Abstract
Since 2005 we have been developing and implementing an electronic medical record (EMR) that supports both individual and population health care of HIV-infected patients in Haiti. Unreliable electrical power and network infrastructure, cultural differences, variable levels of experience and computer literacy, and the geographic dispersion of the team remain challenges, but the system is now implemented in about 40 sites nationwide providing antiretroviral therapy, and includes records for about 18,600 patients. The need to support countrywide monitoring and evaluation drove early architectural decisions to support linking systems under conditions of network uncertainty. We have found surprising end user acceptance of the system, with the adoption of interactive EMR usage exceeding our expectations and timeline.
Introduction
Haiti is the poorest country (per capita GDP) in the Western Hemisphere, with 80% of the population living in poverty. Following both political and economic instability the communications infrastructure is among the weakest in the western hemisphere, but approximately 7.5% of the population have used the Internet, a level of usage which is similar to that in Kenya, which has a similar GDP, and high compared to other similar African and Asian economies.1
Haiti accounts for the largest HIV burden in the Caribbean, despite a recent stabilization of prevalence rates.2 Between 2.2% and 3.8% of Haiti's population is living with HIV–one of the highest percentages outside of Africa–and AIDS remains the leading cause of death among adults age 15–443. Antiretroviral therapy (ART) throughout the Caribbean reaches just one in four (23%) of those who need it. Haiti and the Dominican Republic together account for nearly 75% of the 230,000 people living with HIV in the region.2 Lack of access to ART by infected persons has led to a high rate of vertical transmission of HIV (27–37%), and therefore to a large population of pediatric HIV patients4.
As Haiti scales up efforts to treat this personally and economically devastating disease, it needs a system both to support the care and treatment of these patients, and to conduct population-based monitoring and evaluation (M&E) of publically funded and nationally driven interventions. These M&E needs are defined by the Haitian Ministère de la Santé Publique et de la Population (MSPP) and shaped both by the formal reporting requirements of donor nation programs such as the US-sponsored President's Emergency Plan for AIDS Relief (PEPFAR), as well as those of international organizations such as the World Health Organization to (WHO) and UNAIDS. In addition, the system needs to serve other population health needs, providing quality information to improve care locally and nationally, supporting evidence-based treatment guidelines in Haiti, and creating opportunities to gather population-level research data to better understand the epidemic.
For the past three years, we have endeavored to address both clinical and M&E needs through the development and implementation of a networked electronic medical record (EMR) to support the care of both individuals and populations.
Similar Efforts around the World
The 15 PEPFAR “focus countries”, which include Haiti, are home to about ½ of the world’s 33 million HIV positive individuals.5 Similar efforts to apply both informatics and information and communication technologies (ICT) are underway in a number of those countries as efforts to provide and monitor treatment are rapidly increased. At a recent strategic information conference in Zambia, system developers of OpenMRS, Baobab, SmartCare, CAREWare, Taiwan Medical Board, and other systems presented their work. Though all systems addressed reporting, some emphasized clinical care and others M&E.
Project Origins and Partners
In early 2005, at the request of MSPP and the Centers for Disease Control and Prevention (CDC), the Clinical Informatics Research Group (CIRG) at the University of Washington began working with International Training and Education Center on HIV (I-TECH) to develop an EMR for Haiti. I-TECH was established in 2002 by the Health Resources and Services Administration in collaboration with CDC, with the mission of supporting ongoing development of locally-determined, self-sustaining training in countries hardest hit by the AIDS epidemic.
Methods
The design, development, and implementation of the project are driven by considerations including:
(a) dual use of the system for both clinical care and M&E, for both adult and pediatric patients;
(b) uneven infrastructure in Haiti, requiring both a computerized system for efficiency and an integral paper-based system for fault tolerance;
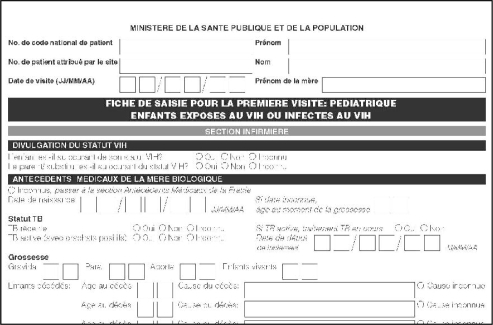
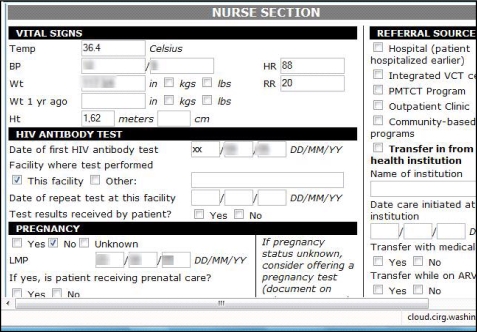
(c) full internationalization support, initially for French and English (figure1);
(d) reliance on highly structured information to support population level aggregation (figure 1);
(e) existing clinical workflow including the specific culture of record-keeping;
(f) local clinical site ICT capacity including limits to electrical power, paper, toner, and Internet access;
(g) the importance of providing information to directly support clinical care, quality improvement, and national M&E reporting;
(h) the potential to develop a national observational research cohort;
(i) a phased implementation from paper-based data capture to computerized forms entry/reporting to an interactive EMR, supporting incremental changes in workflow and processes;
(j) incremental validation against, and replacement of, existing population reporting processes;
(k) local, multi-agency, support for implementation and eventually further development of the system;
(l) and, implementation in a pure Web architecture.
Figure 1.
Portion of a French language version of the Pediatric Intake form, showing typical formatting and highly structured data elements.
It is commonly held that participatory design is essential to the successful adoption of an IT intervention. However, the requirements of this project were initially driven by prior work and programmatic needs. The structured data collection, the data model design, and support for site level quality metrics were based on a university HIV research and reporting system.6 The initial interaction design and national reporting requirements were driven by the MSPP and the strategic information office of the CDC in Haiti. Information used for design iterations currently comes from the site data quality staff, the CDC site support staff, and the field staff and management of the I-TECH Haiti office, rather than directly from end users or usability testing, though despite this the system’s success has validated our design criteria.
Functional Architecture
We began with a hybrid paper-electronic workflow similar to that now used by OpenMRS in Kenya and Rwanda.7 The initial form set was developed by a coauthor (MK), and went through revision in 2006 by a 16 person stakeholder group. The forms reflect the clinical workflow, with discrete sections for registration, initial and follow-up clinical visits, laboratory testing, pharmacy, counseling, and discontinuation. The difference between adult and pediatric care is reflected by the use of separate form sets. Though just-in-time printing of forms with patient-specific data would have afforded considerable workflow benefit, unreliable print supplies made it infeasible. The emphasis on networked transfers of data, despite intermittent communication paths, was driven by needs for both national reporting and fault tolerance. Sites back up data locally, but issues of hardware failure, climate, and difficult ground transportation require extra reliability measures to protect clinical data.
Implementation Architecture & Platforms
We chose to use open source tools as much as possible, tempered by our awareness that Haitian IT expertise lay more with commercial products. Initially implemented on Linux using the Apache Web Server, MySQL, and the PHP scripting language (LAMP), the system was ported to Microsoft Internet Information Server and Microsoft SQL Server (WISP). We will continue WISP support, but are moving back to LAMP because of the advantages of open source. Our replication architecture is generic and works independent of the LAMP/WISP implementation; each source site generates periodic (hourly, daily, weekly) transaction files that can be transmitted over the internet or via “sneaker-net” as desired. The reporting subsystem uses PHP for simple graphs and tables, and JasperReports, running under Tomcat. This works well in both Windows and Linux environments, and allows reports a variety of document formats (e.g. PDF, HTML, Excel, etc.). Initially avoiding JavaScript because of concerns of stability and portability, our newest release uses the Ext JavaScript library extensively, allowing for a richer, more interactive, client-side user experience.
Data model
The system uses a hybrid relational model, employing a combination of fully normalized tables to gain maximum flexibility for the capture of laboratory, diagnosis, and treatment observations while also employing denormalized tables for ease of reporting, simplicity in the development and implementation of interactive forms, and optimal performance during data entry and retrieval. The data model also supports the computation of summary data via special data warehouse tables that are kept up to date throughout the working day via an asynchronous process. These tables provide for improved interactive performance as well as for more sophisticated data analysis. As the system software has evolved, the database schema has evolved as well, with changes to the schema coming with each new release of the software. Each release checks the current database schema version and upgrades it automatically. The standardized nature of SQL and relational databases has allowed us to migrate the database schema from MySql to MS SQL Server and back to MySql with relatively little extra effort.
Results
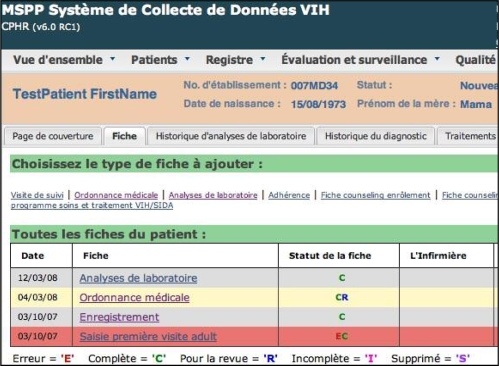
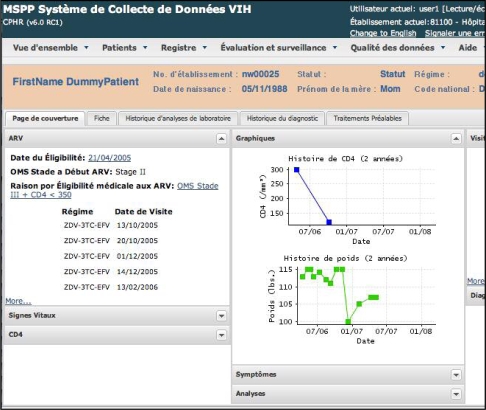
The system initially consisted of a form entry interface, and a reporting subsystem, though we have added components intended for interactive use. The form entry interface consists of a history of forms entered, links to new forms, and form displays that mimic the respective paper forms. Figures 2–4 show some layouts and features from the current release.
Figure 2.
List of forms for a patient, including Adult Intake, Registration, Followup, and Laboratory. Forms marked in red contain unresolved errors, and forms marked in yellow have been marked by the user as “in need of review”.
Figure 4.
The comprehensive patient record view includes a patient coversheet, labs, diagnoses, and treatment history
Reports have been expanded and separated to focus on both data quality and evaluation and surveillance. The latest release includes electronic registries and a consolidated view of clinic patients by status. This consolidated view has proven useful to monitor site-specific activity and software upgrade status.
System Adoption
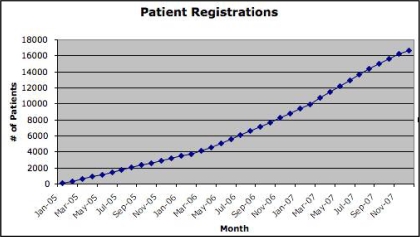
The paper forms were first used by pilot clinical facilities in January 2005 (Figure 5). The first use of the computerized system to enter clinical data was in April 2005 by a single hospital in Port au Prince. They used the system through a satellite link to a server located in a secure facility at the University of Washington.
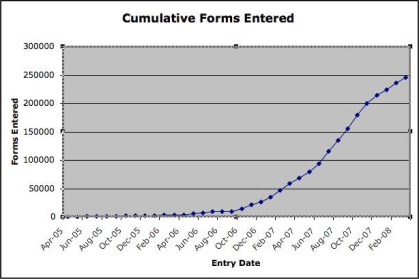
Figure 5.
Cumulative electronic or paper Initial Visit forms (18,600 patients).
A handful of clinics began using the system in this application service provider (ASP) mode at the beginning of 2006. By the end of 2006 the system had gone through three significant enhancement releases and was used by 16 different clinics, all in ASP mode. Aspects of the increase in system use from inception to March 2009 are depicted by the growth in registered patients whose care was documented using paper or electronic forms at their first visit (figure 5), and the total forms (initial, follow-up, lab, etc.) entered into the EMR (figure 6).
Figure 6.
Cumulative total electronic forms, reflecting increasing use of the computerized system.
The first local server was installed in April of 2007, with 6 sites installed by June. By the end of 2007, the system had gone through three additional enhancement releases in the areas of reporting, pediatric patient support, and replication and was used by 28 clinics, of which 11 were running their own local servers. Usage of the system continues to expand. An additional 12 clinics are using the paper system, as a transition to implementing the EMR. The project goal is 86 sites by September 2008 – a challenging undertaking in a country where people struggle with daily power outages, threats to personal safety, and minimal ICT infrastructure and support.
Discussion
Implementation:
We have described many factors which contribute to the challenge of implementing a national, networked EMR in Haiti, not least of which is the scarcity of clinical resources. Staff, time, and money are in short supply, with no evident limit on the need for services. As is typical for an EMR implementation, significant investment is required before users receive tangible benefits from the system. Some sites still face a large backlog of unentered patient records, which lowers the utility for both clinical practice and M&E, so we developed a “registry” model, which allows a subset of patient treatment information to be entered, sufficient for reporting and clinical summary.
Incentives for use:
Making the system useful for clinical care, automated reporting, and local site quality improvement, is a practical way to ensure good data quality – retrospective auditing and correction are very expensive. At one site, manual reporting takes 2 weeks of each month. But, until data are complete and accurate, the benefit of automated reporting cannot be realized, even if the system has clinical utility for a subset of patients. Yet, the funding for these systems is typically driven by reporting. We had to address reporting needs initially, but increasingly turn our attention to enhancing local utility to improve care.
Unintended benefits:
Within the past year, sites that have resolved their backlog, and have sufficient computers, began to directly enter forms into the EMR during patient visits. This concerned us as there is no longer a paper backup for those visits. Recently, we learned that some physicians devised a workflow using prescription forms as computerized physician order entry (CPOE), entering prescription data, flagging the form “for review”, and sending the patient to the dispensary where the pharmacist charts the medicines given on the form, and clears the form status. This creativity shows a desire to exceed the current system capabilities, and reminded us that our preconceptions of the limitations in developing countries must constantly be questioned.
Open source:
Low licensing cost is important for sustainability, as is local technical expertise. We tried both open source and mixed platforms to accommodate these criteria. However, we feel that simplified installation and configuration are also critical for sustainability, and best supported by open source. While we have not yet created a development community around the EMR, open source approaches may better support that goal.
Phased Implementation:
Our experience strongly supports implementation in conjunction with a paper-based system, with paper as both an initial way of introducing uniform workflows, and as a fault-tolerant strategy to deliver clinical care in the face of computers that are broken, missing, or lack power..
Data Model:
Our data model has evolved as the system has been enhanced; addition of linkage between intake/followup visits and labs/prescriptions, tracking of next visit information, and addition of pediatric patients are just three feature areas that required database schema changes. Changes to the data model have in turn required us to develop more sophisticated tools for manipulating the schema, for generating reports, and for facilitating data entry. The greater system complexity creates challenges in changing the schema, but permits performance optimization. Compared to large scale banking or finance applications, these databases are relatively small--often full table scans yield acceptable performance. Our use of asynchronously generated summary warehouse tables supports generally good performance for interactive use and for reporting. Sites still using our ASP server in Seattle often face poor internet performance; the rapid adoption of in-country local clinic servers is due in large part to unhappiness with network response times.
Conclusion
Perhaps the most important conclusions of our work thus far are that success with M&E on a national scale is best driven by creating value at the local level, and that we must closely examine our preconceptions of what health care providers want and need in resource poor settings. There is a strong desire in Haiti to have efficient, comprehensive clinical information systems, and a strong desire to deploy them to support general health care delivery.
Despite major technical challenges, the EMR system has been met with such enthusiasm that final year medical students are presently being trained on how to use EMR in their medical practices.
Though our development and deployment of a national, networked EMR in this challenging setting, we hope we will continue to make contributions to both the care and treatment of people living with HIV in Haiti, and to a general understanding of how to implement complex, linked information systems in resource constrained settings that support both individual and population health.
Project Contacts
Bill Lober, MD, MS, I-TECH EMR Project Informatics Lead, Associate Professor, University of Washington Center for Public Health Informatics, lober@u.washington.edu
Mari Kitahata, MD, MPH, I-TECH EMR Project Clinical Lead, Director of HIV Outcomes and Health Services Research, University of Washington Center for AIDS Research, kitahata@u.washington.edu
Patrice Joseph, MD, MPH, CDC Global AIDS Program, Haiti, Strategic Information Technical Lead, josephp@ht.cdc.gov
Figure 3.
Vitals, HIV test, and Pregnancy screens of current system all closely emulate the paper clinical forms.
Acknowledgments
We would like to acknowledge funding from HRSA, (Cooperative Agreement No. 6 U91HA06801-01-01, CFDA No. 93.145), as well as the support of the CDC GAP staff in both Atlanta and Port au Prince.
In addition, we are grateful to a number of students and staff who have worked on this project: (currently: Jun Shao, Claire Tucker, and Piu Mitra) and to our colleagues in the I-TECH Haiti office, Rachel Coq, Rikérdy Frederic, Rachelle Cassagnol, Rogès Lamothe, Don Rock Pierre Alexis and others.
Along with the Haiti Ministry of Health and Population (MSPP), the US Centers for Disease Control & Prevention (CDC), and I-TECH, other collaborating agencies include: Institut Haitien d'Enfance (IHE), National Alliance of State & Territorial AIDS Directors (NASTAD), Tulane University, and the World Health Organization/ Pan American Health Organization (WHO/PAHO).
Footnotes
Note: Two paragraphs of the introductory section previously appeared in the I-TECH newsletter8.
References
- 1.Central Intelligence Agency, The World Factbook (https://www.cia.gov/library/publications/the-world-factbook/geos/ha.html#Econ, accessed 2008-03-12)
- 2.UNAIDS 2007 epi update
- 3.UNAIDS 2006 reference – consider 2007 epi update instead http://www.unaids.org/en/KnowledgeCentre/HIVData/EpiUpdate/EpiUpdArchive/2007/default.asp
- 4.George Erik, Noël Francine, Bois Gyrlande, et al. Antiretroviral Therapy for HIV_1–Infected Children in Haiti The Journal of Infectious Diseases 2007. 195101411–1418. [DOI] [PubMed] [Google Scholar]
- 5.http://www.pepfar.gov/countries/c19418.htm (accessed 2008-03-12)
- 6.Kitahata MM, et al. Electronic HIV clinical reminder system improves adherence to practice guidelines among the University of Washington HIV Study Cohort. Clin Infectious Diseases. 2003;36(6):803–811. doi: 10.1086/368085. [DOI] [PubMed] [Google Scholar]
- 7.Allen C, Jazayeri D, Miranda J, et al. Experience in implementing the OpenMRS medical record system to support HIV treatment in Rwanda Medinfo 200712(Pt 1)382–6. [PubMed] [Google Scholar]
- 8.I-TECH Update # 15, Fall/Winter 2007, (15)1–5. (http://www.go2itech.org/itech?page=co-23-04, accessed 2008-03-12)