Abstract
In recent years, there have been high expectations for RFID technologies applied in the medical field, particularly for automatic identification and location of patients and medical supplies. However, few studies have measured the applicability of currently available RFID technologies in a medical environment. To determine the technical factors that affect the performance of RFID systems, we examined the performance of different types of tags for medications, medical equipment, nurses, and patients under different experimental conditions. Three kinds of passive RFID tags and one active RFID tag were used in our study. Passive tags were affected by materials such as liquid and metal. Tags based on 13.56MHz were most suited for identifying medications. Tag placement was one of the main factors involved in correct identification of nurses, patients, and medical equipment. The results of this study may help decision makers decide whether (which) RFID technologies are useful for tracking clinical workflow.
Introduction
Applications of radio frequency identification (RFID) technologies are getting common in some fields such as the retail industry or transit systems. In recent years, there have also been high expectations for RFID technologies applications in clinical medicine1. Some authors have proposed that matching medication data to the correct patient using RFID technology may help prevent some types of medical errors2,3. Currently used systems, such as those based on bar coding4, cannot passively perform this type of matching, requiring users to point devices to particular places. However, some researchers reported that the implementation of some types of basic Computerized Physician Order Entry (CPOE) systems (which may or may not include barcode systems or RFID systems) may also induce other medical errors due to inappropriate operation5. For example, caregivers may have to select a certain patient in a computer screen before delivering medications, and they have to log in or log out every time, wasting valuable time. These operations may result in medical errors. The expectation is that accurate RFID, which has the function of passive auto-recognition of patients and caregivers, can help solve this problem6.
However, RFID technologies are very sensitive to many factors, such as characteristics of the environment and tagged objects7. To our knowledge, there have been few previous reports based on on-site experiments showing that RFID is suited for usage in a hospital, specifically for medication delivery and mapping nurse practice workflow8. In a clinical environment, there might be particular needs that have few parallels in other fields. Therefore, a study addressing the usability of RFID in a clinical setting is warranted.
In this study, we conducted a feasibility experiment to measure the performance and the most effective placement of RFID tags on patients, healthcare providers, and objects in a hospital environment. The main purpose of the RFID system we studied was to allow seamless monitoring of certain nurse-patient interactions at the bedside, leading to improvements in the workflow that will increase nurse efficiency, which in turn has the potential to enhance patient safety. In our system, RFID tags were attached not only to patients, providers, and major medical equipment such as a medical cart and an IV pole, but also to medications and small medical supplies.
The system was designed to prevent the misidentification of patients and consequent administration of the wrong medications (including dose and route), or the administration of inappropriate clinical interventions. In the study reported here, we set up an experimental environment based on scenarios of medication-delivery and measured the performance of some components of the RFID system.
Methods
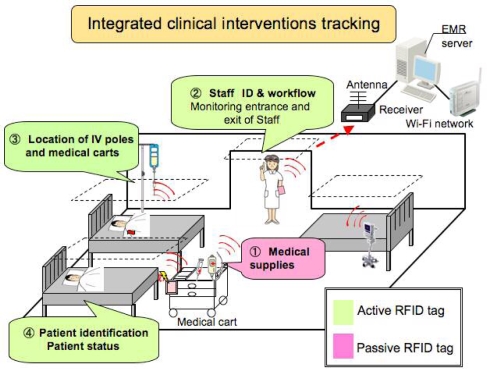
Our system’s purpose was auto-tracking of all RFID data related to clinical interventions. This passive system operation should not add any extra effort in the identification of objects and people. Different types of RFID technology were employed according to different types of clinical scenarios. The purpose of the system was not only to authenticate identification of patients and providers, but also to obtain medication and location data for preventing medical errors and tracking clinical interventions (Figure 1).
Figure 1.
RFID-based system to track clinical interventions at the bedside.
In this experiment, we used four kinds of RFID tags whose brief specifications are listed in Table 1: (1) 13.56MHz passive tags, (2) 2.45GHz passive tags, (3) UHF passive tags, and (4) an active tag that could be tuned to our experimental setting. Passive RFID tags are small, thin, cheap, and they require no battery, so they are more commonly used for identifying small objects such as medical supplies or medications. They are powered by an external tag reader.
Table 1.
Passive and active RFID specifications.
| 13.56 MHz | 2.45 GHz | UHF | Active tag | |
|---|---|---|---|---|
| Frequency | 13.56 MHz | 2.45 GHz | 950 MHz | 300 MHz |
| Memory | 32kbyte | 128bit | 528bit | None |
| Size | 20x30mm | 4x40mm | 40x60mm | 23.8x28x6.4mm |
| Power | None | None | None | DC3V coin battery |
| Maximum communication distance | ~60mm | ~250mm | ~3000mm | ~3000mm |
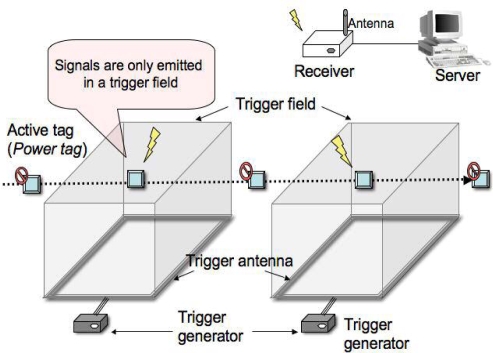
Active tags need a battery and emit signals to a receiver, usually either on a continuous basis or when an embedded accelerometer detects motion. For this experiment, we applied a new active tag technology named Power Tag (from Matrix Inc., Osaka, Japan) 9 that can recognize IDs when the tag is triggered in a specific field. The Power Tag system consists of active tags with battery, a trigger antenna, a trigger generator, and a receiver (Figure 2). When the tag enters a specific area covered by the trigger antenna, the tag ID and the antenna ID signals are transmitted to the receiver. When the tag exits the specified area, the tag stops its transmission, resulting in battery savings. The trigger area can be made basically anywhere and in any formation, by placing an antenna on the floor or on the ceiling. Moreover, the trigger area can be confined or expanded by modifying the antenna radio field strength.
Figure 2.
The Power Tag system. An active RFID tag starts transmitting information when detected by a trigger antenna.
To find the most suitable RFID specification and settings for a typical hospital ward, and to clarify environmental factors that influence RFID’s reading conditions, we conducted an experiment in a simulation hospital environment at the Tokyo Medical and Dental University in Tokyo, Japan.
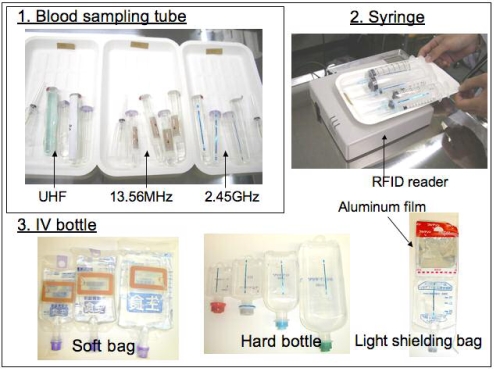
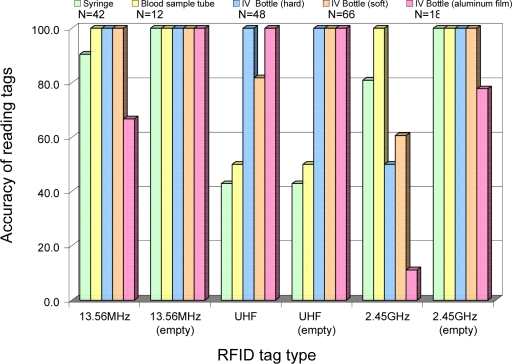
We tested the simultaneous identification of a number of medical supplies by using three kinds of RFID systems (Figure 3). We used different IV bags or bottles, syringes, and blood sampling tubes. To determine the influence of liquids, contents of the IV bags and bottles were varied. We examined accuracies of passive tags on medical supplies for tags based on three frequencies: UHF, 13.56 MHz, and 2.45 GHz. The tags were attached to all medical supplies in advance, the reader was placed on a medical cart, and a nurse put these medical supplies on and off the cart. These procedures were repeated three times for each type of tag.
Figure 3.
Tag types and tagged medical supplies.
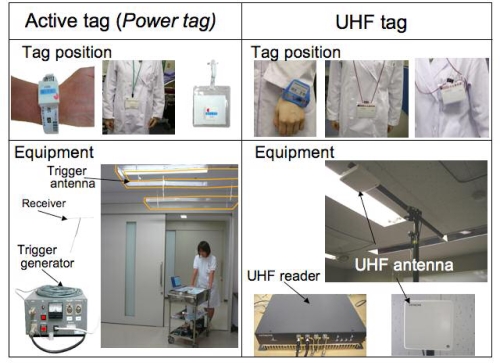
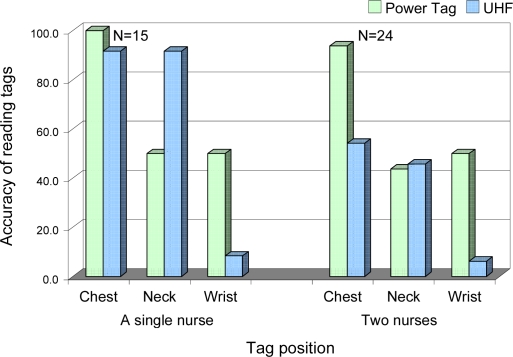
Next, we examined whether RFID tags could be correctly recognized in real time for tracking the location of nurses, patients, and medical equipment. We used active tags (Power Tag) and passive UHF tags for locating patients, providers, and large medical equipment. In a patient room, Power Tag antennas were placed both at the ceiling over the room’s entrance and at the bedside (Figure 4). Two nurses walked under the antenna wearing each different type of tag three times. The tags were placed at different body positions (on necklaces or wristbands). We used several combinations of tag and antenna positions. We conducted additional experiments in which two members of the medical staff walked side-by-side under the antenna wearing different types of tags and also walked in opposite directions.
Figure 4.
Location detection using active Power Tags and UHF tags. Tags are shown at the top. Antenna were placed at the ceiling, over the entrance and the bedside. Readers are shown at the bottom.
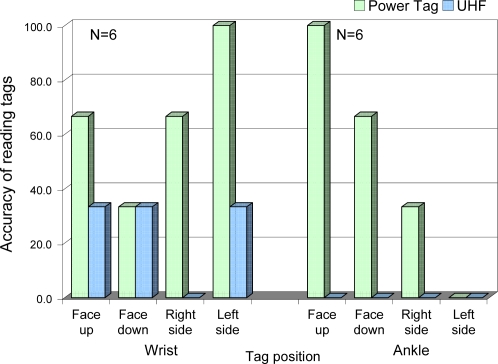
For recognition of patient IDs, a study subject wearing a tag lay down on the hospital bed and changed positions. The tag was attached to both the wrist and ankle and the accuracy of the reading was examined.
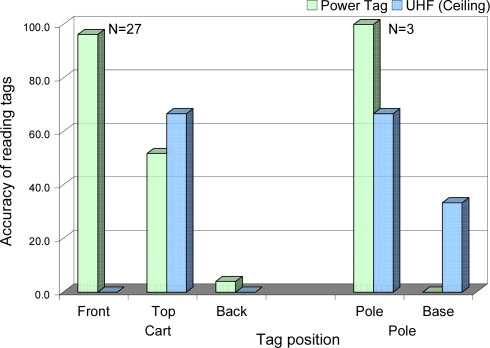
Tags were also attached to medical equipment such as IV poles and a medical cart. On the IV pole, tags were placed at the base and at the pole. Tags were placed at the front, the back, and the top of the medical cart. This equipment was moved under the antenna by study personnel and the accuracy of the measurements was recorded.
Results
Accuracies in the detection of medical supplies are shown in Figure 5. We obtained good performances for all types of RFID tags, with few exceptions. Table 2 summarizes factors that influenced the recognition of RFID tags. The detection of 13.56MHz tags and of 2.45GHz tags on IV bottles was affected by aluminum films. The UHF tag was not affected by metal, but was affected by liquid contents. Distance between readers and tags was, as expected, one of the influencing factors on reading performance. Tags were too large to be attached to small medical supplies such as syringes or blood sampling tubes holding less than 20ml.
Figure 5.
Medical supply detection using different RFID tags.
Table 2.
Effect of liquid content, aluminum film and tag size on tag readings.
| RFID tag type | Liquids | Aluminum film | Tag size |
|---|---|---|---|
| 13.56MHz | n=42 (90.5%) | n=18 (66.7%) | - |
| 13.56MHz (empty) | - | - | - |
| UHF | n=66 (81.8%) | - | n=54 (46.5%) |
| UHF (empty) | - | - | n=54 (46.5%) |
| 2.45GHz | n=156 (63.9%) | n=18 (11.1%) | - |
| 2.45GHz (empty) | - | n=18 (77.8%) | - |
Since medical supplies often contain liquids and also often need metal films to be light-resistant, we concluded that the 13.56 MHz tag was the most appropriate for our bedside system.
Figure 6 shows that the best position for detecting nurse IDs with the Power Tag was on the chest. The performance was, as expected, related to the distance between the tag and the antenna on the ceiling. The UHF tag was correctly detected both on the necklaces and the wristbands. However, if two nurses walked under the antenna at the same time, the accuracy of the tag readings dropped by about half. Considering that a number of nurses are often in the same room, we found the Power Tag was the most adequate for detecting nurse IDs.
Figure 6.
Nurse identification accuracy by tag position. Left bars correspond to detection of a single nurse and on the right detection of two nurses.
Figure 7 shows results related to the detection of patient IDs. The results of the Power Tag on a patient’s wrist changed depending on the patient’s position, because of the setting of single signal direction. However, the radio wave of the Power Tags could be adjusted to be multi-directional. The UHF tag could not detect IDs of patients lying on the bed.
Figure 7.
Patient identification accuracy according to tag placement.
The Power Tag placed in front of the medical cart had the best performance in detecting medical equipment, (Figure 8). Similarly, with IV poles, the Power Tag attached to the pole rather than its base resulted in the best performance. Meanwhile, UHF tags placed on either the medical cart or an IV pole were detected at a rate of approximately 60% and were therefore deemed inadequate for use in this environment.
Figure 8.
Detection of medical equipment.
Discussion
We measured some influencing factors that need consideration before implementing an RFID system in a hospital.
Liquid contents seem to effect on the reading conditions for most RFID tags. Among them, the 13.56MHz tag seems to be the most appropriate. Barcode readers are not affected by liquid contents, but most barcode labels are made of paper and their readability may decrease as they deteriorate10. In addition, barcode systems may perform poorly when IV bags are curved and tags are wrinkled11.
When passive tags were in direct contact with metal, it was somewhat difficult to get accurate readings. UHF tags could not be put on small syringes, but other tags were small enough to put on 1 ml syringes and were reasonably accurate. Barcode labels are also not easy to place on small medical supplies.
For identification of providers and patients, we found the RFID system to have a relative advantage when compared to the barcode system, given that the RFID system provides not only identification information, but also location information in real time. However, the readings need to be more reliable before the system can be applied in a hospital setting.
There are other studies of active tags applications for tracking medical equipment or patients12. However, in some active tag technologies the radio waves are passed through a wall or the ceiling. This can cause false location readings. On the other hand, the Power Tag required us to limit the detection area to that covered by the trigger antenna.
In terms of system operability, a barcode system requires line of sight, precise aiming of the scanner, and the use of two hands in the scanning process. The height of IV poles may create a difficult angle for barcode scanning13. For scanning wristbands, long sleeves constitute a problem. Furthermore, when nurses check their patients during nighttime, it may be difficult to locate the wristband without waking the patient up. There is a potential benefit in using active tags that automatically identify patient IDs, as long as their reliability can be ascertained.
Conclusion
From our experiments, we concluded that environmental factors affected the performances of all RFID systems, and we took the first steps towards the identification of systems that can be used in a hospital setting. Practical, reliable, and seamless monitoring of clinical interventions at the bedside will probably require a combination of both active and passive tag RFID technologies, particularly tailored to their clinical use. The next step in this study is the design and implementation of a practical combined RFID system that is fully integrated with the clinical system, which one day could be employed in large scale for improving clinical workflow and minimizing medical errors.
Acknowledgments
This study was performed with the help of special coordination funds for promoting science and technology from the Ministry of Education, Culture, Sports, Science and Technology, the Japanese government. We would like to acknowledge Hitachi, Ltd., Uniadex Corporation, and Matrix Inc for their collaboration in this research.
References
- 1.Wicks AM, Visich JK, Li S. Radio frequency identification applications in hospital environments. Hosp Top. 2006;84(3):3–8. doi: 10.3200/HTPS.84.3.3-9. [DOI] [PubMed] [Google Scholar]
- 2.Booth P, Frisch PH, Miodownik S. Application of RFID in an integrated healthcare environment. Conf Proc IEEE Eng Med Biol Soc. 2006;1:117–9. doi: 10.1109/IEMBS.2006.259389. [DOI] [PubMed] [Google Scholar]
- 3.Perrin RA, Simpson N. RFID and bar codes-critical importance in enhancing safe patient care. J Health Inf Manag. 2004;18(4):33–9. [PubMed] [Google Scholar]
- 4.Bates DW. Preventing medication errors: a summary. Am J Health Syst Pharm. 2007;64(16):1678. doi: 10.2146/ajhp070190. [DOI] [PubMed] [Google Scholar]
- 5.Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL.Role of computerized physician order entry systems in facilitating medication errors JAMA 2005. 9293101197–203. [DOI] [PubMed] [Google Scholar]
- 6.Nagy P, George I, Bernstein W, Caban J, Klein R, Mezrich R, Park A. Radio frequency identification systems technology in the surgical setting. Surg Innov. 2006;13(1):61–7. doi: 10.1177/155335060601300110. [DOI] [PubMed] [Google Scholar]
- 7.Hosaka R. An analysis for specifications of medical use RFID system as a wireless communication. Conf Proc IEEE Eng Med Biol Soc. 2007;2007:2795–8. doi: 10.1109/IEMBS.2007.4352909. [DOI] [PubMed] [Google Scholar]
- 8.Britton J. An investigation into the feasibility of locating portable medical devices using radio frequency identification devices and technology. J Med Eng Technol. 2007;31(6):450–8. doi: 10.1080/03091900701292141. [DOI] [PubMed] [Google Scholar]
- 9.The Powertag by Matrix Inc http://www.matrix-inc.co.jp/matrix-en/whatis/system.html(Last accessed March 2008)
- 10.Cochran GL, Jones KJ, Brockman J, Skinner A, Hicks RW. USP medical safety forum: errors prevented by and associated with bar-code medication administration systems. Joint Comm J Qual Patient Safety. 2007;33:293–301. doi: 10.1016/s1553-7250(07)33034-1. [DOI] [PubMed] [Google Scholar]
- 11.Young D. Pittsburgh hospital combines RFID, bar codes to improve safety. Am J Health Sys Pharm. 2006;63:2431. doi: 10.2146/news060030. [DOI] [PubMed] [Google Scholar]
- 12.Fry EA, Lenert LA. MASCAL: RFID tracking of patients, staff and equipment to enhance hospital response to mass casualty events. AMIA Annu Symp Proc. 2005:261–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Cummings J, Bush P, Smith D, Matuszewski K. Bar-coding medication administration overview and consensus recommendations. Am J Health Sys Pharm. 2005;62:2626–2629. doi: 10.2146/ajhp050222. [DOI] [PubMed] [Google Scholar]