Abstract
The MidSouth e-Health Alliance is a health information exchange that has been in use in the Memphis, Tennessee region since May, 2006. This health information exchange took two years to develop from the time it was initially conceived. Following on the work done by the Indianapolis project, the MidSouth e-Health Alliance focused initially on implementations in emergency departments throughout this region. A total of 321 clinicians have used the system in the 5 emergency departments since s initial deployment. This paper reports on the processes users are engaged in to use the system as well as the demographics and patient characteristics associated with system use to date.
Background
Health Information Exchange systems have been in place since the early 1990’s beginning with John A. Hartford Foundation’s Community Health Management Information Network (CHIN).1 Over the past decade, these efforts to make data accessible from disparate healthcare settings have enjoyed increasing momentum, only to lose it again until recently. Researchers have evaluated the failures of CHINs and attributed them to organizational, rather than technical challenges.1–3 Beginning in 2002, with funding from non-profit and federal groups, numerous groups began to construct regional health information organizations (RHIOs) to support health information exchange (HIE) within a particular geographic community. In 2004, the State of Tennessee and the Agency for Healthcare Research and Quality funded Vanderbilt University to assist a tri-county area in southwest Tennessee with the development of a RHIO and health information exchange application. Over the ensuing three years, substantial progress was made garnering participation from key regional and statewide stakeholders to share their patient care data through a central, sharable resource. In addition to that work, a team leveraged an existing electronic health record from Vanderbilt University to implement a health information exchange system application in regional emergency departments, based on their established need for patient information generated in other care settings4–7. Five core entities contributing data from 14 organization in the region initially provided data to the HIE application, with other entities committed to participating in data sharing soon thereafter. After significant work was done from the organizational and transformational perspectives, as noted by Frisse,8 the system known as the MidSouth e-Health Alliance (MSeHA) was formed and went live for use in emergency departments in May, 2006. As a part of our evaluation of this system, our team has been interested in the overall and site-specific adoption of the system, as well as the impact users of the system believe it is having. Following a framework that was outlined by Johnson and colleagues9, we report on our overall usage and qualitative results to date.
Materials and Methods
The MSeHA is an operational HIE in the southwest region of Tennessee. A Board of Directors, consisting of members from each of the major health care systems in the area, as well as representatives from other important stakeholders in the community and from Vanderbilt, has guided the organization, development, and implementation of the HIE. The Board continues to oversee its strategic and operational missions. The MSeHA covers an area in which approximately 2 million individuals reside. MSeHA relies on HL7 data streams from 9 hospitals, 15 ambulatory clinics, and the University of Tennessee Medical Group. Examples of patient data being exchanged are demographics, ICD-9 discharge codes, lab results, encounter data, and dictated reports. Each hospital organization’s data are stored in a specific “vault” under its control. Record locator algorithms are used to identify records belonging to the same putative patient across all vaults whenever a particular patient record is queried. Access to these data is provided using a combination of a secure token and user ID/password combination. Patients have the ability to opt-out of this system, in which case no record for the patient will be found. All access and activity is logged.
The primary goal of this phase of the MSeHA evaluation was to assess the overall usage pattern, the characteristics of users of the system and environments in which the MSeHA has been deployed. Multiple data sources were used for this analysis, including user activity logs (i.e., login, logoff, record search, and record access), patient demographics, and clinical data message logs. Log entries were joined to assess the number of records accessed, the number of visits where records were viewed in detail, and the source of data for each patient (contributions of each site to the overall record for the patient.) We also analyzed login data to ascertain the number of active users who are logging in each month, the number of patient visits that were being accessed each month and some characteristics of the visits for each month. Data were summarized and analyzed in Excel 2007 using descriptive techniques.
In addition, at each site a campaign called “What Song Are You Singing?” was employed to encourage voluntarily reporting of both positive and negative aspects of the system (“rockin an’ rollin” vs. “singing the blues”). Each month, cards and emails containing feedback were collected from all of the sites and analyzed systematically by one of the investigators (KBJ).
Results
Data are being exchanged at the rates described in Table 1. An average of 80 million laboratory data elements are being exchanged daily.
Table 1.
Current Data Exchange Rates
| Total patients in system | 1.32 million total |
| Encounter records | 2.1 million total |
| New laboratory data | Averaging 80,000 lab messages received daily |
| New radiology reports | Averaging 1,200 per day |
| New discharge summaries | Averaging 150 per day |
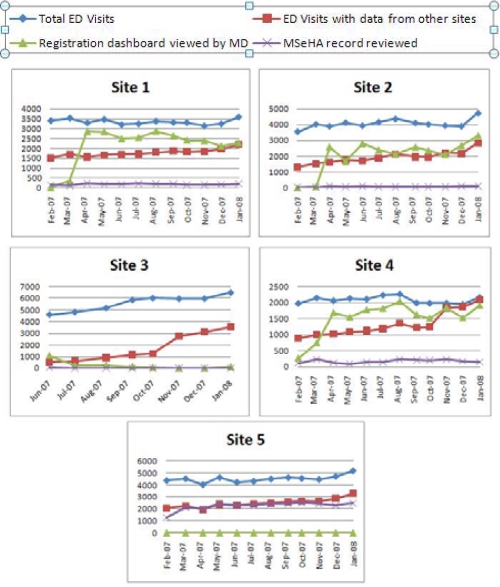
After 12 months of use, stable usage patterns emerged for all of the original five sites. Those data are presented in Figure 1. Site 5 is unique among our initial sites and merits some explanation. Their data feeds were the first full set data feeds received into the HIE. Following the Board’s promise of low cost to participate, Baptist agreed to send a daily batch file to the exchange. The file contained all registrations (minus opted-out records), laboratory tests, radiology reports, and transcribed reports for the day. Subsequent to this work, all other sites provided a real-time feed of registration data, in addition to other shared data elements. Because the data feed from Baptist was up to a day old, when a special dashboard view, known as the recent registration screen was designed and rolled out in April of 2007, Baptist was not able to use it and had to resort to a more labor intensive protocol for their registrars.
Figure 1.
Site Usage Summary Trends
In each Emergency Department (ED), MSeHA was used for an average of 3% of all visits, and for approximately 10% of visits with recent data from another site. Site 5 had a much higher rate of access, but uses a protocol driven by registrars to lookup each patient who registers in their ED. Site 3, which had an almost exclusively pediatric population, has the lowest level of access of the system. Table 3 breaks down each site’s use of the system according to the extent of data in the system about the patient.
Table 3.
Breakdown of Site Use by Data Exchange Coverage
| Site | Visits | Ratio of reviewed visits over total in demographic group (%) | |||
|---|---|---|---|---|---|
| Not seen before at any sites | Seen exclusively at this site | Seen only at other sites | Seen at this and other sites | ||
| Site 1 | 3586 | 40/1366 (2.9%) | 43/888 (4.8%) | 45/582 (7.7%) | 75/750 (10%) |
| Site 2 | 4734 | 14/1463 (1%) | 8/1214 (0.7%) | 30/759 (4%) | 34/1298 (2.6%) |
| Site 3 | 6515 | 2/2668 (0.1%) | 1/3026 (0%) | 0/273 (0%) | 0/548 (0%) |
| Site 4 | 2166 | 34/682 (5%) | 36/483 (7.5%) | 30/347 (8.6%) | 47/654 (7.2%) |
| Site 5 | 5193 | 426/2134 (20%) | 738/1205 (61.2%) | 246/817 (30.1%) | 891/1037 (85.9%) |
The overall number of active users and overall percentage of total available users are displayed in Table 4. This table considers an active user any person who has access to the MSeHA system and has logged in for any reason during that month. On average, 34% of the physician base and 6% of their nurse base uses the system any given month. Site 1 has a large number of nurses using the system—nurses at this site access the system during the triage process based upon whether the patient states that he or she has been seen at any other area facility recently.
Table 4.
Summary of Active Users
| Sites | Roles | Percent of Total Users who logged in at least once | Total Users | |||||
|---|---|---|---|---|---|---|---|---|
| Aug-2007 | Sep-2007 | Oct-2007 | Nov-2007 | Dec-2007 | Jan-2008 | |||
| Site 1 | Nurse | 44% | 38% | 36% | 49% | 38% | 41% | 39 |
| Physician | 42% | 46% | 42% | 29% | 38% | 33% | 24 | |
| Site 2 | Nurse | 0% | 0% | 8% | 13 | |||
| Physician | 57% | 52% | 43% | 48% | 52% | 48% | 21 | |
| Site 3 | Nurse | 12% | 6% | 6% | 12% | 6% | 6% | 17 |
| Physician | 12% | 4% | 4% | 0% | 0% | 8% | 26 | |
| Site 4 | Physician | 50% | 31% | 50% | 56% | 63% | 56% | 16 |
| Registrar | 13% | 27% | 27% | 20% | 13% | 13% | 15 | |
| Site 5 | Nurse | 3% | 6% | 6% | 3% | 6% | 6% | 32 |
| Physician | 46% | 46% | 50% | 58% | 42% | 35% | 26 | |
| Registrar | 66% | 71% | 66% | 58% | 50% | 61% | 38 | |
| Unit Clerk | 75% | 75% | 75% | 63% | 50% | 63% | 8 | |
Qualitative data from each site outline many of the potential advantages and disadvantages to the system. Table 5 summarizes many of the themes associated with qualitative results. The majority of qualitative reports cite avoiding duplicate testing and obtaining medication history as noteworthy comments. Comment cards also cite the potential for biosurveillance and identification of specific patient groups (especially patients with chronic pain and factitious disorder). A general theme has been a decrease in redundant tests as well as an increase in awareness of patients who have frequent visits to emergency departments as a result of using the system.
Table 5.
Themes of Received Comments
| Comment Category | Number of Reports |
|---|---|
| Duplicate testing | 17 |
| Med history | 9 |
| Usability | 6 |
| Discharge decision | 3 |
| Downtime | 3 |
| Missing information | 2 |
| Enhancements | 1 |
| Praise | 1 |
| Biosurveillance | 1 |
| Treatment history | 1 |
| Grand Total | 44 |
Discussion
Operational health information exchange systems are functional byproduct of three environmental attributes: a capable technologic infrastructure, a culture interested in data exchange, and a respected team with appropriate expertise supporting the implementation. The MidSouth e-Health Alliance has now been available to clinicians for over a year. The data described in this paper represent very early and encouraging system use. The overall 3% rate of use for all visits includes patients who have no data in the system, patients who have most of their data in the local electronic health record, and patients whom the ED clinician may believe have chief complaints that do not require additional data to manage safely. It is not yet clear what level of use will achieve maximum benefit. For example, our current approach provides a “dashboard” view that identifies which patients have data from other sites. It is possible that given the current patterns of use, clinicians are able to decide from that screen when it is worth reviewing a record in detail—in which case actual use is underestimating the benefit substantially.
We have increasing evidence that there may be enhanced user interface functionality that may help providers more readily identify specific populations of patients who would benefit from having their records reviewed. For example, although it is uncommon for a patient with straightforward trauma to have their health record reviewed in a health information exchange system, the potential for that patient to have a clinically significant disease such as physical abuse, rather than accidental trauma, could be high. It would be easy for a system containing all visits to all other emergency departments and primary care facilities, as well as all prior radiology reports, to provide a window into the potential for a particular trauma patient to have risk factors for non-accidental trauma.
Qualitative data from the “What Song Are You Singing” Campaign suggests users perceive the system is impacting patient care in the tri-county region by decreasing duplicate tests and improving the awareness of patients who are frequent visitors of emergency departments despite having legitimate medical homes. The availability of HIE – like CPOE – is necessary but not sufficient for achieving certain care improvements. The challenge lies in understanding how such systems can best be incorporated into workflow and used. We believe that the data we have so far, as well as plans for additional analysis, support new initiatives in the tri-county region aimed at improving patient care.
We are heartened by the results of the health information exchange thus far. These results suggest to us a foundation from which we can improve adoption and improve the overall health of the region. Additional work to demonstrate value and sustainability is underway and additional deployment of the system to additional primary care sites and other sites in the region, as directed by our Board, are being planned.
Conclusion
The MidSouth e-Health Alliance reports an approximately 3% level of access of patient records in its first year with an increasing availability of data for each of these patients and a high level of satisfaction for the system used to access these records. Additional efforts are underway to better understand the impact of the system on the health of the Memphis, Tennessee region.
Table 2.
MSeHA Use Summary by Site, January 2008
| Site | Visits | Visits Reviewed | (%) | Other Site Data <= 30 days old | Reviewed Other Site data | (%) |
|---|---|---|---|---|---|---|
| Site 1 | 3586 | 203 | 5.7% | 638 | 85 | 13% |
| Site 2 | 4734 | 86 | 1.8% | 779 | 56 | 7% |
| Site 3 | 6515 | 3 | < 0.05% | 242 | 0 | 0% |
| Site 4 | 2166 | 163 | 8% | 512 | 66 | 13% |
| Site 5 | 5193 | 2581 | 50% | 1130 | 669 | 59% |
| TOTAL (excl. Site 5) | 17001 | 455 | 2.6% | 2171 | 207 | 9.5% |
Acknowledgments
Funding for this project has been obtained through AHRQ Contract 290-04-0006; the State of Tennessee; and Vanderbilt University.
References
- 1.Lorenzi NM, Rosenbloom ST.Strategies for creating successful local health information infrastructure initiatives. In: Services USDoHaH, ed; 2003
- 2.Brennan PF, Schneider SJ, Tornquist EM. Information networks for community health. New York: Springer; 1997. [Google Scholar]
- 3.Hanlon PI. Charting the evolution of community health information networks. Healthc Inf Manage. 1995 Spring;9(2):9–14. [PubMed] [Google Scholar]
- 4.Finnell JT, Overhage JM, McDonald CJ. In support of emergency department health information technology. AMIA Annu Symp Proc. 2005:246–250. [PMC free article] [PubMed] [Google Scholar]
- 5.Finnell JT, Overhage JM, Dexter PR, Perkins SM, Lane KA, McDonald CJ. Community clinical data exchange for emergency medicine patients. AMIA Annu Symp Proc. 2003:235–238. [PMC free article] [PubMed] [Google Scholar]
- 6.Overhage J, McDonald CJ, Suico JG. The Regenstrief medical record system 2000: Expanding the breadth and depth of a community wide EMR. Proc AMIA Symp. 2000:1173. [PMC free article] [PubMed] [Google Scholar]
- 7.Overhage JM, Dexter PR, Perkins SM, et al. A randomized, controlled trial of clinical information shared from another institution. Ann Emerg Med. 2002 Jan;39(1):14–23. doi: 10.1067/mem.2002.120794. [DOI] [PubMed] [Google Scholar]
- 8.Frisse ME. State and community-based efforts to foster interoperability. Health Aff (Millwood) 2005 Sep-Oct;24(5):1190–1196. doi: 10.1377/hlthaff.24.5.1190. [DOI] [PubMed] [Google Scholar]
- 9.Johnson KB, Gadd C. Playing smallball: approaches to evaluating pilot health information exchange systems. J Biomed Inform. 2007 Dec;40(6 Suppl):S21–26. doi: 10.1016/j.jbi.2007.08.006. [DOI] [PubMed] [Google Scholar]