.Treanor, J. J., K. Kotloff, R. F. Betts, R. Belshe, F. Newman, D. Iacuzio, J. Wittes, and M. Bryant. 1999. Evaluation of trivalent, live, cold-adapted (CAIV-T) and inactivated (TIV) influenza vaccines in prevention of virus infection and illness following challenge of adults with wild-type influenza A (H1N1), A (H3N2), and B viruses. Vaccine 18899-906. [DOI] [PubMed] [Google Scholar]
- 50.Vincent, A. L., W. Ma, K. M. Lager, B. H. Janke, R. J. Webby, A. Garcia-Sastre, and J. A. Richt. 2007. Efficacy of intranasal administration of a truncated NS1 modified live influenza virus vaccine in swine. Vaccine 257999-8009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilde, J. A., J. A. McMillan, J. Serwint, J. Butta, M. A. O'Riordan, and M. C. Steinhoff. 1999. Effectiveness of influenza vaccine in health care professionals: a randomized trial. JAMA 281908-913. [DOI] [PubMed] [Google Scholar]