Abstract
Power changes have been identified as a frequent and unintended consequence of the implementation of computerized physician order entry (CPOE). However, no previous study has described the degree or direction of power change, or even confirmed that such a relationship exists. Using a validated, standardized instrument for measuring personal power we collected data from 276 healthcare workers in two different hospitals before and after implementation of CPOE. We identified a significant correlation between power perceptions and attitudes toward CPOE. Examining the direction of change by healthcare position, we found that the power perception values decreased for all positions and that attitudes toward CPOE varied based on use of the system. Understanding the relationship between power and CPOE is the first step in enabling systems developers to change the direction of power changes from negative to positive.
Introduction:
The implementation of computerized provider order entry (CPOE) across the health care system has been slow in realization1. In addition to the inherent financial burden, a significant cause for this delay is the high number of system failures resulting from clinicians’ resistance2,3. Changes in workflow and communication, time demands, system complexity, and changes to power structures have all been identified as consequences of CPOE systems that can cause resistance among clinicians4–6. Of these, we believe that changes in the power structure can be particularly far-reaching. While learning a new method for performing tasks can be temporarily disruptive, it is a common occurrence with relatively short-term consequences7,8. In contrast, changes in one’s perceived power in the workplace can be both personal and profound9,10, and therefore are more likely to trigger great concern and strong resistance11.
In previous qualitative studies, physicians have stated that they felt there was a change in the power structure after CPOE implementation4,6,12. To our knowledge, no previous study has addressed power changes among other healthcare professionals, including nurses, unit secretaries/health unit coordinators (HUCs), and physician extenders. Because order transcription, verification, and communication also represent a substantial portion of their work processes, changes in the power structure resulting from CPOE directly affect them also.
Since the implementation of information technology in business has already been shown to cause changes in organizational, power structures13–15, it is reasonable to believe that workers not directly involved in the unit workflow (e.g. medical coders, medial records personnel, and hospital administrators) can also experience power changes. Therefore, physicians are not the only group affected by power changes as a result of CPOE.
To date, there have been no quantitative studies determining the relationship between personal power (power that an individual perceives they have in the workplace) and attitudes toward CPOE. The purpose of this study was to determine if such a relationship exists. The following questions are addressed in this study:
Is there a relationship between perceptions of power and CPOE attitudes?
Do power perceptions and CPOE attitudes change after implementation of CPOE? If so, in what direction is the change, and do they change in the same direction for all types of workers?
Whose power perception and CPOE attitudes change after the introduction of CPOE and how do they change?
To answer these questions, we developed the Semantic Differential Power Perception (SDPP) survey instrument, which has shown to be both reliable and valid in a previous measurement study16.
Methods
This study is a correlational study that used the Semantic Differential Power Perception (SDPP) instrument to gather data on power perception, and attitudes towards CPOE. The instrument scores responses on an 11 point scale ranging from -5 (negative perceptions or attitudes) to +5 (positive perceptions or attitudes) with 0 as the mid or neutral point. Data on various personal characteristics (e.g. age, gender, unit type, etc.) were also collected. Data was collected by administering this survey at our hospital sites - once before implementation of CPOE, and then a second time at least six months after implementation of CPOE.
The study was conducted in two mid-western hospitals: a 500-bed community hospital and a 144-bed pediatric hospital. The hospitals implemented different CPOE systems using different methods of implementation (Epic using Big Bang vs. Eclipsis using Phased-In, respectively).
Subjects were contacted via email, and the survey was completed online. Participants included HUCs, Nurses, Physicians, Physician Extenders, and a general category labeled “Other” which encompassed hospital personnel that do not interact directly with CPOE. This group included such workers as medical coders, billing clerks, nursing assistants, a social worker, an administrator, and admitting clerks. The same subjects were surveyed before and after implementation of CPOE. A $50 drawing was held after each round of data collection at each hospital as an incentive to participate.
The independent variable is the introduction of CPOE into the work environment. The dependent variables are the clinician’s perception of her/his personal power within the work environment, and her/his attitude about CPOE.
Results for each individual were compared before and after implementation. Pre- and post-implementation data were aggregated using participant variables including gender, age, position, length of time in position, education level, employment status (employed by the hospital or independent practitioner), area of specialty (ICU, Non-ICU), unit structure (Team or Hierarchical) and previous experience with an electronic health record (EHR).
Using SPSS v. 15.0©, mean scores for power and CPOE attitudes were calculated for each subject. The data was analyzed overall and then separately for each healthcare position to determine differences and direction of change in the pre-implementation and post-implementation scores. In addition, Pearson correlations were calculated to determine if a relationship exists between perceptions of power and attitudes toward CPOE. Since this study surveys the same individuals both before and after implementation, a repeated measures, General Linear Model (GLM) was also performed to determine if the differences in the scores over time were significant.
Results
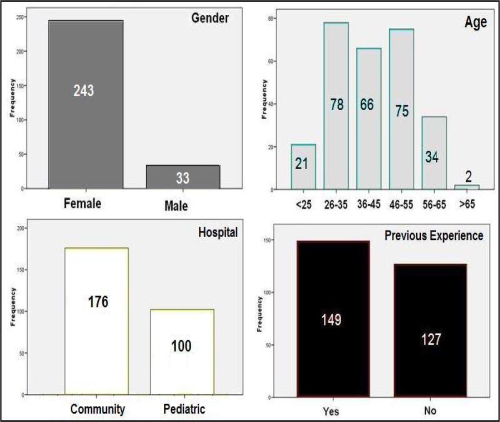
The survey was emailed to a total of 2,801 people, representing all hospital staff at both sites. Pre-implementation, we received 683 responses (24.4% response rate) and post-implementation, we received 276 responses (40% of pre-implementation respondents). However, the pediatric hospital experienced implementation delays. Therefore, the data collected from the pediatric hospital includes only personnel from the two Intensive Care Units (ICU) that have successfully implemented CPOE and those considered as “Other”. Together, these groups represent approximately 25% of the original pediatric hospital responses. For both hospitals, only individuals who responded both pre- and post-implementation were analyzed (Figure 1).
Figure 1.
Demographics of subjects.
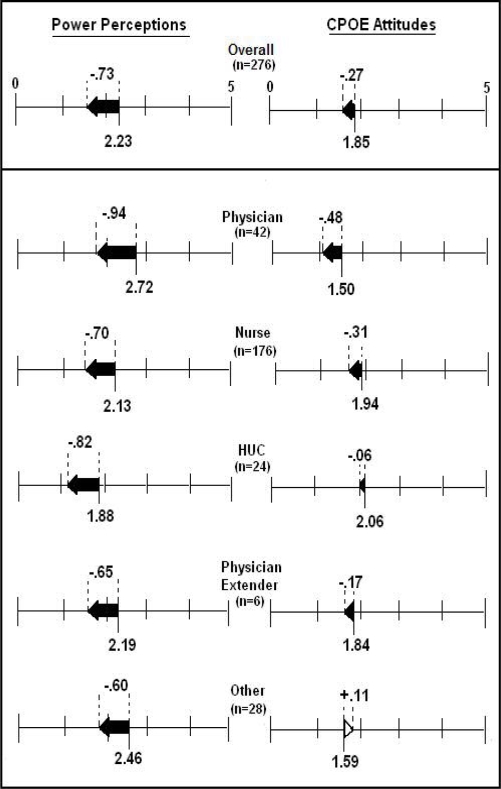
Mean scores for power perception and CPOE attitude from the pre- and post-surveys were calculated, and then aggregated by position (Figure 2). Overall, the change in the power scores was negative (–0.73 decrease). All positions experienced a decrease in perceived power, with physicians experiencing the largest negative change (–0.94 decrease).
Figure 2.
Changes in mean scores for power perceptions and CPOE attitudes, overall and by position. All means were in the positive range, so the scale shown is from 0 to 5, rather than –5 to +5.
The overall difference in CPOE attitudes was also negative, but to a smaller degree (–0.27 decrease). All personnel working directly with CPOE experienced a negative change, but the “Other” group, who did not work directly with CPOE, experienced a positive change in their attitude (+0.11 increase).
Baseline perceptions of personal power from the pre-implementation survey were highest for physicians and lowest for HUCs. Pre-implementation baseline attitudes toward CPOE were the opposite of power perceptions, with HUCs having the highest CPOE attitude score and physicians having the lowest. The results of the repeated measures GLM show that power changes from pre-implementation to post-implementation are significant (F= 130.30, p<.001), as is the case for CPOE attitudes (F= 10.35, p=.001).
Pearson correlations between personal power and CPOE attitude scores were significant both before and after implementation. They remain consistent from pre-implementation to post-implementation (pre-implementation, r=.429, p (two-tailed) <.001, and post-implementation, r=.449, p (two-tailed) <.001). (Table 1)
Table 1.
Correlations between power perceptions and CPOE attitudes - overall and by position.
| N | Pre | Post | |
|---|---|---|---|
| Overall | 276 | .429** | .449** |
| By Position | |||
| HUC | 24 | .594** | .485* |
| Nurse | 176 | .462** | .511** |
| Physician | 42 | .395** | .621** |
| Physician Extender | 6 | .256 | −.310 |
| Other | 28 | .445* | .144 |
**Correlation is significant at the 0.01 level (2-tailed)
* Correlation is significant at the 0.05 level (2-tailed)
Individuals who work with the CPOE system show a significant correlation between power perceptions and CPOE attitudes, with the exception of the Physician Extender group. Post-implementation, power and CPOE attitudes of those who do not work with the CPOE system were not correlated (Table 1).
Discussion
This study is the first to report a quantitative relationship between personal power and CPOE attitude following implementation, and to describe the direction and relationship of these changes. We discuss the results of this study in relationship to the original research questions.
1. Is there a relationship between perceptions of power and CPOE attitudes?
A significant positive correlation exists between perceptions of power and attitudes towards CPOE. This relationship was significant both before and after implementation of CPOE. After implementation, the effect was limited to those subjects who worked directly with the CPOE system. For those who did not use the CPOE system, attitude towards CPOE and perception of personal power moved in opposite directions as a result of implementation.
2. Do power perceptions and CPOE attitudes change after implementation of CPOE? If so, in what direction is the change, and do they change in the same direction for all types of workers?
After the implementation of CPOE, perception of personal power diminished for all subjects, including the group that did not directly use CPOE. Previous studies in business information technology (IT) implementation have shown that IT can and does change the power structure in an organization beyond those directly involved with the change13. We expect that changes in workflow and communication that result from CPOE implementation produce a ripple effect, contributing to changes in power even among staff not directly involved in the process. Changes in their workflow may occur as a result of new communication methods with the clinicians, different reporting patterns, or even a difference in the appearance of the data they work with.
Attitudes toward CPOE diminished for only those subjects that were directly involved with CPOE (HUCs, Nurses, Physicians, and Physician Extenders) and slightly increased for those who were not directly involved with CPOE. This suggests that CPOE causes changes to work patterns for those who use it, but over time, positively affects those on the periphery who experience the benefits of CPOE such as faster processing of orders, more data available, and fewer errors.
Changes in power perceptions were larger than changes in attitudes toward CPOE for all groups. Since perception of one’s own power in the workplace can reflect self-esteem and personal worth9, this is an important observation. Because power diminished for all subjects and the amount of change was larger, it would appear that CPOE implementation has a greater impact on an individual’s perception of personal power than on their attitude toward the system. This suggests that taking steps to reduce or mitigate the impact of power changes will go further toward achieving system acceptance than attempting to influence users’ attitudes toward the CPOE system.
3. Whose power perception and CPOE attitudes change after the introduction of CPOE and by how much?
Not surprisingly, physicians began with a higher perception of power and a more negative attitude toward CPOE than any other group. Physicians’ attitudes and experiences with CPOE systems have consistently shown that they perceive CPOE as interfering with their work, which sets the attitude baseline lower. However, after implementation, both power perceptions and CPOE attitudes became even more negative for physicians; in fact they were more negative than any other group. This could be a result of a self-fulfilling prophecy – “if I expect it to interfere with my work, it will”.
HUCs began with a lower power perception score than any other group and had a drop in power perception that was only exceeded by the physicians. CPOE represents a major change in the HUC’s workflow that could translate into a perception of decreasing importance or loss of control in the workplace. However, even with this decrease in perceived power, their attitudes toward CPOE experienced the smallest degree of negative change. Paradoxically, the fact that they perceive themselves to have less power, they may be more accepting of changes they cannot control, viewing the CPOE system as a “mandatory” part of their job. Also, since their burden of transcribing orders has been minimized, the loss of power may be countered by a positive change in their workflow.
Although physicians and HUCs experienced the greatest decrease in power, their attitudes towards CPOE are very different. Since the effect on the physicians’ work was more negatively affected than the HUCs, we can assume that they incurred greater direct “costs” (e.g. extra time, more work, etc.) resulting in more negative attitudes toward CPOE. Therefore, the greater the direct net effect CPOE has on an individual’s work, the more sensitive their attitudes are to the loss of perceived power. For example, our Other group who don’t directly incur the cost of the new system but receive some of the benefits may be more inclined to overlook their perceived decrease in power.
Because nurses hold the highest percentage of healthcare positions in any hospital, they were also the largest group in the study. We expected that nurses would experience an increase in power and CPOE attitudes since much of the order clarification duty was taken off of their shoulders, but this was not the case. Both power and CPOE attitudes decreased, suggesting that the CPOE system has imposed another layer of control over their work. A recent study of nurses’ perceptions of the impact of electronic health records on their work reflected many of the same issues that physicians mention, such as more time at the computer and less time at the bedside17.
Physician extenders are unique in that they function with CPOE in a manner similar to a physician, but do not have the same power within the healthcare organization as physicians. However the small size of this group precludes more detailed analysis.
Limitations
The pediatric hospital has not yet completed their phased implementation that limited our sample to only approximately 25% of their population. Because the only units implemented at this time are ICUs, the sample population is weighted toward ICU personnel. Further analysis and hospital comparisons will resume when data collection is complete.
Another limitation is that participation in the study may be biased to those subjects that have and use email. These subjects may be more “computer comfortable” than other subjects. If this were the case, it is possible that with more “non-computer comfortable” subjects the CPOE attitudes may have been lower at the start and the change greater than we found in our data.
Future Work
This study lays the groundwork for more detailed analysis of the effects of electronic health records and CPOE on personal power in the workplace. In the future, we expect to use other experimental designs to support a causal relationship between CPOE and diminished power, to analyze the effect of these changes in more detail, and to test possible modifications to the process that could mitigate the effects of CPOE implementation on personal power.
Conclusion
We demonstrate that a significant relationship exists between CPOE attitudes and a healthcare worker’s perception of personal power. We also show that power perceptions diminish for all subjects while CPOE attitudes only diminished for those that work with the CPOE system. For those who work with the CPOE system directly, power perceptions diminish to a greater degree than CPOE attitudes.
This study represents a first step toward measuring power changes at the individual and organizational level during the introduction of CPOE. A more complete understanding of these changes could be an important component in implementation programs designed to minimize the negative effects on personal power. In this way, CPOE related power changes could be transformed from an “unintended consequence” to an “intended intervention”.
Acknowledgments
This study was supported by NLM fellowship grant #5 T15 LM007059-20, and overseen by the University of Pittsburgh IRB, approval #0610080. We would also like to acknowledge the contact people at the participating hospitals who provided mechanisms for recruiting participants.
References
- 1.Ash JS, Gorman PN, Seshadri V, Hersh WR. Computerized physician order entry in U.S. hospitals: results of a 2002 survey. J Am Med Inform Assoc. 2004 Mar-Apr;11(2):95–9. doi: 10.1197/jamia.M1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pare G, Sicotte C, Jacques H. The effects of creating psychological ownership on physicians' acceptance of clinical information systems. J Am Med Inform Assoc. 2006 Mar-Apr;13(2):197–205. doi: 10.1197/jamia.M1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006 Mar-Apr;13(2):121–6. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;13(5):547–56. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aarts J, Doorewaard H, Berg M. Understanding implementation: the case of a computerized physician order entry system in a large Dutch university medical center. J Am Med Inform Assoc. 2004 May-Jun;11(3):207–16. doi: 10.1197/jamia.M1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ash JS, Sittig DF, Poon EG, Guappone K, Campbell E, Dykstra R. The extent and importance of unintended consequences related to computerized provider order entry. J Am Med Inform. 2007;14(4):415–23. doi: 10.1197/jamia.M2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hollingworth W, Devine EB, Hansen RN, Lawless NM, Comstock BA, Wilson-Norton JL, et al. The impact of e-prescribing on prescriber and staff time in ambulatory care clinics: a time motion study. J Am Med Inform Assoc. 2007;14(6):722–30. doi: 10.1197/jamia.M2377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lo HG, Newark LP, Yoon C, Volk LA, Carlson VL, Kittler AF, et al. Electronic health records in specialty care: a time-motion study. J Am Med Inform Assoc. 2007;14(5):609–15. doi: 10.1197/jamia.M2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kipnis D. Does power corrupt? J Pers Soc Psychol. 1972;24(1):33–41. doi: 10.1037/h0033390. [DOI] [PubMed] [Google Scholar]
- 10.Bugental DB, Lewis JC. The Paradoxical misuse of power by those who see themselves as powerless: how does it happen? Journal of Social Issues. 1999;55(1):51–64. [Google Scholar]
- 11.Barley SR. The alignment of technology and structure through roles and networks. Administrative Science Quarterly. 1990;35(1):61–103. [PubMed] [Google Scholar]
- 12.Lapointe L, Rivard S. Getting physicians to accept new information technology: insights from case studies. CMAJ. 2006;174(11):1572–78. doi: 10.1503/cmaj.050281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Constantinides P, Barrett M. Large-scale ICT innovation, power and organizational change. J App Behav Sci. 2006;42(1):76–89. [Google Scholar]
- 14.Butler BS, Gibbons DE. Power distribution as a catalyst and consequence of decentralized technology diffusion. In: McGuire E, Larsen TJ, editors. Information systems and technology innovation and diffusion: issues and directions. Hershey (PA): Idea Group Publishing; 1997. [Google Scholar]
- 15.Markus ML. Power, politics, and MIS implementation. Commun ACM. 1983;26(6):430–44. [Google Scholar]
- 16.Bartos CE, Fridsma DB, Butler BS, Penrod LE, Becich MJ, Crowley RS. Development of an instrument for measuring clinicians' power perceptions in the workplace. J Biomed Inform. 2008 doi: 10.1016/j.jbi.2008.02.004. doi:10.1016/j.jbi.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kossman SP, Scheidenhelm SL. Nurses' perceptions of the impact of electronic health records on work and patient outcomes. Comput Inform Nurs. 2008;26(2):69–77. doi: 10.1097/01.NCN.0000304775.40531.67. [DOI] [PubMed] [Google Scholar]