Abstract
One of the essential ingredients for health information technology implementation is a well-trained and competent workforce. However, this workforce has not been quantified or otherwise characterized well. We extracted data from the HIMSS Analytics™ Database and extrapolated our findings to the US as a whole. We found that there are approximately 108,390 IT professionals in health care the US. In addition, the amount of IT staff hired varies by level of EMR adoption, with the rate of IT FTE per bed started at a level of 0.082 FTE per bed at the lowest level of the EMR Adoption Model (Stage 0) and increasing to 0.210 FTE bed at higher levels (Stage 4). We can extrapolate nationally to conclude that to move the entire US to higher levels of adoption (Stage 4) will require an additional 40,784 IT professionals. There are limitations to this analysis, including that the data are limited to IT professionals who are mainly in hospitals and do not include those who, for example, work for vendors or in non-clinical settings. Furthermore, data on biomedical informatics professionals are still virtually non-existent. Our analysis adds to data that show there must be increasing attention paid to the workforce that will develop, implement, and evaluate HIT applications. Further research is essential to better characterize all types of workers needed for adoption of health information technology, including their job roles, required competencies, and optimal education.
Introduction
Despite calls for wider use of health information technology (HIT) to improve health, health care, public health, and biomedical research [1, 2], there are still barriers to its adoption, such as mismatch of return on investment between those who pay and those who benefit, challenges to workflow in clinical settings, lack of standards and interoperability, and concerns about privacy and confidentiality [3, 4]. Another barrier, lesser studied and quantified but increasingly recognized, is the lack of characterization of the workforce and its training needed to most effectively implement HIT systems [5–7]. We know surprisingly little about the HIT workforce, as most research assessing it has looked only at specific settings or professional groups.
Probably the most comprehensive assessment of the HIT workforce has been carried out in England [8]. An assessment of the English HIT workforce estimated the employment of 25,000 full-time equivalents (FTEs) out of 1.3 million workers in National Health Service (NHS). This equated to the employment of about one information technology (IT) staff per 52 non-IT workers. The workers were found to be distributed among information and communication technology staff (37%), health records staff (26%), information management staff (18%), knowledge management staff (9%), senior managers (7%), and clinical informatics staff (3%).
Most studies done in the United States (US) have focused on one group in the workforce, such as IT or health information management (HIM) professionals. To our knowledge, no studies have quantified numbers of “informaticians,” although some studies have qualitatively assessed certain types, such as Chief Medical Information Officers [9, 10]. Gartner Research has assessed IT staff in integrated delivery systems of varying size [11]. Among 85 such organizations studied, there was a consistent finding of about one IT staff per 56 non-IT employees, which was similar to the ratio noted above in England. The major roles for IT staff were listed as programmer/analyst (51%), support (28%), telecommunications (16%).
Another large-scale study has assessed HIM professionals in the US, finding that the primary work setting for these individuals was hospital inpatient (53.4%), hospital outpatient (7.8%), physician office/clinic (7.2%), and consulting firm (4.2%) [12]. For those involved in EHR implementation, two-thirds were on the planning team and half were on implementation team. Study respondents indicated that the largest need for more education was in areas of IT, legal and regulatory issues, reimbursement methodologies, and healthcare information systems.
An additional workforce study has focused on a specific HIT application, estimating the workforce necessary to deploy a Nationwide Health Information Network (NHIN) in the US. [13]. For a five-year implementation time frame, there would be an estimated need for 7,600 FTE for installation of EHRs for 400,000 practicing physicians who do not currently have them, 28,600 FTE for the 4,000 hospitals that do not have EHRs, and 420 FTE to implement the infrastructure to connect the network.
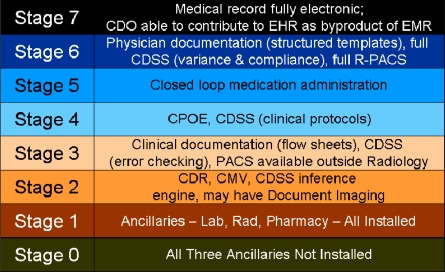
Another view of the HIT workforce can be obtained from the HIMSS Analytics Database (derived from the Dorenfest IDHS+ Database™, http://www.himssanalytics.com). This database contains self-reported data from about 5,000 US hospitals, including elements such as number of beds, total staff FTE, total IT FTE (as well as broken down by major IT job categories), applications, and the vendors used for those applications. A recent addition to the HIMSS Analytics Database is the EMR Adoption Model™, which scores hospitals on eight stages to creating a paperless record environment [14] (see Figure 1). The major limitation of the HIMSS Analytics Database is its reliance on self-reporting from hospitals which is sometimes inaccurate or incomplete (i.e. a hospital may misreport the number of IT employees, or may fail to answer the question at all). In addition, some sites outsource IT to various degrees or have services provided by other entities (e.g., a community hospital that is part of a larger health system network). Another limitation of the database is the lack of FTE categories that would include clinical informatics specialists. Even health care chief information officers acknowledge the importance of understanding health care [15], and clinical informaticians often provide the expertise that spans health care and IT. This has been addressed in a recent update to the database with new fields, although little data has yet been populated in them.
Figure 1.
Description of stages for the EMR Adoption Model [14].
These limitations aside, the HIMSS Analytics Database is the largest and most comprehensive source of data of its kind, and enabled us to investigate three research questions. First, we wanted to quantify the HIT workforce in the US generally. Second, we wanted to explore whether FTE levels for more advanced HIT, as measured by the EMR Adoption Model score, were different than for baseline levels. Finally, we wanted to estimate total HIT workforce needs in the US at present, and what will be required as more health care organizations adopt more advanced HIT. This research is part of our ongoing interest to better characterize the HIT workforce and understand the competencies and educational curricula for that workforce.
Methods
A query of the HIMSS Analytics Database was carried out on March 11, 2008 for the following data elements:
EMR Adoption Model score
Number of beds
Total hospital FTE
Total IT FTE
Total physicians
Number of IT staff by category
Some survey respondents did not provide information on the size of their IT staff, or provided estimates that were unreasonably small (such as 0 IT staff for a 340 bed hospital or 1 staff member for a 394 bed hospital). We excluded all hospitals that did not answer the staff size question or that indicated having fewer than 5 IT staff.
We computed IT staffing ratios, defined as the number of IT full-time equivalents (FTE) per hospital bed for each level of the EMR Adoption Model, and for our dataset overall. In order to allow for generalization, all comparisons were weighted by bed size. We used the staffing ratios to extrapolate the total number of IT staff required for to cover all licensed hospitals beds in the US, estimated at 761,607 according to the American Hospital Directory (http://www.ahd.com/state_statistics.html).
Results
The query of the database yielded a total of 4,929 hospitals for which an EMR Adoption Model score was available. After eliminating hospitals that did not answer the IT FTE question (n=2,490) and hospitals that listed the FTE has fewer than 5 (n=1,121), a total of 1,318 usable hospitals remained. Together, these hospitals had 372,840 licensed beds, representing 49.0% of all licensed hospital beds in the United States.
We found the overall IT staffing ratio to be 0.142 IT FTE per hospital bed. Extrapolating to all hospitals beds in the United States, this suggests a total current hospital IT workforce size of 108,390 FTE. We also found an IT to total staff ratio of 60.7, which was similar to the Gartner and England numbers described above.
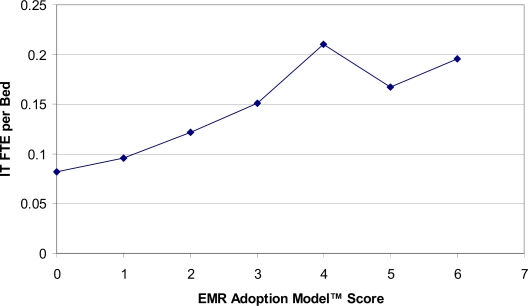
Average IT staffing ratios varied based on EMR Adoption Model score. Table 1 shows the average staffing ratio for each of the stages (there are currently no hospitals in the United States at adoption level 7). Figure 2 shows a graph of this relationship. Average staffing ratios generally increase with adoption score, but hospitals at level 4 have a higher average staffing ratio than hospitals at levels 5 or 6. If all hospitals were operating at the same staffing ratios as level 6 hospitals (0.196 IT FTE per bed), a total of 149,174 IT FTE would be needed to provide coverage – an increase of 40,784 FTE.
Table 1.
Hospitals, beds, and staffing ratios by EMR Adoption Model score.
| EMR Adoption Model | |||
|---|---|---|---|
| Score | Number of Hospitals | Total Beds | IT FTE per Bed |
| 0 | 60 | 9,069 | 0.082 |
| 1 | 132 | 30,391 | 0.096 |
| 2 | 437 | 120,315 | 0.122 |
| 3 | 538 | 157,383 | 0.151 |
| 4 | 81 | 29,439 | 0.210 |
| 5 | 39 | 15,256 | 0.167 |
| 6 | 31 | 10,987 | 0.196 |
Figure 2.
IT FTE per Bed vs. EMR Adoption Model score.
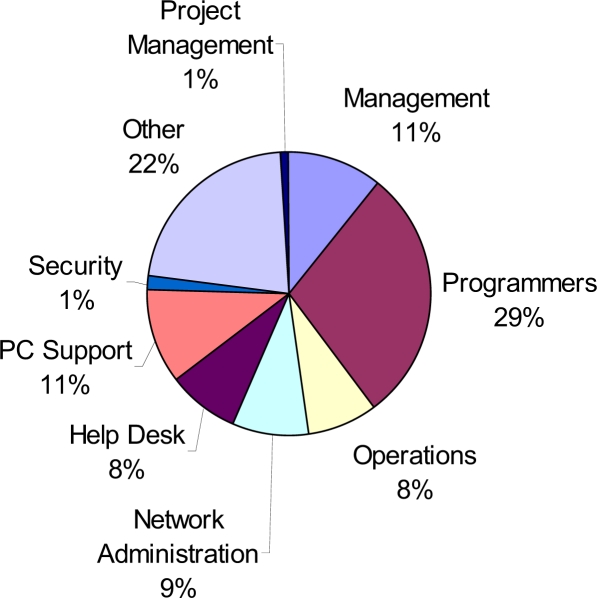
The database also provides a breakdown of IT job categories, although this data is reported with even lower frequency than overall IT staff. For the 816 hospitals in our analyzed set of 1,318 that reported job category data, we tallied the proportion in each category, as shown in Figure 3.
Figure 3.
Distribution of IT job categories.
Discussion
Our results provide one of the most comprehensive pictures to date of IT staffing needs of hospitals. IT staffing requirements rise as a more advanced infrastructure is implemented. While hospitals with basic implementation are utilizing about 0.1 IT staff per bed, this rises to around 0.2 IT staff per bed as hospitals advance from stage 1 to stage 4 implementation based on the HIMSS EMR Adoption Model. If our data represent a correct sampling of the entire US, then the current IT staff workforce is about 108,390 FTE. However, if the US HIT agenda is fulfilled and hospitals move to higher levels of adoption, more than 40,000 additional FTE will be required.
The data do not allow explanation of the leveling off of IT staff per bed at stages 5–6, but we believe this is likely due to the substantial amount of staff required for CPOE and CDS implementation at Stage 4. The IT staff per bed at stages 5–6 are still higher than at stages 0–3.
There are limitations to the data and our analysis. As described above, the HIMSS Analytics Database is self-reported and incomplete. Even further, however, is that the FTE data are currently limited to IT staff, and in particular exclude clinical informatics specialists who play a growing role in HIT implementations. This is being addressed by the database with the addition of new data elements being introduced in 2008 that attempt to capture these individuals.
Another limitation is that the 1,318 hospitals in the sample have 49% of the total US beds, indicating that un-sampled hospitals are small or medium sized hospitals, which may have fewer IT staff. In addition, the database does not indicated whether hospitals used any IT consultants or contractors. Many hospitals, such as Kaiser Permanente, work with IT consulting firms while implementing systems, and these IT consultants/contractors are a part of the IT staff.
As with other analyses of the HIT workforce described above, we have a very incomplete understanding not only of IT staff, but also informaticians, health information managers, and others who play increasingly important roles in implementation. This becomes relevant in the context of studies showing flawed implementations of HIT leading to adverse clinical outcomes [16], which may have been preventable with application of known best practices from informatics [17], and other analyses showing that most of the benefits from HIT have been limited to small numbers of institutions with highly advanced informatics programs [18].
This makes essential a more concerted research agenda to better characterize the HIT workforce and its job roles, required competencies, and optimal education. This will not only help HIT leaders implement systems better, but also assist educational programs in determining the best curricula for students training to fill these roles. Better understanding of the HIT workforce will also allow health care leaders to better understand and overcome the barriers to more effective HIT adoption.
Acknowledgments
We gratefully acknowledge HIMSS Analytics for use of the HIMSS Analytics Database and Dave Garets, Mike Davis, Lisa Pilolla, and Michelle Glenn of HIMSS Analytics for their help in obtaining and interpreting the data.
References
- 1.Brailer DJ. Health Care. Department of Health & Human Services; Washington, DC: 2004. The Decade of Health Information Technology: Delivering Consumer-centric and Information-Rich.http://www.hhs.gov/healthit/documents/hitframework.pdf [Google Scholar]
- 2.Blumenthal D, Glaser JP. Information technology comes to medicine. New England Journal of Medicine. 2007;356:2527–2534. doi: 10.1056/NEJMhpr066212. [DOI] [PubMed] [Google Scholar]
- 3.Hersh W. Health care information technology: progress and barriers. Journal of the American Medical Association. 2004;292:2273–2274. doi: 10.1001/jama.292.18.2273. [DOI] [PubMed] [Google Scholar]
- 4.Poon EG, et al. Overcoming barriers to adopting and implementing computerized physician order entry systems in U.S. hospitals. Health Affairs. 2004;23:184–190. doi: 10.1377/hlthaff.23.4.184. [DOI] [PubMed] [Google Scholar]
- 5.Anonymous, Building the Work Force for Health Information Transformation . American Health Information Management Association and American Medical Informatics Association; Chicago, IL and Bethesda, MD: 2006. http://www.ahima.org/emerging_issues/Workforce_web.pdf [Google Scholar]
- 6.Hersh WR. Who are the informaticians? What we know and should know. Journal of the American Medical Informatics Association. 2006;13:166–170. doi: 10.1197/jamia.M1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perlin JB, Gelinas LS. American Health Information Community; Washington, DC: 2008. Electronic Health Records Workgroup Recommendations.http://www.hhs.gov/healthit/documents/m20080115/09-ehr_recs_ltr.html [Google Scholar]
- 8.Eardley T. ASSIST; London, England: 2006. NHS Informatics Workforce Survey.http://www.bcs.org/upload/pdf/finalreport_20061120102537.pdf [Google Scholar]
- 9.Leviss J, Kremsdorf R, Mohaideen MF. The CMIO - a new leader for health systems. journal of the American Medical Informatics Association. 2006;13:573–578. doi: 10.1197/jamia.M2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaffer V, Lovelock J. Gartner; Stamford, CT: 2007. Results of the 2006 Gartner-AMDIS Survey of CMIOs: Bridging Healthcare’s Transforming Waters.http://www.gartner.com/DisplayDocument?ref=g_search&id=504632 [Google Scholar]
- 11.Gabler J. Gartner Corp; Stamford, CT: 2003. 2003 Integrated Delivery System IT Budget and Staffing Study Results. [Google Scholar]
- 12.Wing P, et al. American Health Information Management Association; Chicago, IL: 2003. Data for Decisions: the HIM Workforce and Workplace - 2002 Member Survey.http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_018947.pdf [Google Scholar]
- 13.Anonymous, Nationwide Health Information Network (NHIN) Workforce Study. Altarum Institute; Ann Arbor, MI: 2007. http://aspe.hhs.gov/sp/reports/2007/NHIN/NHINReport.pdf [Google Scholar]
- 14.Anonymous, The EHR Adoption Model. Healthcare Information Management and Systems Society; Chicago, IL: 2007. http://www.himssanalytics.org/docs/EMRAM_att_corrected.pdf [Google Scholar]
- 15.Monegain B. Healthcare IT: is it a breed apart? Healthcare IT News. Sep 4, 2004. http://www.healthcareitnews.com/story.cms?id=1522
- 16.Han YY, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005;116:1506–1512. doi: 10.1542/peds.2005-1287. [DOI] [PubMed] [Google Scholar]
- 17.Sittig DF, et al. Lessons from “unexpected increased mortality after implementation of a commercially sold computerized physician order entry system”. Pediatrics. 2006;118:797–801. doi: 10.1542/peds.2005-3132. [DOI] [PubMed] [Google Scholar]
- 18.Chaudhry B, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine. 2006;144:742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]