Abstract
The Veterans Health Administration (VHA), of the U.S. Department of Veteran Affairs has instituted a medical record (EMR) that includes electronic documentation of all narrative components of the medical record. To support clinicians using the system, multiple efforts have been instituted to ease the creation of narrative reports. Although electronic documentation is easier to read and improves access to information, it also may create new and additional hazards for users. This study is the first step in a series of studies to evaluate the issues surrounding the creation and use of electronic documentation. Eighty-eight providers across multiple clinical roles were interviewed in 10 primary care sites in the VA system. Interviews were tape-recorded, transcribed and qualitatively analyzed for themes. In addition, specific questions were asked about perceived harm due to electronic documentation practices. Five themes relating to difficulties with electronic documentation were identified: 1) information overload; 2) hidden information; 3) lack of trust; 4) communication; 5) decision-making. Three providers reported that they knew of an incident where current documentation practices had caused patient harm and over 75% of respondents reported significant mis-trust of the system.
INTRODUCTION
Patient safety concerns have been on center stage for the Veterans Health Administration since before the widely acclaimed Institute of Medicine Report, To Err is Human, was released in 1999.[1] One component of VHA’s effort to improve patient safety has been the implementation of a fully electronic medical record with Provider Order Entry that includes full support for comprehensive electronic documentation. Implementation of computerized patient care documentation (CPD) has required significant changes on the part of users. Despite the difficulty, the VA has been successful and most VA hospitals and clinics utilize only electronic charts. As of October 1, 2005, over 750 million patient care documents were stored in VA computer systems and included all classes of text documents commonly found in medical record. Only about 1% of these documents were dictated, indicating a pervasive use of manual input. The purpose of this paper is to report on a pilot study conducted across multiple VA sites and provider roles to identify current concerns, prevalent practices, and user perceptions regarding electronic outpatient documentation
BACKGROUND
The VA has mandated electronic documentation and has supported it with substantial time saving and flexible input methodologies. Providers can dictate, type, copy and paste, insert clinical objects and build personal templates. In the newer versions, they are able to complete reminders, generate orders and pull in structured data entry. Objects that can be automatically inserted included lab values, age, name, medication list, problem list, and any pre-created templated text. Many VA sites have created domain specific object banks that include sophisticated text organized around their specialty, such as Coumadin Clinic progress notes that automatically insert normal History and Physical (H&P) text, the most recent International normalized ratio or blood clotting (INR) and other coagulation laboratory values, vital signs and medication lists. The provider simply changes the incorrect text, inserts abnormal findings for normal findings, and updates medication lists to reflect new changes. The result is that a user can produce a very complicated note and sign off on it in minutes. The major limitation of the VA documentation system has been the difficulty of creating images and graphics, which in some fields, such as ophthalmology, surgery and dermatology are crucial to how notes are constructed.
The narrative component of the medical record has several uses. Narrative is used to convey the line of thought, perspectives and plans of the individual user. As such, it is the main source of communication regarding the overall plan of care between providers. To that end, users have normative expectations regarding how and why information is presented, such as they expect relevant information to be displayed and non-relevant information to be omitted.[2] In addition, narrative notes are a major source of clinical information.[3] Secondly, narrative text is used by coders and billing to create a bill. Coders are trained to extract relevant information regarding procedures, diagnoses and plans of care from structured narrative text. Finally, narrative text is the main source of information for legal and quality review purposes.
Electronic notes facilitate clinical communication in some ways. They are much more legible than handwritten text. They also tend to be more comprehensive and longer then their corresponding paper notes, largely because of the easy ability to copy and paste, insert large amounts of lab values, medication and problem lists. They are also, of course, much easier to read in some ways than handwritten text. [4, 5]
However, three recent studies in the VA have identified several pressing concerns. First, Weir, et al (2003)[5] identified and classified “invisible” documentation errors in an analysis of 60 randomly selected medical ward admissions at an urban academic center. Among 1,891 progress notes manually reviewed, several types of errors were found. Copying errors included clashing information: e.g., a note stating “the lungs were clear” in one place and “significant rales” in another; and improper time representation: e.g. a copied statement appearing on four consecutive days that read: “…ataxia yesterday…MRI done this afternoon.” Other errors included blending older and newer patient data in vital signs blocks, and outdated provider role information with the electronic signature. The percentage of all notes with at least one error was 84% and the average number of significant errors per patient was 7.8. Manual review disclosed copying in 19.8% of notes, generating about one documentation error per copying episode. Computerized patient documentation might violate four normative expectations of documentation: (1) succinctness and precision; (2) correct portrayal of the decision process; (3) temporal accuracy; and (4) consistent format.[2, 5]
In a second study by Hammond, et al, a random sample of 167,000 inpatient and outpatient documents were selected from 1, 479 different patients. Using a plagiarism-detection software, 12.5% of notes were found to have substantial copied material and the mean interval between copy and original was 128 days.[6]
In a third study, Embi et al performed a qualitative analysis of the impact of CPD with 10 physicians and identified four key themes: 1) improvement in availability and legibility; 2) changes in work processes and communication; 3) changes the content of documentation; and 4) less trust or confidence in the accuracy of narrative text.[7]
Other authors have noted that information overload and interference with work processes are problems for users in a fully electronic environment, many of which include electronic documentation.[8–10]
The purpose of this paper is to report on a pilot conducted across multiple VA sites and provider roles to identify current concerns, prevalent practices, and user perceptions regarding CPD in the VA outpatient setting. This study expands on others by crossing multiple sites and focusing at the clinic level to identify work processes in relation to CPD.
METHODS
General Design
Qualitative methods were used to identify overarching themes and patterns. This study was part of a larger study evaluating a specific VA software package.
Sites
An initial group of 44 sites (out of the VA’s 177 total sites) were selected for the purpose of another study. Purposive sampling was used to select eleven sites from the initial study group. Sites were selected in order to maximize differences based on the basis of geography, size, academic affiliation and urban/rural representation.
Respondents
One primary care clinic was randomly selected from within each institution. The total number of primary clinics (including Community-Based-Outpatient Clinics) within each institution ranged from 3 to 16 across the 10 sites participating in this study. All members of each chosen clinic were invited to participate in the interviews. A total of 88 interviews were conducted and included 14 nurses, 53 ordering providers, 3 clerks, and 8 pharmacists. Nobody who was approached refused. However, occasionally individuals were not available on the day of the interview or at the specific time and were not interviewed.
Procedures
Interviews were conducted on-site and included observation, open-ended discussion and answers to specific questions. If possible, practitioners were observed in interaction with patients and each other, given patient consent. If alone and using the computer, they were asked to “think aloud.” All interviews were tape-recorded and transcribed.
Interview Questions
A semi-structured interview focused on how, when, what, and where information was collected in primary care. The investigators extensively piloted the survey and standardized the process. The interview included general queries regarding information management activities and had an overall chronological structure starting with questions regarding how they would begin the day, prepare for a visit, follow-up activities that were required, and clinic-related. The following specific questions were asked at the end: 1) How accurate, complete, or comprehensive is CPRS documentation?; 2) What do you think is the biggest threat to accuracy in terms of CPRS documentation? 3) Do you engage in copy and paste activities? 4) Have you personally seen any harm related to documentation practices? Interviewers asked participants to elaborate on yes or no responses.
Data Analysis
Qualitative data analysis procedures were used to bring order, structure to the text and to identify themes. Analytic procedures began with multiple readings of the interviews, development of coding schemes to facilitate abstraction, and an iterative process of validating the codes by comparing independent reviewers, discussion, and revision. Coding was expanded through processes of aggregation across levels of abstraction and by analysis across persons and events. Investigators met weekly for several months. Coding strategies were developed and tested through comparison of independent reviews, conducted iteratively until categories for documentation themes reached an acceptable level of agreement across categories (kappa = 0.82). [11]
RESULTS
Themes
The following themes were identified and are listed in Table 1 along with corresponding strategies that some respondents identified.
Table 1.
Themes from interviews
| THEMES | STRATEGIES |
|---|---|
| Information Overload | |
| Too many notes | Read a few notes; avoid notes from certain roles |
| Notes too long | Read only conclusions or plans |
| Information w/in notes hard to find. | Scan or skip sections; read only notes from known individuals. |
| Hidden Information | |
| Nurses paper notes | Get verbal report |
| Logs and lists | Learn what lists are kept and where |
| Lack of Trust | |
| Problem list | Type in your own problem list and copy it each time |
| Medication List | Type in your own medication list and copy it each time. |
| Communication | |
| Giving a “hand-off’ to other providers. | Have other provider be a mandated signer. |
| Create a team plan | One note with multiple addendums |
| Decision-Making | |
| Tracking/trending | Keep paper lists |
| Understanding plan | Call provider |
| Patient’s response | Review everything or ask patient. |
Information Overload
All respondents commented on the difficulty of sorting, sifting and locating relevant documents. Because notes are stored by title and arranged chronologically, a provider might have to sort through 30 physical therapy notes to get to the last primary care visit. In addition, notes could be as long as 5 pages (or even more with templates) and substantial time was required to scan through a note to find relevant information. Pharmacists particularly complained of the extensive amount of time required to determine why a patient was on a specific medication. Nursing notes often had extensive templating with up to 90% of the notes having empty or default values. The strategies used to overcome this problem were many, but largely were based on avoiding difficult or non-relevant material So, many physicians reported avoiding social worker and nursing notes in order to save time, assuming that if there was a problem, the allied health professional would call.
Hidden Information
An unexpected complaint from providers was the amount of “hidden information” they encountered. Prior to the electronic chart, all information about the patient was kept in the paper binder. However, since everyone was relying on the electronic chart, important paper documentation was removed from the mainstream process of accessing and sharing information. Some providers assumed that if information wasn’t in the computer, it did not exist. Outside results for procedures, notes from family and other items would often get mislaid. Often, nurses would write notes on the vital sign sheet relating to the patient’s complaint that would not get on a regular electronic progress note. Occasionally, paper with important information would be discarded.
Lack of Trust
Because of the copy and paste, object insertion and automatic text with templates functionalities, many providers had become skeptics about the veracity of the chart. Copied text would not properly reflect changes in patient status. Problem lists would be brought into the note as a whole object, but if they had not been updated (which was often the case), they were not accurate. Some providers were very diligent about editing them, but others were not. Medication lists were noted as the most severe and dangerous of problems. The medication list was taken from the pharmacy fill list, and often did not accurately represent what the patient was intended to be taking. Prescriptions could have officially expired, but the patient would still be taking them. Or, the order may have been cut in half, as a result of a telephone call to the provider, but the dose change not entered in the pharmacy package. And, non-VA filled meds would not be on the list. (This functionality is now being added) Finally, copying would make it hard to determine new versus old material.
The normative expectation that a list of items in the progress notes were reviewed and validated by the signer of that note was, therefore, often not met. The reader would use other cues to determine validity, such as personal knowledge of the documentation practices of individuals or classes of providers. For instance, at some sites, users believed that clinical objects inserted by students were more likely to be verified and updated than when entered by residents.
Communication
Notes were often used to enhance communication. Orders might be actually written in the note and not in the order sections. One provider could “hand-off” a patient by requiring that the new provider be a signer on the note and therefore would get an alert, notifying him of the patient’s needs. Some providers wondered about the legality of this underground consulting system and did not use it. Student oversight would be accomplished by writing an addendum to the student’s note. Team plans could be created by writing a series of addendums, since only one person could be author of an electronic note.
Decision-Making
Most providers reported on the difficult of extracting meaningful data from large number of notes and confusing text. Since many clinical conditions require tracking or trending, individual providers had to resort to paper lists that they would keep in their drawers. In addition, because the objects being pulled into the notes were simply pasted in either chronological or alphabetical order without regard to their relevance to the problem at hand, readers had difficulty discerning the full thoughts and intent of other providers.
Analysis of Responses
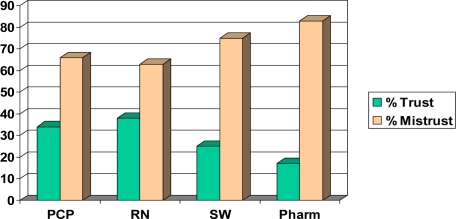
Over two-thirds of the respondents reported significant mistrust in the system. Figure 1 illustrates the differences between roles. In response to the question regarding danger, about a third stated that copy and paste was the most dangerous, but that also differed by role, with pharmacists being more likely to report harm. Next to copy and paste, information overload was listed as the second most dangerous aspect of electronic records. Only three individuals reported seeing actual harm to a patient as a result of the change in documentation practices.
Figure 1.
Ratings of trust/mistrust by primary care providers (PCP), nurses (RN), social workers (SW) and pharmacists (Pharm).
DISCUSSION
Although most researchers and clinicians agree on the ease of access and increased legibility of electronic notes, unexpected difficulties regarding the use of electronic notes are becoming more apparent. In addition, the extensive software support given to providers to enhance rapid and accurate note creation may have unexpected consequences.
Some of these effects might be a result of the known changes of a CPOE system on work processes.[8] Other effects may be a result of changes in how information is displayed. Format, layout and textual features have been shown by Nygren and Henriksson to be critical to the speed and accuracy of text understanding in a medical record.[12]
There are several lessons to be learned from this pilot study. System designers must explicitly consider how coded data is to be used in narrative notes. Like many electronic health records, the VHA’s Computerized Patient Record System uses separate systems for problems, orders, medications and laboratory results. Data is pasted into the notes in the same form that it is stored, regardless of the context of the note. In hand-written notes, providers filter and organize pieces of information that is most relevant to the patient’s care at the time. Automatic insertion of coded clinical data from other systems chunks data together that is often not congruent with the author’s intent. In addition, the insertion of large amounts of data automatically into narratives circumvents some of the cognitive processing that providers would otherwise undertake when constructing a note. Automatically inserted data is left in raw format for several reasons including time costs to edit and verify the information. The inserting provider may not even read it. The task of the system designer is to ensure that insertable coded data is both part of workflow as well as supportive of cognitive processing.
In addition, although all clinicians use copy and past tools, they also complain that it is a dangerous practice. By using software tools that highlights the presence of copy and pasted text, authors may choose to be more careful.
Finally, the use of templates should be minimized as much as possible as they use up a lot of space for very little true information. If more sophisticated tools for creating and inserting more fine-grained coded objects were available, notes could still be created rapidly but be more like normal writing.
This study may lack generalizability as it was a study of only one system and limited to primary care clinics. Future work should focus on other clinical areas and work processes as well as identifying possible patient harm.
Acknowledgments
This study was supported by VA HSR&D # MRC 03-237, TRP 02-147-2 and RCD 02-176-2. Appreciation to Bret Hicken, PhD, Hank Rappaport, MD, Rebecca Campo, MS and Beth LeBar, MSN.
REFERENCES
- 1.Institute of Medicine, To Err is Human. Washington DC: National Academy Press; 2000. [Google Scholar]
- 2.Grice H. In: Logic and Conversation. Syntax and Semantics 3: Speech Acts. Cole P, Morgan JL, editors. Academic Press; New York: pp. 41–58. [Google Scholar]
- 3.Tange HJ, et al. The granularity of medical narratives and its effect on the speed and completeness of information retrieval. J Am Med Inform Assoc. 1998;5(6):571–82. doi: 10.1136/jamia.1998.0050571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang PC, LaRosa MP, Gorden SM. Use of computer-based records, completeness of documentation, and appropriateness of documented clinical decisions. J Am Med Inform Assoc. 1999;6(3):245–51. doi: 10.1136/jamia.1999.0060245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weir CR, et al. Direct text entry in electronic progress notes. An evaluation of input errors. Methods Inf Med. 2003;42(1):61–7. [PubMed] [Google Scholar]
- 6.Hammond K, et al. Are electronic medical records trustworthy? Observations on copying, pasting and duplication. Proceedings, AMIA Symposium; 2003. pp. 269–273. [PMC free article] [PubMed] [Google Scholar]
- 7.Embi PJ, et al. Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians. J Am Med Inform Assoc. 2004;11(4):300–9. doi: 10.1197/jamia.M1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc. 2004;11(2):104–12. doi: 10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ash JS, et al. Perceptions of physician order entry: results of a cross-site qualitative study. Methods Inf Med. 2003;42(4):313–23. [PubMed] [Google Scholar]
- 10.Berg M, et al. Considerations for socio-technical design: experiences with an electronic patient record in a clinical context. Int J Med Inform. 1998;52:1–3. 243–51. doi: 10.1016/s1386-5056(98)00143-9. [DOI] [PubMed] [Google Scholar]
- 11.Patton M. Qualitative Research & Evaluation Methods. 3. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 12.Nygren E, Henriksson P. Reading the medical record. I. Analysis of physicians' ways of reading the medical record. Comput Methods Programs Biomed. 1992;39:1–2. 1–12. doi: 10.1016/0169-2607(92)90053-a. [DOI] [PubMed] [Google Scholar]