Abstract
Inpatient discharge instructions provide critical information for patients to manage their own care. These instructions are typically free-text and not easy for patients to understand and remember. In this pilot study, we developed a set of pictographs through a participatory design process and used them to enhance two mock-up discharge instructions. Tested on 13 healthy volunteers, the pictograph enhancement resulted in statistically significant better recall rates (p<0.001). This suggests that patient comprehension and recall of discharge instructions could be improved by supplementing free texts with pictographs.
Introduction
Inpatient hospital discharge is a complex process involving a team of health providers such as physicians, nurses, dietitians, physical therapists, social workers and care coordinators. The discharge and aftercare planning process begins at admission and continues throughout a patient's hospital stay. Upon discharge, typically a nurse presents and explains written instructions to the patient or patient surrogate.
Discharge instructions provide critical information for patients to manage their own care. These instructions are required by the Centers for Medicare and Medicaid Services (CMS) and the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), as Core Measures to meet accreditation and public reporting requirements [1, 2]. However, prior studies show that many patients (and in some cases a majority of patients) do not fully understand or recall the instructions they receive [3–5]. This lack of comprehension also reduces patient satisfaction and compliance [6–8].
Indeed, understanding and memorizing the hospital discharge instructions can be very challenging. At the time of discharge, patients or family members may be experiencing physical and emotional discomfort. They may be eager to leave, and thus, less interested in the instructions. Moreover, a significant number of patients have low literacy and/or health literacy levels. In addition, the busy hospital setting may distract the patient’s attention from such instruction.
To mitigate these factors, discharge instructions must be presented in an easily understood format for patients to review during and after discharge. To this end, hospitals like the Brigham and Women’s Hospital (BWH), and commercial companies such as Meditech, Exit-Writer, and Carenotes (Micromedex), offer patient-friendly instructions for certain medical conditions, and these instructions sometimes contain pictographs.
A number of studies have shown that pictographs can improve patient comprehension of health information [9–11]. However, instructions that do include pictographs are usually “canned” materials, not targeting specific patients. Most patient-specific discharge instructions still contain only free text. How to provide visual aid to these discharge instructions is a research question that we are trying to answer. As a first step, we conducted a pilot study to develop pictographs for discharge instructions and test their efficacy in improving patient comprehension and recall.
Background
Although numerous studies in health care and other fields have demonstrated that pictographs can improve comprehension, several problems inhibit the use of pictographs in discharge instructions. One problem is the lack of a standard or validated pictograph language for patient communication. Furthermore, pictographs used in health communication were often developed in an ad-hoc fashion.
In the medical informatics domain, Preiss, Starren and Ruland have developed systematic methods to develop icons and pictures for clinical applications [9, 12, 13]. Particularly relevant to this pilot study is Ruland’s study that employed a participatory design approach toward pictograph creation, with pediatric cancer patients as the target audience [9]. In the participatory design process, a graphical designer created an initial set of pictures. The focus group participants were presented with one picture at a time, without any text labels, and were asked what they thought the pictures depicted and why. If the participants did not recognize the picture correctly, they were invited to revise the pictures or draw new ones. The revisions were then incorporated into the final pictograph design.
Materials and Methods
Materials
We first collected a convenient sample of 30 discharge documents (10 discharge instructions and 20 discharge summaries) from the Brigham Integrated Computer System (BICS) system of the BWH in Boston, MA. (Hundreds of thousands of discharge documents may be retrieved from BICS.) The discharge instruction and the care instruction section of the discharge summary contain similar information, however, the former is written in simpler language. This is because the intended audience of discharge instructions is patients rather than clinicians.
We then analyzed the care instructions in the discharge instructions and discharge summaries, and identified six care domains: medication, activity level, dietary restriction, follow-up plan, general care (such as wound care and hygiene), and dangerous signs that need immediate attention by a physician (Table 1). These domains correspond with the CMS and JCAHO reporting requirements. While each document is patient-specific, the language of different documents has a large overlap. Excluding medications route and frequency-related instructions, we extracted 38 distinct instructions from the 30 documents.
Table 1.
Examples of specific discharge instructions.
| Areas | Instructions |
|---|---|
| Activity Level | Do not lift more than 10 lbs. |
| General Care | Avoid tub bath until the wound is completely healed. |
| Medication | Administer iron product minimum 2 hrs before or after levofloxacin. |
| Diet | Low cholesterol and saturated fat diet. |
| Danger Sign | Drainage from the wound |
| Follow up | See Dr. Homer Simpson in 2 weeks. Call 617–123–4556 |
Pictograph Development
To identify the instruction text that can be enhanced by pictographs and create the pictographs, we recruited two nurses and two consumers. Both nurses have years of clinical and patient education experience. (One of the nurses, MH, is a co-author on this paper.) In the participatory design process, we interviewed each participant separately to accommodate their schedules. The participants were first presented with 38 specific instructions and were asked the following questions:
Is the instruction easy to understand?
Can the instruction be made easier to understand or remember with pictorial aid?
If pictorial aid is warranted, how can the instruction be illustrated?
Each nurse interview took 60 to 90 minutes. The nurses suggested that 32 out of the 38 instructions be illustrated to promote understanding. They also commented on how the specific instructions might be illustrated. Each consumer interview, on the other hand, took only 20 to 30 minutes. The consumers did not identify any instruction as specifically requiring pictorial aid, though did think illustration would be helpful in general.
Among the six instructions not recommended for illustration, two instructions (“walking as tolerated” and “no restriction in diet”) were deemed to be self-explanatory, and four (“resume regular exercise,” “do any activity as tolerated,” “out of bed for most of the day” and “house ADA diet 1800 Cals/day”) were deemed to require substantial explanation by nurse when delivering the instructions.
We targeted 20 out of the 32 candidate instruction items in the pictographs design, due to time and resource constraints. We produced the initial pictograph designs and presented them to the nurse and consumer participants. The pictographs were shown with the corresponding text labels. All participants commented as to whether the semantics of the pictographs were clear, whether the semantics matched the text labels, and whether and how they should be improved. The pictographs were then revised accordingly. Figure 1 shows how a pictograph was revised according to the nurses and consumers’ comments.
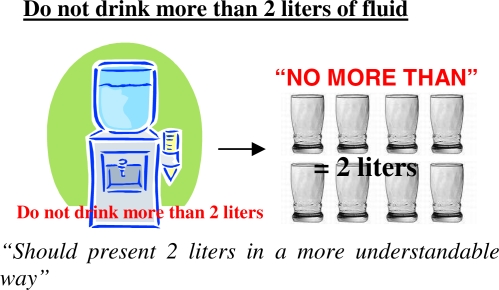
Figure 1.
An example of the pictograph revision process. For the instruction “Do not drink more than 2 liters of fluid”, nurses and consumers suggested representing the quantity of water in a more explicit way (with the number of glasses).
Based on consumers’ and nurses’ suggestions, we decided that medications are best represented by their actual images. For this preliminary study, we searched for images of medications contained by the discharge instructions used in the evaluation study on the Internet. When an actual image can not be found, we substituted a generic icon of medication.
Evaluation
For evaluation, we created two mock-up discharge instructions, each based on a real medical scenario. One was for a surgery patient with hip and spine fracture by fall (case A), and the other was for a diabetes mellitus patient with neuropathy, e.g., ulcer in the foot (case B). (Because of privacy concerns, we did not use the discharge instructions of actual patients.) Two versions of mock-up discharge instructions were created for each case: a text only version reflecting typical BWH discharge instructions, and a pictograph enhanced version containing the original text and the icons we developed and the medication images we collected. Case A contained 15 specific instructions and case B contained 19 specific instructions. Both cases covered the six care domains previously described.
We recruited a convenient sample of thirteen volunteers who are not health care professionals from a BWH office building. About half of the subjects are men; most of the subjects are below 40 years; about half of the subjects have an education level of college or above (Table 2).
Table 2.
Basic demographics of the evaluation study subjects.
| Demographics | N |
|---|---|
| Gender | |
| Male | 7 |
| Female
|
6
|
| Age | |
| <20 | 3 |
| 20–30 | 5 |
| 30–40 | 3 |
| >40
|
2
|
| Education | |
| Lower than college level | 7 |
| College level or more
|
6
|
Each subject was randomly assigned to two groups: Group I receiving the text-based A and the pictograph enhanced B, Group II receiving the text-based B and the pictograph enhanced A. When presented with an instruction, a subject was asked to assume the role of the patient being discharged. An author (HK) who is a registered nurse played the role of a discharge nurse, reviewing the instruction with the subject, providing explanations and answering questions. The subject was then allowed extra time to read the instructions. Immediate recall was collected by asking the subject to write down what he/she remembered immediately after reviewing and reading the instruction. A delayed recall was collected also in writing 5 days later. The same testing procedure was then repeated for the second instruction, after data collection for the first instruction was completed. The study design is presented in Table 3.
Table 3.
Text-based vs. pictograph enhanced instruction recall study design
| Group | Case Version | Testing Procedure | |||||||
|---|---|---|---|---|---|---|---|---|---|
| I | AText | 1st Instr Given | immediate Recall | Wait 5 days | Delayed recall | ||||
| BPictograph | 2nd Instr Given | immediate Recall | Wait 5 days | Delayed recall | |||||
| II | BText | 1st Instr Given | immediate Recall | Wait 5 days | Delayed recall | ||||
| APictograph | 2nd Instr Given | immediate Recall | Wait 5 days | Delayed recall | |||||
The subjects’ recall was scored by one of the authors (HK). Partial points were given when the subjects were able to recall part of an instruction item. Overall recall rate of a discharge instruction is calculated as the percentage of instruction items that were recalled correctly.
The effects of the version, cases, and the time lapse on the recall rates were tested with a linear mixed effect model where the instruction version, case, and the time when the recall rate was tested were set as fixed effect variables. Each respondent was set as a random effect variable and the recall rates was the response variable. This analysis was done using the proc mixed procedure with Statistical Analysis System (SAS) v9.1.
Results
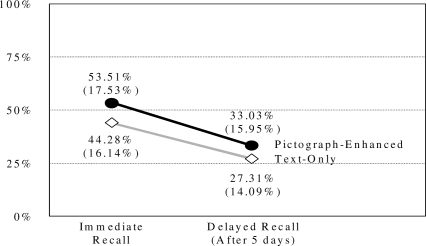
Both immediate and delayed recall rates were higher for the pictograph instruction. The mean recall rates and standard deviations are presented in Figure 2. We observed that on average, the subjects could only recall about half of the content immediately after reviewing the instructions, and less than a third 5 days later.
Figure 2.
Means and standard deviations (in parenthesis) of the immediate and delayed recall.
Mixed factor linear regression analysis found statistically significant effects (P < 0.001) of the version (text vs. pictograph) on the recall rate. This result suggests that the pictographs we developed are indeed effective in improving the recall of discharge instructions. As expected, the effect of time lapse between receiving and recalling the instructions was also statistically significant (P < 0.001). However, the effect of case (A or B) on the recall rate was not significant (p = 0.490).
Discussion
We have conducted a pilot study to develop pictographs for discharge instructions. Receiving proper discharge instruction has significant impact on patient outcome and satisfaction. One recent study analyzed the effect of JCAHO-required discharge instruction on heart failure patients. It found that patients who received all required instructions were significantly less likely to be readmitted for any cause and for heart failure than those who did not [14]. A large survey study also found that patients’ ratings of “instructions given about how to care for yourself at home” showed a strong, consistent positive relationship with overall patient satisfaction [7].
Clearly, discharge instructions should not only be given, but also be made comprehensible to patients and families. Unfortunately, patients often have difficulty understanding and remembering medical instructions. In a study of Emergency department (ED) discharge instructions, more than half of the patients did not fully comprehend the free text instructions they received [10]. According to another study, patients, on average, forget half of what they were told by a doctor within 5 minutes of leaving the outpatient consultation room [15].
In this pilot study, we developed a small set of pictographs through a participatory design process to supplement the free text discharge instructions. These pictographs were then used to enhance two mock-up discharge instructions. Tested on 13 healthy volunteers, the immediate and delayed recall rates were both higher for the pictograph enhanced instructions than the text only instructions. This suggests that pictographs could play an important role in improving the comprehension and recall of free text discharge instructions.
One lesson we learned from this study is the importance of involving both clinicians and lay people in the pictograph design process. The extensive bed-side and patient education experience of the two clinicians (nurses) who participated in the study were especially important in identifying instructions that could be improved with illustration and creating the initial designs. The two lay people who participated in the study contributed significantly to the critique of the initial designs, but made few suggestions as to what instructions should be illustrated and what the initial designs should look like. On one hand, maybe they did not make many suggestions because they were able to understand the instructions themselves and they did not have much experience explaining clinical instructions to others. On the other hand, if they did not understand the instructions themselves, they would not be able to help with creating the initial illustrations.
Recall is often used as a proxy for comprehension in research studies. Nevertheless, perfect comprehension does not always result in perfect recall. Even when a reader can understand the text, seeing a picture could help with recall. Some instructions (e.g. “Avoid tub bath until the wound is completely healed.”) should be comprehensible to most if not all of the subjects in our study. Nevertheless, seeing the picture in Figure 3, appeared to help some subjects remember the “avoid tub bath” instruction.
Figure 3.

Pictograph representation of the “Avoid tub bath” instruction.
For patients who have low health literacy or general English literacy, the benefit of pictographs could be even bigger. The sample size in our evaluation is too small and the sample is not diverse enough to test if the pictograph enhanced instructions would benefit a low literacy audience more. Past research, however, has indicated that graphical illustrations especially improve recall of conceptual knowledge and problem solving information of individuals who have little expertise in the subject matter [11].
In the study, the subjects’ unfamiliarity with and lack of personal interest in the specific medical condition might have lowered their recall rate. Delayed recall for real patients is probably higher if they try to comply with the instructions during the following days. A repeated measure with real patients might even induce higher recall rates the second time. On the other hand, unlike real patients, the healthy subjects were not suffering from any physical and emotional distress that would hinder the comprehension and recall of information. In the evaluation, the order of the versions (text and pictograph) was not randomized, which may cause carry-over effects. Because of the small sample size, we also did not analyze which pictographs or pictographs of which domains were particularly helpful.
In the future, we hope to develop a large set of pictographs and test them on actual discharge instructions of real patients. More importantly, we plan to develop a software tool that will be able to parse patient-specific instructions and enhance them with appropriate pictographs.
Conclusion
We conducted a pilot study to develop pictographs for discharge instructions through a participatory design process and test their efficacy in improving patient comprehension and recall. The pictograph enhancement resulted in better immediate and delayed recall rates. This suggests that we could improve patient comprehension and recall of discharge instructions by supplementing free texts with pictographs.
Acknowledgments
The authors thank the study participants. This work is supported by the NIH grant R01 LM07222, R01 DK75837.
References
- [1].JCI Accreditation Standards For Hospitals. Third Edition. The Joint Commission On Accreditation Of Healthcare Organizations; 2007. [Google Scholar]
- [2].Facts about ORYX® for Hospitals, Core Measures and Hospital Core Measures 2008 [cited 2008 Jan 24]; Available from: http://www.jointcommission.org/AccreditationPrograms/Hospitals/ORYX/oryx_facts.htm
- [3].Heng KW, Tham KY, How KY, Foo JS, Lau YH, Li AY. Recall of discharge advice given to patients with minor head injury presenting to a Singapore emergency department. Singapore medical journal. 2007 Dec;48(12):1107–10. [PubMed] [Google Scholar]
- [4].Spandorfer JM, Karras DJ, Hughes LA, Caputo C. Comprehension of discharge instructions by patients in an urban emergency department. Annals of emergency medicine. 1995 Jan;25(1):71–4. doi: 10.1016/s0196-0644(95)70358-6. [DOI] [PubMed] [Google Scholar]
- [5].Hwang SW, Tram CQ, Knarr N. The effect of illustrations on patient comprehension of medication instruction labels. BMC family practice. 2005 Jun 16;6(1):26. doi: 10.1186/1471-2296-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Clarke C, Friedman SM, Shi K, Arenovich A, Culligan C. Emergency department discharge instructions comprehension and compliance study. Cjem. 2005 Jan;7(1):5–11. doi: 10.1017/s1481803500012860. [DOI] [PubMed] [Google Scholar]
- [7].Clark PA, Drain M, Gesell SB, Mylod DM, Kaldenberg DO, Hamilton J. Patient perceptions of quality in discharge instruction. Patient Educ Couns. 2005 Oct;59(1):56–68. doi: 10.1016/j.pec.2004.09.010. [DOI] [PubMed] [Google Scholar]
- [8].Watt D, Wertzler W, Brannan G. Patient expectations of emergency department care: phase I -a focus group study. Cjem. 2005 Jan;7(1):12–6. doi: 10.1017/s1481803500012872. [DOI] [PubMed] [Google Scholar]
- [9].Ruland CM, Starren J, Vatne TM. Participatory design with children in the development of a support system for patient-centered care in pediatric oncology. J Biomed Inform. 2007 Nov 13; doi: 10.1016/j.jbi.2007.10.004. [DOI] [PubMed] [Google Scholar]
- [10].Austin PE, Matlack R, 2nd, Dunn KA, Kesler C, Brown CK. Discharge instructions: do illustrations help our patients understand them? Annals of emergency medicine. 1995 Mar;25(3):317–20. doi: 10.1016/s0196-0644(95)70286-5. [DOI] [PubMed] [Google Scholar]
- [11].Mayer RE, Gallini JK. When is an illustration worth ten thousand words? Journal of Educational Psychology. 1990;82(4):715–26. [Google Scholar]
- [12].Preiss B, Echave V, Preiss SF, Kaltenbach M. UVAL-MED a universal visual associative language for medicine. Proc Annu Symp Comput Appl Med Care. 1994:262–6. [PMC free article] [PubMed] [Google Scholar]
- [13].Payne TH, Martin DR. How useful is the UMLS metathesaurus in developing a controlled vocabulary for an automated problem list. Proc Annu Symp Comput Appl Med Care. 1993:705–9. [PMC free article] [PubMed] [Google Scholar]
- [14].VanSuch M, Naessens JM, Stroebel RJ, Huddleston JM, Williams AR. Effect of discharge instructions on readmission of hospitalised patients with heart failure: do all of the Joint Commission on Accreditation of Healthcare Organizations heart failure core measures reflect better care? Quality & safety in health care. 2006 Dec;15(6):414–7. doi: 10.1136/qshc.2005.017640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kitching JB. Patient information leaflets: the state of the art. J R Soc Med. 1990;83:298–300. doi: 10.1177/014107689008300506. [DOI] [PMC free article] [PubMed] [Google Scholar]