Abstract
We applied a model of usage categories of electronic health records for outpatient physicians to a large population of physicians, using an established electronic health record. This model categorizes physician users according to how extensively they adopt the various capabilities of electronic health records. We identified representative indicators from usage statistics for outpatient physician use of the HELP-2 outpatient electronic medical record, in use at Intermountain Healthcare. Using these indicators, we calculated the relative proportion of users in each category. These proportions are useful for predicting the expected benefits of electronic health record adoption.
BACKGROUND
For the past decade, adoption of electronic health records (EHRs) has increasingly been suggested as one of the most viable approaches to improving health care in the United States1. EHR adoption has been prominent in political platforms, and is frequently promoted along with proposals to expand health care coverage. While there have been some recent increases in adoption, rates remain low, between 20–25%2. Many see the challenges to adoption as being technical (lack of consistent national standards) or financial (high purchase cost of EHRs)3, leading to efforts in creating standards for interoperability, and local and national efforts to provide funding for initial purchase of systems4.
The argument for improving adoption has been based on projections of benefit that show significant improvement in the cost and quality of care5. These projections recognize these technical and financial barriers to adoption; in fact, the projections are calculated based on an assumption of full adoption after the technical and financial barriers are removed. However, even if these two challenges are fully eliminated, it is unclear that EHR adoption will increase to the level required to achieve the benefits that are currently being promoted. Even when EHRs are purchased and fully interoperable with other systems, lack of actual physician usage can still reduce any benefits. Additionally, others have raised concerns that adoption may not necessarily result in the quality of care improvements that lead to the most substantial benefits of EHRs.
Previously, research around EHR adoption has been considered only in the context of models that considered one level or type of usage, such as Rogers diffusion of innovation model6. Since EHRs consist of multiple components, usage itself can vary, and varied usage can also affect benefits. Recent studies have shown that the use of EHR functions varies substantially among different physicians and physician practices7, and that different functions are correlated to different benefits. This is especially challenging because some of the greatest benefits associated with EHRs are also some of the least likely functions to be implemented8.
As statistics have shown variations in the functions that are adopted by different clinicians, other studies have tried to qualitatively characterize the different types of physician usage. Miller and Sim identified types of physician users within the category of adopters, who varied notably in both the costs and benefits related to EHR use6. They classified physicians that they interviewed as viewers, basic users, strivers, arrivers, or system changers. This research was significant in identifying clear variations in usage patterns; however, since it was assessed and reported qualitatively, it is difficult to make projections on how these categories can be used to quantitatively assess changes in expected benefit. In addition, without clear quantitative indicators to identify the categories, further empirical studies that investigate the facilitators and barriers to improved adoption are difficult. While studies exist that assess quantitatively how physicians use EHRs based on surveying physicians7, research that assesses actual activities performed by physicians within an EHR and relates it to clinician usage are limited.
In this paper, we describe our application of the Miller-Sim categories to a population, to quantitatively assess relative proportions of different categories of EHR adopters. We applied these categories to a large group of physicians, who already had an EHR available, that was already interoperable with other systems in an integrated delivery network, and that had been used in some part by the physician group for over a decade. We identified explicit indicators of usage to categorize physicians according to their use of specific EHR functions, which were directly related to the Miller-Sim categories. For this research, we specifically focus on functions related to increasing quality and decreasing costs for the health care system as a whole; i.e., benefits from quality of care and improved efficiency, rather than simply improved billing and reimbursement.
METHODS
Our analysis was performed with the outpatient clinical information systems at Intermountain Healthcare. Intermountain is a not-for-profit integrated health care delivery system consisting of 21 hospitals, more than 90 outpatient clinics, an employed physician group, and an insurance plan for patients located in Utah and southeastern Idaho. Intermountain has extensive clinical information systems, and a history of using those information systems to improve patient care.9–12 Hospital and outpatient data are interfaced to a longitudinal patient record and stored in the Clinical Data Repository (CDR), which contains records for 2.5 million patients. In the ambulatory setting, providers enter visit notes, problems, and medications into the CDR. The ambulatory EHR, HELP-2, has been in use with periodic updates since 1996. Over 6,000 clinicians use the ambulatory EHR each month to access the records of 331,000 patients. Desktop applications allow users in either inpatient or ambulatory settings to view laboratory results, text reports, and radiology images, regardless of where the care was provided. They also allow documentation of both structured and unstructured data through templates, and ordering of outpatient medications. This information system also contains advanced auditing capabilities, that record the actions of users in accessing various forms of patient data.
Miller and Sim identified in their analysis seven main types of clinical capabilities in EHRs, corresponding to seven sets of clinical activities6. These capabilities are viewing, documenting, ordering, messaging, care management, analysis and reporting, and patient-directed. Below we describe each of these capabilities, and how we measured their use in the Intermountain HELP-2 system.
Viewing represents the core results reviewing capability of the EHR, where laboratory or other assessment results are available. In the Intermountain system, this consists of accessing any stored clinical data in the CDR, whether it be laboratory, observations, or clinical notes. We therefore measured viewing as any time a physician accessed the EHR system, and retrieved data from the CDR.
Documenting is the act of entering data into the system. This can be in structured or unstructured form. At Intermountain, where electronically documented notes were considered part of the medical record, both structured templates and user-configured macros were available for documentation. The structured templates also created text-based clinical notes for viewing within the notes module. As a result, we measured documenting as any time a physician’s actions resulted in the documentation of a clinical note stored to the CDR.
Ordering includes the capability to enter prescriptions into electronic forms as patient medications. The HELP-2 system included electronic prescribing capability, which was helpful to physicians especially in ordering prescription refills. Any new prescription was stored in the CDR, and could be included in various clinical notes. We measured use of ordering by medications stored in the CDR.
Messaging is inter-provider electronic communication within the EHR. The HELP-2 messaging application is called Message Log. This module allows clinicians to receive patient-specific alerts, lab result notifications, or communication from other clinicians or office staff. These messages and any annotations become part of the patient’s electronic medical record. We therefore were able to measure message log use by the messages that were stored to patients’ medical records.
Care management represents disease-specific activities designed to longitudinally manage patient conditions. In the HELP-2 system, problems and allergies could be stored and followed longitudinally with a patient. In addition, specific measures related to treatment of clinical conditions can be documented within structured notes. Decision support tools, such as a patient summary and reminder worksheet13, can then give specific care reminders for treatment or follow-up based on this documentation. We measured two types of care management documentation: structured problems and allergies, and disease-specific structured notes.
Analysis and reporting capabilities allow the review of population data to identify patterns of care across multiple clinical encounters. In the research of Miller and Sim, this analysis and reporting was very limited. At Intermountain, the analysis is directed by physician groups who are part of clinical leadership teams called clinical programs14, and performed by analysts working with the data warehouse. Use of analysis and reporting is thus assessed by measuring the number of physicians participating in clinical program leadership.
Patient directed capabilities allow direct communication with patients through the EHR. Miller and Sim observed almost no patient directed activities in their evaluation. At Intermountain, the patient directed capabilities of the EHR were the least mature in the system, and still being implemented only in pilot mode. Therefore, they were not included in this analysis as representing a core category of EHR usage.
We queried the audit logs and data storage information in the CDR to identify the number of physicians and degree of use for each of these functional capabilities of the EHR. We queried unique physician users for different types of usage during one month of use. We then grouped these capabilities according to the different usage categories of viewers, basic users, strivers, arrivers, and system changers, identified by Miller and Sim.
Viewers were defined as physicians who only used the viewing capability of the EHR. Basic users were physicians who only used the capabilities that provided direct benefit to physicians, such as improving efficiency of documentation or prescription refills. Strivers were physicians who began to use structured documentation for problems and allergies, but did not document within structured templates that were designed to support evidence-based guidelines. Arrivers were physicians who used structured templates for adherence to guidelines. System changers were physicians who advocated for changes either in clinical program leadership meetings or user group meetings.
Once the capabilities representing these usage categories were identified, we computed the proportion of total physician users who met each category.
RESULTS
In January 2008, there were 4127 total physician users who had access to the HELP-2 EHR. Of these, 3348 physicians (81%) actually accessed the EHR, and 2511 of these 3348 physicians (75%) also entered data into the system, in the form of notes or medications. Of these, 650 physicians (19%) stored structured data, in the form of problems and allergies (373 physicians, 11% of physicians using the system), or other structured data (277 physicians, 8%). Table 1 shows the percentages of users of the system.
Table 1.
Types of use of HELP-2 EHR, January
| EHR use | Total physicians | % |
|---|---|---|
| Access to system | 3348 | 100 |
| Entered notes/medications | 2511 | 75 |
| Stored problems/allergies | 373 | 11 |
| Stored other structured data | 277 | 8 |
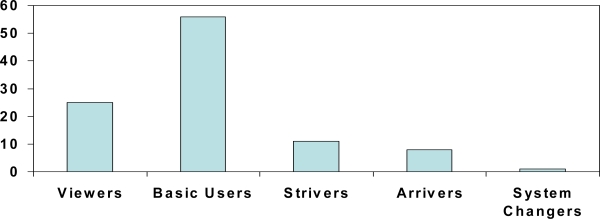
From this data, physician users were extrapolated into the following categories: viewers (25%), basic users (56%), strivers (11%), arrivers (8%).
Additionally, we identified approximately 20 physicians who participated in the primary care clinical program leadership or in HELP-2 user groups, that had recommended changes to the system. They represented system changers, at less than 1% of users. Figure 1 shows a histogram of the various user categories.
Figure 1.
Relative percentages of various categories of users, based on analysis of ambulatory HELP-2 users, January 2008.
DISCUSSION
The different categories of EHR use demonstrate varying levels of use of functionality within an EHR, even after the system has overcome the main barriers of adoption. The Intermountain EHR, HELP-2, was supplied at no incremental cost to the Intermountain physicians, and the system was already integrated with longitudinal data from multiple ancillary services. Yet even though the main barriers to adoption were removed, and the system was mostly adopted at some level, there was still a significant lack of use of core EHR functions among users.
These functions that showed minimal use are specifically related to improved quality of care, due to decision support around evidence-based guidelines. This supports survey results obtained by Menachemi et al., showing that there is a late uptake of key components of EHRs 8. However, this finding suggests that the delay may be more significant, and may be related to other issues than just the natural progression along a technology acceptance model. HELP-2 was not a recent installation with these users, but rather they had use of the system for a relatively long period of time. This adoption reflects more a steady state point.
It is important to recognize that the users of HELP-2 at Intermountain were not specifically forced to use the system for documentation or for care management functions. The system was implemented according to the requests of the physician groups. There were incentives implemented according to the clinical program structure, however, which was similar to many pay-for-performance initiatives. It is therefore informative that even pay-for-performance initiatives may not be sufficient to spur adoption of quality-specific EHR functions.
Of interest in this study is the high level of use of documentation, with a corresponding low level of use of structured documentation. Other studies at Intermountain have demonstrated that documentation is itself a frequently used component of the EHR, with use growing over time15. The use of documentation has its own incentives, but they are more applicable at Intermountain to efficiency rather than improved use of quality initiatives. For example, physicians using documentation tools have decreased transcription costs while decreasing documentation time. This is in large part to specific documentation tools that have been developed for efficiency purposes, such as macro-based templates16. Structured documentation is also used, and Intermountain has a history of developing structured forms for storing coded data that can be used for decision support purposes15. However, these templates do not represent the majority use case of documentation in the EHR.
There are specific weaknesses to this study. First, the study was performed at a single institution, and adoption patterns may be different at other organizations. It has been mentioned above that Intermountain did not mandate EHR use; a similar study at an institution that more aggressively implemented systems, such as the Veterans Administration, may result in different findings. However, Intermountain does have a long history of information systems use, and it is reasonable to expect that it represents more advanced usage patterns. Additionally, some incentive structures, such as a pay-for-performance type initiative was in place. Other limitations were that we did not study the use of the system longitudinally. It may be important to identify what types of users move from basic users to strivers to arrivers, to identify the actual barriers to use. We have performed studies that looked at the use of the system over time, but these studies did not differentiate between basic users and more advanced users; they only studied whether physicians used documentation at all15. Finally, we did not study the specific incentives and barriers to moving between adoption levels. This study should be seen as initial work that can support such studies, however. By identifying methods for categorizing physician users according to these levels of adoption, further studies can investigate additional characteristics of the physicians in the different categories, or measure the effects of different incentives to move between categories. Such research can inform and improve current policy initiatives aimed at improving EHR adoption, which currently focus only on the technical and financial barriers to use.
CONCLUSION
Physician use of specific electronic health record functionalities was shown to vary substantially across categories of usage. The more advanced, structured components of the EHR, that are presumed to have the greatest effect on improved quality and costs, that have spurred movements for adoption of EHRs, are actually the less-used components of the systems. Policies advocating the adoption of EHRs should focus on incentives that will result in the use of these more advanced components, rather than simply pushing for basic purchasing and use of EHRs.
References
- 1.Institute of Medicine . Crossing the Quality Chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 2.Jha AK, Ferris TG, Donelan K, et al. How common are electronic health records in the United States? A summary of the evidence. Health Aff (Millwood) 2006 Nov-Dec;25(6):w496–507. doi: 10.1377/hlthaff.25.w496. [DOI] [PubMed] [Google Scholar]
- 3.Overcoming barriers to electronic health record adoption. http://www.hfma.org/NR/rdonlyres/4FE68E23-0A47-4674-ABBA-F1A4AA1E73A9/0/ehr.pdf. Accessed March 14, 2008.
- 4.Smith VK, Gifford K, Kramer S, Dalton J, MacTaggart P, Warner ML.State E-Health Activities in 2007: Findings From a State SurveyThe Commonwealth FundFebruary2008
- 5.Walker J, Pan E, Johnston D, Adler-Milstein J, Bates DW, Middleton B.The value of health care information exchange and interoperability Health Aff (Millwood) Jan-Jun 2005. Suppl Web Exclusives:W5-10-W15-18 [DOI] [PubMed]
- 6.Miller RH, Sim I, Newman J.Electronic medical records: lessons from small physician practicesCalifornia HealthCare Foundation; October 20032003
- 7.Simon SR, McCarthy ML, Kaushal R, et al. Electronic health records: which practices have them, and how are clinicians using them? J Eval Clin Pract. 2008 Feb;14(1):43–47. doi: 10.1111/j.1365-2753.2007.00787.x. [DOI] [PubMed] [Google Scholar]
- 8.Menachemi N, Ford EW, Beitsch LM, Brooks RG. Incomplete EHR adoption: late uptake of patient safety and cost control functions. Am J Med Qual. 2007 Sep-Oct;22(5):319–326. doi: 10.1177/1062860607304990. [DOI] [PubMed] [Google Scholar]
- 9.Evans RS, Pestotnik SL, Classen DC, et al. A computer-assisted management program for antibiotics and other antiinfective agents. N Engl J Med. 1998 Jan 22;338(4):232–238. doi: 10.1056/NEJM199801223380406. [DOI] [PubMed] [Google Scholar]
- 10.Clayton PD, Narus SP, Huff SM, et al. Building a comprehensive clinical information system from components. The approach at Intermountain Health Care. Methods Inf Med. 2003;42(1):1–7. [PubMed] [Google Scholar]
- 11.Haug PJ, Gardner RM, Tate KE, et al. Decision support in medicine: examples from the HELP system. Comput Biomed Res. 1994 Oct;27(5):396–418. doi: 10.1006/cbmr.1994.1030. [DOI] [PubMed] [Google Scholar]
- 12.Kuperman GJ, Maack BB, Bauer K, Gardner RM. Innovations and research review: the impact of the HELP computer system on the LDS Hospital paper medical record. Top Health Rec Manage. 1991 Nov;12(2):76–85. [PubMed] [Google Scholar]
- 13.Wilcox A, Jones SS, Dorr D, et al. Use and impact of a computer-generated patient summary worksheet for primary care. Proc AMIA Annu Fall Symp. 2005 [PMC free article] [PubMed] [Google Scholar]
- 14.Larsen DL, Cannon W, Towner S. Longitudinal assessment of a diabetes care management system in an integrated health network. J Manag Care Pharm. 2003 Nov-Dec;9(6):552–558. doi: 10.18553/jmcp.2003.9.6.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clayton PD, Naus SP, Bowes WA, 3rd, et al. Physician use of electronic medical records: issues and successes with direct data entry and physician productivity. AMIA Annu Symp Proc. 2005:141–145. [PMC free article] [PubMed] [Google Scholar]
- 16.Wilcox AB, Narus SP, Bowes WA., 3rd Using natural language processing to analyze physician modifications to data entry templates. Proc AMIA Symp. 2002:899–903. [PMC free article] [PubMed] [Google Scholar]