Abstract
This paper presents methods for generating nurse profiles using computerized documentation. NuProGen (Nurse Profile Generator), a custom-built knowledge discovery tool, enabled profile generation by calculating the numbers of various complicated patient cases (including high body mass index, bleeding, and multiple gestation) managed by each of 91 Labor and Delivery nurses at a single Intermountain Healthcare facility during the 3-month study period of January through March 2007. The tool identified patterns of documentation recorded by each nurse, as well as nursing care patterns associated with each of the three patient conditions examined in the study. Individual nurse profiles supported identification of expert and novice nurses corresponding to the management of specific conditions. A discussion of the benefits provided by available nurse profile data is also presented.
Introduction
Integration of structured documentation into computerized information systems (CISs) provides tremendous opportunities for improving clinical and administrative processes. Documentation of nursing activities, including the timing of task completion and information about the patient for whom nursing activities were performed, enables modeling and analysis of nursing practice patterns as well as support for management of nursing resources. Individual nurse profiles facilitate the automated pairing of expert nurses (experienced in managing specific patient conditions) with less experienced nurses, potentially aiding both patients and nurse staff. Informed nurse assignments provide patients with care from experienced providers while nursing staff expand competencies through exposure to complicated cases. Furthermore, tracking the clinical experiences of novice nurses could aid in orientation within the practice setting, supporting training and education objectives. Profiles that describe individual nurse behaviors enable a comparison of behaviors in managing similar patient cases. Last, nurse profiles, chronicling details of patient level interactions, potentially support adjustment of reimbursements for nursing intensity1 and facilitate analysis of nursing care effects on individual patient outcomes.
Many investigators responded to the call from the Institute of Medicine (IOM) requesting empirical evidence demonstrating the effects of nurse staffing and mix on patient outcomes2 by publishing research where representations of nursing care were based on measured nurse-to-patient ratios. Though some studies established correlations between nurse staffing rates and patient outcomes at a unit-wide level, those studies did not measure the amount of nursing care received by individual patients.3,4 At least one other study failed to establish any correlation between nurse staffing rates and patient outcomes.5 Strategies for measuring nursing care resources at the unit or hospital level may help to identify available nursing resources; however, they do not capture the quantity or quality of nursing care interactions at the patient level, nor do they account for variation in the distribution of nursing resources according to patient acuities. Many of the studies conducted in response to the IOM call relied on administrative data, which have been identified as poor measurements of complications, in the analysis of patient outcomes.6 Thus, although there is evidence to support an association between nurse staffing and outcomes, results are still inconclusive.7
In a previous study, we developed a patient profiling mechanism supporting forecasting of statistically-likely outcomes based on cases from patients sharing similar attributes and clinical conditions.8 In a continuation of the study, representations of the quantity of nursing care received at the individual patient level were derived from electronic point-of-care nursing documentation.9 Quantified care scores supported an analysis of relationships among patient attributes, care processes, and patient outcomes.
The present study expanded on previous findings by demonstrating methods for generating nurse profiles using a custom-built software application. The resulting profiles provided a ranking of nurses according to the number of complication-specific cases managed during a 3-month study period. The profiles also supported a comparison of individual nurses’ documentation activity patterns with those of other nurses in the same care unit.
Methods
A retrospective, descriptive analysis was performed, which included 739,675 documented nursing events generated by 91 nurses for 1,084 Labor and Delivery (L&D) patients (no exclusions). The data were generated at a single facility during the 3-month period of January through March 2007. The institutional review boards at the University of Utah and Intermountain Healthcare approved the project, and a waiver of informed consent was obtained.
In 2007, Intermountain Healthcare provided medical and nursing care to approximately 30,000 L&D patients in Utah and Southern Idaho. The Labor and Delivery CIS (Storkbytes™, Intermountain Healthcare, Salt Lake City, UT), installed at 15 Intermountain facilities, combined automatic fetal monitor measurements with computerized nurse charting.10 Deployed in the 1980s, the CIS has undergone iterative modifications in response to ongoing feedback from clinical users. The L&D Nursing Standards and Education work group of Intermountain’s Women and Newborn Clinical Program has provided ongoing validation and refinement of the nurse documentation elements to ensure that the system has accurately represented nursing care processes. Also, documentation of procedures and supplies has reduced variability in charge capture by automating the billing process.11 The CIS provided a menu-driven interface allowing structured documentation of nursing interventions and observations (2,552 such concepts were supported). Metadata were recorded with each data point identifying the documenting nurse, the time of documentation, and the time that the nursing activity occurred. Data recorded within the CIS were extracted to Intermountain Healthcare’s enterprise data warehouse and retrieved for study analysis.
According to recommendations from clinical domain experts, three patient conditions were selected to support nurse profile generation. These included multiple gestation patients, patients that required bleeding management, and patients with a high body mass index (BMI). For classifying patient conditions, specific thresholds for bleeding and BMI were adjusted to user-specified clinically appropriate values. By default, standard categories of BMI for non-pregnant patients were used, where a BMI of 30.0 – 34.9 kg/m2 signified obesity, and a BMI > 35 kg/m2 indicated morbid obesity. Nurse documentation data were retrieved and processed by a custom-developed object-oriented application.
Each nursing event was comprised of a de-identified patient identifier, a nurse identifier, a flag indicating multiple gestation status, a coded representation of the event type, and event details. For example, a documentation event might appear as follows:
“72”, “9”, “1”, “AGG102” (patient height), “Height 64 in. (163 cm)”
While parsing documentation events, the Nurse Profile Generator (NuProGen) application managed information by instantiating and updating objects for each unique patient and nurse. Patient objects contained a patient identifier, values for total blood loss, height, weight, and calculated BMI, and Boolean values signifying whether or not the patient met each of the three selected clinical criteria. Additionally, counts of each event type documented for the patient were stored, as was a list of nurse identifiers associated with the patient. Each Nurse object contained a unique nurse identifier, and counts of the number of bleeding, high BMI, and multiple gestation patients managed by that nurse. Also, the object contained complete lists of patients managed and events documented by the nurse.
Following the processing of documentation events, the user could enter thresholds for determining patient inclusion in the bleeding and high BMI categories. User selection of which of the three conditions to review prompted NuProGen to refresh patient inclusion status according to the threshold specified in the application interface. For each nurse, a count of patients meeting each clinical criterion was tabulated using the nurse’s list of patients and the patient status indicated in each Patient object. NuProGen ranked the nurses by the number of patients with the selected condition whom they managed during the 3-month study period. NuProGen also ranked by frequency the type of nursing care events documented for patients with the selected condition. To review the documentation pattern of a specific nurse, the tool enabled the user to specify a nurse identifier. The events documented by that nurse were ranked and displayed from most to least frequent. Also listed was a mean per patient calculation of each event type documented by the specified nurse along with a mean per patient calculation of the event type as documented by all of the nurses in the study.
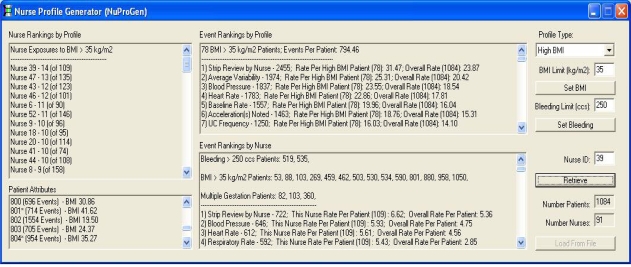
As an example (see Figure 1), to review high BMI patients, a high BMI threshold of 35 kg/m2 was entered into the NuProGen user interface, and the application automatically performed the analysis based on the classification. In this example, it was easy to discover that nurse 39 managed 14 patients with BMI > 35 kg/m2 during the study period. Nurse 47 managed 13 patients with BMI > 35kg/m2, two nurses (43 and 46) managed 12 patients with BMI > 35 kg/m2, and so forth. NuProGen identified 78 patients meeting the high BMI criteria during the analysis period. For the 78 patients, “Strip Review by Nurse” (review of fetal monitor data) was the most common event documented at 31.5 times per high BMI patient compared to 23.9 times for the entire patient population. Calculations of the other documented events were likewise displayed.
Figure 1.
Interface for the NuProGen application displaying nurses, patients, and documentation patterns associated with a user-specified BMI threshold of 35 kg/m2.
The user could select individual nurses for further information. Following summary counts of the numbers and types of patients managed by the nurse was a ranked list of activities which the nurse documented. For example, the most common event documented by nurse 39 was “Strip Review by Nurse” at a rate of 6.6 times per patient compared to 5.4 times per patient by the overall nurse population. Nurse profiles were generated for each of the 91 nurses in the study and were displayed by specifying the corresponding nurse identifier.
Results
Tables 1–3 present the number of nurses that managed various numbers of patient cases with each of the three investigated clinical conditions. For high BMI and bleeding, the tables are further stratified by the degree of the condition. Of the 91 nurses in the study, 18 (19.8%) had no exposure to the 78 patients with BMI > 35 kg/m2 and 35 (38.5%) of the nurses had no exposure to the 26 patients with BMI > 40 kg/m2. Over one quarter (24) of the nurses had no exposure managing the 75 patients with bleeding > 100 ccs. Nearly half (45) of the nurses had no exposure managing the 13 patients with bleeding > 500 ccs. Of the 91 nurses in the study, 63 (69.3%) managed at most one of the 24 multiple gestation patients treated during the study period with 42 of those nurses (46.2%) managing no multiple gestation patients.
Table 1.
The number of nurses managing various numbers and degrees of patients with high BMI.
| Encounters with High BMI Patients | Number of Nurses (Percentage of Total %)
|
|||||
|---|---|---|---|---|---|---|
| > 35 kg/m2 (78 Patients) | > 40 kg/m2 (26 Patients) | > 45 kg/m2 (6 Patients) | ||||
| 0 | 18 | (19.8) | 35 | (38.5) | 67 | (73.6) |
| 1 | 13 | (14.3) | 21 | (23.1) | 20 | (22.0) |
| 2 | 10 | (11.0) | 13 | (14.3) | 4 | (4.4) |
| 3 | 6 | (6.6) | 8 | (8.8) | – | |
| 4 | 4 | (4.4) | 12 | (13.2) | – | |
| 5 | 8 | (8.8) | – | – | ||
| 6 | 10 | (11.0) | 2 | (2.2) | – | |
| 7 | 7 | (7.7) | – | – | ||
| 8 | 2 | (2.2) | – | – | ||
| 9 | 2 | (2.2) | – | – | ||
| 10 | 5 | (5.5) | – | – | ||
| 11 | 2 | (2.2) | – | – | ||
| 12 | 2 | (2.2) | – | – | ||
| 13 | 1 | (1.1) | – | – | ||
| 14 | 1 | (1.1) | – | – | ||
Table 3.
The number of nurses managing various numbers of multiple gestation patients.
| Encounters with Multiple Gestation Patients | Number of Nurses (Percent of Total %)
|
|
|---|---|---|
| (24 Patients) | ||
| 0 | 42 | (46.2) |
| 1 | 21 | (23.1) |
| 2 | 12 | (13.2) |
| 3 | 9 | (9.9) |
| 4 | 5 | (5.5) |
| 5 | 2 | (2.2) |
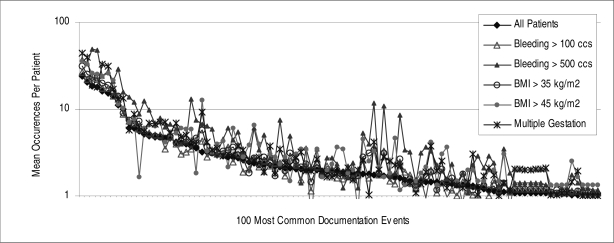
Figure 2 shows the calculated mean number of times per patient that the 100 most common events were documented for various patient subgroups. Table 4 presents details of the ten most common activities documented for each of the subgroups represented in Figure 2.
Figure 2.
Logarithmic representation of the mean number of times that each of the 100 most common documented events was performed for various patients subgroups.
Table 4.
The rank and mean number of times that common events were documented for various patient subgroups.
| Documented Event | Mean Times Documented Per Patient (Rank Within Patient Subgroup) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Patients (1,084 patients) | Bleeding > 100 ccs (53 patients) | Bleeding > 500 ccs (13 patients) | BMI > 35 kg/m2 (78 patients) | BMI > 45 kg/m2 (6 patients) | Multiple Gestation (24 patients) | |||||||
| All Events | 682.4 | -- | 735.8 | -- | 1170.9 | -- | 794.5 | -- | 941.5 | -- | 897.5 | -- |
| Strip Reviewed by Nurse | 23.9 | (1) | 28.9 | (1) | 37.8 | (3) | 31.5 | (1) | 36 | (1) | 44.5 | (1) |
| Average Variability | 20.4 | (2) | 24.0 | (4) | 33.9 | (4) | 25.3 | (2) | 33 | (2) | 39.1 | (2) |
| Blood Pressure | 18.5 | (3) | 26.0 | (2) | 48.9 | (1) | 23.6 | (3) | 26 | (3) | 18.8 | (5) |
| Heart Rate | 17.8 | (4) | 24.8 | (3) | 47.6 | (2) | 22.9 | (4) | 25.3 | (5) | 18.1 | (6) |
| Baseline Rate | 16.0 | (5) | 18.8 | (6) | 24.0 | (7) | 20.0 | (5) | 24.2 | (6) | 33.2 | (3) |
| Acceleration(s) Noted | 15.3 | (6) | 19.0 | (5) | 27.3 | (6) | 18.8 | (6) | 25.8 | (4) | 31.3 | (4) |
| Uterine Contraction Frequency | 14.1 | (7) | 14.6 | (8) | 20.8 | (8) | 16.0 | (7) | 21.5 | (7) | 16.8 | (7) |
| Respiratory Rate | 11.0 | (8) | 15.6 | (7) | 29.0 | (5) | 14.0 | (8) | 11.3 | (9) | 13.0 | (9) |
| Uterine Contraction Duration | 9.9 | (9) | 10.5 | (9) | 15.5 | (9) | 9.0 | (9) | 10.2 | (10) | 13.5 | (8) |
| Temperature | 6.1 | (10) | 7.9 | (11) | 13.8 | (10) | 7.4 | (10) | 7.2 | (12) | 5.7 | (18) |
Discussion
As demonstrated by Figure 2, the patterns of nursing activities performed for patients varied depending on the specific conditions being managed. Though rankings of the most common events were relatively consistent across patient subgroups, the mean number of times each event was documented varied by condition. Also, more variation existed between the rates and rankings of moderately common events. In particular, the patterns associated with multiple gestation patients and patients with bleeding > 500 ccs (cubic centimeters) had large deviations in the number of times that various activities were documented as compared to those corresponding to the overall patient set. Documentation patterns generated collectively by the unit also provide a useful point of reference for individual nurses.
Calculating the number and type of patient cases managed by each nurse within a timeframe has a number of potential uses. The results shown in Tables 1–3 indicated that during the 3-month study period a large percentage of nurses did not have experience managing the selected conditions. Individual patient needs dictate that when providing care to patients with complicated cases, nurses should have recent experience managing similar conditions.
A scheduling system could assist in ensuring that during any given shift, nurse staff were collectively experienced in managing a variety of complicated cases. In a real-time environment, a nurse management system could inform nurse assignments. Nurse managers could identify available nurses having recent experience managing patients with a particular condition as well as those nurses that could benefit from an assignment to a patient with a condition they had not recently managed. Pairing a nurse experienced in managing a specific condition with a nurse who has not had recent experience managing that condition potentially offers benefits to both the nursing staff and the patient – the novice nurse gains exposure to a particular condition while the patient benefits by receiving care from an experienced provider. This may be particularly valuable for nurse residency programs in maternal-child nursing, and in planning unit-based education.
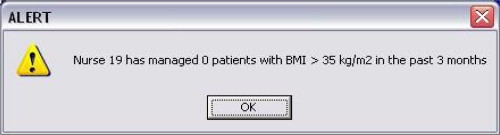
During the assignment of a nurse with little recent experience managing a specific patient condition, an alert could be issued (see Figure 3). The alert could be customized with a condition specific minimum patient number threshold for which to inform the nurse manager. Additionally, the timeframe used to calculate the number of exposures could be lengthened or shortened depending on the requirements of a particular unit.
Figure 3.
Example nurse management system alert.
In a research setting, a measurement of nurse experience would support an analysis of relationships between nursing care and patient outcomes. Adjusting the quantity of individual nurse contributions (as generated in previous efforts using the same data source9) with an experience-based weight potentially supports more accurate analysis of the effects of nursing care on patient outcomes.
The current analysis was limited by not considering the mix of nurses represented by the information system. Though over 90% of the CIS users were Registered Nurses the analysis could benefit from studying variations in activities according to the nurse’s level of training and education. Future efforts will focus on integrating these details into the NuProGen analysis tool calculations.
Conclusion
This paper introduced NuProGen, a knowledge discovery tool that generated nurse profiles from computerized nurse documentation. Analysis of profiles relating to three patient conditions demonstrated variability in the experiences of individual nurses. Also, the paper discussed potential benefits of integrating nurse profile data into real-time scheduling and management systems.
Table 2.
The number of nurses managing various numbers and degrees of patients with bleeding.
| Encounters with Bleeding Patients | Number of Nurses (Percentage of Total %)
|
|||||
|---|---|---|---|---|---|---|
| > 100 ccs (75 Patients) | > 250 ccs (23 Patients) | > 500 ccs (13 Patients) | ||||
| 0 | 24 | (26.4) | 38 | (41.8) | 45 | (49.5) |
| 1 | 13 | (14.3) | 25 | (27.5) | 26 | (28.6) |
| 2 | 10 | (11.0) | 8 | (8.8) | 10 | (11.0) |
| 3 | 11 | (12.1) | 5 | (5.5) | 5 | (5.5) |
| 4 | 5 | (5.5) | 8 | (8.8) | 4 | (4.4) |
| 5 | 3 | (3.3) | 5 | (5.5) | 1 | (1.1) |
| 6 | 2 | (2.2) | 2 | (2.2) | – | |
| 7 | 8 | (8.8) | – | – | ||
| 8 | 3 | (3.3) | – | – | ||
| 9 | 1 | (1.1) | – | – | ||
| 10 | 5 | (5.5) | – | – | ||
| 11 | 1 | (1.1) | – | – | ||
| 12 | 1 | (1.1) | – | – | ||
| 15 | 1 | (1.1) | – | – | ||
| 16 | 1 | (1.1) | – | – | ||
| 18 | 1 | (1.1) | – | – | ||
| 20 | 1 | (1.1) | – | – | ||
Acknowledgments
This research was funded under National Library of Medicine Training Grant No. 1T15LM07124-08.
References
- 1.Welton JM, Zone-Smith L, Fischer MH. Adjustment of inpatient care reimbursement for nursing intensity. Policy Polit Nurs Pract. 2006;7(4):270–80. doi: 10.1177/1527154406297510. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Washington, DC: National Academy Press; 1996. Nursing staff in hospitals and nursing homes: Is it adequate? [PubMed] [Google Scholar]
- 3.McGillis Hall L, Doran D, Pink GH. Nurse staffing models, nursing hours, and patient safety outcomes. J Nurs Adm. 2004;34(1):41–5. doi: 10.1097/00005110-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346(22):1715–22. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 5.Bolton LB, Jones D, Aydin CE, Donaldson N, Brown DS, Lowe M, et al. A response to California's mandated nursing ratios. J Nurs Scholarsh. 2001;33(2):179–84. doi: 10.1111/j.1547-5069.2001.00179.x. [DOI] [PubMed] [Google Scholar]
- 6.Lawthers AG, McCarthy EP, Davis RB, Peterson LE, Palmer RH, Iezzoni LI. Identification of inhospital complications from claims data. Is it valid? Med Care. 2000;38(8):785–95. doi: 10.1097/00005650-200008000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Needleman J, Buerhaus P. Nurse staffing and patient safety: current knowledge and implications for action. Int J Qual Health Care. 2003;15(4):275–7. doi: 10.1093/intqhc/mzg051. [DOI] [PubMed] [Google Scholar]
- 8.Hall ES, Thornton SN. Extracting nursing practice patterns from structured labor and delivery data sets; AMIA Annu Symp Proc; November 10–14; Chicago, IL. 2007. [PMC free article] [PubMed] [Google Scholar]
- 9.Hall ES, Poynton MR, Narus SP, Thornton SN.Modeling the distribution of nursing effort using structured labor and delivery documentation J Biomed Inform 2008April20[Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Twede M, Gardner RM, Hebertson RM. A PC-based system for intrapartum monitoring. Contemporary OB/GYN “Special Issue -- Technology 1985”. 1984;24:13–17. [Google Scholar]
- 11.Thornton SN, Yu H, Gardner RM. Using point of service clinical documentation to reduce variability in charge capture. AMIA Annu Symp Proc; 2002 November 9–13; San Antonio, TX. 2002. pp. 782–6. [PMC free article] [PubMed] [Google Scholar]