Portal vein thrombosis (PVT) or thrombosis of its tributaries has been a formidable surgical challenge in orthotopic hepatic transplantation (OHT). At one time, PVT was considered a relative contraindication for OHT. However, refinements of the technique to reconstruct the portal vein after thrombosis have included venous grafting procedures (1, 2). The technique of the venous “jump” graft from the superior mesenteric vein (SMV) for PVT has been standardized and should be considered in cases of PVT to establish portal flow to the hepatic allograft (1-5). One of the limiting factors of the venous jump-graft technique is the lack of a sufficient segment of SMV from which the venous graft can be anastomosed. Herein, we report a technique of anastomosing two iliac venous allografts separately to two jejunal branches of the SMV to reconstitute portal vein flow to the hepatic allograft in a patient with both portal vein and SMV thrombosis.
TECHNIQUE
A 73-year-old woman with hepatic failure secondary to primary biliary cirrhosis underwent an OHT on November 11, 1995. During evaluation for transplantation, a Doppler ultrasonography showed a thrombosed portal vein. Subsequently, an angiogram confirmed PVT extending caudally with involvement of the confluence of the SMV and the portal vein. At the time of operation, exploration of the SMV (4, 6) revealed a thrombosed retropancreatic segment of the SMV. Two vein branches were identified in the mesenteric root, each with a diameter not exceeding 1 cm. To establish an adequate portal flow to the donor liver, the entire venous iliac allograft from the same donor, constituted by the inferior vena cava and the two common iliac veins (7), was brought into the operative field. The donor’s two iliac veins were anastomosed, each one separately to the two SMV branches of the recipient, in an end-to-side fashion. After the two anastomoses were completed and the clamps released, the bifurcated caval-iliac allograft filled promptly, assuming a “pants” configuration. The hepatectomy was then performed using a piggy-back technique (8). The donor portal vein was anastomosed end-to-end to the interior vena cava of the caval-iliac allograft previously brought in the supramesocolic area through an avascular window of the transverse mesocolon (Fig. 1).
Fig. 1.
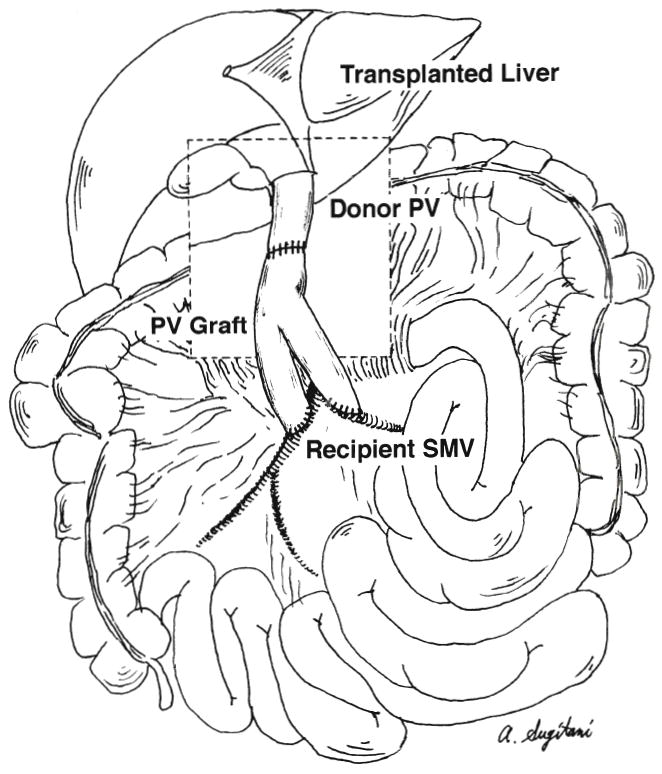
The “pants” graft. The donor iliac veins are anastomosed end-to-side to two jejunal branches of the superior mesentenic vein. The donor portal vein is anastomosed end-to-end to the inferior vena cava of the caval-iliac allograft. For the sake of clarity, the transverse mesocolon and the transverse colon have been deleted in the window. SMV, Superior mesenteric vein, and PV, portal vein.
The liver perfused promptly and produced bile immediately, and the transplantation was completed with the rearterialization of the hepatic allograft and reconstruction of the bile duct with a Roux-en-Y technique. The total blood loss was 6 U of packed red blood cells.
Two subsequent Doppler ultrasonographic examinations performed during the first two weeks after the OHT showed good portal venous flow in the hepatic allograft. The patient left the hospital two weeks after the OHT, and hepatic function was normal.
DISCUSSION
Thrombosis of the portal vein constitutes a surgical challenge during OHT. The use of a venous jump graft from the SMV has been considered the standardized method of revascularization in cases of PVT (1-4). Problems with this technique may arise if the thrombosis involves the SMV at the site of the surgically accessible segment of the vein (4, 6).
In the case reported, a previous angiogram (one year before OHT) had revealed a patent SMV; however, at the time of OHT, the SMV appeared thrombosed with sclerosis of the vein wall. Two venous branches were identified as suitable sites for the venous inflow of the graft. These two branches were separated and not in continuity with each other. Although evidence is lacking that the venous flow provided by two sites would be better than the flow from just one site, compartmentalized portal hypertension has been noted in certain situations such as in the presence of splenic thrombosis. The absence of a clear anatomical communication between these two veins made us wary that reconstructing the portal vein using a single venous branch may not have provided enough venous flow to the hepatic allograft during reperfusion.
References
- 1.Starzl TE, Halgrimson CG, Koep LJ, et al. Vascular homografts from cadaveric organ donors. Surg Gynecol Obstet. 1979;149:76–77. [PMC free article] [PubMed] [Google Scholar]
- 2.Shaw WB, Iwatsuki S, Bron KM, et al. Portal vein graft in hepatic transplantation. Surg Gynecol Obstet. 1985;161:66–68. [PMC free article] [PubMed] [Google Scholar]
- 3.Burdick JF, Pitt HA, Colombani PM, et al. Superior mesenteric vein inflow for liver transplantation when the portal vein is occluded. Surgery. 1990;107:342–345. [PubMed] [Google Scholar]
- 4.Stieber AC, Zetti G, Todo S, et al. The spectrum of portal vein thrombosis in liver transplantation. Ann Surg. 1991;213:199–206. doi: 10.1097/00000658-199103000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moreno-Gonzalez E, Garcia Garcia I, Gomez Sanz R, et al. Liver transplantation in patients with thrombosis of the portal, splenic or superior mesenteric vein. Br J Surg. 1993;80:81–85. doi: 10.1002/bjs.1800800127. [DOI] [PubMed] [Google Scholar]
- 6.Cameron JL. Rapid exposure of the portal and superior mesenteric veins. Surg Gynecol Obstet. 1993;176:395–398. [PubMed] [Google Scholar]
- 7.Starzl TE, Hakala TR, Shaw WB, et al. A flexible procedure for multiple organ procurement. Surg Gyneol Obstet. 1984;158:223–230. [PMC free article] [PubMed] [Google Scholar]
- 8.Tzakis A, Todo S, Starzl TE. Orthotopic liver transplantation with preservation of the inferior vena cava. Ann Surg. 1989;210:649–652. doi: 10.1097/00000658-198911000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]


