Abstract
We describe the architecture of a virtual patient model, the Virtual ED Patient, for scenarios in emergency medicine. The model is rule-based, and uses four vital signs as a representation of its state. The model is used in a multi-person learning environment based on online gaming technology. The efficacy of the model and the Virtual ED learning environment is evaluated in a study where advanced medical students and first year residents manage six trauma cases. Pre and post-test performance results show significant learning, with results comparable to those obtained in human manikin simulators. Some future directions for development of the model are also presented.
Introduction
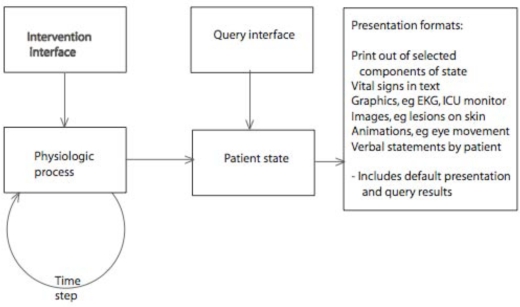
Numerous patient simulations have been developed, with underlying medical models. Most of these simulations have been a snapshot of the patient’s condition (patient state) at the time of encounter with the physician (learner). In these cases, the simulation represents a single medical state, often in considerable detail, and with relevant graphics, audio and visual media displaying the patient’s medical condition1. Some simulations support the evolution of the patient’s state, both with and without medical intervention. Figure 1 is a generalized representation of such Virtual Patient models.
Figure 1.
Block Diagram of Virtual Patient medical model and patient presentation
The medical model is represented by the “Physiologic Process” block together with the evolution of the physiologic process, as represented by the feedback loop “Time Step”. The “Intervention interface” represents the ability to change the physiologic state through clinical, surgical or pharmacologic intervention. The “Patient state” is represented by the current values of the “Physiologic process” variables. The “Patient State” is presented to the learner in many ways. The “Query interface” is the method through which the learner can obtain additional information about or from the patient. Some of this information may be available by default, such as the initial appearance of the patient, or the report from the referring physician or the ambulance personnel. In the simplest form, the presentation can be in text and numbers. Alternatively, rich multimedia may be used. The choice of presentation format is usually based on the learning goal. Some of the “Patient state” variables may not be observable, or may require sophisticated and time consuming tests.
Method
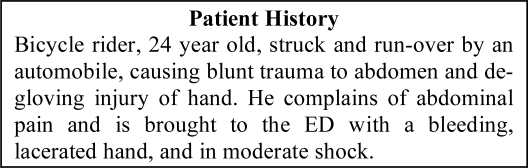
We have developed a Virtual ED (Emergency Department) with trauma patients whose medical condition evolve over time. Each patient presents with a brief medical history as reported by the ambulance team (fig. 2). The underlying medical model determines initial and evolving medical state.
Figure 2.
Initial patient report
Four important vital signs were selected for modeling the physiologic dynamics of trauma cases – blood pressure, heart rate, respiratory rate and oxygenation. Each is assumed to remain constant in a normal person. Under trauma, any or all of them may be programmed to change because of a physiologic insult. For example, if the trauma case includes possible internal injury, the corresponding loss of blood is accompanied by a steadily decreasing blood pressure and increasing heart rate. In our model, this is simulated as a linear change over time in these two variables. A different type of trauma, such as a blocked airway, may cause a more sudden change in a variable such as respiratory rate.
The medical model is “rule-based”, and differs significantly from the highly detailed mathematical models that underlie the pharmaco-physiologic medical models appropriate for anesthesia simulation2. (See code fragments in Appendix for our rule-based method.). The four vital signs represent the “observable” state of the model. Other unobservable states, such as blood volume, impact parameters such as rate of change of blood pressure, but their value and change are not computed in our basic medical model. The vital signs are not linked computationally such as through a simulation of the cardiovascular or respiratory system.
In this model, we can specify both gradual changes in physiologic variables as well as a number of discrete important “states”, with the patient moving from state to state based on the trauma and on the actions taken by the learner. The “Intervention interface” and “Query interface” include a rich repertoire of actions. Each action is initiated by clicking on a menu button. Each action is used to collect information, to change the Patient state, or both.
In the Virtual ED, the execution of each intervention is represented as an animation, with the corresponding avatar making the motions for that intervention. Some interventions change the state of the vital signs, and their corresponding display. Certain Patient State variables change if the corresponding interventions have happened. This information is stored in flags (yes/no variables).
Advantages and disadvantages of Virtual ED Patient model
A key advantage of this model is that it is easy for medical subject matter experts (physicians) to understand how to design patient cases. For any trauma victim, they can describe how the vital signs will be altered, and the other symptoms that should be displayed. The rules themselves are easily programmed in any language (we used Javascript). The limitation has been our ability to display animations of the many complex interventions. We have chosen to animate a few, and have simply implemented others as text responses to menu selections. The disadvantage is that as the number of correlated physiologic variables increases, the programming effort, and the possibility of error, increases. Therefore, at present, this method is best suited to implementation of simple physiologic situations.
Results
Twelve senior medical students and four first year EM residents trialed the Virtual ED. All reviewed basic trauma management and EMCRM team leadership skills prior to initial orientation to the simulation system. Pairs of trainees were teamed with two standardized team players—an ED physician and nurse—for a half-day training session. The four-member teams worked together over the internet, in real time with voice communication, to manage a virtual patient exhibiting signs and symptoms of a traumatic injury. Users selected the appropriate avatar actions from the menu to virtually assess and manage the cases. Guided by the Emergency Medicine Crisis Resource Management (EMCRM) curriculum, the team worked through cases, applying basic principles of trauma management and effective teamwork.
Each team managed six cases, including a pre and post assessment case, with trainees alternating the leadership role. An ED faculty member led the debriefing sessions after each training case.
The ED faculty member and standardized team members were trained on using the EMCRM objective, structured, rating scale. They observed and rated each trainee’s team performance on the pre and post assessment cases. Trainees also completed a questionnaire to provide feedback on their perceptions of the learning experience.
A pretest-posttest comparison of mean scores was computed and the difference was found to be statistically significant (Wilcoxon Signed Ranks test, Z=−3.52, p=0.00) showing that the trainees’ performance scores improved between the pretest and the posttest cases. All trainees reported feeling this type of simulation would be either “useful” (19%) or “very useful” (81%) in learning to initially assess and manage trauma patients.
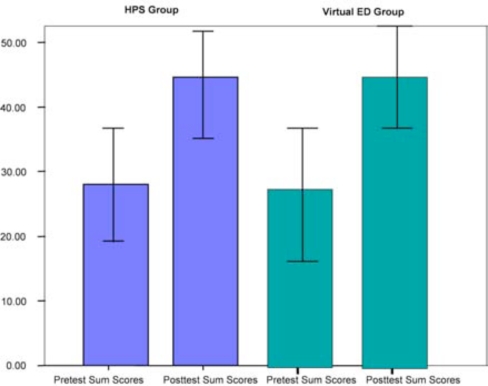
The performance of this group was compared with that of a similar group who managed the same six cases in a human manikin simulator environment. The two groups showed similar improvement, indicating the capability of the Virtual ED as a valid learning environment3 (fig. 3).
Figure 3.
Mean scores are shown for students in the Human Patient Simulator group (first two bars) and in the Virtual ED group (second two bars). Significant and comparable improvement is displayed by both groups between pre-test and post-test cases.
Conclusion
We are currently extending the patient model to support training scenarios for two types of mass casualty disaster, as they impact the hospital’s ED:
– Sarin aerosol attack – liquid dispersion of sarin gas in a subway train
– “Dirty Bomb” attack – explosion of a bomb with radiological materials in a car at the front of a building.
Our initial analysis indicates that the Virtual ED Patient model may be extendable while retaining its rule-based approach. The training scenarios will include the medical events in Table 5.
Table 5.
Medical events.
| Medical Event | Parameters |
|---|---|
| Trauma | |
| Heart Attack | Type, Location, Severity |
| Stroke | |
| Seizure | |
| Anxiety Attack | Type, Severity |
| Exposure to Toxins | Type, Concentration, Duration |
The scenarios will require additional presentation of injury or pathology, a few of which are presented in table 6. We indicate how we plan to deal with the additional computational and visualization needs. Additional diagnostic procedures are planned (table 7) with some related treatments in table 8.
Table 6.
Selected methods of presenting or triggering Medical Conditions
| Condition | Process | Description |
|---|---|---|
| Bleeding | Modify Texture | If this is dynamic, when does it start, is it steady, or does it change suddenly |
| Wounded Limb or Torso | Animation | This is a patient state variable (flag) but is not dynamic |
| Coughing | Animation | Does coughing change during the simulation. Does it respond to changes in physiologic condition. For example, death. |
| Heavy or Shallow Breathing | Animation | Does the depth of breathing correlate with the respiration rate, which is already modeled. |
| Seizures | Animation | This could be an animation that is triggered randomly. Alternatively, a new physiologic variable could be created that triggers seizures. |
| Unconsciousness | Animation | Same as above. |
Table 7.
Selected diagnostic procedures
| Examination Name | Instrument (visuals) | Output |
|---|---|---|
| Measure heart rate | Stethoscope | Heart rate variable exists. Can trigger text, graph, or audio if available. |
| Measure papillary constriction, tears | Our variable – “Examine Pupils”, generates text output.. Could use image or animation. | |
| Examine airway | Tongue blade | Our variable – “Check Airway”, generates text output. |
| Measure blood pressure | Sphygmomanometer | Variable exists. Reports text. |
| Record ECG | ECG Monitor | Heart rate variable could trigger an ECG tracing (image). Complexities in ECG may need additional variables. |
| Imaging of injured regions | X-Ray | New variable. Its values are the various possible states of the injured regions. (text) |
| Glasgow Coma Scale (GCS) | New variable. Is this expected to change during the course of the simulation? Its values could be the various possible consciousness states. (text) |
Table 8.
Selected treatment procedure
| Treatment | Instruments (need visuals) | Response of model |
|---|---|---|
| Tongue Blade, Oral Airway | Place appliance, latex gloves | Change value of airway state |
| Tourniquet | Latex rubber strip, latex gloves | Change flag to say tourniquet is applied |
| Bandages | Bandages, tape, towels, latex gloves | May impact blood loss. Other effect? |
| Fluid Therapy | IV bag and tubing, needles, latex gloves | Impact blood volume |
| Administer Oxygen (O2) | Face mask, tube, canister | Impact oxygenation |
| Insert Chest Tube | Skin prep.,chest-tube, bandages, latex gloves | Variable for pneumothorax. Exists in SUMMIT model |
| Administer Medications | Prep., needle/syringe, IV ; e.g., 2-PAM (Pralidoxime), atropine, 50% dextrose, morphine, analgesics, latex gloves | Impacts vital signs. May need additional variables. |
| Transfuse Blood | Prep., needle/syringe, IV ; blood pack cells, latex gloves | Impacts blood volume. |
Table 1.
“Patient state” variables in the Virtual ED Patient model
| State variable (vital signs) | Dynamics of state variable |
|---|---|
| Heart Rate | Constant, changing linearly because of specified trauma condition, or changing discretely because of intervention |
| Respiratory Rate | same |
| Blood Pressure | same |
| pO2 | same |
Table 2.
“Interventions” available in the Virtual ED Patient model
| Intervention (and Query) | Outcome |
|---|---|
| Trendelenberg | tilts the gurney by swapping models (change BP) |
| Flatten Gurney | flatten the gurney by swapping models (change BP) |
| Clear Airway | reports back findings (clear if blocked) |
| Administer Glucose | reports back findings (change vitals) |
| Give Blood | prompts for more information (change vitals) |
| Administer O2 | reports results (change vitals) |
| Chest Needle | reports results (change vitals) |
| Insert IV | prompts for more info (change vitals) |
| Hyperventilate | reports results (change vitals) |
| Endotracheal tube | reports results (change vitals) |
| Chest tube | reports results (change vitals) |
Table 3.
“Queries” available in the Virtual ED Patient model. “Reports back findings” gives a text message.
| Query only | Outcome |
|---|---|
| Get Patient Report | presents report to all users |
| Check Femoral Pulse | reports back current pulse |
| Check Radial Pulse | reports back current pulse |
| Check Pedal Pulse | reports back current pulse |
| Check Precordial Pulse | reports back current pulse |
| Palpate Head and Neck | reports back findings |
| Palpate Upper Extremities | reports back findings |
| Palpate Thorax | reports back findings |
| Palpate Lower Extremities | reports back findings |
| Palpate Back | reports back findings |
| Send for X Rays | prompts for more information |
| Rectal Exam | reports back findings |
| Examine Pupils | reports back findings |
| Attach Pulse Oximeter | displays pO2 in vital signs panel |
| Attach Chest Leads | displays HR, RR in vital signs panel |
| Check Airway | reports back findings |
| Auscultate Chest | |
| Take Blood Pressure | displays BP in vital signs panel |
| Auscultate Abdomen | reports back findings |
| Palpate Abdomen | |
| Ultrasound |
Table 4.
“Patient state” flags in the Virtual ED Patient model
| Patient state flags | Flag state |
|---|---|
| caseNumber | store the case number |
| sessionStart | flag to indicate whether task has been done |
| insertIV | flag to indicate whether task has been done |
| takeBP | flag to indicate whether task has been done |
| chestNeedleDone | flag to indicate whether task has been done |
| IVhand (R/L) | flag indicating whether item is present |
| IVcubital (R/L) | flag indicating whether item is present |
| IVjugular (R/L) | flag indicating whether item is present |
| chestTubeFlag | flag indicating whether item is present |
| airwayFlag | flag indicating whether item is present |
| endoFlag | flag indicating whether item is present |
Acknowledgments
This research was funded in part by the Wallenberg Foundation, TATRC and Adobe Systems.
Appendix. Sample Code
//This part continually loops to update the vital signs
loadAll = new Object();
loadAll.timestep = function(now)
{
curHR =
baseHR+incrHR+Math.round(HRRate*(now-startT))+Math.round(3*Math.random());
if (curHR < 115) curHR = 115;
if (curHR > 145) curHR = 145;……..
curBPs =
baseBPs+incrBPs+Math.round(BPsRate*(now-startT))+Math.round(2*Math.random());
curBPd =
baseBPd+incrBPd+Math.round(BPdRate*(now-startT))+Math.round(2*Math.random());
if (curBPs < 50) curBPs = 50;
if (curBPs > 85) curBPs = 85;
if (curBPd < 30) curBPd = 30;
if (curBPd > 55) curBPd = 55;
}
//This shows the message presented when pushing the 'Palpate Head' button
PalpateHeadB.onClick = function()
{
if (atRightArm(player.position) ||
atLeftArm(player.position) || atHead(player.position)) {
sendJS(“alert(\”There is a wound on the forehead.\“);”);
}
else {
sendJS(“alert(\”You are not in the correct location to palpate the head and neck region.\“);”);
}
}
References
- 1.Lyon HC, Jr, Healy JC, Bell JR, O'Donnell JF, Shultz EK, Moore-West M, Wigton RS, Hirai F, Beck JR. PlanAlyzer, an interactive computer-assisted program to teach clinical problem solving in diagnosing anemia and coronary artery disease. Acad Med. 1992;67:821–8. doi: 10.1097/00001888-199212000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Garfield JM, Paskin S, Philip JH. An evaluation of the effectiveness of a computer simulation of anaesthetic uptake and distribution as a teaching tool. Medical Education. 1989;23:457–462. doi: 10.1111/j.1365-2923.1989.tb00902.x. [DOI] [PubMed] [Google Scholar]
- 3.Youngblood P, Srivastava S, Harter P, Dev P, Wallen C-J, Tsai L, Heinrichs WL. Validation of a web-based VR simulation for training trauma teams. MMVR’. 2005;2005 [Google Scholar]