Abstract
The infusion of health care technologies into the home leads to substantial changes in the nature of work for home care nurses and their patients. Nurses and nursing practice must change to capitalize on these innovations. As part of a randomized field experiment evaluating web-based support for home care of patients with chronic heart disease, we engaged nine nurses in a dialogue about their experience integrating this modification of care delivery into their practice. They shared their perceptions of the work they needed to do and their perceptions and expectations for patients and themselves in using technologies to promote and manage self-care. We document three overarching themes that identify preexisting factors that influenced integration or represent the consequences of technology integration into home care: doing tasks differently, making accommodations in the home for devices and computers, and being mindful of existing expectations and skills of both nurses and patients.
Introduction
Technology is assuming an increasingly important role in quality and patient safety in the current health care environment [1], and nurses and models of patient care delivery are at the core of many technology innovations. In response, technological supports for clinical decision-making [2], electronic documentation systems [3], and information seeking resources are being implemented.
Although nurses play key roles in the integration of information technology into patient care, their roles are rarely made explicit in the design and deployment of consumer health informatics applications. For example, the Baby CareLink project [4] deployed a video link and web resources between Neonatal Intensive Care Units and patient homes. Nurses played significant roles: positioning the camera to allow parents to view the infant during the care process, instructing families on the use of the web site, and assessing parents’ readiness to understand and interpret the web resource. Though their role was critical in the implementation, the nurses were neither research subjects nor research staff.
This paper reports the experience of nurses participating in the HeartCare II study, a randomized field experiment evaluating the impact of a web-based support for home care patients on selected clinical outcomes. The web-based resource was designed based on existing nursing practice approaches to caring for patients with chronic heart disease. It was envisioned to add technology support to both the nurse and the patient, affording such support as recording of vital signs, creating trend plots of daily weights, providing access to educational materials, and serving as a communication link between patients and providers. The system was designed for use by the patient alone, the nurse alone, or the nurse and the patient together. Patients were permitted to use their own computers; project funds paid for computers and internet access for patients who did not have them.
The study took place in a home care nursing agency situated within a defined radius of a Midwest metropolitan area. Six agency offices were randomly assigned: three experimental and three comparison. Demographic data, including socioeconomic status, educational level, race, and the mix of rural/suburban/urban households was comparable between the two groups. In the experimental offices all nurses were engaged in the design of the web-based resources and all received in-depth training in the use of the technology as well as strategies to enhance elders’ abilities to capitalize on the self-management tools provided by the technology. Home care nurses played a central role in this study. While neither research subject nor research staff, they were part of the work system that we anticipated would be modified by the technology.
The purpose of this qualitative study was to explore factors that shaped the integration of technology into nursing practice by the nurses of the HeartCare II study. This study examines nurses’ perceptions of a broad range of issues and factors that emerge in a significantly different environment than the typical clinical environments commonly found in health IT installations—the patient’s home.
Theoretical Framework
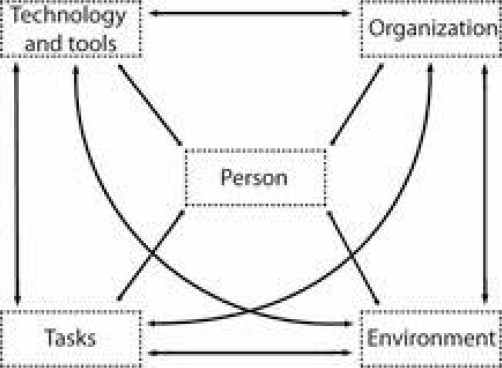
While many frameworks can be used to understand how technology influences clinical practice (e.g. the Technology Acceptance Model [5]), we chose the SEIPS work systems model (Figure 1) [6]. Drawn from Socio-technical Systems Theory, the model characterizes work as a series of tasks accomplished through the use of certain tools and technologies by individuals under a given organizational context located in a specific physical environment. Although the interactions and mutual influence possible across these five elements is shown as bidirectional relationships, the model conceptually includes multilevel interactions that cannot be physically represented on a two-dimensional drawing. This interaction and mutual influence is the “work system”. In our case, the nurse’s task is to teach self-management to patients with chronic cardiac disease, with home care nurses and their patients using tools (blood pressure monitors, weight scales, etc) in the patients’ homes. The web-based technology becomes a shared tool for nurses and patients in this implementation.
Figure 1.
SEIPS Work System Model [6]
Methods
We conducted a purposive sampling of home care nurses involved in using the HeartCare II website in their practice- the Experimental Group. In an attempt to efficiently understand the range of experiences, we specifically sought out nurses who expressed strong feelings about the technology, both positive and negative. The nurses who were asked to participate were identified by their ability to express their views. Imposing this requirement may have imposed a risk of bias; however, the nature of our questions required the articulation of viewpoints. Specific interview questions were developed around the main research question: “What are the experiences of home care nurses using technology to enhance their practice?”
Ten nurses from the three home care offices involved in the experimental arm of the study consented to participate; nine were present for the discussions and were compensated for their time. Two-hour semi-structured group interview sessions were conducted and moderated by two graduate students (one in engineering and one in nursing) for one group of 5 nurses and one group of 4 nurses.
Data Analysis
After each focus group the graduate students discussed the sessions informally and identified broad themes. Digital audio recordings, written transcripts, and field notes were analyzed after the sessions were completed. Using inductive content analysis [7], 35 minor themes were identified during data review.
First independently and then through consensus, these 35 themes were examined in the context of the SEIPS model. True to the interactive nature of the elements, researchers found it difficult to consistently sort the themes into single model elements; the identified themes represented more than one model element. For example, the theme “Some patients don’t want technology in their homes” is reflection of a person and their values, and it is an environment.
After careful thought and consideration, we identified three overarching themes that codify the experiences of these nine nurses with technology integration in the home. These three themes represent preexisting factors influencing integration as well as the consequences of technology integration into home care: doing tasks differently, making accommodations in the home, and being mindful of existing expectations and skills of both nurses and patients.
Results
Doing tasks differently: Person, Technology/Tools, and Task
In addition to completing a physical assessment, the central task of the home care nurse is to teach self-monitoring and self-management. Use of the HeartCare II website involved a shift of this task from a person-to-person activity to a technology supported activity. This was such a shift that some nurses were unclear as to how this would benefit their patients.
I wanted to make my point of … you know, diet, exercise, all those things, and not … spend as much time on the technology.
A ripple effect of this shift was that nurses were required to deal with technology issues, such as difficulty logging in, slow connection speeds, password issues, re-boots - tasks not considered to be in the domain of nursing.
I shouldn’t have to deal with technology-type things. But I was asked to do that, and I was not appreciative of that either.
This technology was new for many of the patients as well. Because of the level of computer literacy of some patients, the task of learning self-monitoring expanded to include learning some basic computer skills. Passwords were a stumbling block.
Just ‘click on ME’, something real basic. The password is what stumbled a lot of people … And I think that’s what stopped them from doing it in when we first got into the home.
Nurses felt that, for themselves, the data entry (weight, blood pressure) was a redundant task; information still had to be entered on their own documentation system. Some wished for remote access of patient monitoring, but commented that any changes to patient condition still required a call to the physician. Physician monitoring of data was not seen as realistic.
Despite all of these comments, nurses felt that the HeartCare knowledge resources 1) improved their clinical teaching, 2) prompted further information seeking, 3) made teaching more interactive and exciting for the patient, and 4) provided current medication information to keep nurses up to date or triggered oft missed points.
Making accommodations in the home: Person, Technology/Tools, and Environment
Putting computers into homes was met with more resistance than expected. Environments were described by nurses as being cluttered, with patients not enthusiastic about moving their belongings. Moving furniture to make space for a computer only to discover that the outlet or phone jack was nonfunctioning was frustrating for nurses and patients alike.
Well there’s a phone jack behind the bed. The bed wouldn’t budge. The bed weighed 7,000 pounds, so we moved the bed, there’s no jack there; you know? Or, “Take it out of here, you know? I don’t want this thing. Get rid of it. It doesn’t fit in the bedroom.”
I did have some situations where, because of certain family members, they purposely DID NOT want the computer in the house. They thought it would be damaged, (or) they had animals, (or) had family members that would steal.
High-speed internet service was difficult to obtain or was unreliable in some rural and urban areas, creating long waits for page loading. Some nurses used this time to complete patient physical assessments; others became too frustrated to continue using it.
Being mindful of expectations and skills of both nurse and patient: Person, Task, Technology/Tools, Organization
This overarching theme holds rich data about the preexisting perceptions of both the nurse and the patient with the application of this innovation. Since nurse demographics were not collected for this study, the age, experience or training of the nurse cannot be evaluated as a factor affecting integration.
As stated earlier, the technology required basic computer skills, different skills than those expected in the nurses’ daily work performed on a stand- alone computer system. Not having some requisite skills caused anxiety, especially when the patient was looking to the nurse to be the expert.
Look at me: I’m a very competent, good nurse, and yet my computer skills are pretty minimal. I get nervous when I have to do it.
A “train the trainer” model [8] was used in preparing nurses to teach patients to use the technology, but many nurses felt that this was not adequate. Many wanted detailed and printed step-by-step instructions, “like a recipe”, to carry with them, despite the fact that they were given pocket manuals outlining functions and use of the system.
There was a very strong sentiment by some of the nurses, and in some of the nurses’ perceptions of the patients, that technology did not belong in the home. Their vision of home care nursing did not include any technology beyond that which they were already using. Some nurses expressly stated:
Putting the computer in there is like adding in a cold component to what should be a more personal relationship
Some people just don’t want those technologies installed into their homes… they’ve got their own kind of things going on, their own make up, their own karma, and that doesn’t belong there.
Nurses felt pressed for time in terms of single visit length and number of visits. A corollary to this is that nurses felt that time was too short to incorporate the technology into their practice.
We’re looking at less than 2 weeks. I frequently had only 1 or 2 visits left before they started Cardiac Rehab; I mean there was just no TIME for it. Now if you’ve got a regular CHFer and you KNOW you’ve got … 3-4-5 (visits), then you’re better off.
We’re just trying to teach a boat load of information and “X’ amount of visits and they’re already overwhelmed … you say “Computers” and you’ve already lost them.
Overall, home care nurses felt that the following patient characteristics made integration more difficult: older patients who were “unable to see font size”, those who had “slow typing skills”, and patients described as acutely ill.
Other ones were… in there doing it; they’re having a good old time; that’s how I knew about the med (information), you know, certain places where they went to eat, and this and that. And so it just depends upon the person. That was what I found out. (But) for the demands of what’s on these folks, to teach my patients … it was a pain, because it was just that much more I had to do, and I wanted to make my point of the teaching, not the computer.
However, one nurse kept encouraging her patients.
And I keep telling them “The more you use it, the more (comfortable) you’re going to get to it, and … it’s going to be a great experience. But you have to use it; you cannot be afraid of it.” “Well, I think I might break it.” “No, you’re not going to break it. Just play with it.” I couldn’t get anyone to do that.
Nurses reported that patient familiarity with computers, and a desire to use the computer to self-manage their illness, or to “prove” their compliance with a recommended regimen made integration easier.
…and I think he had a computer in his room too. But he was very motivated to do everything he could to keep himself out of the hospital.
Patients have their own priorities and expectations.
We do have a lot of non-compliance from people who come from a low socio-economic background; the last thing they worry about is (their) health when (they) barely know where (they’re) going to stay from day-to-day. We could never get over that. (He’d say) “You’re here to help me…it’s your job.”
Discussion
The technology of the HeartCare II project, designed to enhance nursing practice, represented significant changes to the home health nurses’ work system. The SEIPS work system model guided our understanding of the nurses’ expressed experiences, and led us to the identification of factors that influenced technology integration in the home.
The task of teaching self-management using hard copy information changed to one with a more collaborative nature using technology. The technology begins as a shared tool, and as the patient progresses toward autonomy, he or she becomes primary owner. The overarching theme of “Doing tasks differently” highlights the need to see immediate value in changes or additions to the current tasks. Some patients and nurses were able to accomplish this. The theme of “Making accommodations in the home” illuminates the difference in the “structure” of this health care setting. “Being mindful of patient and nurse expectations and skills” represents subtle psychosocial factors influencing integration. The patient may be preserving the dependency of the “sick role”. Nurse perceptions of the patient as too sick to use the technology preserve the traditional nursing role of the nurse taking care of the patient. Personal views of the purview of nursing, from both patient and nurse, are revealed.
The SEIPS element of “person” is common to every theme. What is highlighted by this study is the fact that there are two persons in this health care interaction, representing dynamic and sometimes overlapping work systems.
Conclusion
Although the results of this small study spotlight the highly interactive nature of the work system, it is useful to return to five identified SEIPS model elements to couch implications for the national health care IT agenda. Technology and tools must be sensitive to physical limitations (sensory, cognitive, pain, medication side effects). In the home, privacy was not deemed to be an issue and the use of passwords was an impediment to use. In terms of the organization, the data entry by patients and nurses must be used, either for physician retrieval during appointments or for remote monitoring by the nurse or physician office. If a current system of data entry is already “working” (e.g., recording my weight on the calendar), data entry to another system is redundant, especially if no one else uses the information. Home health IT must fit easily in the physical environment, and be congruent to the personal choices and values of the person who lives there, and it must acknowledge the limited technology resources currently available in some urban and rural areas. Tasks are carried out autonomously in the home care setting, putting both the decision to integrate and the onus of IT support on the home care nurses, who are already experiencing definite tension about the amount of tasks to do on a home care visit, and the time allotted to complete them.
The final model element in this work system, person, represents two different individuals – nurse and patient. The fact that some of the nurses found and used the medication information may signal online reference tools as a starting point for the integration of other IT support practice tools. The National League for Nursing [9] and others highlight the need for preparing the next generation of nurses to practice in a technology-rich environment, but today’s home care nurses--those who are in place and testing IT implementations--are not new graduates. Medical-surgical nursing experience is an expected background in this autonomous environment; the home care nurse is one who is more seasoned. Teaching computer technology to the experienced home care nurse, who may have left hospital nursing specifically to escape the technological environment, implies the need for a different kind of continuing education.
For patients, home health IT requires a more active role, which may be limited by pain, medication use, sensory limitations, economic condition, and personal values and opinions. If data input from the patient is received and acted upon, the patient is more likely to see value in recording and monitoring, and more likely to become a more active participant in their care.
Acknowledgments
This work was supported in part by a grant from National Library of Medicine (R01-LM6249) and the National Science Foundation Graduate Research Fellowship Program (Fellowship ID# 2005024457). We acknowledge the collaborating Home Care agency and thank the Brennan Health Systems Lab for its support.
References
- 1.Ball MJ, Weaver C, Abbott PA. Enabling technologies promise to revitalize the role of nursing in an era of patient safety. International Journal of Medical Informatics. 2003;69:29–38. doi: 10.1016/s1386-5056(02)00063-1. [DOI] [PubMed] [Google Scholar]
- 2.Weber S. Critical care nurse practitioners and clinical nurse specialists interface patterns with computer-based decision support systems. J of Amer Acad of Nurse Practitioners. 2007;19:580–590. doi: 10.1111/j.1745-7599.2007.00262.x. [DOI] [PubMed] [Google Scholar]
- 3.Saletnik NA, Niedlinger MK, Wilson M. Nursing resource considerations for implementing an electronic documentation system. AORN. 2008;87(3):583–596. doi: 10.1016/j.aorn.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 4.Gray JE, Safran C, Davis RB, et al. Baby CareLink: using the internet and telemedicine to improve care for high-risk infants. Pediatrics. 2000;106(6):1318–24. doi: 10.1542/peds.106.6.1318. [DOI] [PubMed] [Google Scholar]
- 5.Venkatesh V, Davis F. A theoretical extension of the technology acceptance model: four longitudinal field studies. Management Science. 2000;46(2):186–204. [Google Scholar]
- 6.Carayon P, Schoofs Hunt A, Karsh B-T, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(Suppl 1):i50–i58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patton MQ. Qualitative Research Methods. 3rd ed. Thousand Oaks: Sage; 2002. [Google Scholar]
- 8.Or KL, Valdez RS, Casper GR, et al. Human factors, ergonomics, and health information technology in home care – a perspective from work system analysis. Work._Accepted for publication in 2009.
- 9.National League for Nursing. (2008, May 9). Position Statement: Preparing the next generation of nurses to practice in a technology-rich environmentan informatics agenda. Retrieved June 26, 2008 from http://www.non.org/aboutnln/positionstatements/index.htm